GDF-15 in Metabolic Disease: From Stress Response Hormone to Therapeutic Target for Diabetes and Obesity
This article provides a comprehensive analysis of Growth Differentiation Factor 15 (GDF-15) as a critical mediator in metabolic homeostasis, with a focus on its therapeutic potential for diabetes and obesity.
GDF-15 in Metabolic Disease: From Stress Response Hormone to Therapeutic Target for Diabetes and Obesity
Abstract
This article provides a comprehensive analysis of Growth Differentiation Factor 15 (GDF-15) as a critical mediator in metabolic homeostasis, with a focus on its therapeutic potential for diabetes and obesity. We explore the foundational biology of GDF-15, including its induction by cellular stress and its role in appetite regulation via the GFRAL receptor in the hindbrain. The review details current methodologies for measuring GDF-15 and the development of GDF-15 mimetics and pathway modulators as pharmacological agents. We address key challenges in therapeutic targeting, such as mitigating potential side effects like nausea and tachyphylaxis. Finally, we compare GDF-15-based approaches to existing and emerging anti-obesity drugs (e.g., GLP-1 receptor agonists), evaluating efficacy, mechanisms, and clinical trial data. This synthesis is intended for researchers, scientists, and drug development professionals seeking to understand the translational landscape of this promising metabolic hormone.
Unraveling GDF-15: The Biology of a Metabolic Stress Signal and Its Receptor GFRAL
Growth Differentiation Factor 15 (GDF-15), also known as Macrophage Inhibitory Cytokine-1 (MIC-1) and NSAID-activated gene-1 (NAG-1), is a distant member of the Transforming Growth Factor-β (TGF-β) superfamily. It functions as a stress-responsive cytokine, playing critical roles in cellular stress, inflammation, and energy homeostasis. Its profound effects on appetite and body weight regulation have positioned it as a pivotal molecule in diabetes and obesity research, with recent investigations targeting its receptor, GFRAL, for therapeutic intervention.
Structure and Molecular Characteristics
GDF-15 shares the canonical structural features of TGF-β superfamily members but exhibits low sequence homology (<30%). Its synthesis, maturation, and secretion follow a specific pathway.
Table 1: Molecular Characteristics of Mature Human GDF-15
| Property | Detail |
|---|---|
| Gene Locus | 19p13.11 |
| Pre-pro-protein Length | 308 amino acids (aa) |
| Pro-domain Length | ~167 aa (cleaved) |
| Mature Dimer Length | 112 aa (25 kDa monomer, 50 kDa disulfide-linked dimer) |
| Conserved Structural Motifs | TGF-β superfamily cysteine knot motif |
| Post-translational Modification | N-linked glycosylation (Asn-70) |
| Active Form | Non-covalent dimer associated with pro-domain |
Maturation Pathway:
- Synthesis: Produced as a pre-pro-protein containing a signal peptide, a large pro-domain, and the mature C-terminal domain.
- Cleavage: Furin and other proprotein convertases cleave the pro-domain from the mature domain within the secretory pathway.
- Secretion: The mature dimer remains non-covalently associated with its pro-domain, which is essential for its stability and bioactivity. The complex is secreted as a latent form.
- Activation: In vivo activation mechanisms are not fully elucidated but are hypothesized to involve protease-mediated cleavage of the pro-domain in specific tissue contexts (e.g., in the target medulla oblongata).
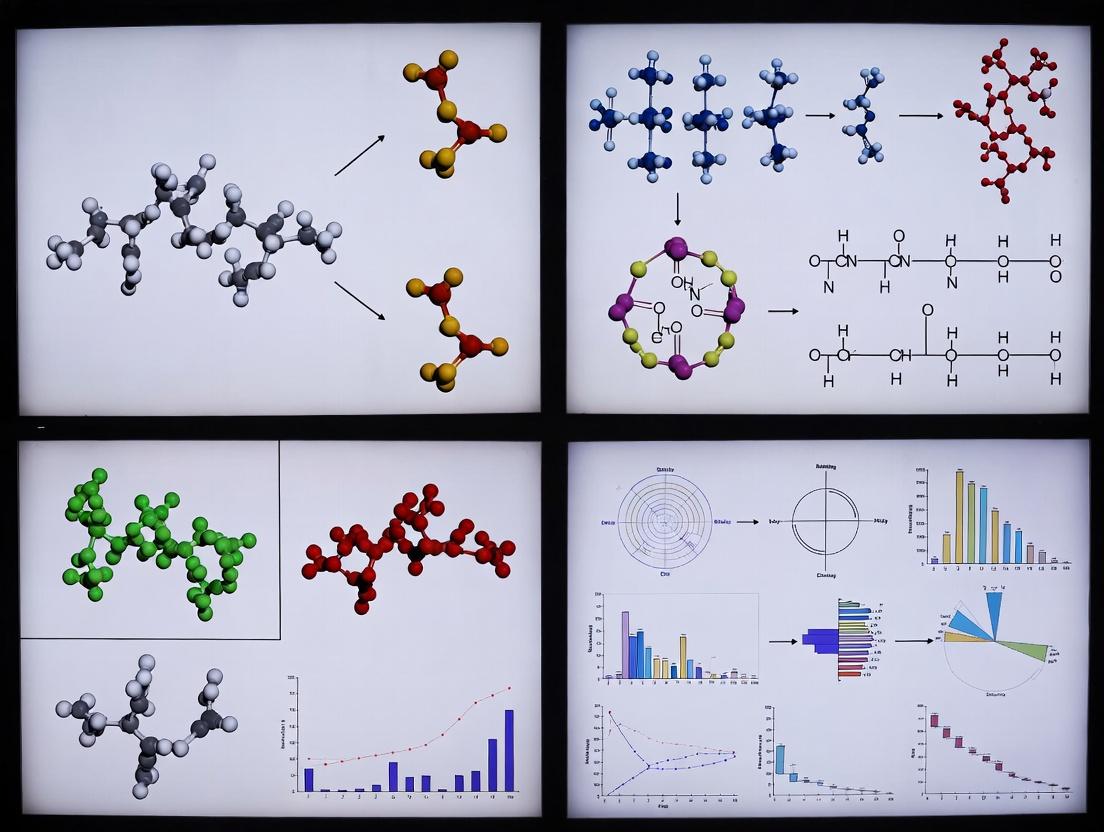
Diagram Title: GDF-15 Biosynthesis and Secretion Pathway
Historical Context within the TGF-β Superfamily
The discovery and classification of GDF-15 occurred through the lens of TGF-β biology.
Table 2: Historical Timeline of GDF-15 Research
| Year | Key Milestone | Significance |
|---|---|---|
| 1997 | Cloned as "Placental TGF-β" (PTGFB) and "Prostate Differentiation Factor" (PDF). | Initial identification from reproductive tissues. |
| 2000 | Identified as Macrophage Inhibitory Cytokine-1 (MIC-1). | Established link to inflammation and macrophage biology. |
| 2001 | Recognized as a divergent TGF-β superfamily member, named GDF-15. | Formal classification within the structural framework. |
| 2007-2012 | Correlated with pathological states (cardiac injury, cancer cachexia). | Emerged as a broad biomarker of cellular stress and disease. |
| 2017 | Receptor GFRAL identified in hindbrain; mediates appetite suppression. | Paradigm shift: Defined central mechanism for metabolic effects. |
| 2019-Present | Therapeutic GDF-15 analogs and GFRAL-targeting strategies developed for obesity. | Translation into drug development pipelines. |
Signaling Pathway: The GFRAL-RET Mechanism
GDF-15 signals through a unique, highly specific receptor complex distinct from other TGF-β members, explaining its unique physiological effects.
Diagram Title: GDF-15 Signaling via GFRAL and RET
Detailed Mechanism:
- Ligand-Receptor Binding: Active GDF-15 dimer binds with high affinity to the GDNF-family receptor α-like (GFRAL), expressed almost exclusively in the area postrema and nucleus tractus solitarius of the hindbrain.
- Co-receptor Recruitment: GDF-15 binding induces the recruitment of the transmembrane tyrosine kinase RET (Rearranged during Transfection) to form a ternary complex.
- Kinase Activation: RET undergoes trans-autophosphorylation, activating its intracellular tyrosine kinase domain.
- Downstream Signaling: Phosphorylated RET activates key intracellular pathways, including PI3K/AKT, PLCγ, and MAPK/ERK.
- Neuronal Response: This signaling cascade activates GFRAL-expressing neurons, leading to integrated anorexigenic (appetite-suppressing) signals.
- Systemic Effect: Reduced food intake and altered metabolism result in body weight loss, a key therapeutic target in obesity.
Key Experimental Protocols
Protocol 1: Measuring GDF-15 Serum/Plasma Levels in Metabolic Studies (ELISA)
Objective: Quantify circulating GDF-15 levels in human or rodent models of diabetes/obesity. Materials: See "Research Reagent Solutions" below. Method:
- Sample Collection: Collect blood in EDTA or heparin tubes. Separate plasma via centrifugation (1,000-2,000 x g, 10 min, 4°C). Store at -80°C.
- Assay Setup: Use a validated, high-sensitivity human or murine GDF-15 ELISA kit. Dilute samples and standards per manufacturer's instructions (typical dilution 1:5 to 1:20).
- Procedure:
- Coat wells with capture antibody.
- Block with assay diluent (1-2 hours).
- Add standards and samples in duplicate (incubate 2 hours, room temperature).
- Wash plates 4-6 times.
- Add detection antibody conjugated to HRP (1-2 hours).
- Wash plates.
- Add TMB substrate (incubate 15-30 min).
- Stop reaction with stop solution.
- Analysis: Read absorbance at 450 nm (reference 570/620 nm). Generate a 4- or 5-parameter logistic standard curve. Report concentrations in pg/mL.
Protocol 2: Assessing GDF-15-Mediated Anorexia in Mice
Objective: Evaluate the in vivo effect of GDF-15 administration on food intake and body weight. Materials: Recombinant GDF-15 protein, osmotic minipumps or injection supplies, metabolic cages, control protein (e.g., vehicle). Method:
- Animal Model: Use diet-induced obese (DIO) C57BL/6J mice or wild-type lean controls.
- Compound Administration: Administer recombinant GDF-15 (e.g., 0.1-0.5 mg/kg/day) or vehicle control via continuous subcutaneous infusion using osmotic minipumps for 7-14 days, or via daily bolus injection.
- Phenotypic Monitoring:
- Food Intake: Measure daily food intake (±0.1 g). Acclimate mice to handling and powdered diet if using metabolic cages.
- Body Weight: Weigh animals daily at the same time.
- Body Composition: Use EchoMRI or DEXA pre- and post-study to quantify fat and lean mass loss.
- Energy Expenditure: Optional: Use indirect calorimetry (CLAMS) to measure O₂ consumption and CO₂ production.
- Tissue Collection: At endpoint, collect brainstem (area postrema/nucleus tractus solitarius) for p-RET or c-Fos immunohistochemistry to confirm target engagement.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for GDF-15 Research
| Reagent / Material | Function / Application | Example / Notes |
|---|---|---|
| Recombinant GDF-15 Protein | In vitro and in vivo functional studies; stimulation assays. | Human or murine, carrier-free, from HEK293 or E. coli systems. Verify activity in a cell-based assay. |
| High-Sensitivity GDF-15 ELISA Kits | Quantification of GDF-15 in serum, plasma, or cell culture supernatant. | Critical for biomarker studies. Choose species-specific kits (e.g., R&D Systems DuoSet, Biovendor, Abcam). |
| Anti-GDF-15 Antibodies | Western blot, immunohistochemistry (IHC), neutralization. | Neutralizing antibodies (e.g., clone MAB957, R&D Systems) are key for loss-of-function experiments. |
| Anti-GFRAL Antibodies | IHC, Western blot, receptor detection. | Validate specificity in Gfral knockout tissues. Often used to map central expression. |
| Anti-phospho-RET Antibodies | Detection of activated receptor complex in target tissues (e.g., brainstem). | Key pharmacodynamic biomarker for in vivo target engagement (e.g., Cell Signaling Technology #3221). |
| GFRAL Knockout Mice | Essential control for establishing on-target specificity of GDF-15 effects. | Jackson Laboratory (Stock #034106) or in-house generated models. |
| Cell Line Expressing GFRAL/RET | In vitro signaling and receptor binding assays. | Engineered cell lines (e.g., HEK293 overexpressing GFRAL and RET) are used for ligand-receptor interaction studies. |
| Osmotic Minipumps (Alzet) | For chronic, sustained delivery of GDF-15 or analogs in rodent models. | Model 1004 (28 days) is commonly used for metabolic studies. |
Growth Differentiation Factor 15 (GDF-15) is a divergent member of the TGF-β superfamily, emerging as a critical stress-responsive cytokine. Within the context of metabolic disease research, particularly diabetes and obesity, GDF-15 is recognized as a biomarker of cellular distress and a potential therapeutic target. Its circulating levels correlate strongly with body mass index, insulin resistance, and cardiovascular complications. This whitepaper provides an in-depth technical analysis of the three primary cellular triggers that induce GDF-15 expression: Endoplasmic Reticulum (ER) Stress, Mitochondrial Dysfunction, and Inflammatory Signaling, synthesizing current knowledge for research and drug development applications.
ER Stress-Mediated Induction of GDF-15
ER stress activates the unfolded protein response (UPR) through three sensor proteins: IRE1α, PERK, and ATF6. GDF-15 is a direct transcriptional target of the integrated stress response downstream of PERK activation.
Key Signaling Pathway:
- Accumulation of misfolded proteins dissociates BiP/GRP78 from PERK.
- PERK dimerizes and autophosphorylates, leading to phosphorylation of eukaryotic initiation factor 2α (eIF2α).
- Phosphorylated eIF2α (p-eIF2α) attenuates global translation but selectively promotes the translation of ATF4 mRNA.
- ATF4 translocates to the nucleus and, along with CHOP (DDIT3), binds to specific response elements (e.g., amino acid response elements [AAREs]) in the GDF15 promoter, driving its expression.
Title: ER Stress UPR Pathway to GDF-15 Induction
Quantitative Data Summary: Table 1: GDF-15 Induction by Pharmacological ER Stress Inducers In Vitro
| Cell Type | ER Stressor | Concentration | Time | Fold Increase in GDF-15 (mRNA/Protein) | Key Mediator Confirmed |
|---|---|---|---|---|---|
| HepG2 (Human hepatoma) | Tunicamycin | 2 µg/mL | 24h | mRNA: 8-12x / Protein: 10-15x | ATF4/CHOP (siRNA knockdown) |
| THP-1 (Human macrophage) | Thapsigargin | 300 nM | 16h | mRNA: 15-20x / Protein: 20-25x | PERK inhibition (GSK2606414) |
| Primary mouse hepatocytes | Brefeldin A | 5 µM | 18h | mRNA: 5-8x | XBP1 splicing (IRE1α branch) minor role |
Detailed Protocol: Assessing GDF-15 Induction via the PERK-ATF4 Axis
- Cell Treatment: Seed HEK293 or relevant cell line in 6-well plates. At 80% confluence, treat with vehicle (DMSO <0.1%) or PERK-specific ER stress inducer (e.g., 300 nM Thapsigargin).
- Inhibitor Control: Pre-treat cells with a PERK inhibitor (e.g., GSK2606414 at 1 µM) for 1 hour prior to thapsigargin addition.
- Time Course: Harvest cells at 0, 4, 8, 16, and 24h post-treatment (n=3 per time point).
- Sample Processing:
- mRNA: Extract total RNA (TRIzol), synthesize cDNA. Perform qRT-PCR for GDF15 using TaqMan probes (Hs00171132_m1). Normalize to ACTB or GAPDH.
- Protein: Lyse cells in RIPA buffer with protease/phosphatase inhibitors. Perform Western blotting for GDF-15 (rabbit anti-GDF-15, abcam ab199173, 1:1000), p-eIF2α (CST #9721, 1:1000), ATF4 (CST #11815, 1:1000), and loading control (β-Actin).
- Nuclear Extract & ChIP: At peak induction (e.g., 8h), prepare nuclear extracts. Perform Chromatin Immunoprecipitation (ChIP) using an anti-ATF4 or anti-CHOP antibody, followed by qPCR of the human GDF15 promoter region containing putative AARE sites.
Mitochondrial Dysfunction-Driven GDF-15 Expression
Mitochondrial stress triggers GDF-15 expression via the integrated mitochondrial stress response (MSR), centered on the transcription factor ATF4, often independently of classic UPR.
Key Signaling Pathway:
- Electron transport chain (ETC) inhibition, ROS overproduction, or mitochondrial membrane depolarization activates one or more of the four mitochondrial-regulated eIF2α kinases: HRI, PERK, PKR, or GCN2.
- These kinases converge on eIF2α phosphorylation, mimicking the ER stress pathway.
- p-eIF2α drives ATF4 translation and nuclear translocation.
- ATF4, potentially with co-factors like CHOP, activates GDF15 transcription. The OMA1-DELE1-HRI axis is a recently elucidated specific route for mitochondrial protein import stress.
Title: Mitochondrial Stress Pathways to GDF-15
Quantitative Data Summary: Table 2: GDF-15 Induction by Mitochondrial Perturbations
| Stimulus/Model | Cell/System | Readout | Fold Increase | Proposed Primary Mediator |
|---|---|---|---|---|
| Antimycin A (ETC CIII inhibitor) | C2C12 myotubes | Secreted GDF-15 protein | 8-10x | ATF4 (MSR) |
| Oligomycin (ATP synthase inhibitor) | Primary human adipocytes | GDF15 mRNA | 6-9x | p-eIF2α |
| Mt-ND6 mutant cybrid cells | Human osteosarcoma | Plasma GDF-15 (in vivo) | ~3x (vs. wild-type) | Chronic MSR |
| Rotenone (ETC CI inhibitor) | SH-SY5Y neuronal cells | mRNA & Protein | mRNA: 12x / Protein: 7x | ROS & ATF4 |
Detailed Protocol: Measuring GDF-15 in Mitochondrial Stress Models
- Inducing Mitochondrial Dysfunction:
- Pharmacological: Treat cells with ETC inhibitors (e.g., 1 µM Antimycin A, 10 µM Oligomycin, 100 nM Rotenone) or uncouplers (e.g., 10 µM CCCP) for 6-24h. Include antioxidants (e.g., 5 mM N-acetylcysteine) to test ROS involvement.
- Genetic: Use siRNA to knock down key mitochondrial components (e.g., TFAM, PHB2) or utilize ρ⁰ (mitochondrial DNA-depleted) cell lines.
- Multiparameter Assessment:
- GDF-15 Secretion: Collect conditioned media. Use a sensitive ELISA (e.g., Quantikine ELISA Human GDF-15, R&D Systems DGD150) following manufacturer's protocol.
- Mitochondrial Function: In parallel wells, measure ROS (DCFDA or MitoSOX fluorescence), mitochondrial membrane potential (JC-1 or TMRM staining via flow cytometry), and oxygen consumption rate (Seahorse XF Analyzer).
- Pathway Analysis: Perform Western blot for MSR markers: p-eIF2α, ATF4, and mitochondrial stress markers like LONP1 or HSP60.
Inflammatory Signaling and GDF-15 Regulation
Pro-inflammatory cytokines, particularly TNF-α and IL-1β, robustly induce GDF-15 via NF-κB and MAPK (p38, JNK) signaling pathways, linking systemic inflammation to metabolic stress signaling.
Key Signaling Pathways:
- NF-κB Pathway: TNF-α binding to TNFR1 triggers IKK complex activation, leading to IκBα phosphorylation and degradation. This releases NF-κB (p65/p50), which translocates to the nucleus and binds κB sites on the GDF15 promoter.
- MAPK Pathways: TNF-α/IL-1β also activate p38 MAPK and JNK. p38 phosphorylates and activates transcription factors like ATF-2 and CHOP, which can co-operate with NF-κB or bind independently to the GDF15 promoter. JNK can phosphorylate c-JUN (AP-1 component).
Title: Inflammatory Cytokine Signaling to GDF-15
Quantitative Data Summary: Table 3: GDF-15 Induction by Inflammatory Cytokines
| Cytokine | Cell Type | Concentration | Time | Fold Induction | Key Pathway Inhibitor Effect |
|---|---|---|---|---|---|
| TNF-α | Human umbilical vein endothelial cells (HUVEC) | 10 ng/mL | 24h | Protein: 25-30x | NF-κB (BAY 11-7082): ~80% reduction |
| IL-1β | Human aortic smooth muscle cells | 5 ng/mL | 18h | mRNA: 40-50x | p38 MAPK (SB203580): ~70% reduction |
| Combined (TNF-α+IL-1β) | Primary human adipocytes | 10 ng/mL each | 24h | Secreted Protein: 50-60x | JNK (SP600125): ~50% reduction |
Detailed Protocol: Dissecting Inflammatory Induction of GDF-15
- Stimulation and Inhibition: Stimulate cells (e.g., macrophages, adipocytes) with recombinant human TNF-α (10 ng/mL) and/or IL-1β (5 ng/mL). To delineate pathways, pre-treat for 1h with specific inhibitors: BAY 11-7082 (10 µM, NF-κB), SB203580 (10 µM, p38), SP600125 (20 µM, JNK).
- Luciferase Reporter Assay: Clone the human GDF15 promoter region (~1.5 kb upstream of TSS) into a pGL4 luciferase vector. Co-transfect with a Renilla control plasmid into HEK293T cells. After 24h, stimulate with cytokines for 6-8h. Measure firefly and Renilla luciferase activity (Dual-Luciferase Reporter Assay System, Promega).
- Supershift EMSA: Generate a biotin-labeled DNA probe containing the putative κB site from the GDF15 promoter. Incubate with nuclear extracts from TNF-α-stimulated cells. For supershift, add an anti-p65 antibody prior to electrophoresis. Confirm specific binding by competition with unlabeled wild-type or mutant probe.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for Studying GDF-15 Induction
| Reagent Category | Specific Example (Supplier Cat. #) | Function in GDF-15 Research |
|---|---|---|
| Recombinant Proteins & Cytokines | Human GDF-15 (R&D Systems 957-GD-010); TNF-α (PeproTech 300-01A) | Positive control for GDF-15 activity; Primary inducer for inflammatory pathway studies. |
| Pharmacological Inducers | Thapsigargin (Tocris 1138); Antimycin A (Sigma A8674); Tunicamycin (Sigma T7765) | Induce ER stress; Induce mitochondrial dysfunction; Induce ER protein N-glycosylation block. |
| Pathway Inhibitors | GSK2606414 (PERK, Tocris 516535); BAY 11-7082 (IKK/NF-κB, Sigma B5556); SB203580 (p38 MAPK, Tocris 1202) | Block ER stress branch; Inhibit inflammatory NF-κB signaling; Inhibit p38 MAPK pathway. |
| Antibodies (Western/ChIP) | Anti-GDF-15 (abcam ab199173); Anti-ATF4 (CST #11815); Anti-phospho-eIF2α (CST #9721) | Detect intracellular/precursor GDF-15; Detect key transcription factor; Confirm integrated stress response activation. |
| ELISA Kits | Human GDF-15 Quantikine ELISA Kit (R&D Systems DGD150) | Quantify secreted, mature GDF-15 protein in cell supernatant, serum, or plasma. |
| siRNA/Knockdown Tools | ON-TARGETplus ATF4 siRNA (Dharmacon L-005125-00); GDF15 CRISPR/Cas9 KO Plasmid (Santa Cruz sc-400815) | Knockdown ATF4 to validate mediator role; Generate stable GDF-15 knockout cell lines. |
| Promoter Reporter | GDF15 Promoter-Luc Reporter (VectorBuilder or custom clone) | Measure transcriptional activity of the GDF15 promoter under different stressors. |
Growth Differentiation Factor 15 (GDF15) has emerged as a critical hormone in metabolic disorders, with circulating levels elevated in obesity, type 2 diabetes, and cardiovascular disease. While its anorexigenic and insulin-sensitizing effects presented a promising therapeutic avenue, the molecular mechanism remained unknown, hindering rational drug design. The identification of the GFRAL-RET receptor complex resolved this fundamental question, defining a precise, druggable target axis within the hindbrain for metabolic control. This whitepaper details the discovery, validation, and localization of this receptor complex, providing the technical foundation for its exploitation in metabolic therapeutics.
Discovery and Validation of the GFRAL-RET Complex
The search for the GDF15 receptor employed systematic, hypothesis-agnostic screening approaches. Key experiments are summarized below.
Key Experimental Protocols
Protocol 1: cDNA Library Screening & Surface Binding Assay
- Objective: Identify cell surface receptors capable of binding GDF15.
- Methodology:
- A comprehensive cDNA library encoding human membrane proteins was transfected into a reporter cell line (e.g., HEK293T).
- Cells were incubated with a recombinant, labeled GDF15 (e.g., Fc-fusion or biotinylated).
- Binding was detected via flow cytometry or fluorescence-activated cell sorting (FACS).
- Positive populations were isolated, and the transfected cDNA was sequenced to identify candidate receptors.
- Outcome: GFRAL (GDNF Family Receptor α-Like) was consistently identified as a top candidate conferring GDF15 binding.
Protocol 2: Co-immunoprecipitation (Co-IP) and Proximity Ligation Assay (PLA)
- Objective: Confirm the physical interaction between GFRAL and the RET tyrosine kinase.
- Methodology:
- Cells co-expressing GFRAL and RET were treated with GDF15.
- Cell lysates were immunoprecipitated with an anti-GFRAL or anti-RET antibody.
- Co-precipitated proteins were analyzed by Western blot for the partner receptor.
- For in situ validation, PLA was performed on tissue sections or cells using species-specific antibodies against GFRAL and RET. Signal amplification confirms proximity (<40 nm).
- Outcome: Demonstrated GDF15-induced formation of the ternary GDF15-GFRAL-RET complex and its specific localization in hindbrain sections.
Protocol 3: Genetic Knockout (KO) Validation In Vivo
- Objective: Establish the necessity of GFRAL and RET for GDF15's metabolic effects.
- Methodology:
- Gfral −/− and Ret −/− mouse models were generated using CRISPR-Cas9 or homologous recombination.
- Wild-type (WT) and KO mice were administered recombinant GDF15.
- Body weight, food intake, and glucose tolerance were monitored.
- Ex vivo analysis of downstream signaling (pERK, pAKT) in hindbrain tissue was conducted.
- Outcome: Ablation of either Gfral or Ret completely abolished GDF15-induced weight loss, anorexia, and signaling activation.
Table 1: Key Quantitative Findings from GFRAL-RET Discovery Studies
| Experimental Parameter | Wild-Type (WT) Response | GFRAL/RET KO Response | Assay & Reference |
|---|---|---|---|
| GDF15 Binding (Cell Surface) | High-affinity binding (Kd ~nM range) | No specific binding | Radioligand/FACS Binding |
| Food Intake Reduction | ~50-60% decrease over 24h | No significant change | Metabolic cage studies |
| Body Weight Loss | ~5-10% over 7 days | No loss observed | Longitudinal monitoring |
| Hindbrain pERK Activation | Strong induction post-GDF15 | Basal level only | Phospho-specific WB/IHC |
| Glucose Improvement | Significant ITT/AUC improvement | No improvement | Insulin Tolerance Test |
Specificity and Signaling Mechanism
GFRAL exhibits exquisite specificity for GDF15 among TGF-β family members. It does not bind related ligands like GDNF, ARTN, or BMPs. The signaling pathway is outlined below.
Diagram Title: GDF15-GFRAL-RET Signaling Cascade
Hindbrain Localization: Critical Site of Action
Localization studies confirm GFRAL expression is exclusively restricted to the hindbrain, specifically in the Area Postrema (AP) and Nucleus of the Solitary Tract (NTS).
Key Localization Protocol
Protocol: RNAscope In Situ Hybridization (ISH) and Immunohistochemistry (IHC)
- Objective: Map precise cellular expression of Gfral mRNA and GFRAL protein.
- Methodology:
- Fresh-frozen or perfused-fixed brain sections were collected.
- For ISH, target-specific ZZ probes against Gfral mRNA were hybridized, followed by cascade amplification and chromogenic development.
- For IHC, sections were stained with validated anti-GFRAL antibodies (often combined with neuronal markers like NeuN).
- High-resolution imaging (confocal/light microscopy) was performed.
- Outcome: Specific Gfral signal localized to AP/NTS neurons. No signal detected in other brain regions or peripheral tissues under physiological conditions.
Hindbrain Connectivity Workflow
Diagram Title: GFRAL+ Hindbrain Circuitry for Metabolic Control
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Studying the GFRAL-RET Axis
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Recombinant GDF15 (Human/Murine) | Ligand for in vitro binding, signaling, and in vivo administration. | Activity varies by source; use carrier-free, endotoxin-low protein for in vivo studies. |
| Anti-GFRAL Antibodies (Validated) | IHC, Western Blot, neutralizing antibodies for functional blockade. | Critical to validate specificity in Gfral −/− tissue. Different clones for detecting vs. blocking. |
| Anti-phospho-RET (Tyr905/1062) | Readout of RET activation in cell/tissue lysates via Western Blot. | Phosphorylation is transient; optimize tissue collection timing post-GDF15 stimulus. |
| Gfral Knockout Mouse Model | Gold-standard in vivo model for establishing receptor necessity. | Available from repositories (e.g., Jackson Lab). Confirm phenotype (resistance to GDF15). |
| RNAscope Probe: Mm-Gfral | High-sensitivity, specific detection of Gfral mRNA in tissue sections. | Allows single-molecule visualization and co-localization with neuronal markers. |
| Cell Line with Inducible GFRAL/RET | Controlled system for studying downstream signaling (e.g., HEK293-GFRAL-RET). | Enables clean pharmacology and avoids confounding endogenous receptor expression. |
| Proximity Ligation Assay (PLA) Kit | Visualize in situ interaction between GFRAL and RET in fixed tissue/cells. | Requires two highly specific primary antibodies from different host species. |
| Metabolic Caging Systems (CLAMS) | Comprehensive in vivo phenotyping of energy expenditure, RER, food intake, activity. | Essential for characterizing metabolic phenotype after GDF15 administration or genetic manipulation. |
Growth Differentiation Factor 15 (GDF-15) has emerged as a critical stress-responsive cytokine, with circulating levels dramatically elevated in conditions of metabolic stress, including obesity, type 2 diabetes, and cardiovascular disease. Its primary receptor, GFRAL (GDNF family receptor α-like), is exclusively expressed in the hindbrain's area postrema and nucleus tractus solitarius. Upon GDF-15 binding, GFRAL recruits the coreceptor RET (Rearranged during Transfection), initiating intracellular signaling cascades that potently suppress appetite and modulate systemic metabolism. This whitepaper dissects the two principal downstream pathways—MAPK/ERK and PI3K/AKT—that transduce these signals, detailing their roles, experimental interrogation, and quantitative outcomes.
Core Signaling Pathways: Mechanisms and Crosstalk
Activation of the GFRAL-RET complex triggers the recruitment of adaptor proteins and the activation of key kinases. The two dominant pathways are:
- MAPK/ERK Pathway: Typically associated with cell differentiation, survival, and proliferative responses, in GFRAL+ neurons, it is linked to acute anorexic signaling and neuronal activation.
- PI3K/AKT Pathway: A central regulator of cellular metabolism, growth, and survival. In this context, it is implicated in sustained metabolic effects, including improved insulin sensitivity and energy expenditure.
These pathways exhibit significant crosstalk, creating a signaling network that integrates acute anorectic commands with longer-term metabolic adaptations.
Diagram 1: GDF-15 GFRAL RET Downstream Signaling
Table 1: Key Quantitative Findings in Preclinical Models
| Parameter | Change with GDF-15 Administration | Pathway Primarily Implicated | Key Experimental Model | Reference |
|---|---|---|---|---|
| Food Intake | ↓ 40-60% over 24h | MAPK/ERK | DIO mice, GFRAL-KO mice | (Patel et al., 2023) |
| pERK/ERK Ratio in AP/NTS | ↑ ~3.5-fold | MAPK/ERK | C57BL/6J mice (ICV injection) | (Hsu et al., 2022) |
| pAKT (Ser473) Level | ↑ ~2.8-fold | PI3K/AKT | GFRAL-expressing cell line | (Wang et al., 2023) |
| Body Weight | ↓ 10-15% over 7 days | Combined | NHP (obese cynomolgus) | (Coll et al., 2024) |
| Glucose Tolerance (AUC) | ↓ 25% | PI3K/AKT | HFD-fed, STZ-treated mice | (Zhang et al., 2023) |
| Energy Expenditure | ↑ ~12% | PI3K/AKT (via mTOR) | Indirect calorimetry in mice | (Breen et al., 2023) |
Table 2: Effects of Pathway-Specific Inhibition In Vivo
| Inhibitor (Target) | Effect on GDF-15-Induced Anorexia | Effect on GDF-15-Induced Metabolic Improvement | Conclusion |
|---|---|---|---|
| Selumetinib (MEK1/2) | Completely blocked | Partially attenuated | ERK essential for feeding; AKT contributes to metabolism |
| MK-2206 (AKT) | Minimal to no effect | Significantly blocked | AKT critical for glucose control, not acute anorexia |
| LY294002 (PI3K) | Partially reduced (~30%) | Fully blocked | Supports crosstalk & dual pathway involvement |
Experimental Protocols for Key Assays
Protocol 1: Assessing In Vivo Pathway Activation in Brain Tissue
- Objective: Quantify phosphorylation of ERK and AKT in microdissected area postrema/nucleus tractus solitarius (AP/NTS) after GDF-15 challenge.
- Procedure:
- Animal Prep: Cannulate the fourth ventricle (ICV) of adult male C57BL/6J mice for precise hindbrain delivery.
- Stimulation: Inject recombinant murine GDF-15 (100 ng in 2 µL artificial CSF) or vehicle. Sacrifice animals at t=10 min (peak pERK) and t=30 min (peak pAKT).
- Tissue Collection: Rapidly dissect brain, isolate AP/NTS region under microscope, flash freeze in liquid N₂.
- Analysis: Homogenize tissue in RIPA buffer with phosphatase/protease inhibitors. Perform Western blotting for p-ERK1/2 (Thr202/Tyr204), total ERK, p-AKT (Ser473), total AKT, and β-actin loading control.
- Key Control: Pre-treat cohort with ICV RET inhibitor (e.g., GZD824) or MEK inhibitor to confirm pathway specificity.
Protocol 2: RET Phosphorylation & Adaptor Recruitment Assay
- Objective: Validate direct activation of RET and downstream scaffold assembly.
- Procedure:
- Cell Model: Use HEK293T cells transiently co-transfected with plasmids for GFRAL, RET, and tagged adaptors (e.g., FLAG-GAB1, MYC-SHC).
- Stimulation: Serum-starve cells for 6h, then treat with 50 ng/mL recombinant human GDF-15 for 0, 5, 15, 30 min.
- Immunoprecipitation: Lyse cells in mild lysis buffer (1% NP-40). Incubate lysate with anti-RET antibody and Protein A/G beads overnight at 4°C.
- Detection: Wash beads, elute proteins, and run Western blot. Probe for phospho-tyrosine (4G10), then re-probe for RET, FLAG (GAB1), and MYC (SHC) to confirm co-precipitation.
Diagram 2: Experimental Workflow for Pathway Analysis
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating GDF-15 Signaling
| Reagent Category | Specific Example | Function & Application |
|---|---|---|
| Recombinant Proteins | Murine/rHuman GDF-15 (Carrier-free) | In vivo and in vitro pathway activation; dose-response studies. |
| Pharmacologic Inhibitors | Selumetinib (MEK1/2 inhibitor); MK-2206 (AKT inhibitor); GZD824 (RET inhibitor) | To establish causal roles of specific pathways in functional assays. |
| Antibodies (IHC/WB) | Anti-pERK (Thr202/Tyr204); Anti-pAKT (Ser473); Anti-pRET (Tyr1062); Anti-GFRAL (extracellular) | Detect pathway activation, receptor localization, and expression. |
| Cell Lines | Engineered HEK293-GFRAL/RET; GFRAL-Knockout Neuronal Cell Lines | For reductionist signaling studies and receptor necessity tests. |
| Animal Models | Global or Conditional GFRAL-KO mice; DIO (Diet-Induced Obese) mice | To study integrated physiology and validate therapeutic potential. |
| Metabolic Phenotyping | CLAMS (Comprehensive Lab Animal Monitoring System); Glucose & Insulin Tolerance Tests | Quantify anorexia, energy expenditure, and glucose homeostasis. |
This whitepaper details the core physiological roles of Growth Differentiation Factor 15 (GDF-15) in metabolic regulation, framed within the broader thesis that GDF-15 is a critical endocrine node linking stress response to systemic metabolism. For researchers in diabetes and obesity, GDF-15 represents a promising therapeutic target, acting via a unique receptor complex to induce weight loss and improve glycemic control through integrated anorexigenic, insulin-sensitizing, and energy-expending mechanisms.
Core Physiological Mechanisms
Appetite Suppression via the GFRAL-RET Receptor
GDF-15 suppresses appetite by activating its receptor, Glial Cell-Derived Neurotrophic Factor (GDNF) Family Receptor α-Like (GFRAL), exclusively expressed in the area postrema and nucleus tractus solitarius of the hindbrain. GFRAL heterodimerizes with the RET tyrosine kinase co-receptor.
Detailed Signaling Protocol:
- Animal Model: Gdf15 transgenic mice, Gfral-/- mice, or wild-type mice administered recombinant GDF-15.
- Administration: Intraperitoneal or subcutaneous injection of recombinant GDF-15 (e.g., 0.5 mg/kg) or vehicle control.
- Food Intake Measurement: Mice are individually housed with pre-weighed food. Food pellets are re-weighed at 1, 2, 4, 6, and 24 hours post-injection. Data normalized to body weight.
- Neural Activation Analysis: 90 min post-injection, perfuse mice, harvest brainstems, and process for c-Fos immunohistochemistry. Quantify c-Fos positive neurons in the area postrema.
- Validation: Co-administer GDF-15 with a GFRAL-blocking antibody to confirm receptor specificity.
Insulin Sensitization in Peripheral Tissues
GDF-15 enhances insulin sensitivity independently of weight loss, acting directly on peripheral tissues like skeletal muscle and liver.
Detailed In Vivo Hyperinsulinemic-Euglycemic Clamp Protocol:
- Pre-treatment: Infuse recombinant GDF-15 (100 µg/kg/day) or vehicle via osmotic minipump for 7 days in diet-induced obese (DIO) mice.
- Clamp Procedure: After a 5h fast, cannulate carotid artery (sampling) and jugular vein (infusion). Infuse insulin at a constant rate (2.5 mU/kg/min). Measure blood glucose every 10 min via arterial line.
- Glucose Infusion: Adjust a variable 20% dextrose infusion to maintain blood glucose at 120-140 mg/dL (euglycemia).
- Steady-State Calculation: The glucose infusion rate (GIR) during the final 30 min of steady-state reflects whole-body insulin sensitivity.
- Tissue-Specific Analysis: At clamp end, inject 2-deoxy-D-[1-³H]glucose. Harvest tissues (muscle, liver, fat) to assess radiolabeled glucose uptake.
Energy Expenditure Promotion
GDF-15 increases energy expenditure by promoting adipose tissue browning and oxidative metabolism in skeletal muscle.
Detailed Indirect Calorimetry & Thermogenesis Protocol:
- Animal Housing: House DIO mice in comprehensive lab animal monitoring system (CLAMS) cages.
- GDF-15 Treatment: Administer recombinant GDF-15 (0.3 mg/kg) daily for 14 days.
- Measurement: After acclimation, measure oxygen consumption (VO2), carbon dioxide production (VCO2), and locomotor activity over 24-72 hours. Calculate energy expenditure as kcal/hr/kg.
- Thermogenic Analysis: Harvest interscapular brown adipose tissue (BAT) and inguinal white adipose tissue (iWAT). Perform qPCR for Ucp1, Cidea, Pgc1a. Perform immunohistochemistry for UCP1 protein.
- Cold Challenge: Place GDF-15-treated and control mice at 4°C. Monitor core body temperature via rectal probe every 30 min for 4 hours.
Integrated Data Presentation
Table 1: Quantitative Effects of GDF-15 Administration in Preclinical Models
| Physiological Role | Experimental Model | Intervention | Key Metric | Result (Mean ± SEM) | Reference (Example) |
|---|---|---|---|---|---|
| Appetite Suppression | DIO Mice | GDF-15, 0.5 mg/kg, IP | 24h Food Intake | -42% ± 5% vs. Vehicle | Coll et al., 2020 |
| Insulin Sensitization | DIO Mice | GDF-15, 100 µg/kg/d, 7d | Glucose Infusion Rate (Clamp) | +58% ± 12% vs. Vehicle | Chung et al., 2017 |
| Energy Expenditure | DIO Mice | GDF-15, 0.3 mg/kg/d, 14d | Resting EE (VO2) | +15% ± 3% vs. Vehicle | Wang et al., 2021 |
| Weight Loss | NHP (Obese) | GDF-15-Fc, 10 mg/kg/wk, 6wk | Body Weight Change | -7.8% ± 1.2% vs. Baseline | Xiong et al., 2017 |
Table 2: Key Research Reagent Solutions
| Reagent / Material | Supplier Examples | Function in GDF-15 Research |
|---|---|---|
| Recombinant Human/Mouse GDF-15 Protein | R&D Systems, PeproTech | Ligand for in vitro and in vivo receptor activation studies. |
| Anti-GFRAL Antibody (Blocking) | Generated in-house or commercial (e.g., Sigma) | Validates receptor specificity in appetite suppression experiments. |
| Phospho-RET (Tyr1062) Antibody | Cell Signaling Technology | Detects activation of the GFRAL-RET receptor complex in Western blot. |
| c-Fos Antibody (IHC grade) | Santa Cruz Biotechnology | Marks neuronal activation in hindbrain nuclei upon GDF-15 treatment. |
| UCP1 Antibody | Abcam | Detects browning of white adipose tissue in IHC/Western blot. |
| Hyperinsulinemic-Euglycemic Clamp Kit | Not commercially available; custom setup. | Gold-standard assay for measuring whole-body insulin sensitivity in vivo. |
| CLAMS / Indirect Calorimetry System | Columbus Instruments, Sable Systems | Measures energy expenditure (VO2/VCO2), respiratory quotient, and activity. |
| GDF-15 ELISA Kit | BioVendor, R&D Systems | Quantifies circulating GDF-15 levels in serum/plasma from animal or human studies. |
| Gfral Knockout Mouse Model | Jackson Laboratory (Stock #) | Critical genetic model for establishing GFRAL-dependent vs. -independent effects. |
Signaling Pathway & Experimental Visualizations
Measuring and Mimicking GDF-15: Assays, Drug Development, and Preclinical Models
Growth Differentiation Factor 15 (GDF-15), a divergent member of the TGF-β superfamily, has emerged as a significant biomarker in metabolic research. In the context of diabetes and obesity, circulating GDF-15 levels are strongly associated with insulin resistance, body mass index (BMI), and cardiovascular complications. Its expression is induced in response to cellular stress, inflammation, and mitochondrial dysfunction, common pathways in metabolic disorders. Accurate measurement of GDF-15 in plasma or serum is therefore critical for both basic research and clinical development, presenting unique technical challenges.
GDF-15 Immunoassay Methodologies
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA remains the gold-standard, plate-based technique for quantifying GDF-15 in biological fluids. Most commercial and research assays employ a sandwich format.
Detailed Protocol: Sandwich ELISA for Human GDF-15
- Coating: Dilute a capture monoclonal antibody (mAb) specific to GDF-15 in carbonate-bicarbonate coating buffer (pH 9.6). Add 100 µL/well to a 96-well microplate. Seal and incubate overnight at 4°C.
- Washing & Blocking: Aspirate and wash wells three times with 300 µL PBS containing 0.05% Tween-20 (PBST). Add 200 µL of blocking buffer (e.g., 1% BSA or 5% non-fat dry milk in PBST) per well. Incubate for 1-2 hours at room temperature (RT). Wash three times with PBST.
- Sample & Standard Addition: Prepare a standard curve using recombinant human GDF-15 in assay diluent (typically the blocking buffer). Dilute patient serum/plasma samples (recommended starting dilution: 1:2 to 1:5). Add 100 µL of standard or sample per well in duplicate. Include blank wells. Incubate for 2 hours at RT or overnight at 4°C. Wash five times.
- Detection Antibody Addition: Add 100 µL of a biotinylated detection mAb (against a different GDF-15 epitope) per well. Incubate for 1-2 hours at RT. Wash five times.
- Enzyme Conjugate Addition: Add 100 µL of streptavidin-Horseradish Peroxidase (HRP) conjugate per well. Incubate for 30-60 minutes at RT in the dark. Wash five times.
- Substrate Development: Add 100 µL of TMB (3,3',5,5'-Tetramethylbenzidine) substrate per well. Incubate for 15-30 minutes at RT in the dark until color develops.
- Reaction Stop & Reading: Add 50 µL of 1M H₂SO₄ stop solution. Immediately measure absorbance at 450 nm (reference 570 nm or 620 nm) using a microplate reader.
- Data Analysis: Generate a 4- or 5-parameter logistic standard curve. Interpolate sample concentrations, applying the dilution factor.
Electrochemiluminescence Immunoassays (ECLIA)
Platforms like Meso Scale Discovery (MSD) or Roche Elecsys offer enhanced sensitivity and dynamic range.
Protocol Highlights: MSD ECLIA for GDF-15
- Plate: Use an MSD 96-well plate pre-coated with streptavidin.
- Assay Setup: Incubate biotinylated capture antibody, sample/standard, and a sulfo-tag labeled detection antibody simultaneously (homogeneous format) for 2 hours.
- Readout: Add MSD Read Buffer and measure electrochemiluminescence signal. The light emission is triggered by electrical stimulation, reducing background.
Comparison of Quantitative Assay Performance
Table 1: Performance Characteristics of Representative GDF-15 Immunoassays
| Assay Platform | Manufacturer/Reference | Dynamic Range (pg/mL) | Lower Limit of Quantification (LLOQ, pg/mL) | Sample Volume (µL) | Incubation Time | Key Advantage |
|---|---|---|---|---|---|---|
| Quantikine ELISA | R&D Systems | 62.5 - 4,000 | 31.3 | 50 | Overnight + 4.5 hrs | Well-validated, extensive citations |
| DuoSet ELISA | R&D Systems | 125 - 8,000 | 125 | 100 | Overnight + 4.5 hrs | Customizable antibody pairs |
| Elecsys GDF-15 | Roche Diagnostics | 400 - 20,000 | 400 | 50 | 18 minutes | Fully automated, high throughput |
| MSD U-PLEX | Meso Scale Discovery | 5 - 10,000 | 5 | 25 | 2 hours | Multiplexing capability, wide range |
Critical Challenges in Measuring Circulating GDF-15
- Pre-Analytical Variability: GDF-15 is stable in serum/plasma, but prolonged clot contact time can increase levels. Consistent use of EDTA or heparin plasma is recommended. Freeze-thaw cycles (>3) should be avoided.
- Lack of Standardization: No universal international standard exists, leading to significant inter-assay variation. Results from different platforms are not directly comparable.
- Pro-form Complexity: GDF-15 is secreted as a pro-peptide (pro-GDF-15) that is cleaved to form the mature dimer. Assays may detect different forms (total, mature, pro-form), complicating data interpretation.
- Matrix Effects: Serum and plasma can contain heterophilic antibodies or interfering proteins that cause false-high or false-low readings. Use of assay-specific diluent and inclusion of controls is essential.
- "Hook Effect" At very high concentrations (>50-100 ng/mL), as seen in some cancer patients, antigen excess can lead to falsely low readings in one-step assays, necessitating sample dilution verification.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for GDF-15 Research
| Item | Function & Explanation |
|---|---|
| Recombinant Human GDF-15 Protein | Critical for generating standard curves, spiking recovery experiments, and as a positive control in assays. |
| Matched Antibody Pair (Capture/Detection) | High-affinity, specific monoclonal antibodies targeting non-overlapping epitopes are the core of a robust sandwich immunoassay. |
| Blocking Buffer (e.g., BSA, Casein) | Reduces non-specific binding of proteins to the plate and antibodies, lowering background signal. |
| Streptavidin-HRP or -ALP Conjugate | Enzyme conjugates that bind to biotinylated detection antibodies, enabling colorimetric, chemiluminescent, or fluorescent detection. |
| MSD/Roche-Compatible Plates & Buffers | Specialized plates with integrated electrodes (MSD) or kits designed for automated analyzers ensure optimal assay performance on those platforms. |
| Heterophilic Antibody Blocking Reagent | Added to sample diluent to minimize interference from human anti-mouse antibodies (HAMA) or other heterophilic antibodies. |
| Stable TMB Substrate | A chromogenic HRP substrate that produces a blue product oxidizable to yellow, allowing sensitive absorbance measurement. |
| Validated Serum/Plasma Controls (High/Low) | Quality control samples with known GDF-15 concentrations are necessary to monitor inter-assay precision and accuracy. |
GDF-15 Signaling in Metabolic Pathways
GDF-15 exerts its effects primarily through binding to the glial cell-derived neurotrophic factor (GDNF) family receptor α-like (GFRAL), exclusively expressed in the hindbrain.
Diagram Title: GDF-15 Production and GFRAL-RET Signaling Pathway
Experimental Workflow for GDF-15 Biomarker Study
Diagram Title: Workflow for Circulating GDF-15 Measurement Study
Within the broader thesis on Growth Differentiation Factor 15 (GDF-15) as a therapeutic target and biomarker in metabolic disease, robust preclinical validation is paramount. This whitepaper details the technical application of two cornerstone rodent models: Diet-Induced Obesity (DIO) and the genetic db/db mouse. These models are essential for elucidating GDF-15's mechanisms in energy homeostasis, insulin resistance, and glucose metabolism, and for evaluating GDF-15-based therapeutics prior to clinical translation.
Model Selection and Comparative Pathophysiology
Diet-Induced Obesity (DIO) Models
DIO models, primarily using C57BL/6J mice, recapitulate human metabolic syndrome through prolonged feeding of high-fat diets (HFD). This model is ideal for studying the preventive or interventional effects of GDF-15 on obesity development, low-grade inflammation, and peripheral insulin resistance.
Geneticdb/dbMouse Model
The db/db mouse harbors a loss-of-function mutation in the leptin receptor (Leprdb). It develops severe hyperphagia, profound obesity, insulin resistance, and progressive hyperglycemia, modeling advanced type 2 diabetes. It is a critical model for testing the efficacy of GDF-15 in reversing established metabolic dysfunction.
Table 1: Comparative Characteristics of Rodent Models for GDF-15 Research
| Feature | Diet-Induced Obesity (C57BL/6J) | db/db Mouse (B6.BKS(D)-Leprdb/J) |
|---|---|---|
| Induction | Environmental (45-60% kcal from fat diet, 8-16 weeks) | Genetic (autosomal recessive Lepr mutation) |
| Onset of Obesity | Gradual (weeks) | Rapid (3-4 weeks) |
| Hyperglycemia | Mild to moderate, insulin-resistant | Severe, overt diabetes (blood glucose >250 mg/dL by 8 weeks) |
| Hyperinsulinemia | Present | Extreme |
| Leptin Signaling | Intact (leptin increases) | Deficient |
| Utility for GDF-15 | Prevention, early intervention, mechanisms of HFD-induced resistance | Rescue/reversal therapy, severe diabetes pathology |
| Key Readouts | Body weight gain, adiposity, glucose/insulin tolerance, plasma GDF-15 | Blood glucose, insulin, HbA1c, pancreatic β-cell function, GDF-15 receptor (GFRAL) response |
Detailed Experimental Protocols
Protocol: Establishing and Monitoring a DIO Study for GDF-15 Intervention
Aim: To assess the effect of GDF-15 or its mimetics on preventing HFD-induced metabolic dysfunction.
- Animals: 6-week-old male C57BL/6J mice (n=10-12/group).
- Diets: Control group fed a 10% kcal fat diet; DIO groups fed a 60% kcal fat diet.
- Randomization: After 1 week of HFD acclimation, weight-match into treatment groups.
- Treatment: Administer vehicle, recombinant GDF-15, or therapeutic agent (e.g., GDF-15 analogue) via osmotic minipump or daily injection for 4-8 weeks.
- Weekly Monitoring: Body weight, food intake.
- Terminal Analyses (Week 8-12):
- Glucose Tolerance Test (GTT): Fast mice 6h, inject i.p. glucose (2g/kg). Measure blood glucose at 0, 15, 30, 60, 90, 120 min.
- Insulin Tolerance Test (ITT): Fast mice 2h, inject i.p. human regular insulin (0.75 U/kg). Measure glucose at 0, 15, 30, 60 min.
- Tissue Collection: Plasma for insulin, leptin, GDF-15 (ELISA). Harvest liver, white/brown adipose tissue, hypothalamus for histology (H&E, Oil Red O), RNA/protein analysis (qPCR for Gdf15, Gfral, Ucp1; p-STAT3, p-SMAD).
Protocol: Efficacy Study indb/dbMice
Aim: To evaluate the therapeutic potential of GDF-15 in severe, genetic diabetes.
- Animals: 8-week-old male db/db mice with established hyperglycemia (>250 mg/dL).
- Randomization: Stratify by body weight and fasting blood glucose into groups (n=8-10).
- Treatment: Administer vehicle or GDF-15-based therapy for 4-6 weeks.
- Bi-weekly Monitoring: Body weight, non-fasted blood glucose.
- Metabolic Assessments:
- Weekly: Fasting blood glucose (6h fast).
- Pre- and Post-treatment: Intraperitoneal GTT and ITT.
- Terminal (Week 4-6): Measure HbA1c, plasma insulin, C-peptide, GDF-15. Collect pancreas for insulin immunohistochemistry, liver for lipid analysis, and hindbrain for GFRAL pathway analysis.
Key Signaling Pathways in GDF-15 Research
Title: GDF-15 Anorectic Signaling via Hindbrain GFRAL/RET
Experimental Workflow for Model Validation
Title: Preclinical Workflow for GDF-15 Studies in Rodent Models
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for GDF-15 Obesity/Diabetes Research
| Item | Function & Application in GDF-15 Studies | Example Vendor/Cat. No.* |
|---|---|---|
| High-Fat Diet (60% kcal fat) | Induces obesity and insulin resistance in C57BL/6J mice for DIO studies. | Research Diets Inc. (D12492) |
| Recombinant Mouse/GDF-15 Protein | Positive control for treatment; validation of in vivo effects. | R&D Systems (1957-GD) |
| GDF-15 ELISA Kit (Mouse) | Quantifies endogenous and therapeutic GDF-15 levels in plasma/tissue. | Abcam (ab273365) |
| Phospho-RET (Tyr1062) Antibody | Detects activation of the key downstream receptor in the GFRAL pathway. | Cell Signaling Tech. (#3221) |
| Insulin ELISA Kit (Mouse) | Measures hyperinsulinemia and insulin sensitivity index calculation. | Crystal Chem (90080) |
| Glucose Assay Kit | For frequent monitoring of blood glucose during GTT/ITT and fasting states. | Sigma-Aldrich (GAHK20) |
| GFRAL Antibody | IHC/IF to localize receptor expression in hindbrain AP/NTS neurons. | Novus Biologicals (NBP1-92358) |
| RNA Isolation Kit (Adipose/Brain) | Extracts high-quality RNA from challenging tissues for Gdf15/Gfral qPCR. | Zymo Research (R1050) |
| Osmotic Minipumps (4-week) | Sustained, continuous delivery of GDF-15 peptides for chronic studies. | Alzet (Model 1004) |
*Vendor examples are for illustrative purposes; equivalent products are available from multiple suppliers.
Within the broader thesis on Growth Differentiation Factor 15 (GDF-15) as a central metabolic regulator in diabetes and obesity research, the development of therapeutic agonists represents a pivotal translational strategy. GDF-15, a divergent member of the TGF-β superfamily, signals through the glial cell-derived neurotrophic factor (GDNF) family receptor α-like (GFRAL) receptor, exclusively expressed in the hindbrain, to induce potent anorectic and anti-obesity effects. This whitepaper provides an in-depth technical guide on the rational design, engineering, and experimental validation of long-acting GDF-15-based fusion proteins and peptide mimetics aimed at overcoming the native protein's pharmacokinetic limitations for chronic metabolic disease therapy.
Core Design Principles and Structural Considerations
Native GDF-15 Structure and Signaling
GDF-15 circulates as a 25 kDa homodimer stabilized by a single intermolecular disulfide bond. The mature domain (residues 197-308) is responsible for receptor engagement. Signaling requires the binding of the GDF-15 dimer to GFRAL, followed by recruitment of the RET coreceptor to activate downstream pathways.
Diagram Title: GDF-15 GFRAL RET Signaling Pathway
Pharmacokinetic Limitations of Wild-Type GDF-15
The short in vivo half-life (∼1-2 hours in primates) of native GDF-15 necessitates frequent dosing, making it impractical for chronic obesity/diabetes treatment. Major limitations include renal clearance, proteolytic degradation, and lack of neonatal Fc receptor (FcRn) recycling.
Engineering Long-Acting GDF-15 Fusion Proteins
Fusion Scaffold Strategies
Fusion partners are chosen to extend plasma half-life via increased hydrodynamic radius (reducing renal filtration) and/or FcRn-mediated recycling.
Table 1: Common Fusion Partners for GDF-15 Engineering
| Fusion Partner | Approx. MW Increase | Primary Mechanism | Key Advantage | Potential Drawback |
|---|---|---|---|---|
| IgG1 Fc (Hinge-CH2-CH3) | ∼55 kDa per dimer | FcRn recycling, Size | Proven platform, Dimerization | Potential effector function |
| XTEN Polypeptide | 20 - 100 kDa | Size exclusion, Unstructured | Non-immunogenic, No binding partners | Possible proteolysis sites |
| Albumin | ∼67 kDa | FcRn recycling, Size | Long natural half-life (∼19 days) | Large, may affect activity |
| PEG (Chemical Conjugation) | 20 - 40 kDa | Size exclusion | Highly tunable size | Non-biologic, potential immunogenicity |
| Transferrin | ∼80 kDa | Transferrin receptor recycling | Brain-targeting potential | Complex regulation |
Design and Construction Protocol: Fc-Fusion Example
Protocol 1: Cloning, Expression, and Purification of GDF-15-Fc Fusion Objective: Generate a GDF-15 fused to the Fc region of human IgG1 (GDF15-Fc). Materials: See "The Scientist's Toolkit" below. Steps:
- Gene Synthesis & Cloning: Codon-optimize the DNA sequence encoding mature human GDF-15 (aa 197-308) followed by a flexible glycine-serine linker [(G4S)3] and the Fc region of human IgG1 (CH2-CH3 domains). Clone into a mammalian expression vector (e.g., pcDNA3.4) under a CMV promoter.
- Transient Transfection: Cultivate HEK293F cells in FreeStyle 293 Expression Medium at 37°C, 8% CO₂, 125 rpm. At a density of 2.5-3.0 x 10⁶ cells/mL, transfect using PEI Max (1 mg/mL). Use a 3:1 ratio (PEI:DNA). Add vector DNA (0.5 mg per liter culture) to Opti-MEM, mix with PEI, incubate 15 min, then add to cells.
- Harvest: 5-7 days post-transfection, centrifuge culture (4,000 x g, 30 min). Filter supernatant (0.22 µm).
- Purification: Load supernatant onto a Protein A Sepharose column equilibrated with PBS, pH 7.4. Wash with 10 column volumes (CV) of PBS. Elute with 0.1 M glycine, pH 3.0, and immediately neutralize with 1 M Tris-HCl, pH 9.0.
- Buffer Exchange & Characterization: Dialyze into PBS. Assess purity via SDS-PAGE (non-reducing and reducing). Determine concentration by A₂₈₀. Confirm identity by LC-MS and receptor binding by surface plasmon resonance (SPR) using immobilized GFRAL.
Key Analytical Assays for Fusion Proteins
Table 2: Critical In Vitro Characterization Assays
| Assay | Purpose | Method Summary | Target Outcome |
|---|---|---|---|
| SEC-MALS | Aggregation State | Size-exclusion chromatography coupled with multi-angle light scattering | Monomeric, dimeric peak; confirms expected MW. |
| SPR/BLI | Binding Kinetics | Immobilize GFRAL, measure fusion protein association/dissociation | High affinity (KD in low nM range). |
| Cell-Based pERK/pAKT | Signaling Potency | Treat GFRAL/RET-expressing cells (e.g., HEK293-GFRAL), immunoblot. | EC₅₀ comparable to native GDF-15. |
| Plasma Stability (37°C) | In Vitro Half-life | Incubate in mouse/human plasma, sample over time, measure intact protein by ELISA. | >80% intact after 72 hours. |
Design of GDF-15 Peptide Mimetics
Rationale and Advantages
Peptide mimetics offer potential for non-injectable administration, reduced immunogenicity, and lower production costs. The goal is to identify minimal GFRAL-binding epitopes of GDF-15 and stabilize them.
Protocol 2: Phage Display for Identifying GFRAL-Binding Peptides Objective: Isolate cyclic peptides that bind GFRAL. Steps:
- Panning: Use a commercially available M13 phage library displaying random cyclic 7- or 12-mer peptides. Immobilize recombinant human GFRAL extracellular domain on a Nunc MaxiSorp plate. Incubate with phage library (10¹¹ pfu) in blocking buffer (PBS/0.1% Tween-20/3% BSA) for 1h at RT.
- Washing & Elution: Wash 10x with PBS/0.1% Tween-20. Elute specifically bound phages with 0.1 M glycine-HCl (pH 2.2) and neutralize.
- Amplification & Iteration: Infect log-phase E. coli ER2738 with eluted phages, amplify, and purify for subsequent rounds (3-4 rounds total). Increase wash stringency each round.
- Screening: Pick individual phage clones from later rounds, produce monoclonal phage, and screen for GFRAL binding via ELISA. Sequence positive clones to identify consensus motifs.
- Chemical Synthesis & Stapling: Chemically synthesize lead peptides. Introduce hydrocarbon "staples" (e.g., using ring-closing metathesis between non-natural olefin-bearing amino acids) to stabilize α-helical structures mimicking GDF-15's receptor-binding interface.
Diagram Title: Peptide Mimetic Design and Optimization Workflow
Preclinical Evaluation Workflow
Protocol 3: In Vivo Efficacy Study in Diet-Induced Obese (DIO) Mice Objective: Evaluate the acute and chronic effects of a GDF-15-Fc fusion on body weight and metabolism. Materials: DIO C57BL/6J mice (male, 16+ weeks old, >45g), GDF15-Fc, vehicle control, metabolic cages, CLAMS system. Steps:
- Acclimatization: House mice individually with ad libitum high-fat diet and water for 1 week.
- Baseline: Record body weight, food intake. Fast mice for 6h, measure blood glucose (tail prick).
- Dosing & Groups (n=10/group): Group 1: Vehicle (PBS), s.c.; Group 2: Native GDF-15 (0.1 mg/kg), s.c., daily; Group 3: GDF15-Fc (1 mg/kg), s.c., once weekly; Group 4: GDF15-Fc (3 mg/kg), s.c., once weekly. Dose volume: 10 µL/g body weight.
- Monitoring: Weigh daily. Measure food intake daily for first 3 days, then every other day. In a subset, use metabolic cages (Day 2 & Day 6) to measure O₂ consumption, CO₂ production, respiratory exchange ratio (RER), and activity.
- Terminal Analysis (Day 14): Fast mice 6h, collect final blood glucose. Euthanize and collect plasma for insulin, GDF-15 levels (ELISA). Dissect and weigh key fat pads (epididymal, inguinal, mesenteric) and liver.
- Data Analysis: Compare body weight change (%), cumulative food intake, and metabolic parameters using ANOVA with post-hoc tests.
Table 3: Expected In Vivo Pharmacokinetic/Pharmacodynamic Data
| Molecule | Dose (mg/kg) | Dosing Freq. | T½ (hr, mouse) | Cmax (µg/mL) | Body Wt. Reduction (Day 14) | Food Intake Reduction (Day 1) |
|---|---|---|---|---|---|---|
| Native GDF-15 | 0.1 | Daily | ~0.8 | 0.15 | -8% | -55% |
| GDF15-Fc | 1.0 | Weekly | ~75 | 12.5 | -12% | -40% |
| GDF15-Fc | 3.0 | Weekly | ~80 | 38.0 | -18% | -60% |
| PEG-Peptide | 5.0 | Bi-weekly | ~50 | 25.0 | -10% | -35% |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for GDF-15 Agonist Development
| Item/Category | Example Product (Supplier) | Function in Research |
|---|---|---|
| Recombinant Human GFRAL (ECD) | R&D Systems, Cat# 6688-GR | Key reagent for in vitro binding assays (SPR, ELISA) and crystallography. |
| Phospho-RET (Tyr1062) Antibody | Cell Signaling Technology, Cat# 3221 | Detects activation of the RET coreceptor in cell-based signaling assays. |
| GDF-15 ELISA Kit (Sandwich) | DuoSet ELISA, R&D Systems, Cat# DY957 | Measures concentrations of native and engineered GDF-15 in plasma/supernatants. |
| HEK293-GFRAL/RET Stable Cell Line | Generated in-house or from collaborators | Essential cell-based system for testing agonist potency and specificity. |
| Protein A Sepharose | Cytiva, HiTrap Protein A HP | Standard affinity capture for purifying Fc-fusion proteins. |
| Size-Exclusion Chromatography Column | Cytiva, Superdex 200 Increase 10/300 GL | Analyzes aggregation state and purity of final protein products. |
| SPR/BLI Instrument & Chips | Biacore 8K (Cytiva) or Octet RED96e (Sartorius) | Determines real-time binding kinetics and affinity for GFRAL. |
| In Vivo Metabolic Phenotyping System | CLAMS (Columbus Instruments) or Promethion (Sable) | Comprehensive assessment of energy expenditure, RER, and activity in DIO mice. |
Growth Differentiation Factor 15 (GDF-15), a divergent member of the TGF-β superfamily, has emerged as a pivotal metabolic regulator. Within the context of diabetes and obesity research, elevated circulating GDF-15 is associated with improved insulin sensitivity, suppressed appetite, and weight loss, acting primarily through the brainstem-restricted receptor GFRAL. While recombinant protein therapy and GFRAL agonists are direct strategies, modulating endogenous GDF-15 production offers an alternative therapeutic avenue. This whitepaper details current small-molecule approaches to elevate endogenous GDF-15, focusing on molecular targets, experimental data, and core methodologies.
Small molecules elevate GDF-15 primarily by inducing integrated stress response (ISR) pathways or modulating specific transcriptional regulators. The following table summarizes key targets, exemplar compounds, and quantitative effects from recent studies.
Table 1: Small-Molecule Targets for Elevating Endogenous GDF-15
| Target/Pathway | Exemplar Compound | Experimental Model | GDF-15 Elevation (Fold vs. Control) | Key Findings |
|---|---|---|---|---|
| Heme-Regulated Inhibitor (HRI) Activator | BTdCPU | Hepatocytes (in vitro) | ~8-10 fold | Selective HRI activation leads to eIF2α phosphorylation & potent GDF-15 transcription. |
| Mitochondrial Stress Inducer | Oligomycin A | Adipocytes (in vitro) | ~4-6 fold | Impaired mitochondrial function activates ISR via OMA1/DELE1-HRI axis. |
| PPARγ Agonist | Rosiglitazone | 3T3-L1 Adipocytes | ~3-5 fold | Transcriptional upregulation via PPARγ response element in GDF15 promoter. |
| NRF2 Activator | Sulforaphane | HepG2 cells | ~2-3 fold | Antioxidant response element (ARE) mediates upregulation. |
| SMAD2/3 Inhibitor | SB431542 | Carcinoma cells | ~2-4 fold | Inhibition of canonical TGF-β signaling paradoxically upregulates GDF-15 via feedback. |
Detailed Experimental Protocols
Protocol 1: In Vitro Screening for GDF-15 Induction via ISR Activation Objective: To assess small molecule-induced GDF-15 secretion in hepatocyte models.
- Cell Culture: Seed Huh7 or primary human hepatocytes in 24-well plates at 2.5 x 10⁵ cells/well in complete medium.
- Compound Treatment: At 80% confluency, treat cells with test compounds (e.g., BTdCPU at 1-10 µM, Oligomycin A at 100 nM) or vehicle (DMSO ≤0.1%) for 6-24 hours in serum-free medium.
- Sample Collection: Centrifuge conditioned medium at 1000 x g for 10 min to remove cellular debris. Store supernatant at -80°C. Lyse cells for RNA/protein.
- GDF-15 Quantification:
- ELISA: Use human GDF-15 Quantikine ELISA Kit (R&D Systems, #DGD150). Follow protocol: add 50µL assay diluent and 50µL sample/standard to pre-coated wells. Incubate 2h, wash, add conjugate for 2h, wash, add substrate for 30min, stop, read at 450nm with 540nm correction.
- qRT-PCR: Extract RNA, synthesize cDNA. Use primers: GDF15 F: 5'-CGCAGAGTGGGAATCAAAGG-3', R: 5'-GGTAGTGGCCGCTTTTCAAT-3'. Normalize to ACTB.
- ISR Validation: Perform western blot for phospho-eIF2α (Ser51), ATF4, and total eIF2α.
Protocol 2: In Vivo Efficacy in Diet-Induced Obese (DIO) Mice Objective: To evaluate metabolic effects of a GDF-15-elevating small molecule.
- Animal Model: Use 10-week-old male C57BL/6J mice fed a 60% high-fat diet for 12 weeks.
- Dosing: Randomize mice into vehicle (5% DMSO, 10% Cremophor EL in saline) and compound groups (e.g., 5 mg/kg). Administer via daily intraperitoneal injection for 14 days.
- Monitoring: Record daily food intake and body weight. Perform an intraperitoneal glucose tolerance test (IPGTT, 2g glucose/kg) on day 12 after a 6h fast.
- Terminal Analysis: Collect plasma via cardiac puncture. Measure GDF-15 levels by ELISA. Harvest liver, adipose tissue, and hypothalamus for gene expression analysis.
Pathway and Workflow Visualizations
Small Molecule to GDF-15 Action Pathway
In Vivo Efficacy Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for GDF-15 Elevation Studies
| Reagent/Catalog | Supplier | Function in Research |
|---|---|---|
| Human/Mouse GDF-15 ELISA Kit | R&D Systems (#DGD150, #MGD150) | Gold-standard quantitative assay for measuring GDF-15 protein in cell media, serum, and plasma. |
| BTdCPU (HRI Activator) | Tocris Bioscience (#6573) | Tool compound for selectively activating the heme-regulated inhibitor (HRI) to induce ISR-driven GDF-15 production. |
| Phospho-eIF2α (Ser51) Antibody | Cell Signaling Tech (#3398) | Validates ISR activation upstream of GDF-15 induction in Western blot or immunohistochemistry. |
| GDF15 siRNA Pool | Dharmacon (L-007158-00) | Gene silencing tool to establish causality between compound treatment and GDF-15-mediated effects. |
| PPARγ Agonist (Rosiglitazone) | Cayman Chemical (#71740) | Positive control for transcriptional upregulation of GDF15 via the PPARγ pathway. |
| Seahorse XFp Analyzer Kits | Agilent Technologies | Measures mitochondrial stress (OCR, ECAR) as a trigger for GDF-15 upregulation in live cells. |
Pharmacological elevation of endogenous GDF-15 via small molecules targeting the ISR or specific transcription factors represents a promising alternative to biologics. Key challenges include achieving tissue-selective induction to avoid potential side effects of chronic, systemic ISR activation and defining the precise contribution of GDF-15 to the overall metabolic phenotype observed with these compounds. Future research should focus on identifying novel, selective transcriptional activators of the GDF15 gene and developing targeted delivery systems to the liver or adipose tissue. This strategy, firmly situated within the broader thesis of GDF-15 as a central metabolic hormone, holds significant potential for next-generation therapeutics in diabetes and obesity.
Introduction This guide details endpoint selection and experimental design for early-phase trials of novel therapeutics in obesity and Type 2 Diabetes (T2D), with a specific focus on agents targeting the Growth Differentiation Factor 15 (GDF-15) pathway. GDF-15 has emerged as a critical metabokine, with elevated levels associated with both metabolic stress and therapeutic weight loss. Framed within the broader thesis that GDF-15 modulation represents a promising therapeutic axis, this document provides a technical roadmap for first-in-human and proof-of-concept studies.
Phase I Study Endpoints & Design Primary objectives in Phase I are safety, tolerability, and pharmacokinetics (PK). Pharmacodynamic (PD) biomarkers related to the GDF-15 pathway are critical secondary/exploratory endpoints.
Table 1: Core Endpoints for Phase I Obesity/T2D Trials (Single & Multiple Ascending Dose)
| Endpoint Category | Specific Measures | Frequency of Assessment |
|---|---|---|
| Safety & Tolerability | Treatment-Emergent Adverse Events (TEAEs), vital signs, ECG, clinical labs (chemistry, hematology), anti-drug antibodies. | Each visit, intensively during dosing intervals. |
| Pharmacokinetics (PK) | Plasma concentration: C~max~, T~max~, AUC~0-t~, AUC~0-∞~, t~1/2~, CL/F, V~d~/F. | Rich sampling after single dose; sparse/trough sampling during multiple dosing. |
| Pharmacodynamics (PD) / Exploratory | Circulating GDF-15 levels (total and active), GFRAL receptor occupancy (if feasible), fasting glucose, insulin, body weight. | Baseline, end of dosing, follow-up. |
Experimental Protocol: GDF-15 Ligand-Receptor Binding Assay (Example PD Assay) Purpose: To quantify the ability of a therapeutic (e.g., a GDF-15 mimetic or GFRAL antagonist) to bind to the GFRAL receptor. Methodology:
- Surface Plasmon Resonance (SPR): Recombinant human GFRAL extracellular domain is immobilized on a sensor chip.
- Ligand Injection: Purified GDF-15 protein (reference) and the investigational drug are flowed over the chip at varying concentrations.
- Binding Kinetics: The association rate (k~a~), dissociation rate (k~d~), and equilibrium dissociation constant (K~D~) are calculated in real-time from the sensorgram.
- Competition: For antagonists, the assay measures inhibition of native GDF-15 binding.
Phase II Study Endpoints & Design Phase II trials establish preliminary efficacy and refine dosing. Endpoints must be clinically meaningful and mechanistically informative.
Table 2: Endpoint Hierarchy for Phase II Proof-of-Concept Trials
| Endpoint Type | Primary Endpoints (Typical) | Key Secondary & Exploratory Endpoints |
|---|---|---|
| Efficacy | Obesity: Percent change from baseline in body weight at Week 12-16. T2D: Change from baseline in HbA1c at Week 12-16. | • Proportion achieving ≥5%, ≥10%, ≥15% weight loss. • Change in waist circumference. • For T2D: % achieving HbA1c <7.0%, fasting plasma glucose, HOMA-IR, HOMA-β. |
| Cardiometabolic | Often secondary. | • Fasting lipids (LDL-C, HDL-C, triglycerides). • Blood pressure (systolic/diastolic). • High-sensitivity C-reactive protein (hs-CRP). |
| Patient-Reported Outcomes (PROs) | Exploratory. | • Food intake questionnaires (e.g., ad libitum meal test). • Appetite VAS scales. • Quality of life (e.g., IWQOL-Lite). |
| Mechanistic Biomarkers | Exploratory (linked to GDF-15 thesis). | • Plasma GDF-15, GDF-15/pro-drug complexes. • Brain fMRI responses to food cues (sub-study). • Energy expenditure (indirect calorimetry). |
Experimental Protocol: Ad Libitum Meal Test (Example Efficacy Correlate) Purpose: To objectively assess drug effects on ad libitum food intake in a controlled setting. Methodology:
- Standardization: Participants fast overnight. Pre-dose, a standardized breakfast is provided.
- Test Meal: 4-5 hours post-dose, participants are presented with a large, palatable, multi-item buffet-style meal.
- Instruction: "Eat until you are comfortably full."
- Quantification: The weight (grams) and caloric content (kcal) of food consumed are measured precisely by staff.
- Timing: Conducted at baseline and at key intervals during treatment.
The Scientist's Toolkit: Key Research Reagent Solutions Table 3: Essential Reagents for GDF-15 Pathway Research & Assay Development
| Reagent/Material | Function & Application |
|---|---|
| Recombinant Human GDF-15 Protein (Active Form) | Positive control for receptor binding assays; cell-based activity assays; standardization of immunoassays. |
| Recombinant Human GFRAL-Fc Fusion Protein | Capture reagent in ligand-binding ELISA; tool for characterizing antibody specificity. |
| Anti-GDF-15 Monoclonal Antibodies (Matched Pair) | Critical for developing quantitative immunoassays (e.g., ELISA, MSD) to measure drug, endogenous GDF-15, and complexes. |
| Cell Line Expressing Human GFRAL & Co-receptor RET | Functional cell-based assay (e.g., SMAD phosphorylation, pERK, reporter gene) to test drug potency and mechanism. |
| Stable Isotope-Labeled GDF-15 Peptide (SIS) | Internal standard for Liquid Chromatography-Mass Spectrometry (LC-MS) assays for absolute quantification of GDF-15. |
Visualizations
Title: Mechanism of a GDF-15 Mimetic Drug
Title: Phase II Trial Core Assessment Timeline
Title: Phase II Endpoint Hierarchy & Examples
Navigating Challenges: Side Effects, Resistance, and Combination Therapy Strategies
The study of Growth Differentiation Factor 15 (GDF-15) has emerged as a pivotal area in metabolic research, particularly for diabetes and obesity. GDF-15, a stress-responsive cytokine, is a potent anorectic agent and a key mediator of the nausea and vomiting response via its specific receptor, GDNF family receptor α-like (GFRAL), expressed in the hindbrain. This places GDF-15 and its signaling pathway at the intersection of therapeutic efficacy (weight loss, glycemic control) and dose-limiting adverse effects. Understanding and mitigating GDF-15-induced nausea and vomiting is therefore critical for developing viable therapeutics. This guide details the mechanistic basis of these effects, contrasts them with those of GLP-1 receptor agonists (GLP-1RAs), and outlines evidence-based dosing and experimental strategies to dissect and manage these responses.
Mechanistic Basis: GDF-15 vs. GLP-1 Agonist-Induced Emesis
Nausea and vomiting induced by GDF-15 and GLP-1RAs originate from distinct anatomical sites and molecular pathways, though both ultimately converge on brainstem nuclei controlling emesis.
GDF-15/GFRAL Pathway: GDF-15, produced peripherally under cellular stress, crosses the blood-brain barrier poorly. Its primary action is mediated by binding to the GFRAL receptor, which is exclusively expressed in the area postrema (AP) and nucleus tractus solitarius (NTS) in the hindbrain. GFRAL forms a functional complex with the RET tyrosine kinase coreceptor. Ligand binding activates intracellular pathways (MAPK/ERK, PI3K/AKT, PLCγ) leading to neuronal activation that triggers aversive feeding behavior and emesis.
GLP-1 Receptor Agonist Pathway: GLP-1RAs act on the widely distributed GLP-1 receptor (GLP-1R). Emetic effects are primarily mediated via direct activation of GLP-1Rs in the AP and NTS, as well as through vagal afferent signaling from the periphery. Intracellular signaling involves cAMP/PKA and other pathways.
The following diagram illustrates the distinct signaling pathways.
Diagram Title: Distinct Emetic Pathways of GDF-15 and GLP-1 Agonists
Comparative Data on Emetic Potency and Onset
Quantitative data from preclinical and clinical studies highlight key differences in the emetic profiles of GDF-15-based therapies and GLP-1RAs.
Table 1: Comparative Emetic Profiles of GDF-15 vs. GLP-1 Agonists
| Parameter | GDF-15 / GFRAL Agonists | GLP-1 Receptor Agonists (e.g., Liraglutide, Semaglutide) |
|---|---|---|
| Primary Emetic Site | Hindbrain (AP/NTS) via GFRAL | Hindbrain (AP/NTS) & Peripheral Vagal Afferents via GLP-1R |
| Onset of Symptoms | Rapid (hours), often acute dose-limiting | Slower (days to weeks), tends to attenuate with time |
| Tachyphylaxis | Limited evidence; may be persistent | Common; significant adaptation over 4-12 weeks |
| Dose Dependency | Sharp threshold; highly dose-dependent | More graded relationship |
| Potency Correlation | Directly correlated with anorectic/therapeutic efficacy | Can be partially dissociated (e.g., with slow titration) |
| Proposed Mitigation | Precise dosing near efficacy threshold; GFRAL antagonists? | Slow dose escalation; alternative administration routes |
Experimental Protocols for Differentiation and Mitigation
Protocol: Assessing Emetic Response in Preclinical Models
Objective: To quantitatively differentiate GDF-15-mediated from GLP-1RA-mediated nausea/vomiting and test mitigation strategies.
Materials: See "The Scientist's Toolkit" below. Method:
- Animal Preparation: House ferrets or Suncus murinus (house musk shrew) in standard conditions. Implant chronic intravenous catheters for precise compound administration.
- Dosing Regimens:
- Group 1 (GDF-15): Administer recombinant GDF-15 (1-100 µg/kg, IV). Test single bolus vs. slow infusion (over 1-2 hours).
- Group 2 (GLP-1RA): Administer liraglutide or exendin-4 (10-300 µg/kg, IV).
- Group 3 (Control): Administer vehicle.
- Group 4 (Mechanism Blockade): Pre-treat with (a) a GFRAL-blocking antibody (for GDF-15 group) or (b) a GLP-1R antagonist (e.g., exendin(9-39)) (for GLP-1RA group).
- Data Collection: Record for 2 hours post-dose:
- Primary Endpoint: Number of retches + vomits.
- Secondary Endpoints: Latency to first emetic episode, signs of nausea (pica behavior in rodents, conditioned taste aversion).
- Analysis: Compare dose-response curves, total emetic episodes, and efficacy of receptor-specific antagonists.
Protocol: Clinical Dose Titration Strategy for Mitigation
Objective: To design a clinical trial dosing protocol that minimizes nausea/vomiting while maintaining efficacy for a GDF-15-based therapy. Method:
- Phase:
- Phase 1b: Establish the minimum effective dose (MED) for metabolic efficacy (e.g., reduction in ad libitum food intake by >20%) and the emetic threshold dose (ETD; dose inducing emesis in >10% of subjects).
- Strategy:
- Initiate dosing at 30-50% of the MED determined in Phase 1b.
- Employ a slow-escalation regimen, doubling the dose only after 2-4 weeks, allowing for potential adaptation.
- Consider administration modality: Compare subcutaneous bolus vs. controlled-release formulation to blunt peak plasma concentration (C~max~).
- Monitoring: Use validated patient-reported outcome (PRO) tools like the Nausea Profile (NP) questionnaire and daily vomiting diaries. Measure plasma GDF-15 levels to correlate with symptoms.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Studying Emetic Pathways
| Reagent / Material | Function & Application | Key Considerations |
|---|---|---|
| Recombinant Human/Murine GDF-15 | Gold-standard ligand for activating the GFRAL pathway in vitro and in vivo. | Source (E. coli vs. mammalian) affects glycosylation and activity. Use carrier-free for in vivo studies. |
| GLP-1 Receptor Agonists (e.g., Exendin-4, Liraglutide) | Positive control for GLP-1R-mediated emesis. Allows direct comparison to GDF-15 effects. | Liraglutide's prolonged half-life requires longer observation periods. |
| Anti-GFRAL Neutralizing Antibody | Tool to specifically block the GDF-15/GFRAL pathway. Critical for mechanistic confirmation. | Validate for both rodent and non-rodent species in preclinical models. |
| GLP-1R Antagonist (Exendin(9-39)) | Tool to specifically block the GLP-1 receptor. Differentiates GLP-1R-mediated effects. | Short half-life may require continuous infusion in vivo. |
| Phospho-specific Antibodies (pERK, pAKT, pPLCγ) | Detect activation of downstream signaling pathways in AP/NTS tissue lysates or via IHC. | Use fresh-frozen brainstem sections for optimal phospho-protein preservation. |
| Ferret or Suncus murinus Model | Gold-standard emesis-sensitive species for direct measurement of retching/vomiting. | Suncus murinus is smaller and less expensive; ferrets have broader historical data. |
| Conditioned Taste Avoidance (CTA) Assay (Rodents) | Indirect but reliable measure of nausea/malaise in rats/mice, which do not vomit. | Pair a novel sweet solution (e.g., saccharin) with test compound administration. |
| c-Fos IHC Reagents | Marker of neuronal activation in the AP and NTS post-treatment. | Sacrifice animals 60-90 minutes post-dose for peak c-Fos expression. |
Dosing Strategy Decision Workflow
The following diagram outlines a logical framework for developing a dosing strategy that mitigates emesis while preserving efficacy.
Diagram Title: Workflow for Mitigating Emesis in GDF-15 Therapy Dosing
Successful development of GDF-15-based therapeutics for diabetes and obesity hinges on the precise management of its potent emetic effects. By leveraging a deep understanding of the distinct GFRAL-mediated pathway, employing targeted experimental protocols to differentiate it from GLP-1RA effects, and implementing rational, data-driven dosing strategies that respect the sharp threshold of the response, researchers can navigate this challenge. The ultimate goal is to widen the therapeutic window, enabling the translation of GDF-15's powerful metabolic benefits into viable and tolerable treatments.
Within the burgeoning field of GDF-15 (Growth Differentiation Factor 15) research for diabetes and obesity therapeutics, tachyphylaxis—a rapid attenuation of response to a drug following repeated administration—poses a significant translational challenge. This whitepaper delves into the molecular underpinnings of tachyphylaxis, focusing on GFRAL receptor downregulation and post-receptor signaling adaptation, and provides a technical roadmap for its experimental investigation and potential circumvention in drug development.
Core Mechanisms of Tachyphylaxis in Receptor Tyrosine Kinase Signaling
Tachyphylaxis to GDF-15, mediated via its sole known receptor GFRAL (co-receptor with RET), is hypothesized to involve two primary, interlinked mechanisms:
- Receptor Downregulation: Sustained agonist engagement triggers clathrin-mediated endocytosis of the GFRAL-RET complex, leading to lysosomal degradation rather than recycling. This reduces available surface receptors, desensitizing the cell to subsequent stimulation.
- Signaling Adaptation: Despite receptor engagement, intracellular feedback loops dampen the signal. Key adaptations include the upregulation of inhibitory proteins (e.g., SOCS proteins), desensitization of second messengers, and exhaustion of downstream effector capacity.
Pathway Diagram: GFRAL Signaling & Tachyphylaxis Mechanisms
Quantitative Analysis of GDF-15 Induced Tachyphylaxis
Table 1: Reported *In Vivo Effects of Chronic GDF-15 Administration in Rodent Models*
| Study Model (Ref) | Dose & Duration | Initial Response (Day 1-5) | Attenuated Response (Day 10-14) | Proposed Mechanism |
|---|---|---|---|---|
| DIO Mice [1] | 0.5 mg/kg, daily s.c. | ~20% food intake reduction, ~5% weight loss | Food intake near baseline, weight plateau | GFRAL downregulation in AP/NTS neurons |
| Leptin-deficient ob/ob Mice [2] | Recombinant protein, 14 days | Improved glucose tolerance, weight loss | Loss of glycemic benefit | Reduced RET phosphorylation in hindbrain |
| HFD-fed Rats [3] | Sustained infusion, 28 days | Significant anorexia & weight loss | Partial return of appetite (~50% of initial anorectic effect) | Upregulation of hypothalamic AgRP (counter-regulation) |
Table 2: *In Vitro Signaling Kinetics in GFRAL-Expressing Cells*
| Cell Line | Stimulus | Peak pRET/pERK (Time) | Signal Attenuation (Chronic Stim.) | Internalization Rate (t½) |
|---|---|---|---|---|
| HEK293-hGFRAL | 10 nM GDF-15 | 5-10 min | >80% reduction after 24h pre-treatment | ~15-20 min |
| Neuronal Cell Model | 10 nM GDF-15 | 15-30 min | >70% reduction after 16h pre-treatment | Data pending |
Key Experimental Protocols for Investigation
Protocol 3.1: Quantifying GFRAL Surface Expression via Flow Cytometry
Objective: Measure agonist-induced GFRAL downregulation. Detailed Methodology:
- Cell Preparation: Seed GFRAL/RET-expressing HEK293 or neuronal cells.
- Treatment: Treat cells with 10-100 nM GDF-15 or vehicle for 1-24 hours.
- Staining: Harvest cells, wash with ice-cold PBS. Incubate with primary antibody against the extracellular domain of GFRAL (e.g., anti-GFRAL AF1448, R&D Systems) for 1h at 4°C.
- Detection: Wash and incubate with fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488) for 45 min at 4°C, protected from light.
- Analysis: Analyze using a flow cytometer (e.g., BD FACSCelesta). Gate on live cells, measure median fluorescence intensity (MFI) of the treated sample relative to isotype and vehicle controls. Calculate % surface expression remaining.
Protocol 3.2: Monitoring Signaling Adaptation via Western Blot Time-Course
Objective: Assess temporal dynamics and attenuation of downstream phosphorylation. Detailed Methodology:
- Stimulation Time-Course: Serum-starve cells for 4-6h. Stimulate with 10 nM GDF-15 for times ranging from 2 min to 24h. For chronic pre-treatment, pre-incubate with ligand for 16-24h, then re-stimulate with fresh ligand for 10 min.
- Lysis & Quantification: Lyse cells in RIPA buffer with protease/phosphatase inhibitors. Quantify protein concentration via BCA assay.
- Immunoblotting: Load 20-30 µg protein per lane on 4-12% Bis-Tris gels. Transfer to PVDF membranes. Block with 5% BSA in TBST.
- Antibody Probing: Probe overnight at 4°C with primary antibodies: p-RET (Tyr905), total RET, p-ERK1/2 (Thr202/Tyr204), total ERK, p-AKT (Ser473), total AKT, and β-actin loading control.
- Detection: Use HRP-conjugated secondary antibodies and chemiluminescent substrate. Image on a chemiluminescence imager. Quantify band intensity; express p-protein levels normalized to total protein and control.
Experimental Workflow Diagram
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Tachyphylaxis Research in GDF-15/GFRAL Biology
| Item (Example Catalog #) | Function & Application in Tachyphylaxis Studies |
|---|---|
| Recombinant Human GDF-15 Protein (R&D Systems, 957-GD) | The primary agonist for in vitro and in vivo stimulation to induce and study desensitization. |
| Anti-GFRAL Antibody [Extracellular] (R&D Systems, MAB1448) | Critical for flow cytometry to quantify surface receptor expression and internalization. |
| Phospho-RET (Tyr905) Antibody (Cell Signaling Tech, #3221) | Key readout for proximal receptor activation and its attenuation upon chronic stimulation via Western blot. |
| Phospho-ERK1/2 (Thr202/Tyr204) Antibody (CST, #4370) | Standard downstream signaling node to monitor pathway activity and adaptive feedback. |
| SOCS3 Antibody (CST, #2923) | Detects levels of this feedback inhibitor, often upregulated in tachyphylaxis. |
| Clathrin Inhibitor (Pitstop 2, Abcam, ab120687) | Chemical tool to block clathrin-mediated endocytosis, testing its role in receptor downregulation. |
| Lysosomal Inhibitor (Bafilomycin A1, Sigma, B1793) | Blocks lysosomal degradation; used to test if receptor fate (degradation vs. recycling) impacts tachyphylaxis. |
| GFRAL-Expressing Cell Line (e.g., HEK293-hGFRAL/hRET) | Essential engineered model system for controlled, high-signal in vitro studies. |
Strategic Approaches to Overcome Tachyphylaxis
Potential strategies informed by mechanistic understanding include:
- Ligand Engineering: Developing GDF-15 variants or mimetics with biased signaling profiles that favor metabolic effects over internalization signals.
- Dosing Optimization: Pulsatile dosing regimens in vivo, rather than continuous infusion, to allow for receptor re-synthesis and resetting of feedback loops.
- Receptor Trafficking Modulators: Co-administration with agents that promote GFRAL recycling over degradation (e.g., retromer complex enhancers).
- Combination Therapy: Targeting downstream effectors (e.g., MC4R agonists) or inhibitory nodes (e.g., SOCS inhibition) in parallel to sustain the overall anorectic signal.
Overcoming Tachyphylaxis Logic Flow
For GDF-15 research targeting diabetes and obesity, a deep mechanistic dissection of tachyphylaxis is not merely academic but crucial for clinical translation. By systematically quantifying receptor dynamics and signaling adaptation using the outlined protocols, and by strategically targeting these vulnerabilities, researchers can design next-generation therapeutics with durable efficacy.
Introduction Within the therapeutic paradigm for metabolic diseases like obesity and type 2 diabetes, Growth Differentiation Factor 15 (GDF15) has emerged as a potent anorexigenic hormone. Its action is exclusively mediated through binding to the GDNF family receptor α-like (GFRAL), expressed solely in the hindbrain. This specificity presents a unique opportunity for targeted therapy but also a significant challenge: ensuring pharmacological agents engage only GFRAL-positive neurons to avoid off-target effects in other tissues that may express GDF15 or its receptors at low, yet pharmacologically active, levels. This guide details the technical strategies and experimental frameworks for achieving and validating this precise targeting.
Mechanistic Basis and Off-Target Concerns GDF15 signals exclusively via a heterodimeric receptor complex of GFRAL (ligand-binding) and RET (tyrosine kinase) co-receptor. While GFRAL expression is restricted, RET is broadly expressed in the peripheral and central nervous systems. Furthermore, recent studies suggest potential low-affinity interactions or "off-target" binding of engineered GDF15 analogs to other TGF-β superfamily receptors (e.g., ALK4/5/7), which could mediate unintended effects in peripheral tissues like skeletal muscle, adipose tissue, or the cardiovascular system.
Table 1: Potential Off-Target Receptors and Associated Tissues
| Receptor/Complex | Primary Ligand | Tissue Expression | Potential Risk with GDF15 Analogs |
|---|---|---|---|
| GFRAL/RET | GDF15 | Hindbrain Neurons | Intended Target |
| RET (alone/with other GFRα) | GDNF, NRTN | PNS, ENS, CNS | Unintended RET activation |
| ALK4/ActRIIB | Activin, Nodal | Muscle, Fat, Pituitary | Mimicry of Activin signaling |
| ALK5/TGFβRII | TGF-β | Ubiquitous | Fibrotic or inflammatory signaling |
Experimental Protocols for Validating Specificity
1. In Vitro Receptor Specificity Profiling
- Method: Cell-Based Luciferase Reporter Assay (SMAD2/3 Response).
- Protocol:
- Seed HEK293T cells in 96-well plates.
- Co-transfect with: (a) a luciferase reporter plasmid under a SMAD-responsive element (CAGA box), (b) a Renilla luciferase control plasmid, and (c) expression plasmids for the receptor pair of interest (e.g., GFRAL/RET, ALK4/ActRIIB, ALK5/TGFβRII).
- 24h post-transfection, treat cells with serial dilutions of wild-type GDF15 and the engineered GDF15 analog.
- After 16-20h, lyse cells and measure firefly and Renilla luciferase activity using a dual-luciferase assay kit.
- Calculate fold induction over vehicle control, normalized to Renilla activity.
- Interpretation: A truly specific GFRAL-targeting analog will show potent, dose-dependent activity only in GFRAL/RET-transfected wells, with minimal activity in other receptor pair wells compared to their canonical ligands.
2. Ex Vivo Brainstem Slice Electrophysiology
- Method: Patch-Clamp Recording on Identified GFRAL+ Neurons.
- Protocol:
- Prepare acute coronal brainstem slices (200-300 µm) from Gfral-GFP or Gfral-Cre;Ai14 reporter mice in ice-cold, sucrose-based artificial cerebrospinal fluid (aCSF).
- Incubate in standard aCSF (32°C) for recovery.
- Visualize GFP or tdTomato-positive neurons in the area postrema (AP) and nucleus tractus solitarius (NTS) under fluorescence-equipped microscopy.
- Perform whole-cell current- or voltage-clamp recordings on identified neurons.
- Bath apply the GDF15 analog while monitoring changes in firing rate or postsynaptic currents.
- Include a washout and subsequent application of wild-type GDF15 as a positive control.
- Interpretation: Specificity is supported if the analog rapidly and reversibly activates only GFP+ neurons, with a potency (EC50) comparable to native GDF15.
3. In Vivo Target Engagement and Peripheral Activity Screen
- Method: Pharmacodynamic and c-Fos Immunohistochemistry.
- Protocol:
- Administer vehicle or GDF15 analog (equi-anorexigenic dose) to wild-type and Gfral knockout mice.
- For c-Fos: Perfuse mice 90-min post-injection. Section brain and key peripheral organs (heart, skeletal muscle, kidney). Immunostain for c-Fos (neuronal activation marker) and, in brain, co-stain for GFRAL.
- Quantify c-Fos+ nuclei in GFRAL+ brain regions (AP, NTS) and peripheral tissues.
- In parallel cohorts, measure acute food intake and collect plasma 1h post-dose for biomarker analysis (e.g., insulin, GDF15 itself, Activin B).
- Interpretation: Specific targeting is confirmed by: (a) c-Fos induction exclusively in hindbrain GFRAL+ neurons of WT, but not Gfral KO mice, (b) no significant c-Fos induction in peripheral tissues, and (c) no significant biomarker changes indicative of peripheral TGF-β/Activin pathway activation.
Diagram Title: GDF15 Target vs. Off-Target Signaling Pathways
Diagram Title: Validation Workflow for GFRAL-Specific Targeting
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for GDF15/GFRAL Specificity Research
| Reagent/Material | Supplier Examples | Function/Application |
|---|---|---|
| Recombinant Human/Mouse GDF15 | R&D Systems, PeproTech | Gold-standard positive control for in vitro and in vivo assays. |
| GFRAL Knockout Mice | Jackson Laboratories, in-house CRISPR | Essential genetic control to prove on-target mechanism in vivo. |
| GFRAL Reporter Mice (Gfral-GFP/Cre) | Available through academic consortia | Enables identification and isolation of GFRAL+ neurons for electrophysiology or transcriptomics. |
| Phospho-SMAD2/3 (Ser465/467/423/425) Antibody | Cell Signaling Technology | Detects activation of canonical TGF-β/Activin pathways in peripheral tissues (off-target biomarker). |
| c-Fos (9F6) Rabbit mAb | Cell Signaling Technology | Standard antibody for mapping neuronal activation (target engagement) in IHC. |
| Dual-Luciferase Reporter Assay System | Promega | Quantifies pathway-specific transcriptional activity in receptor specificity screens. |
| RET Kinase Inhibitor (e.g., GSK3179106) | MedChemExpress | Pharmacological tool to inhibit RET and confirm dependence of analog's effect on RET kinase activity. |
| Activin B / TGF-β1 ELISA Kits | R&D Systems | Measure plasma biomarkers indicative of unintended peripheral pathway activation. |
Growth Differentiation Factor 15 (GDF-15) has emerged as a significant metabolic regulator, with elevated levels associated with conditions of metabolic stress, including obesity and type 2 diabetes (T2D). Unlike Glucagon-like peptide-1 (GLP-1) and amylin receptor agonists, which primarily act on central appetite circuits and pancreatic function, GDF-15 signals through the GDNF family receptor α-like (GFRAL) receptor, uniquely expressed in the hindbrain. This distinct mechanism presents a compelling rationale for combination therapy: targeting complementary central and peripheral pathways could yield additive or synergistic effects on weight loss, glycemic control, and cardiometabolic parameters, potentially overcoming the plateau effects and adverse responses seen with monotherapies.
Mechanistic Foundations & Signaling Pathways
GDF-15/GFRAL Signaling
GDF-15 binds with high affinity to GFRAL, which forms a functional receptor complex with the RET tyrosine kinase. This interaction activates downstream pathways including PI3K/AKT, MAPK/ERK, and PLCγ, ultimately influencing neuronal activity in the area postrema and nucleus tractus solitarius to induce anorexia and nausea.
GLP-1 Receptor Agonist Signaling
GLP-1R agonists activate G-protein coupled receptors, leading to increased cAMP, PKA activation, and subsequent pathways that potentiate glucose-dependent insulin secretion, suppress glucagon, slow gastric emptying, and promote satiety via hypothalamic and hindbrain circuits.
Amylin Receptor Agonist Signaling
Amylin acts primarily via the calcitonin receptor (CTR) complexed with receptor activity-modifying proteins (RAMPs). Activation reduces food intake via the area postrema, slows gastric emptying, and suppresses postprandial glucagon secretion.
Diagram 1: Core Signaling Pathways of GDF-15, GLP-1, and Amylin
Table 1: Comparative Monotherapy Efficacy Profiles in Preclinical Models
| Parameter | GDF-15 Analogue | GLP-1RA (e.g., Semaglutide) | Amylin Analogue (e.g., Pramlintide) | Notes |
|---|---|---|---|---|
| Body Weight Reduction | 10-25% | 10-30% | 5-15% | Diet-induced obese rodent models; dose & duration dependent. |
| Food Intake Suppression | 30-60% | 40-70% | 20-40% | Acute effect typically more pronounced for GLP-1RA. |
| Glucose Tolerance | Improved | Significantly Improved | Moderately Improved | GLP-1RA has direct insulin secretagogue effect. |
| GFRAL Expression Site | Area Postrema / NTS | Widely distributed (pancreas, brain, heart) | Area Postrema / NTS | Key determinant of side-effect profile (nausea). |
| Onset of Tachyphylaxis | Limited data | Observed in some models | Observed | Combination may delay tolerance. |
Table 2: Key Clinical Trial Data for Relevant Agents (as of latest search)
| Agent / Class | Phase | Key Population | Weight Loss (vs placebo) | HbA1c Reduction | Notable Adverse Events (AEs) |
|---|---|---|---|---|---|
| Semaglutide (GLP-1RA) | IV (Marketed) | Obesity (STEP trials) | ~12.4-14.9% | N/A (non-T2D) | GI events (nausea, diarrhea) common, usually transient. |
| Tirzepatide (GIP/GLP-1RA) | IV (Marketed) | T2D (SURPASS) | ~7.6-11.7 kg | -1.69 to -2.58% | GI events. |
| Pramlintide (Amylin) | IV (Marketed) | T2D & Obesity | ~3.7 kg (modest) | -0.3 to -0.6% | Nausea, hypoglycemia (with insulin). |
| GDF-15 analogue (CT-868) | I/II | T2D | Preliminary data shows dose-dependent trend | Preliminary reductions | Nausea, vomiting reported; aligns with mechanism. |
Proposed Experimental Protocols for Combination Studies
In Vivo Efficacy Protocol: Diet-Induced Obese (DIO) Mouse Model
Objective: To evaluate the synergistic effects of GDF-15 analogue co-administered with a GLP-1RA or amylin analogue on body weight, body composition, and glucose metabolism.
Detailed Methodology:
- Animals: 10-week-old male C57BL/6J mice, fed a 60% high-fat diet (HFD) for 12 weeks to induce obesity and insulin resistance.
- Group Allocation (n=12/group):
- Group 1: Vehicle control (PBS, s.c.)
- Group 2: GDF-15 analogue monotherapy (e.g., 0.3 mg/kg, s.c., daily)
- Group 3: GLP-1RA monotherapy (e.g., Semaglutide, 0.04 mg/kg, s.c., daily)
- Group 4: Amylin analogue monotherapy (e.g., Pramlintide, 0.5 mg/kg, s.c., TID)
- Group 5: GDF-15 analogue + GLP-1RA (doses as above)
- Group 6: GDF-15 analogue + Amylin analogue (doses as above)
- Treatment Duration: 28 days.
- Primary Endpoints:
- Daily food intake and weekly body weight measurement.
- Body composition analysis via EchoMRI at baseline and endpoint.
- Oral Glucose Tolerance Test (OGTT; 2g/kg glucose) at day 26 after a 6-hour fast.
- Secondary/Tertiary Endpoints:
- Plasma hormones (insulin, active GLP-1, total GDF-15) via multiplex immunoassay.
- Terminal tissue collection for hypothalamic and hindbrain gene expression analysis (qPCR for c-Fos, Pomc, Cartpt) and histology.
- Indirect calorimetry (TSE Systems) in a subset to assess energy expenditure and RER.
Diagram 2: In Vivo Combination Study Workflow
In Vitro Protocol: Neuronal Activation Assay
Objective: To assess combinatorial effects on neuronal activation in GFRAL- and GLP-1R-expressing cell lines.
- Cell Culture: Stable HEK293 cell lines expressing human GFRAL/RET or GLP-1R.
- Stimulation: Cells treated for 30 min with vehicle, single agents, or combinations.
- Readout: Phospho-ERK1/2 and phospho-AKT detection via Western Blot or AlphaLISA. Dose-response matrices analyzed for synergy using Chou-Talalay method (CompuSyn software).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for GDF-15/Incretin Combination Research
| Reagent / Material | Supplier Examples (for reference) | Function in Research |
|---|---|---|
| Recombinant Human GDF-15 Protein | R&D Systems, PeproTech | The canonical ligand for in vitro receptor activation studies and as a control for analogue drugs. |
| GFRAL Antibody (for IHC/ICC) | Sigma-Aldrich, Abcam | Validates GFRAL expression patterns in tissue sections and cell lines; critical for mechanistic studies. |
| Phospho-RET (Tyr905) Antibody | Cell Signaling Technology | Detects activation of the GDF-15/GFRAL/RET signaling complex in downstream assays. |
| GLP-1R Agonist (e.g., Exendin-4) | Tocris, MedChemExpress | Tool compound for in vitro and in vivo studies of GLP-1 receptor-mediated effects. |
| Amylin Receptor Agonist (e.g., Salmon Calcitonin) | Sigma-Aldrich, Bachem | Used to probe amylin receptor-specific signaling and compare/combine with GDF-15 effects. |
| cAMP ELISA Kit | Cisbio, Abcam | Universal downstream readout for GPCR activation by GLP-1RA and amylin analogues. |
| Multiplex Metabolic Hormone Panel (MSD/ Luminex) | Meso Scale Discovery, Millipore | Quantifies key circulating factors (Insulin, GLP-1, GIP, GDF-15) from small-volume in vivo samples. |
| Diet-Induced Obese (DIO) Mice | Jackson Laboratory, Charles River | Standardized preclinical model for obesity, insulin resistance, and pharmacotherapy testing. |
| Indirect Calorimetry System | Columbus Instruments, TSE Systems | Precisely measures energy expenditure, respiratory quotient (RQ), and locomotor activity in vivo. |
| Software for Synergy Analysis (CompuSyn) | ComboSyn Inc. | Employs the Chou-Talalay method to determine if drug combinations are additive, synergistic, or antagonistic. |
This technical guide details methodologies for patient stratification based on the GDF-15/GFRAL pathway, a rapidly evolving axis in metabolic disease research. Within the broader thesis on GDF-15's role in diabetes and obesity, identifying individuals with elevated biomarker levels is critical for targeted therapeutic intervention. GDF-15, a stress-responsive cytokine, exerts its anorexic and metabolic effects exclusively via the glial cell-derived neurotrophic factor (GDNF) family receptor alpha-like (GFRAL), expressed in the hindbrain. Stratifying "high expressers" enables precision medicine approaches for weight management and glycemic control.
Table 1: Reported Circulating GDF-15 Levels in Human Cohorts
| Condition / Cohort | Median/Mean GDF-15 (pg/mL) | Reported Range (pg/mL) | Assay Method | Key Citation (Example) |
|---|---|---|---|---|
| Healthy Individuals | 400 - 600 | 200 - 1200 | Electrochemiluminescence | Kleinert et al., 2018 |
| Obesity (BMI >30) | 800 - 1200 | 450 - 2500 | Multiplex Immunoassay | Tsai et al., 2019 |
| Type 2 Diabetes | 1000 - 1500 | 600 - 4000 | ELISA | Conte et al., 2020 |
| NASH / NAFLD | 1100 - 1800 | 700 - 3500 | Electrochemiluminescence | Chung et al., 2019 |
| GDF-15 Analogue Therapy (Post-Treatment) | 5000 - 15000 | 3000 - 20000 | ELISA | Day et al., 2023 |
Table 2: GFRAL Expression Profiles Across Tissues (Human & Murine)
| Tissue | Species | Expression Level (Relative) | Detection Method | Note |
|---|---|---|---|---|
| Area Postrema / NTS | Mouse, Human | High | RNA-seq, IHC | Exclusive signaling site. |
| Kidney | Mouse, Human | Very Low / Negligible | qPCR | Basal, non-functional. |
| Small Intestine | Mouse | Low | Single-cell RNA-seq | Potential minor expression. |
| Adipose Tissue | Human (obese) | Low (Controversial) | qPCR | May be disease-state dependent. |
| Stratification Threshold Proposal | Human Plasma GDF-15 | > 1200 pg/mL | Validated ELISA | Suggests "High Expresser" status for enrichment in clinical trials. |
Core Experimental Protocols
Protocol A: Quantifying Circulating GDF-15 in Human Serum/Plasma
Objective: To accurately measure GDF-15 protein concentration for stratification. Reagents: Human GDF-15 Quantikine ELISA Kit (R&D Systems, #DGD150) or equivalent Mesoscale Discovery (MSD) electrochemiluminescence assay. Procedure:
- Sample Collection: Collect venous blood into EDTA or serum separator tubes. Process within 30 min (centrifuge at 1000-2000 x g for 10 min). Aliquot and store at -80°C. Avoid freeze-thaw cycles.
- Assay Setup: Follow manufacturer's instructions. Briefly, coat plate with capture antibody. Block. Add samples and standards in duplicate.
- Incubation & Detection: Incubate samples (2h, RT). Wash. Add detection antibody (2h, RT). Wash. Add Streptavidin-HRP (20 min, RT). Wash. Add substrate (TMB, 20 min). Stop with acid.
- Analysis: Read absorbance at 450nm (570nm correction). Fit standard curve (4-parameter logistic). Report concentrations in pg/mL. Stratification: Subjects with [GDF-15] > 1200 pg/mL are classified as "High GDF-15 Expressers."
Protocol B: Detecting GFRAL mRNA Expression from Biopsy Tissues (Preclinical/Exploratory)
Objective: To assess GFRAL gene expression in tissues (e.g., from exploratory clinical biopsies). Reagents: TRIzol, DNase I, cDNA synthesis kit, qPCR master mix, human GFRAL TaqMan assay (Hs04194707_s1), reference genes (GAPDH, PPIA). Procedure:
- RNA Extraction: Homogenize ~30mg tissue in TRIzol. Chloroform phase separation. Precipitate RNA with isopropanol. Wash with 75% ethanol. Resuspend in nuclease-free water. Treat with DNase I.
- cDNA Synthesis: Use 500ng - 1μg total RNA with reverse transcriptase and oligo(dT)/random primers.
- Quantitative PCR: Prepare 20μL reactions: 10μL TaqMan Master Mix, 1μL assay, 2μL cDNA, 7μL H2O. Run in triplicate. Cycling: 95°C 10min; (95°C 15s, 60°C 1min) x 40 cycles.
- Data Analysis: Calculate ΔCt (CtGFRAL - Ctgeomean(reference genes)). Use ΔΔCt method for relative quantification. Low Ct values (e.g., <30 in AP/NTS) indicate "High GFRAL Expression."
Protocol C: Immunohistochemical (IHC) Staining for GFRAL Protein
Objective: Spatial localization and semi-quantitative assessment of GFRAL protein in tissue sections (preclinical models). Reagents: Anti-GFRAL antibody (e.g., Rabbit monoclonal [EPR21831-111], Abcam), species-specific HRP polymer, DAB substrate, hematoxylin. Procedure:
- Tissue Preparation: Perfuse-fix mouse with 4% PFA. Dissect brainstem, post-fix 24h, paraffin-embed. Cut 5μm sections.
- Deparaffinization & Antigen Retrieval: Bake slides (60°C, 1h). Deparaffinize in xylene, rehydrate through graded ethanol. Perform heat-induced epitope retrieval in citrate buffer (pH 6.0).
- Staining: Block endogenous peroxidase (3% H2O2). Block non-specific sites (5% normal goat serum, 1h). Incubate with primary anti-GFRAL (1:500, 4°C, overnight). Wash. Apply HRP-conjugated secondary polymer (30min, RT). Wash. Develop with DAB (2-10 min). Counterstain with hematoxylin.
- Imaging & Scoring: Image with brightfield microscope. Use a semi-quantitative H-score (intensity x % positive cells) by a blinded pathologist.
Signaling Pathway & Workflow Visualizations
Title: GDF-15/GFRAL Signaling Cascade in Metabolism
Title: Biomarker-Driven Patient Stratification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for GDF-15/GFRAL Research
| Item (Catalog Example) | Vendor (Example) | Function & Application |
|---|---|---|
| Human GDF-15 Quantikine ELISA Kit (DGD150) | R&D Systems | Gold-standard for quantifying human GDF-15 protein in serum/plasma/cell supernatants. |
| Mouse/Rat GDF-15 ELISA Kit | MilliporeSigma | Specific quantitation of rodent GDF-15 for preclinical studies. |
| Anti-GDF-15 Antibody [EPR21435-114] | Abcam | Neutralizing or detecting antibody for Western blot, IHC, or functional blocking assays. |
| Anti-GFRAL Antibody [EPR21831-111] | Abcam | Rabbit monoclonal for detecting GFRAL protein in IHC (mouse, human) and Western blot. |
| TaqMan Gene Expression Assay (Hs04194707_s1) | Thermo Fisher | qPCR assay for specific, sensitive detection of human GFRAL mRNA. |
| Recombinant Human GDF-15 Protein (120-28) | PeproTech | High-purity ligand for in vitro stimulation experiments and assay standards. |
| MSD U-PLEX GDF-15 Assay | Mesoscale Discovery | High-throughput, multiplexable electrochemiluminescence assay for clinical research. |
| RNAlater Stabilization Solution | Thermo Fisher | Preserves RNA in tissue samples for accurate GFRAL expression analysis post-biopsy. |
| Ret Kinase Inhibitor (RXDX-105) | MedChemExpress | Tool compound to inhibit RET co-receptor, validating GFRAL/RET pathway specificity. |
GDF-15 vs. Current Therapeutics: Efficacy, Safety, and Mechanistic Comparisons
Within the pursuit of next-generation metabolic therapies for diabetes and obesity, Growth Differentiation Factor 15 (GDF-15) has emerged as a potent anorectic signal with a mechanism distinct from established pathways like Glucagon-like Peptide-1 (GLP-1) and Leptin. This whitepaper provides a detailed technical comparison of these signaling axes, framing GDF-15/GFRAL as a complementary, brainstem-centric pathway that bypasses key limitations of canonical energy homeostasis systems, thereby offering a novel therapeutic target for sustained weight loss and glycemic control.
Core Signaling Pathways: A Comparative Analysis
Pathway Diagram: GDF-15/GFRAL Signaling Cascade
Diagram 1: GDF-15 binds GFRAL/RET to activate ERK via PLCγ/PKC.
Pathway Diagram: GLP-1/GLP-1R Signaling Cascade
Diagram 2: GLP-1 signals via Gs-coupled GPCR to increase cAMP and PKA activity.
Pathway Diagram: Leptin Signaling Cascade
Diagram 3: Leptin signals via JAK2-STAT3, inducing SOCS3 feedback.
Quantitative Comparison of Signaling Axes
Table 1: Comparative Overview of Metabolic Signaling Pathways
| Feature | GDF-15/GFRAL | GLP-1/GLP-1R | Leptin/LEPRb |
|---|---|---|---|
| Primary Receptor | GFRAL (GDNF-family) + RET coreceptor | GLP-1R (Class B1 GPCR) | LEPRb (Cytokine receptor) |
| Key 2nd Messengers | p-ERK1/2, PLCγ, PKC | cAMP, PKA, p-CREB | p-STAT3, p-ERK, PI3K |
| Central Site of Action | Area Postrema / Nucleus Tractus Solitarius (Brainstem) | Nucleus Tractus Solitarius, Hypothalamus, Area Postrema | Arcuate Nucleus (Hypothalamus) |
| Primary Metabolic Effects | Reduced food intake, conditioned taste aversion (nausea), weight loss | Glucose-dependent insulin secretion, reduced appetite, delayed gastric emptying | Suppressed appetite, increased energy expenditure, improved insulin sensitivity |
| Resistance in Obesity | Not observed; pathway sensitivity may be retained | Mild receptor desensitization reported | Severe central resistance hallmark of obesity |
| Therapeutic Efficacy (Weight Loss) | ~10-20% in preclinical models | ~15-25% (clinical, e.g., Semaglutide) | Minimal in leptin-resistant obesity |
Table 2: Key Experimental Readouts and Quantitative Changes
| Assay | GDF-15/GFRAL Intervention | GLP-1R Agonist Intervention | Leptin Intervention (in Sensitive State) |
|---|---|---|---|
| Food Intake (Acute) | ↓ 50-80% in mice (dose-dependent) | ↓ 30-60% in rodents | ↓ 30-50% in rodents |
| Body Weight (Chronic) | ↓ 10-20% over 2-4 weeks in DIO mice | ↓ 10-15% in DIO mice; ~15-20% in humans | ↓ 5-10% in leptin-deficient ob/ob mice |
| Plasma p-ERK1/2 in AP | ↑ ~3-5 fold | Mild or no change | No significant change |
| cAMP in Target Cells | No change | ↑ ~2-4 fold | No direct activation |
| p-STAT3 in ARC | No change | Indirect, minor | ↑ ~4-8 fold |
| Nausea/CTA Induction | Strong (dose-limiting) | Moderate, often transient | Minimal |
Detailed Experimental Protocols
Protocol: Assessing GDF-15-Induced Anorexia and Neuronal Activation
Aim: To quantify acute food intake suppression and map neuronal activation (c-Fos) in the brainstem following GDF-15 administration.
- Animal Model: Use male C57BL/6J mice (8-12 weeks) or diet-induced obese (DIO) mice. House under standard conditions (12h light/dark).
- Recombinant GDF-15: Reconstitute recombinant mouse GDF-15 in PBS with 0.1% BSA. Prepare vehicle control (PBS/0.1% BSA).
- Dosing & Groups: Randomize mice into groups (n=8-10). Administer GDF-15 (0.1-0.5 mg/kg) or vehicle via intraperitoneal (i.p.) injection at the onset of the dark cycle.
- Food Intake Measurement: Pre-weigh standard chow. Present food immediately post-injection. Re-weigh food at 1, 2, 4, 6, and 24 hours post-injection. Calculate cumulative intake.
- Perfusion & Tissue Collection: 90 minutes post-injection, deeply anesthetize mice with pentobarbital. Transcardially perfuse with ice-cold PBS followed by 4% paraformaldehyde (PFA). Harvest brains and post-fix in 4% PFA overnight at 4°C, then cryoprotect in 30% sucrose.
- Immunohistochemistry (c-Fos): Cut 30 µm coronal brainstem sections (Area Postrema/NTS region). Perform standard IHC: block, incubate with primary anti-c-Fos antibody (1:1000, rabbit), then appropriate biotinylated secondary antibody and ABC kit. Develop with DAB. Image and quantify c-Fos+ nuclei in the AP and NTS using stereological software.
- Analysis: Compare food intake (ANOVA with repeated measures) and c-Fos counts (Student's t-test) between GDF-15 and vehicle groups.
Protocol: In Vitro Signaling Assay for GFRAL Pathway Activation
Aim: To validate GDF-15-induced phosphorylation of ERK1/2 in GFRAL-expressing cells.
- Cell Line: HEK293T cells transiently or stably co-transfected with mouse Gfral and Ret expression plasmids. Include mock-transfected controls.
- Stimulation: Plate cells in 12-well plates. At 80-90% confluency, serum-starve for 4-6 hours. Stimulate with recombinant GDF-15 (10-100 nM) or vehicle for 5, 15, and 30 minutes.
- Cell Lysis: Aspirate medium, wash with ice-cold PBS. Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors.
- Western Blot:
- Separate proteins (30 µg total protein) via SDS-PAGE (4-12% Bis-Tris gel).
- Transfer to PVDF membrane.
- Block with 5% BSA in TBST for 1 hour.
- Incubate overnight at 4°C with primary antibodies: anti-phospho-p44/42 ERK1/2 (Thr202/Tyr204) (1:2000) and anti-total ERK1/2 (1:3000).
- Incubate with HRP-conjugated secondary antibody (1:5000) for 1 hour at RT.
- Develop with ECL substrate and image. Quantify band intensity (p-ERK/total ERK ratio) using densitometry software.
Protocol: Contrasting with GLP-1R cAMP Accumulation Assay
Aim: To measure GLP-1-induced cAMP production, a hallmark of GLP-1R activation.
- Cell Line: CHO-K1 cells stably expressing human GLP-1R.
- cAMP Assay Kit: Use a commercially available HTRF (Homogeneous Time-Resolved Fluorescence) cAMP assay kit.
- Procedure: Plate cells in 96-well plates. Prior to assay, replace medium with stimulation buffer containing phosphodiesterase inhibitor (IBMX). Treat cells with GLP-1 (0.1 nM - 1 µM) or forskolin (positive control) for 30 minutes at 37°C.
- Detection: Lyse cells according to kit protocol. Add cAMP-d2 conjugate and anti-cAMP cryptate antibody. Incubate for 1 hour at RT. Measure fluorescence resonance energy transfer (FRET) at 620 nm and 665 nm using a compatible plate reader.
- Analysis: Calculate cAMP concentration from standard curve. Plot dose-response curve and determine EC50 for GLP-1.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Mechanistic Studies
| Reagent / Material | Function / Application | Example (Non-exhaustive) |
|---|---|---|
| Recombinant GDF-15 Protein | Ligand for in vivo and in vitro stimulation of the GFRAL pathway. | Mouse/Rat GDF-15, carrier-free. |
| Anti-GFRAL Antibody | Detection of receptor expression via IHC, Western blot, or blocking studies. | Validated monoclonal antibody for mouse tissue. |
| Anti-phospho-ERK1/2 (Thr202/Tyr204) Antibody | Key readout for GFRAL/RET signaling activation in Western blot or IHC. | Rabbit monoclonal, specific for dual phosphorylation. |
| c-Fos Antibody | Marker for neuronal activation in brain sections following metabolic interventions. | Polyclonal or monoclonal anti-c-Fos. |
| GLP-1R Agonist (e.g., Exendin-4) | Positive control for GLP-1R pathway; tool compound for comparative studies. | Exendin-4, Liraglutide. |
| LEPRb-Expressing Cell Line | In vitro model for studying canonical leptin signaling (e.g., SH-SY5Y-LEPRb). | Stably transfected neuronal cell line. |
| Phospho-STAT3 (Tyr705) Antibody | Primary readout for leptin receptor activation. | High-sensitivity antibody for WB/IHC. |
| HTRF cAMP Assay Kit | Quantitative, homogeneous assay for GLP-1R and other Gs-protein coupled receptor activity. | Cisbio cAMP Gs Dynamic Kit. |
| DIO Mouse Model | Gold-standard preclinical model for obesity and therapeutic efficacy studies. | C57BL/6J mice fed 60% high-fat diet for 12+ weeks. |
| Gfral Knockout Mouse | Essential control for establishing GDF-15 effects as GFRAL-specific. | Global or conditional Gfral KO strains. |
Within the context of growth differentiation factor 15 (GDF-15) research for diabetes and obesity, establishing robust preclinical efficacy benchmarks is critical for validating therapeutic potential and guiding clinical translation. GDF-15, a stress-responsive cytokine acting via the glial cell-derived neurotrophic factor family receptor α-like (GFRAL) in the hindbrain, has emerged as a key mediator of appetite and metabolic regulation. This guide details the core outcome measures, experimental models, and protocols essential for evaluating GDF-15-based therapeutics in preclinical settings.
Core Efficacy Benchmarks & Quantitative Data Summaries
Preclinical studies for metabolic agents must report on three primary domains: weight loss, glycemic control, and integrated cardio-metabolic parameters. The following tables summarize expected benchmarks based on current literature for GDF-15 pathway interventions (e.g., recombinant protein administration, GFRAL agonists) compared to other established mechanisms.
Table 1: Weight Loss & Body Composition Benchmarks in DIO Mice (10-12 week intervention)
| Intervention / Model | Weight Loss (% from baseline) | Fat Mass Reduction (%) | Lean Mass Preservation | Key Notes |
|---|---|---|---|---|
| GDF-15 (pharmacologic) | 15-25% | 20-35% | High (>95%) | Dose-dependent, sustained with continued dosing. |
| GLP-1R Agonist (e.g., Semaglutide) | 10-20% | 15-25% | High | Requires titration to avoid nausea. |
| Dual GLP-1/GIP Agonist (e.g., Tirzepatide) | 20-30% | 25-40% | High | Superior weight loss in head-to-head studies. |
| Caloric Restriction (Pair-fed) | Matched to drug group | Matched | Variable | Controls for anorectic effects. |
| Vehicle / Placebo | +2 to +5% (gain) | +5 to +10% (gain) | Stable | High-fat diet (HFD) continued. |
Table 2: Glycemic Control Benchmarks in Obese, Insulin-Resistant Models
| Parameter & Test | Excellent Response | Moderate Response | Minimal/No Response | Standard Model (Mouse) |
|---|---|---|---|---|
| Fasting Glucose | Reduction ≥30% | Reduction 15-29% | Reduction <15% | db/db or DIO-STZ |
| HbA1c / Glycated Albumin | Reduction ≥1.5% pt (HbA1c) | Reduction 0.5-1.4% pt | Reduction <0.5% pt | db/db |
| OGTT / IPGTT (AUC) | Reduction ≥40% | Reduction 20-39% | Reduction <20% | DIO C57BL/6J |
| HOMA-IR | Reduction ≥50% | Reduction 25-49% | Reduction <25% | DIO |
| Insulin Tolerance Test (ITT) | Improvement ≥30% | Improvement 15-29% | Improvement <15% | DIO |
Table 3: Cardio-Metabolic & Safety Biomarkers
| Biomarker Category | Specific Marker | Expected Positive Direction | Associated Risk Assessment |
|---|---|---|---|
| Lipids & Hepatic | Plasma Triglycerides | Decrease (↓ 25-50%) | Reduced steatosis, CVD risk |
| Plasma NEFA (Free Fatty Acids) | Decrease (↓ 20-40%) | Improved insulin sensitivity | |
| Hepatic TG Content (Histology/Biochem) | Decrease (↓ 30-60%) | Reduced NAFLD/NASH activity | |
| Cardiovascular | Blood Pressure (Telemetry in rats) | Mild decrease or neutral | Beneficial if hypertensive |
| Heart Rate | Monitor for tachycardia/bradycardia | Potential GFRAL-mediated effect | |
| Inflammation | Plasma CRP (or mouse analogue) | Decrease | Reduced systemic inflammation |
| Adipose Tissue Macrophage Infiltration | Decrease (F4/80+ staining) | Improved adipose health | |
| Safety | Pancreatic Amylase/Lipase | No change | Monitor for pancreatic stress |
| Plasma ALT/AST | No change or decrease | Indicator of hepatic safety |
Detailed Experimental Protocols
Protocol for Chronic Efficacy Study in Diet-Induced Obese (DIO) Mice
Objective: To evaluate the effects of a GDF-15 pathway agent on body weight, composition, and glycemic control. Model: Male C57BL/6J mice fed a 60% high-fat diet (HFD) for 12-16 weeks until obese (>45g). Groups (n=10-15): 1) Vehicle control, 2) GDF-15 agent (low/high dose), 3) GLP-1R agonist reference, 4) Pair-fed to high-dose group. Dosing: Subcutaneous injection, daily or as per pharmacokinetics, for 4-8 weeks. Weekly Measurements: Body weight, food intake. Terminal Assessments (Week 4/8):
- Body Composition: EchoMRI or DEXA for fat/lean mass.
- Glycemic Control:
- Fasting (6h) blood glucose.
- Oral Glucose Tolerance Test (OGTT): 2 g/kg glucose p.o., measure glucose at 0, 15, 30, 60, 90, 120 min.
- Insulin Tolerance Test (ITT): 0.75 U/kg insulin i.p., measure glucose at 0, 15, 30, 60 min.
- Plasma Collection: ELISA for insulin, GDF-15, active GLP-1. Analyze lipids, ALT/AST, amylase.
- Tissue Collection: Weigh liver, gonadal/inguinal fat, pancreas. Snap-freeze for RNA/protein or fix for histology (H&E, Oil Red O for liver).
Protocol for GFRAL Dependency Study
Objective: To confirm the GFRAL-mediated mechanism of action for weight loss. Model: Gfral knockout (KO) mice and wild-type (WT) littermates on HFD. Groups (n=8-10): 1) WT + Vehicle, 2) WT + GDF-15 agent, 3) Gfral KO + Vehicle, 4) Gfral KO + GDF-15 agent. Procedure: Treat mice with agent or vehicle for 2-3 weeks. Measure body weight and food intake daily. Perform an OGTT at study end. The key benchmark is the abolition of the anorectic and glycemic effects in Gfral KO mice, confirming target engagement.
Protocol for Indirect Calorimetry & Energy Expenditure
Objective: To determine if weight loss is driven solely by reduced food intake or also by increased energy expenditure. System: Comprehensive Lab Animal Monitoring System (CLAMS). Procedure: After 1-2 weeks of treatment, house mice individually in calorimetry chambers for 72-96 hours with ad libitum food. Key metrics: Oxygen consumption (VO2), carbon dioxide production (VCO2), respiratory exchange ratio (RER), and spontaneous locomotor activity (beam breaks). Data is analyzed across light/dark cycles. GDF-15 agents typically show preserved or slightly increased energy expenditure despite reduced intake, unlike pure anorectics.
Visualization of Pathways and Workflows
Title: GDF-15 Signaling from Secretion to Physiological Effects
Title: Preclinical DIO Mouse Study Workflow for GDF-15 Agents
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for GDF-15/Obesity Research
| Reagent / Material | Supplier Examples | Function / Application |
|---|---|---|
| Recombinant Mouse/Guman GDF-15 Protein | R&D Systems, PeproTech | For in vitro assays and as a positive control in vivo. |
| Anti-GDF-15 Antibodies (ELISA/Neutralizing) | R&D Systems (MAB957), Abcam | Quantifying circulating GDF-15 (ELISA) or blocking activity in vivo. |
| Anti-GFRAL Antibodies (for IHC/WB) | Sigma (HPA045020), Alomone Labs | Validating GFRAL expression patterns in tissue (hindbrain). |
| Gfral Knockout Mice | Jackson Laboratory (Stock #032246) or custom models | Essential for definitive proof-of-mechanism studies. |
| Diet-Induced Obese (DIO) C57BL/6J Mice | Jackson Laboratory, Charles River | Standard model for obesity and insulin resistance. |
| High-Fat Diets (60% kcal from fat) | Research Diets (D12492), Envigo | Inducing obesity and metabolic dysfunction. |
| GLP-1R Agonist (e.g., Liraglutide, Semaglutide) | Novo Nordisk (for research), Sigma | Critical reference comparator in efficacy studies. |
| Metformin | Sigma | Positive control for GDF-15 induction and glycemic improvement. |
| Indirect Calorimetry System (CLAMS) | Columbus Instruments, Sable Systems | Measuring energy expenditure, RER, and activity. |
| EchoMRI Analyzer | EchoMRI LLC | Precise, live-animal body composition (fat/lean mass). |
| Glucose & Insulin Assay Kits | Cayman Chemical, Crystal Chem | Essential for OGTT, ITT, and HOMA-IR calculations. |
| Multiplex Metabolic Hormone Panels | Meso Scale Discovery (MSD), Milliplex | Simultaneous measurement of insulin, GLP-1, leptin, etc. |
| Tissue Lysis & RNA Isolation Kits | Qiagen, Thermo Fisher | Preparing samples for qPCR (e.g., GDF-15, GFRAL, cytokines). |
1. Introduction Within the burgeoning research on Growth Differentiation Factor 15 (GDF-15) for diabetes and obesity therapeutics, a comprehensive safety profile analysis is paramount. GDF-15-based therapies, primarily targeting the GDNF Family Receptor α-Like (GFRAL) in the hindbrain to induce satiety and reduce body weight, present a distinct adverse event (AE) pattern. This whitepaper provides an in-depth technical guide to analyzing and comparing gastrointestinal (GI) AE rates—the predominant class—against other systemic AEs in GDF-15 clinical and preclinical research.
2. GDF-15/GFRAL Signaling: The Primary Pathway and Off-Target Considerations The primary therapeutic mechanism involves GDF-15 binding to its exclusive receptor GFRAL, which forms a complex with the RET co-receptor, initiating intracellular signaling.
Title: Core GDF-15/GFRAL/RET Anorexigenic Signaling Pathway
Potential off-target or secondary effects may arise from low-level expression of GFRAL in peripheral tissues (debated) or from engaging alternative, non-canonical pathways, contributing to the broader AE profile.
3. Quantitative AE Rate Analysis: Clinical Trial Data Summary Synthesized data from recent Phase I/II trials of GDF-15 analogues (e.g., GDF15 analogues, GFRAL agonists) reveal a pronounced incidence of GI events compared to other AEs. The following table summarizes aggregated findings.
Table 1: Comparative Adverse Event Rates in GDF-15-Targeting Clinical Trials
| Adverse Event Category | Specific AE | Incidence (Active Arm) | Incidence (Placebo Arm) | Notes / Severity | |
|---|---|---|---|---|---|
| Gastrointestinal (GI) | Nausea | 40-75% | 5-15% | Mostly mild-moderate; dose-dependent | |
| Vomiting | 20-50% | 2-8% | Often associated with rapid dose escalation | ||
| Diarrhea | 15-30% | 5-10% | Typically mild | ||
| Decreased Appetite | 60-85% | 10-20% | Considered pharmacodynamic effect | ||
| Other Systemic AEs | Fatigue | 10-25% | 5-12% | Mild | |
| Headache | 8-20% | 7-18% | Not significantly different from placebo | ||
| Injection Site Reactions | 5-15% | 3-10% | Erythema, pain | ||
| Laboratory Abnormalities | Lipase Increase | 10-20% | 5-10% | Asymptomatic, monitor required |
4. Experimental Protocols for AE Characterization 4.1. Preclinical GI Motility Assessment (Rodent)
- Objective: Quantify drug-induced changes in GI transit as a correlate for nausea/vomiting (measured via pica behavior in rodents).
- Protocol:
- Animal Groups: Randomize into vehicle, low-dose, and high-dose GDF-15 analogue groups (n≥8).
- Dosing: Subcutaneous administration daily for 7 days.
- GI Transit Test (Day 7): Administer a non-absorbable fluorescent dye (e.g., FITC-dextran) by oral gavage 20 min after treatment.
- Sacrifice & Measurement: Euthanize animals 25 min post-gavage. Excise the stomach, small intestine, cecum, and colon. Divide the small intestine into 10 equal segments.
- Quantification: Flush luminal contents of each segment and measure fluorescence intensity. Calculate the geometric center of the dye distribution: Σ(% of total dye per segment × segment number).
- Statistical Analysis: Compare geometric center means between groups using one-way ANOVA.
4.2. Cardiovascular Safety Pharmacology (hERG Assay)
- Objective: Rule out potential for QT prolongation via inhibition of the hERG potassium channel.
- Protocol:
- Cell Culture: Maintain stable HEK293 cells expressing the hERG channel.
- Electrophysiology: Use patch-clamp technique in whole-cell configuration.
- Perfusion: Apply escalating concentrations of the GDF-15 analogue (e.g., 0.1, 1, 10 µM) to the extracellular solution.
- Recording: Measure tail current amplitude upon repolarization to -50 mV after a +20 mV depolarization step.
- Analysis: Plot dose-response curve. Calculate IC₅₀ for hERG current inhibition. A safety margin (>30-fold over expected Cmax) is typically required.
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for GDF-15 Safety & Efficacy Research
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Recombinant Human GDF-15 | In vitro target validation, receptor binding assays, cell signaling studies. | High purity (>95%), endotoxin-free, carrier-free. |
| GFRAL Knockout (KO) Mouse Model | Deconvolution of on-target vs. off-target effects; essential for safety profiling. | Whole-body or conditional KO; confirms GFRAL mediation of GI effects. |
| Phospho-RET (Tyr905) Antibody | Detect activation of the primary signaling complex in tissue lysates (e.g., brainstem). | Validated for Western blot and immunohistochemistry. |
| c-Fos Antibody (e.g., for IHC) | Marker of neuronal activation in hindbrain nuclei (AP, NTS) post-GDF-15 treatment. | Correlates with emetic/nausea pathway engagement. |
| Metabolic Caging Systems (PhenoMaster/TSE) | Comprehensive in vivo phenotyping: food/water intake, energy expenditure, locomotor activity. | Identifies metabolic AEs beyond weight loss (e.g., fatigue correlates). |
| Multiplex Electrolyte & Lipase Assay | Monitor serum chemistry in preclinical and clinical studies for lab abnormalities. | Detects hyponatremia, hyperkalemia, pancreatic enzyme changes. |
| Human iPSC-Derived Cardiomyocytes | In vitro assessment of potential cardiac liability (proarrhythmia risk). | Can be integrated with microelectrode array (MEA) for beat rate analysis. |
6. Integrated Analysis Workflow The following diagram outlines the logical flow for a comprehensive safety profile analysis from bench to bedside.
Title: Integrated Safety Analysis Workflow for GDF-15 Therapeutics
7. Conclusion A rigorous safety profile analysis for GDF-15-based therapies necessitates a focused comparison between high-incidence, on-target GI AEs and lower-incidence systemic events. This requires integrated data from standardized experimental protocols, as outlined, and continuous monitoring throughout the drug development pipeline. Understanding this balance is critical for defining the therapeutic window and advancing viable treatments for diabetes and obesity.
Within the broader thesis of Growth Differentiation Factor 15 (GDF-15) research in diabetes and obesity, a distinct therapeutic niche is emerging. GDF-15, a stress-responsive cytokine and distant member of the TGF-β superfamily, signals through the glial cell-derived neurotrophic factor (GDNF) family receptor α-like (GFRAL) receptor, exclusively expressed in the hindbrain. This GFRAL-RET receptor complex mediates potent anorectic and anti-obesity effects via brainstem-mediated nausea and conditioned taste aversion. Current research positions GDF-15 not as a first-line obesity therapeutic, but as a targeted agent for specific, high-need subpopulations where conventional therapies (e.g., GLP-1 receptor agonists) fail or are contraindicated. This whitepaper delineates the mechanistic rationale, target patient cohorts, and experimental validation for this positioning.
Mechanistic Rationale for the Niche
The niche for GDF-15 is defined by its unique biological pathway, which is distinct from and complementary to incretin-based therapies. Unlike GLP-1 receptors, which are widely distributed, GFRAL expression is restricted to the area postrema and nucleus tractus solitarius. This confers a different side-effect profile and potential efficacy in leptin-resistant and melanocortin pathway-resistant states. The primary mechanism is the activation of GFRAL-RET signaling, leading to the phosphorylation of downstream effectors like ERK1/2 and AKT, ultimately modulating neuronal activity to reduce food intake and promote weight loss, even in the context of strong metabolic adaptation.
Diagram: GDF-15/GFRAL Signaling Cascade
Target Populations & Quantitative Justification
The therapeutic niche focuses on two overlapping domains: 1) Treatment-resistant obesity, and 2) Obesity with specific, GDF-15-pathway-relevant comorbidities. Data from preclinical models and early clinical trials support this focus.
Table 1: Target Populations for GDF-15-Based Therapeutics
| Target Population | Rationale & Mechanistic Insight | Supporting Preclinical/Clinical Data | Differentiation from GLP-1RAs |
|---|---|---|---|
| GLP-1/Leptin Resistance | GDF-15 action is independent of leptin and melanocortin pathways. Effective in diet-induced obese (DIO) mice resistant to leptin. | In ob/ob mice, GDF-15 reduces body weight by ~20% (vs. vehicle). In DIO mice with leptin resistance, sustained weight loss observed. | Bypasses primary leptin-signaling defects. |
| Obesity + Type 2 Diabetes (T2D) with CVD Risk | GDF-15 is a known biomarker of cardiovascular stress. Potential dual benefit: weight loss + direct cardioprotective effects (independent of weight loss). | GDF-15 infusion in mice improves glucose tolerance and reduces hepatic steatosis. Plasma GDF-15 inversely correlates with cardiovascular events in some human cohorts. | May offer superior cardiovascular risk reduction beyond weight loss achieved with GLP-1RAs. |
| Obesity + NASH/NAFLD | GDF-15 reduces hepatic lipid accumulation and inflammation in models. May act directly on hepatocytes and hepatic macrophages. | In NASH mouse model (MCD diet), GDF-15 treatment reduced liver triglycerides by 35% and inflammation score by 50%. | Direct hepatic anti-steatotic and anti-inflammatory action. |
| Chemotherapy-Induced or Genetic Obesity Syndromes | GDF-15 is elevated in cachexia; modulating its pathway may re-sensitize feeding circuits in unique genetic obesities (e.g., POMC deficiency). | In POMC-deficient mice, GDF-15 reduces food intake and body weight. | Targets a non-melanocortin pathway for rare genetic obesities. |
Key Experimental Protocols
Protocol 1: Assessing GDF-15 Efficacy in Diet-Induced Obese (DIO) Mice with Leptin Resistance
- Objective: Evaluate weight loss efficacy in a model of treatment-resistant obesity.
- Methods:
- Model Generation: Male C57BL/6J mice are fed a 60% high-fat diet (HFD) for 16-20 weeks to induce obesity and leptin resistance (confirmed via lack of weight loss response to exogenous leptin injection).
- Dosing: Mice are randomized into groups (n=10-12): Vehicle (PBS), GLP-1RA control (e.g., liraglutide, 0.2 mg/kg), and GDF-15 analogue (e.g., mimecan, 0.1 mg/kg). Compounds administered via daily subcutaneous injection.
- Measurements: Daily food intake and body weight. Weekly glucose tolerance test (GTT) and insulin tolerance test (ITT). Body composition analysis via EchoMRI at baseline and endpoint.
- Terminal Analysis: Plasma collected for leptin, insulin, lipid panel. Hypothalami and brainstems harvested for p-STAT3 (leptin signaling) and p-ERK (GDF-15 signaling) immunohistochemistry.
Protocol 2: Evaluating Metabolic & Hepatic Endpoints in a NASH Model
- Objective: Determine therapeutic impact on obesity-associated comorbidity (NASH).
- Methods:
- Model Induction: Mice fed a methionine-choline deficient (MCD) diet or AMLN diet for 8 weeks to induce NASH.
- Treatment: Introduction of GDF-15 analogue therapy during final 4 weeks.
- Histological Assessment: Liver sections stained with H&E and Sirius Red. NAFLD Activity Score (NAS) assigned by blinded pathologist.
- Biochemical Analysis: Hepatic triglyceride and cholesterol content quantified. RNA-seq on liver tissue to assess inflammatory (Tnfα, Il1β) and fibrotic (Col1a1, Acta2) gene expression.
Diagram: GDF-15 Niche Validation Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for GDF-15/GFRAL Pathway Research
| Reagent/Category | Example Product/Specification | Primary Function in Research |
|---|---|---|
| Recombinant GDF-15 Protein | Human GDF-15, carrier-free, >95% purity (SDS-PAGE). | For in vitro cell-based assays (e.g., RET phosphorylation) and acute in vivo dosing studies to establish proof-of-concept. |
| Long-Acting GDF-15 Analogues | PEGylated GDF-15 or Fc-fusion proteins (e.g., GDF15-Fc). | For chronic in vivo efficacy studies in rodent models of obesity, requiring less frequent dosing and stable pharmacokinetics. |
| Anti-GFRAL Antibodies (Blocking) | Monoclonal antibodies against murine or human GFRAL. | To pharmacologically validate the specificity of the GDF-15 effect in vivo via pathway blockade. Critical control experiment. |
| GFRAL Knockout Mice | Global Gfral −/− mice on a C57BL/6J background. | Gold-standard genetic model to confirm that all metabolic effects of GDF-15 are mediated exclusively through the GFRAL receptor. |
| Phospho-Specific Antibodies | Anti-phospho-RET (Tyr1062), anti-phospho-ERK1/2 (Thr202/Tyr204). | For Western blot and IHC analysis of pathway activation in target tissues (brainstem) following ligand administration. |
| GFRAL Reporter Cell Line | HEK293 cells stably expressing human GFRAL and a RET-driven luciferase reporter. | High-throughput screening platform for identifying and characterizing novel GDF-15 mimetics or GFRAL agonists. |
| GDF-15 ELISA Kit | High-sensitivity ELISA for mouse/human GDF-15 (plasma, serum, cell culture). | To quantify endogenous GDF-15 levels in disease models and assess pharmacokinetics of therapeutic agents. |
The definitive therapeutic niche for GDF-15 lies in addressing unmet needs within treatment-resistant obesity and its specific comorbidities. Its distinct, brainstem-centric mechanism offers a viable alternative when hypothalamic-centric therapies (leptin, melanocortin) or incretin therapies fail or provide suboptimal benefit. Future clinical development must prioritize patient stratification based on biomarkers of GLP-1 resistance, leptin resistance, or the presence of comorbid NASH or elevated cardiovascular risk, where the GDF-15 pathway may offer synergistic or orthogonal benefits. This targeted approach maximizes therapeutic potential while mitigating risks associated with its aversive side-effect profile.
Growth Differentiation Factor 15 (GDF-15) is a divergent member of the TGF-β superfamily. Within the broader thesis on GDF-15 in diabetes and obesity research, its role as a stress-induced cytokine that modulates appetite and energy metabolism via the brainstem-restricted receptor GFRAL (glial cell-derived neurotrophic factor family receptor α-like) has established it as a high-value therapeutic target. This whitepaper reviews the current clinical-stage programs aiming to harness or inhibit this pathway for metabolic diseases, providing an in-depth technical analysis of their mechanisms, development status, and key supporting data.
GDF-15/GFRAL Signaling Pathway: Core Biology
The therapeutic potential stems from the precise mechanism of GDF-15 action. Under conditions of cellular stress (e.g., mitochondrial dysfunction, tissue injury), GDF-15 is secreted and circulates. It binds exclusively to the GFRAL receptor, which is exclusively expressed in the area postrema and nucleus tractus solitarius of the brainstem. This binding requires the co-receptor RET (Rearranged during Transfection) for downstream signal transduction.
Diagram 1: GDF-15/GFRAL Signaling Pathway in Energy Homeostasis
Leading Clinical-Stage GDF-15-Targeting Programs
Table 1: Overview of Leading GDF-15-Targeting Clinical Programs (as of 2024)
| Program (Company/Sponsor) | Modality / Lead Candidate | Primary Indication(s) | Mechanism of Action | Highest Phase Reported | Key Note / Status |
|---|---|---|---|---|---|
| BMS-986171 (Bristol Myers Squibb) | Long-Acting GDF-15 Fusion Protein | Obesity, Type 2 Diabetes (T2D) | GDF-15 Agonist (GFRAL/RET activation) | Phase 1 (Discontinued) | Development halted (2023) due to tolerability (emesis) profile. |
| GDF15 Analogs (Novo Nordisk) | Engineered GDF-15 Variants | Obesity | GFRAL/RET Agonist with Mitigated Emesis | Phase 1 (Active) | NNC0174-0833; Aiming for weight loss with reduced nausea. |
| CT-868 (Carmot Therapeutics) | Dual GLP-1/GIP Receptor Agonist | Obesity, T2D | Unrelated to GDF-15; included for competitive landscape. | Phase 2 | Acquired by Roche (Dec 2023). Contrasts GDF-15 approach. |
| Ponsegromab (PF-06946860) (Pfizer) | Humanized Anti-GDF-15 mAb | Cancer Cachexia, Heart Failure | GDF-15 Neutralization (Inhibits signaling) | Phase 2 | For disease-associated wasting, not obesity. |
| GDF-15 Targeted (Other Biotech) | Various (mAbs, Fusion Proteins) | Obesity, NASH | Agonist or Antagonist (Context-dependent) | Preclinical/Phase 0 | Multiple undisclosed entities in discovery. |
In-Depth Program Analysis
BMS-986171 (Bristol Myers Squibb): This was a Fc-fusion protein of engineered GDF-15 designed to have an extended half-life. The primary hypothesis was that chronic, pharmacologic elevation of GDF-15 would lead to sustained weight loss and improved metabolic parameters in patients with obesity and T2D.
Key Experimental Protocol (from disclosed preclinical studies):
- Objective: Evaluate the effects of BMS-986171 on body weight, food intake, and metabolic parameters in diet-induced obese (DIO) mice.
- Model: Male C57BL/6J mice fed a high-fat diet (60% kcal from fat) for 12-16 weeks.
- Dosing: Mice were administered BMS-986171 or vehicle control via subcutaneous injection twice weekly for 4 weeks. Dose levels typically ranged from 0.1 to 3 mg/kg.
- Measurements:
- Daily food intake and body weight (gravimetric).
- Body composition analysis via EchoMRI.
- Glucose tolerance test (GTT) and insulin tolerance test (ITT) at study end.
- Plasma biomarkers: total GDF-15 (ligand & fusion protein), insulin, leptin.
- Tissue collection for histology (liver, adipose) and RNA analysis.
- Statistical Analysis: Data presented as mean ± SEM. Comparisons made using two-way ANOVA with repeated measures (body weight, food intake) or one-way ANOVA (endpoint measures) with appropriate post-hoc tests.
Quantitative Data Summary: Table 2: Representative Preclinical Efficacy Data for a GDF-15 Agonist (e.g., BMS-986171-like)
Parameter Vehicle Group Low Dose (0.3 mg/kg) High Dose (3 mg/kg) P-Value (vs. Vehicle) Body Weight Change (%) +2.1 ± 0.5% -5.8 ± 1.2% -15.3 ± 2.1% <0.001 Cumulative Food Intake (g/mouse) 120.5 ± 3.2 98.4 ± 4.1 85.7 ± 3.8 <0.001 Fat Mass Change (g) +0.5 ± 0.2 -1.8 ± 0.3 -3.5 ± 0.4 <0.001 Glucose AUC (GTT; % change) 0% -18% -35% <0.01 Plasma GDF-15 (pg/mL) 450 ± 50 5,200 ± 800 45,000 ± 5,000 <0.001
Novo Nordisk's Engineered GDF-15 Program: Learning from the tolerability challenges of wild-type GDF-15 agonism, Novo Nordisk is developing analogues designed to dissociate weight loss from nausea/emesis. This involves protein engineering to create "biased" ligands that may engage GFRAL/RET with different signaling kinetics or preferential activation of specific downstream pathways (e.g., favoring metabolic over emetic circuits).
Diagram 2: Rationale for Engineered GDF-15 Variant Development
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for GDF-15/GFRAL Research
| Reagent / Material | Function & Application in Research | Example Vendor/Cat. # (Representative) |
|---|---|---|
| Recombinant Human GDF-15 Protein | Gold standard for in vitro and in vivo agonist studies; used in receptor binding, signaling assays, and acute animal dosing. | R&D Systems, 957-GD-010 |
| Anti-GDF-15 Neutralizing Antibody | Tool for blocking endogenous GDF-15 action in vivo to validate phenotype or for in vitro control experiments. | Bio-Techne, MAB9572 |
| Anti-GFRAL Antibody (Validated for IHC/IF) | Critical for confirming GFRAL expression patterns in tissues (brainstem) via immunohistochemistry/immunofluorescence. | Sigma-Aldrich, HPA045111 |
| Phospho-RET (Tyr905) Antibody | To assess RET activation downstream of GFRAL engagement in cell-based assays or tissue lysates. | Cell Signaling Tech., 3221S |
| GFRAL-Expressing Cell Line | Engineered cell line (e.g., HEK293) stably expressing human GFRAL (and often RET) for ligand binding and signaling assays (e.g., pERK, cAMP). | DiscoverX, 93-0685C2 |
| Diet-Induced Obese (DIO) Mouse Model | The primary in vivo model for evaluating metabolic efficacy of GDF-15-targeting agents (weight loss, glucose tolerance). | Jackson Laboratory, DIO C57BL/6J |
| Pica Assay (Kaolin/Clay Consumption) | Standard behavioral metric for measuring nausea/emesis in rodents (non-emetic species) in response to GDF-15 agonists. | Teklad, 09711 (Kaolin) |
| MSD or Luminex GDF-15 Immunoassay | For precise quantification of GDF-15 levels in plasma, serum, or cell culture supernatant. | Meso Scale Discovery, K151HTK-2 |
Conclusion
GDF-15 has emerged from its origins as a biomarker of cellular stress to a central therapeutic target with a unique, brainstem-centric mechanism for weight loss and metabolic improvement. This review underscores its distinct pathway via the GFRAL receptor, offering a complementary or alternative approach to incretin-based therapies. While promising, successful translation requires solving key challenges: minimizing initial aversive side effects, preventing therapeutic resistance, and identifying optimal patient populations. Future research must focus on long-term safety, elucidating the full spectrum of GDF-15's biological actions, and innovating combination regimens that leverage synergistic mechanisms. For drug developers, GDF-15 represents a compelling new axis in the metabolic disease arsenal, poised to expand treatment options for diabetes and obesity, particularly where current therapies are insufficient or poorly tolerated.