A Practical Guide to ELISA Biomarker Validation: From Protocol Optimization to Clinical Acceptance
This article provides a comprehensive, up-to-date guide for researchers and drug development professionals on using ELISA for robust biomarker validation.
A Practical Guide to ELISA Biomarker Validation: From Protocol Optimization to Clinical Acceptance
Abstract
This article provides a comprehensive, up-to-date guide for researchers and drug development professionals on using ELISA for robust biomarker validation. It covers fundamental principles and assay selection, details critical methodological steps and best practices for precise quantification, addresses common troubleshooting scenarios and optimization strategies, and discusses validation criteria, comparative performance against newer technologies, and the path to clinical acceptance. The guide synthesizes current industry standards to bridge the gap between research discovery and reliable clinical application.
Understanding ELISA Fundamentals: Choosing the Right Assay for Your Biomarker
What is ELISA? Core Principles and Evolution for Quantitative Analysis.
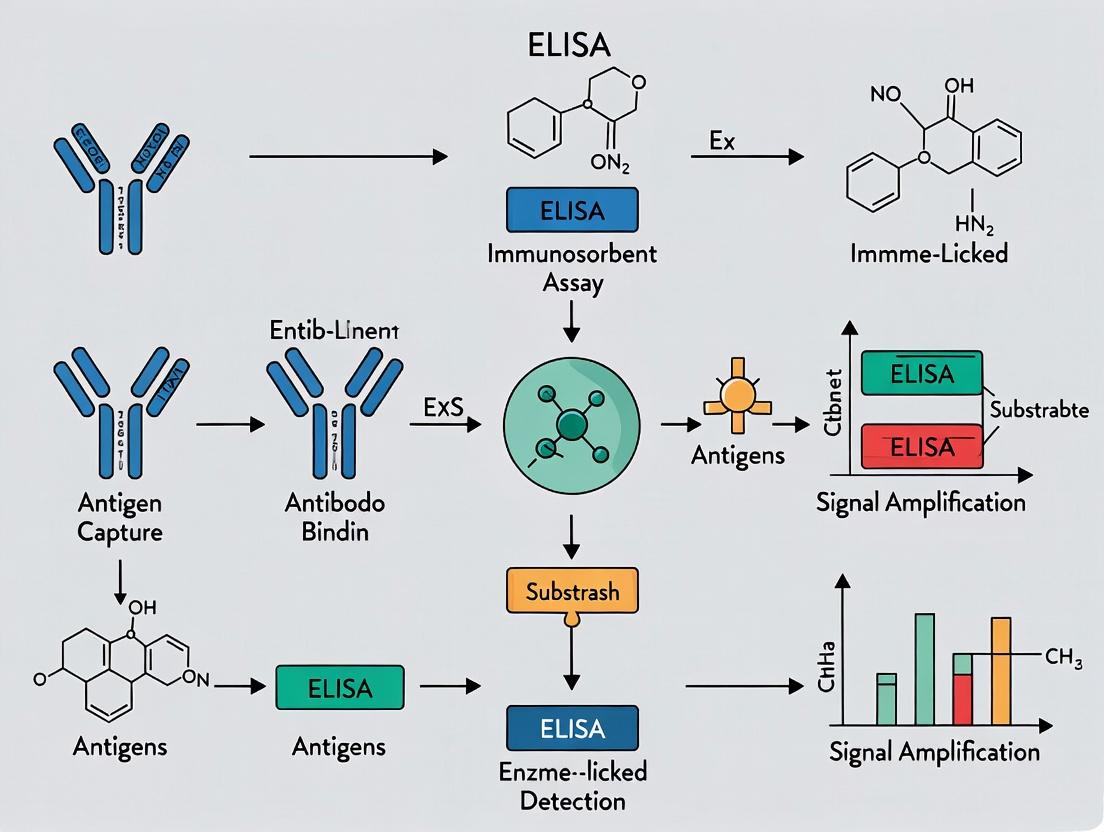
Within the critical framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) stands as a foundational pillar. This technique's unparalleled specificity and sensitivity for detecting and quantifying antigens or antibodies make it indispensable for confirming biomarker presence, concentration, and dynamics in complex biological matrices. This whitepaper details the core principles, evolutionary advancements, and rigorous protocols that establish ELISA as a gold standard for quantitative analysis in drug development and clinical research.
Core Principles and Mechanism
ELISA is an immunological plate-based assay that leverages the specificity of antibody-antigen binding coupled with an enzyme-mediated colorimetric (or other) signal amplification system for detection. The fundamental components include a solid-phase surface (typically a polystyrene microplate), a capture molecule (antibody or antigen), a detection antibody conjugated to an enzyme (e.g., Horseradish Peroxidase, Alkaline Phosphatase), and a chromogenic substrate.
The core principle involves immobilizing one component of the immuno-complex, followed by sequential binding and wash steps to isolate the specific interaction. The attached enzyme catalyzes the conversion of a substrate into a measurable product, with signal intensity directly proportional to the target analyte concentration in the sample.
Evolution for Quantitative Analysis
ELISA has evolved significantly from its initial qualitative applications to a highly quantitative tool.
Key Evolutionary Milestones:
- Homogeneous vs. Heterogeneous: Development of heterogeneous (requires wash steps) assays vastly improved specificity and sensitivity over early homogeneous formats.
- Signal Amplification: Introduction of biotin-streptavidin systems (see diagram below) and enzymatic amplification cycles increased sensitivity to the femtomolar range.
- Detection Modalities: Shift from colorimetric to chemiluminescent and electrochemical detection expanded the dynamic range and lowered detection limits.
- Multiplexing: Advent of planar and bead-based multiplex ELISA (e.g., Luminex) enabled concurrent quantification of dozens of biomarkers in a single sample.
- Automation & Digital Integration: Full automation of liquid handling, washing, and data analysis has enhanced reproducibility, throughput, and integration with Laboratory Information Management Systems (LIMS).
Experimental Protocols: Key Methodologies
Protocol 1: Sandwich ELISA for Cytokine Quantification
Objective: Quantify IL-6 concentration in human serum. Principle: A "capture" antibody specific to IL-6 is coated onto the plate. Serum samples containing IL-6 are added and bind. A second, enzyme-linked "detection" antibody binds to a different epitope on the captured IL-6, forming a "sandwich."
Detailed Steps:
- Coating: Dilute capture antibody in carbonate/bicarbonate coating buffer (pH 9.6) to 2-4 µg/mL. Add 100 µL/well to a 96-well plate. Seal and incubate overnight at 4°C.
- Washing: Aspirate and wash plate 3 times with 300 µL/well of PBS containing 0.05% Tween-20 (PBST).
- Blocking: Add 200 µL/well of blocking buffer (e.g., 5% BSA in PBS or 1% Casein). Incubate for 1-2 hours at room temperature (RT). Wash 3x with PBST.
- Sample & Standard Addition: Prepare a serial dilution of recombinant IL-6 standard in sample diluent. Add 100 µL of standards and pre-diluted serum samples per well. Incubate 2 hours at RT. Wash 3-5x.
- Detection Antibody Addition: Add 100 µL/well of biotinylated anti-IL-6 detection antibody (diluted per manufacturer's recommendation). Incubate 1-2 hours at RT. Wash 3-5x.
- Enzyme Conjugate Addition: Add 100 µL/well of Streptavidin-HRP conjugate (typically 1:5000-1:10000 dilution). Incubate 30 minutes at RT in the dark. Wash 3-5x.
- Substrate Addition: Add 100 µL/well of TMB (3,3',5,5'-Tetramethylbenzidine) substrate. Incubate for 5-30 minutes at RT in the dark.
- Stop Reaction & Readout: Add 50 µL/well of stop solution (e.g., 1M H₂SO₄). Immediately measure absorbance at 450 nm (reference 570/620 nm) using a microplate reader.
Protocol 2: Competitive ELISA for Small Molecule Detection
Objective: Quantify a hapten (e.g., digoxin) in patient plasma. Principle: Sample antigen and a fixed amount of enzyme-labeled antigen compete for binding to a limited number of immobilized antibody sites. Signal is inversely proportional to analyte concentration.
Detailed Steps:
- Coating: Coat plate with anti-digoxin antibody (2 µg/mL) as in Protocol 1, Step 1-3.
- Competitive Incubation: Pre-mix a constant concentration of digoxin-HRP conjugate with serial dilutions of digoxin standard or patient plasma samples. Add 100 µL of these mixtures to the washed, blocked plate. Incubate 1-2 hours at RT.
- Washing: Wash plate 5x thoroughly to remove unbound conjugate.
- Substrate & Readout: Proceed with TMB substrate addition, stop, and reading as in Protocol 1, Steps 7-8.
Data Presentation: Comparative Analysis of ELISA Formats
Table 1: Characteristics of Major ELISA Formats for Biomarker Quantification
| Format | Principle | Best For | Advantages | Key Consideration for Biomarker Research |
|---|---|---|---|---|
| Direct | Antigen coated; direct enzyme-antibody conjugate. | High-concentration antigens, antibody screening. | Speed, minimal steps. | Lower sensitivity; no signal amplification. |
| Indirect | Antigen coated; primary then enzyme-secondary antibody. | Antibody titer determination (serology). | Signal amplification via secondary Ab; flexible. | Potential cross-reactivity from secondary Ab. |
| Sandwich | Capture antibody, antigen, enzyme-detection antibody. | Complex samples (serum, CSF) with low [analyte]. | High specificity (two Abs), high sensitivity. | Requires two non-competing epitopes. |
| Competitive | Analyte & labeled analyte compete for limited Ab sites. | Small molecules (haptens), degraded antigens. | Robust for complex matrices; measures small analytes. | Inverse curve; dynamic range optimization critical. |
Table 2: Evolution of ELISA Detection Systems
| System | Enzyme Example | Substrate | Detection Mode | Approx. Sensitivity | Dynamic Range |
|---|---|---|---|---|---|
| Colorimetric | Horseradish Peroxidase (HRP) | TMB, ABTS | Absorbance (405-450 nm) | pg/mL | 1-2 logs |
| Chemiluminescent | HRP, Alkaline Phosphatase (AP) | Luminol, dioxetane | Light Emission (RLU) | fg-pg/mL | 3-5 logs |
| Electrochemilum. | Ruthenium chelate | Tripropylamine | Electrical Signal | fg/mL | >5 logs |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in ELISA | Critical Considerations for Validation |
|---|---|---|
| Microplate | Solid phase for immobilization. | Material (PS, PVDF); binding capacity; well-to-well uniformity. |
| Capture & Detection Antibodies | Provide assay specificity. | Must target different, non-competing epitopes (sandwich); validate pair. |
| Blocking Buffer | Prevents non-specific binding. | Optimize (BSA, casein, serum); must not interfere with antibodies. |
| Detection Enzyme | Signal generation (HRP, AP). | Conjugate purity and specific activity; stability. |
| Signal Amplification System | Enhances sensitivity (Biotin-Streptavidin). | Multi-biotin antibodies and streptavidin-polymer conjugates common. |
| Chromogenic/Chemilum. Substrate | Enzyme substrate for readout. | Stability, signal-to-noise ratio, linear range of detection. |
| Plate Washer | Removes unbound material. | Consistency, precision, and completeness of washing are critical. |
| Microplate Reader | Quantifies signal output. | Requires appropriate filters/wavelengths for chosen detection mode. |
| Reference Standard | Calibrates the assay. | Must be highly purified and internationally traceable for validation. |
Within the critical framework of biomarker validation research, the selection of an appropriate Enzyme-Linked Immunosorbent Assay (ELISA) format is a foundational decision that dictates the success, specificity, and sensitivity of quantitation. This technical guide provides an in-depth analysis of the four core ELISA formats—Direct, Indirect, Sandwich, and Competitive—framed within the thesis that meticulous method alignment with target analyte and research context is paramount for generating robust, reproducible data in drug development.
Core Principles and Comparative Analysis
Each ELISA format is distinguished by its antigen-antibody configuration, detection strategy, and consequent suitability for specific target types.
Table 1: Comparative Overview of Core ELISA Formats
| Format | Antigen Type | Key Steps | Primary Advantages | Primary Limitations | Best For |
|---|---|---|---|---|---|
| Direct | Immobilized antigen | 1. Antigen coat2. Enzyme-conjugated primary Ab detection3. Substrate addition | Fast, minimal steps, low cross-reactivity | Low signal, every primary Ab must be conjugated, less flexible | High-abundance antigens, screening monoclonal Ab clones |
| Indirect | Immobilized antigen | 1. Antigen coat2. Primary Ab binding3. Enzyme-conjugated secondary Ab detection4. Substrate addition | High sensitivity (signal amplification), flexible primary Ab use | More steps, potential for cross-reactivity from secondary Ab | General antibody detection (e.g., serology), immunogenicity assays |
| Sandwich | Immobilized capture Ab | 1. Capture Ab coat2. Antigen binding3. Detection Ab binding4. Enzyme-conjugated secondary Ab detection*5. Substrate addition | Very high specificity & sensitivity, works well with complex samples | Requires two non-competing Abs for distinct epitopes | Complex samples, low-abundance biomarkers (cytokines, hormones) |
| Competitive | Immobilized antigen | 1. Sample antigen + labeled antigen compete for limited primary Ab2. Transfer to coated antigen well3. Substrate addition | Measures small antigens, robust with impure samples, less susceptible to sample matrix effects | Inverse signal relationship, narrower dynamic range | Small molecules (haptens), drugs, peptides |
Step 3-4: Detection can be direct if detection Ab is pre-conjugated.*Alternative: Immobilized antibody format also common.
Table 2: Typical Performance Characteristics (Generalized Ranges)
| Format | Typical Sensitivity Range | Dynamic Range (Log) | Assay Time | Sample Volume Required | Cost per Sample |
|---|---|---|---|---|---|
| Direct | Moderate (ng/mL) | 2-3 | Shortest (~2-3 hrs) | Low | Low |
| Indirect | High (pg/mL - ng/mL) | 3-4 | Moderate (~3-4 hrs) | Moderate | Low-Moderate |
| Sandwich | Very High (pg/mL) | 3-4 | Long (~4-5 hrs) | Low-Moderate | High |
| Competitive | Moderate-High (pg/mL - ng/mL) | 2-3 | Moderate (~3-4 hrs) | Moderate | Moderate |
Selection Algorithm and Strategic Application
The optimal format is determined by target analyte characteristics, available reagents, and required assay performance.
Title: ELISA Format Selection Decision Tree
Detailed Experimental Protocols
Protocol 1: Sandwich ELISA for Cytokine Biomarker Quantitation
This protocol is foundational for validating soluble protein biomarkers in serum or cell culture supernatant.
Key Reagents:
- Coating Buffer: 0.2 M Carbonate-Bicarbonate, pH 9.4.
- Wash Buffer: PBS with 0.05% Tween-20 (PBST).
- Blocking Buffer: 1-5% BSA or 5% non-fat dry milk in PBST.
- Recombinant Cytokine Standard.
- Matched Antibody Pair: Capture mAb and biotinylated detection mAb.
- Streptavidin-Horseradish Peroxidase (HRP) conjugate.
- Substrate: TMB (3,3',5,5'-Tetramethylbenzidine).
- Stop Solution: 1M H2SO4 or 1M HCl.
Procedure:
- Coating: Dilute capture antibody in coating buffer. Add 100 µL/well to a 96-well microplate. Seal and incubate overnight at 4°C.
- Washing: Aspirate and wash plate 3x with >300 µL/well of wash buffer using a plate washer or multichannel pipette. Blot dry on lint-free paper.
- Blocking: Add 300 µL/well of blocking buffer. Incubate for 1-2 hours at room temperature (RT). Wash as in step 2.
- Sample & Standard Addition: Prepare serial dilutions of the standard in assay diluent (e.g., blocking buffer). Add 100 µL of standard or sample per well in duplicate/triplicate. Incubate for 2 hours at RT or overnight at 4°C. Wash.
- Detection Antibody: Add 100 µL/well of optimally diluted biotinylated detection antibody. Incubate 1-2 hours at RT. Wash.
- Enzyme Conjugate: Add 100 µL/well of streptavidin-HRP at recommended dilution. Incubate 30 minutes at RT in the dark. Wash.
- Signal Development: Add 100 µL/well of TMB substrate. Incubate in the dark for 5-30 minutes until color develops.
- Stop Reaction: Add 50-100 µL/well of stop solution. Read absorbance immediately at 450 nm (with 540-570 nm reference).
Title: Sandwich ELISA Step-by-Step Workflow
Protocol 2: Competitive ELISA for Small Molecule Drug Monitoring
This protocol is essential for quantifying small molecules (e.g., therapeutic drugs, hormones) where only one antibody is available.
Key Reagents:
- Drug-Protein Conjugate (for plate coating).
- Anti-Drug Antibody (primary).
- Drug Standard (unlabeled, for competition).
- HRP-conjugated Anti-Species Secondary Antibody (for indirect detection) or HRP-conjugated Drug Analog (for direct detection).
- Substrate and Stop Solution.
Procedure (Indirect Detection Format):
- Coating: Coat plate with 100 µL/well of drug-protein conjugate (e.g., drug-BSA) overnight at 4°C.
- Blocking: Wash, then block with 300 µL/well of blocking buffer for 1-2 hours at RT. Wash.
- Competition: Pre-mix a constant concentration of primary antibody with serial dilutions of the drug standard or sample. Incubate for 1 hour at RT to allow competition.
- Transfer & Binding: Transfer 100 µL of each antibody-drug mixture to the coated plate. Incubate 1 hour at RT. Free antibody binds to immobilized drug. Wash.
- Detection: Add HRP-conjugated secondary antibody. Incubate 1 hour at RT. Wash.
- Development & Readout: Add substrate, stop, and read. Signal is inversely proportional to drug concentration in the sample.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential ELISA Materials and Their Functions
| Reagent/Material | Primary Function | Critical Considerations |
|---|---|---|
| High-Binding Microplates (e.g., Polystyrene) | Solid-phase support for immobilizing proteins or antibodies via passive adsorption. | Uniform well geometry is essential for consistent optical density (OD) readings. |
| Matched Antibody Pair (Capture & Detection) | Core reagents for Sandwich ELISA; ensure specific and sensitive target recognition. | Must bind distinct, non-overlapping epitopes. Require rigorous cross-reactivity testing. |
| Recombinant Protein Standard | Provides a known concentration curve for absolute target quantitation. | Should be highly pure and biologically active. Source (e.g., mammalian vs. E. coli) can affect antibody recognition. |
| Biotin-Streptavidin System | Signal amplification system. Biotin on detection Ab binds multiple streptavidin-enzyme conjugates. | Offers significant sensitivity gain over direct secondary antibody conjugation. |
| HRP or AP Enzyme Conjugates | Catalyzes substrate conversion to detectable colored (chromogenic) or luminescent product. | HRP is more common; Alkaline Phosphatase (AP) is more stable but slower. |
| Chromogenic Substrate (e.g., TMB, OPD) | Enzyme substrate that produces a soluble colored product measurable by absorbance. | TMB is most common (450 nm read). Requires acid stop, which also stabilizes signal. |
| ELISA Diluent/Blocking Buffer | Reduces non-specific binding by occupying leftover protein-binding sites on the plate. | Must be optimized (BSA, casein, serum). Should match sample matrix when possible. |
| Precision Plate Washer | Removes unbound reagents between steps, critical for reducing background noise. | Automated systems provide reproducibility; manual washing requires careful technique. |
| Microplate Reader (Spectrophotometer) | Measures absorbance of developed color in each well across defined wavelengths. | Must be capable of reading at substrate-specific wavelengths (e.g., 450 nm for TMB). |
Within the framework of ELISA (Enzyme-Linked Immunosorbent Assay) principles for biomarker validation research, the selection and optimization of core reagents are non-negotiable determinants of success. The assay's sensitivity, specificity, reproducibility, and quantitative accuracy hinge on the precise function and quality of four fundamental reagent classes: Antibodies, Conjugates, Substrates, and Standards. This whitepaper provides an in-depth technical guide to these reagents, placing their function and characterization within the critical context of generating robust, validated data for drug development and clinical research.
Antibodies: The Primary Engines of Specificity
Antibodies are the foundation of ELISA, providing the molecular recognition essential for capturing and detecting the target biomarker. For biomarker validation, the choice between monoclonal and polyclonal antibodies is strategic.
- Monoclonal Antibodies (mAbs): Produced by a single B-cell clone, they recognize a single, specific epitope. This ensures high specificity and lot-to-lot consistency, critical for quantitative validation assays. However, they may be sensitive to minor changes in the epitope structure.
- Polyclonal Antibodies (pAbs): A mixture of antibodies from multiple B-cell clones, recognizing multiple epitopes on the same antigen. This often increases assay sensitivity and robustness against epitope variation but at the cost of potential cross-reactivity and variable lot composition.
Critical Validation Parameters:
- Affinity & Avidity: High-affinity antibodies (low K_D, typically ≤10^-9 M) are essential for sensitive detection of low-abundance biomarkers.
- Specificity: Must be rigorously confirmed against related proteins, isoforms, and sample matrix components to avoid false positives.
- Cross-Reactivity: Should be ≤1% against key homologous targets, as validated by Western blot or multiplex immunoassays.
Table 1: Comparative Analysis of Antibody Types for ELISA
| Parameter | Monoclonal Antibody | Polyclonal Antibody |
|---|---|---|
| Epitope Recognition | Single, defined epitope | Multiple, diverse epitopes |
| Specificity | Very High | Moderate to High |
| Sensitivity | Can be high with optimal pairing | Typically high due to multi-epitope binding |
| Lot-to-Lot Consistency | Excellent | Variable |
| Production & Cost | High cost, immortalized cell line | Lower cost, animal immunizations |
| Ideal Use Case | Quantitative, validated assays; paired detection systems | Capture antibodies; detection of denatured or variable antigens |
Conjugates: The Signal-Generating Link
Conjugates are detection antibodies or streptavidin chemically linked to an enzyme reporter. This linkage must be stable and not impair the binding function of the antibody or the catalytic activity of the enzyme.
Common Enzyme Reporters:
- Horseradish Peroxidase (HRP): Small size (44 kDa), high turnover rate, but sensitive to azide and thiol inhibitors.
- Alkaline Phosphatase (AP): Larger (140 kDa), robust but slower, requires specific buffer (e.g., Tris) for optimal activity.
Conjugation Methods:
- Periodate Oxidation (for HRP): Oxidizes sugar residues on HRP to aldehydes, which then react with antibody amine groups.
- Glutaraldehyde Cross-linking: A two-step protocol linking amine groups on both the enzyme and antibody.
- Maleimide-Thiol Coupling: Site-specific conjugation using engineered thiol groups on the antibody, improving homogeneity.
Experimental Protocol: HRP Conjugation via Periodate Oxidation
- Dialyze 5 mg of purified antibody against 0.01 M carbonate buffer, pH 9.5, at 4°C overnight.
- Dissolve 8 mg HRP in 1 mL deionized water. Add 0.2 mL of 0.1 M NaIO₄, stir for 20 min at room temperature (RT) in the dark.
- Dialyze the activated HRP against 1 mM acetate buffer, pH 4.4, at 4°C overnight.
- Adjust the oxidized HRP pH to 9.5 with 0.2 M carbonate buffer. Immediately mix with the dialyzed antibody.
- Incubate for 2 hours at RT with gentle stirring.
- Add 0.1 mL of fresh NaBH₄ solution (4 mg/mL) and incubate for 2 hours at 4°C.
- Purify the conjugate via size-exclusion chromatography (e.g., Sephadex G-25) in PBS. Store with 1% BSA at 4°C or -20°C.
Substrates: Amplifying the Signal
Substrates are converted by the enzyme conjugate into a measurable signal (colorimetric, chemiluminescent, or fluorescent). The choice dictates the assay's dynamic range and sensitivity.
Table 2: Key Characteristics of Common ELISA Substrates
| Substrate Type | Enzyme | Output Signal | Detection Limit | Dynamic Range | Key Advantage |
|---|---|---|---|---|---|
| TMB (3,3',5,5'-Tetramethylbenzidine) | HRP | Colorimetric (Blue->Yellow) | Moderate (~pg/mL) | ~2 logs | Safe, soluble, good for kinetic reads |
| OPD (o-Phenylenediamine dihydrochloride) | HRP | Colorimetric (Orange) | Moderate | ~2 logs | High molar absorptivity |
| PNPP (p-Nitrophenyl Phosphate) | AP | Colorimetric (Yellow) | Moderate | ~2 logs | Simple, single-component |
| Enhanced Chemiluminescent (e.g., Luminol/H2O2) | HRP | Light Emission (Luminescence) | High (fg-pg/mL) | ~3-4 logs | Highest sensitivity, wide dynamic range |
| ATTOPHOS / 4-MUP | AP | Fluorescence | High | ~3-4 logs | Sensitive, stable signal |
Standards: The Linchpin of Quantification
Accurate biomarker quantification is impossible without a well-characterized standard. The standard curve defines the relationship between signal and analyte concentration.
Critical Attributes of a Validated Standard:
- Matrix Matching: The standard should be diluted in a matrix that closely mimics the sample (e.g., 1% BSA/PBS for serum assays) to correct for background interference.
- Purity & Identity: >95% purity, confirmed by SDS-PAGE and mass spectrometry.
- Stability: Lyophilized standards are preferred for long-term stability; reconstituted aliquots must be stored per validated conditions.
- Traceability: Should be referenced to an internationally recognized material when available (e.g., WHO IS).
Experimental Protocol: Standard Curve Preparation and Validation
- Reconstitution: Reconstitute the lyophilized protein standard in the specified buffer. Vortex gently and allow to equilibrate for 15 minutes.
- Serial Dilution: Perform a 1:2 or 1:3 serial dilution series in the designated matrix (e.g., assay buffer/1% BSA) to span the expected dynamic range of the assay. Use low-protein-binding tubes.
- Plate Layout: Run the standard curve in duplicate or triplicate on every assay plate to control for inter-plate variability.
- Curve Fitting: Fit the signal (O.D. or RLU) vs. concentration using a 4- or 5-parameter logistic (4PL/5PL) model, which best handles the non-linear sigmoidal response of ELISA.
- QC Parameters: The curve's R² should be >0.99. Back-calculated standard concentrations should be within 20% of the expected value (15% for the lower limit of quantification, LLOQ).
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Robust ELISA Development
| Reagent / Material | Function & Purpose in ELISA |
|---|---|
| High-Affinity Matched Antibody Pair | Monoclonal antibodies targeting non-overlapping epitopes for specific capture and detection. |
| Validated Protein Standard | Pure, quantitated antigen for generating the standard curve and assigning concentration values to unknown samples. |
| HRP or AP Conjugated Detection Antibody | Generates the measurable signal via enzyme-substrate reaction. |
| High-Sensitivity Chemiluminescent Substrate | Maximizes signal-to-noise ratio and extends the dynamic range for low-abundance biomarker detection. |
| Low-Binding Microplates (e.g., C8, C18 Greiner) | Minimizes non-specific protein adsorption, improving sensitivity and precision. |
| Blocking Buffer (e.g., 3-5% BSA or Casein) | Saturates unbound sites on the plate surface to prevent non-specific binding of reagents. |
| Wash Buffer with Surfactant (e.g., PBS + 0.05% Tween-20) | Removes unbound reagents while minimizing well-to-well cross-contamination. |
| Sample Diluent (Matrix-Matched) | Preserves antigen integrity and minimizes matrix effects during sample dilution. |
Visualizing ELISA Workflows and Relationships
Within the critical framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technology. The transition from a detectable analyte to a validatable biomarker hinges on the rigorous assessment of specific analytical characteristics. This guide delineates these core characteristics, providing methodologies for their evaluation within the context of ELISA-based validation.
Fundamental Analytical Characteristics of a Validatable Biomarker Assay
For an assay to be considered valid for biomarker quantification in complex biological matrices (e.g., serum, plasma, cerebrospinal fluid), it must demonstrate proficiency across the following parameters.
Table 1: Core Analytical Characteristics for Biomarker Assay Validation
| Characteristic | Definition | Acceptance Criterion (Typical) |
|---|---|---|
| Accuracy | The closeness of agreement between measured value and true value. | Mean bias within ±20% (±25% at LLOQ). |
| Precision | The closeness of agreement between independent measurements. | CV ≤20% (≤25% at LLOQ). |
| Lower Limit of Quantification (LLOQ) | The lowest analyte concentration quantified with acceptable accuracy and precision. | Signal ≥5x signal of blank (S/N ≥5). |
| Upper Limit of Quantification (ULOQ) | The highest analyte concentration quantified with acceptable accuracy and precision. | Defined by the standard curve's linear range. |
| Linearity & Range | The ability to produce results proportional to analyte concentration within a given range. | R² ≥0.99 for calibration curve. |
| Specificity/Selectivity | The ability to measure analyte unequivocally in the presence of interfering components. | Recovery within 80-120% in spiked matrix. |
| Dilutional Linearity | Accuracy of measured analyte concentration after matrix dilution. | Recovery within 80-120% after dilution. |
| Stability | Analytic integrity under specified conditions (freeze-thaw, benchtop, long-term). | Recovery within 80-120% of baseline. |
Detailed Experimental Protocols for ELISA-Based Validation
Protocol for Assessing Accuracy and Precision
Objective: To determine intra-assay (within-run) and inter-assay (between-run) precision and accuracy. Methodology:
- Prepare Quality Control (QC) samples at Low, Mid, and High concentrations across the expected range in the relevant biological matrix.
- For intra-assay precision/accuracy, analyze each QC level in a minimum of 5 replicates within a single assay run.
- For inter-assay precision/accuracy, analyze each QC level in duplicate across a minimum of 3 independent assay runs performed on different days.
- Calculate the mean observed concentration, standard deviation (SD), and coefficient of variation (%CV) for each level.
- Calculate accuracy as percentage recovery: (Mean Observed Concentration / Nominal Concentration) x 100%.
Protocol for Determining LLOQ
Objective: To establish the lowest concentration distinguishable from zero with defined accuracy and precision. Methodology:
- Prepare a series of low-concentration samples by serially diluting the analyte in the matrix of interest.
- Analyze a minimum of 6 replicates of each low-concentration sample and a matrix blank.
- The LLOQ is the lowest concentration where:
- The signal is at least 5 times the mean signal of the blank (Signal-to-Noise ≥5).
- The analyte recovery is within 80-120% of nominal.
- The precision (%CV) is ≤25%.
Protocol for Evaluating Specificity/Selectivity
Objective: To assess interference from matrix components or structurally similar molecules. Methodology:
- Prepare samples by spiking the analyte at known concentrations (Low and High QC) into at least 10 individual lots of the biological matrix (e.g., from 10 different donors).
- Analyze all samples and calculate the measured concentration for each.
- Assess recovery for each individual lot and calculate the overall mean recovery and CV.
- Cross-reactivity Test: Spike potential interfering substances (e.g., homologous proteins, common metabolites) at high concentrations into the analyte sample. Measure response compared to analyte-only control.
Visualization of Core Concepts
Title: Path to a Validated Biomarker Assay
Title: ELISA Biomarker Assay Development and Validation Cycle
The Scientist's Toolkit: Essential Reagents & Materials for ELISA Validation
Table 2: Key Research Reagent Solutions for Biomarker ELISA Validation
| Item | Function in Validation |
|---|---|
| High-Quality Capture & Detection Antibodies | Ensure assay specificity and sensitivity. Must be characterized for minimal cross-reactivity. |
| Recombinant/Purified Target Antigen | Serves as the standard for calibration curve generation and QC sample preparation. |
| Matrix-Matched Diluent | Diluent formulated with "blank" matrix (e.g., charcoal-stripped serum) to maintain sample integrity. |
| Biological Matrix from Multiple Donors | Used for selectivity testing to account for individual variability. |
| Validated ELISA Substrate (e.g., TMB, ECL) | Provides stable, detectable signal proportional to analyte concentration. |
| Precision Microplate Washer & Reader | Essential for reproducible liquid handling and accurate optical density/ luminescence measurement. |
| Stability-Tested QC Samples | Pre-aliquoted samples at defined concentrations for monitoring inter-assay performance. |
| Plate Sealers & Low-Binding Microtubes | Prevent evaporation and non-specific adsorption of analyte, critical for accuracy at low concentrations. |
In the structured pathway of biomarker validation, the pre-analytical and analytical phases are paramount. This guide, framed within the broader thesis that rigorous ELISA (Enzyme-Linked Immunosorbent Assay) principles form the bedrock of reliable biomarker data, details the critical first step: a systematic assessment of biomarker suitability and pre-validation feasibility. This stage determines whether a candidate biomarker possesses the inherent characteristics and supporting evidence to justify the significant investment in full, fit-for-purpose assay validation.
Core Assessment Criteria & Quantitative Benchmarks
A feasibility assessment must evaluate multiple, interlinked domains. Quantitative data from recent literature and guidelines are summarized below.
Table 1: Key Assessment Criteria for Biomarker Feasibility
| Assessment Domain | Key Questions | Quantitative Benchmarks / Indicators |
|---|---|---|
| Biological & Clinical Rationale | Is the biomarker's role in the pathophysiology well-defined? Is there a clear linkage to the clinical endpoint? | Strong association in preclinical models (e.g., p < 0.01, effect size > 2); Supporting evidence from ≥2 independent -omics studies (GWAS, proteomics). |
| Biomarker Physicochemical & Kinetic Properties | Is the molecule stable in the intended matrix? What is its expected concentration range and kinetics? | In vitro stability in matrix: <20% degradation over 24h at 4°C. Expected physiological range spanning 3-4 orders of magnitude (e.g., pg/mL to ng/mL). Half-life relevant to sampling schedule. |
| Matrix & Pre-Analytical Factors | What is the impact of sample collection, processing, and storage? | CV from pre-analytical variables (e.g., freeze-thaw, time-to-centrifugation) should be <15%. Documented stability in intended storage conditions (-80°C) for ≥6 months. |
| Analytical Detectability | Can the biomarker be reliably detected and measured in the target matrix with available tools? | Signal in target matrix ≥3x above assay's Lower Limit of Detection (LLOD). Spike-and-recovery rates of 80-120%. Parallelism (dilutional linearity) with R² > 0.95. |
| Reagent & Tool Availability | Are specific, high-affinity binders (antibodies) available or developable? | Antibody affinity (KD) ≤ 1 nM for sandwich ELISA. Minimal cross-reactivity (<5%) with homologous family members. Commercial availability or credible development timeline (6-12 months). |
| Regulatory & Ethical Path | Are there intellectual property constraints? Is sample availability from well-characterized cohorts feasible? | Clear IP landscape for commercial use. Access to ≥50 pilot samples per relevant clinical group from ethically approved biobanks. |
Experimental Protocols for Pre-Validation Feasibility
The following core experiments, grounded in ELISA methodology, generate the data required for Table 1.
Protocol 3.1: Preliminary Analytical Detectability & Matrix Interference
- Objective: To confirm the biomarker is detectable in the target biological matrix (e.g., serum, plasma, CSF) and assess matrix effects.
- Materials: Candidate ELISA kit or reagent pair (capture/detection antibodies), target matrix samples (at least 5 individual donor pools), appropriate biomarker standard.
- Method:
- Matrix Spike & Recovery: Prepare samples spiked with known concentrations of recombinant biomarker at low, mid, and high levels within the expected range. Include a standard curve diluted in assay buffer (not matrix).
- Parallelism/Dilutional Linearity: Serially dilute a high-concentration native matrix sample (expected to contain the biomarker) with the assay buffer.
- Run all samples in a singlicate or duplicate on the same ELISA plate per manufacturer's protocol.
- Calculate recovery (%) for spiked samples: (Observed Concentration / Expected Concentration) * 100.
- Plot the measured concentration of the diluted native sample against the dilution factor. Perform linear regression.
- Success Criteria: Average spike recovery between 80-120%; dilution curve linearity with R² > 0.95.
Protocol 3.2: Pre-Analytical Stability Assessment
- Objective: To evaluate the impact of short-term storage conditions on biomarker integrity.
- Materials: Freshly collected matrix samples (pooled), conditions simulating common handling delays (room temperature, 4°C).
- Method:
- Aliquot a pooled matrix sample into multiple tubes.
- Expose aliquots to different conditions: 0h (baseline), 2h, 6h, 24h at room temperature and at 4°C. Centrifuge all at the same time-point to separate cells/clots if needed.
- Immediately freeze all processed aliquots at -80°C after their respective hold times.
- Analyze all samples in the same ELISA run to minimize inter-assay variability.
- Express the measured concentration as a percentage of the 0h baseline measurement.
- Success Criteria: <15% deviation from baseline under intended handling conditions (e.g., 6h at 4°C).
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents & Materials for Feasibility Assessment
| Item | Function & Critical Specification |
|---|---|
| Matched Antibody Pair (Capture/Detection) | Core of a sandwich ELISA. Requires high specificity and affinity (KD < 1nM) for the target biomarker epitope. Must be validated for the target matrix. |
| Recombinant Biomarker Protein | Serves as the standard for calibration curves. Must be pure, fully characterized (mass spec, sequencing), and biologically active if possible. |
| Matrix-Compatible ELISA Buffer System | Blocks non-specific binding and minimizes matrix interference. Often contains heterogeneous proteins (e.g., BSA, casein) and detergents. |
| Stable, Sensitive Detection Substrate (e.g., TMB, Amplex UltraRed) | Generates a quantifiable signal (colorimetric, chemiluminescent). Must have low background and high signal-to-noise ratio. |
| Validated Biological Matrix Samples | Disease-state and control samples from well-characterized cohorts. Critical for assessing real-world detectability and range. |
| Pre-Analytical Factor Simulation Kit | Controlled materials to test effects of anticoagulants, tube types, freeze-thaw cycles, etc. |
Visualizing the Assessment Workflow and Biological Context
Feasibility Assessment Decision Workflow
Biomarker Origin & ELISA Detection Pathway
Step-by-Step ELISA Protocol: From Sample Prep to Data Generation
Within the thesis framework of ELISA Principles for Biomarker Validation Research, the importance of the pre-analytical phase cannot be overstated. Variability introduced during sample collection, handling, and storage is a predominant source of error, often irreversibly compromising biomarker integrity and leading to unreliable ELISA data. This guide details standardized protocols to ensure sample quality, thereby underpinning the validity of downstream analytical results.
Sample Collection: Matrix-Specific Protocols
The choice of collection protocol is dictated by the biomarker's native matrix and susceptibility to degradation.
Blood-Derived Samples
Protocol: Peripheral Venous Blood Collection for Plasma/Serum Biomarkers
- Patient Preparation: Standardize patient fasting status, time of day, and physical activity prior to collection as per study protocol.
- Tourniquet Application: Apply for ≤1 minute. Prolonged application causes hemoconcentration and analyte shift.
- Venipuncture: Use a 21G needle. The first tube drawn should be used for chemistry/serology, not for biomarker analysis, to avoid tissue thromboplastin contamination.
- Tube Selection:
- Serum: Use serum separator tubes (SST). Allow to clot for 30 minutes at room temperature (RT) in an upright position.
- Plasma: Use anticoagulant tubes (e.g., EDTA for proteomics, citrate for coagulation markers, heparin for cytokines). Invert gently 8-10 times immediately after draw.
- Centrifugation: Spin at 2,000-3,000 x g for 10-15 minutes at 4°C (unless protocol specifies RT). For plasma, process within 30 minutes of collection. For serum, process after complete clot formation.
- Aliquoting: Carefully aspirate the supernatant (serum/plasma) using a pipette, avoiding the buffy coat or any pellet. Aliquot into low-protein-binding cryovials to avoid freeze-thaw cycles.
Table 1: Blood Collection Tube Selection Guide
| Tube Type / Additive | Primary Use | Critical Handling Step | Typical Storage Temp |
|---|---|---|---|
| Serum Separator (SST) | General chemistry, antibodies, hormones | Allow complete clot formation (30 min, RT) before spin. | -80°C |
| K2/K3 EDTA | Proteomics, cell-free DNA, genomics | Mix by inversion immediately after draw. Process plasma within 30 min. | -80°C |
| Sodium Citrate | Coagulation factors, platelet biomarkers | Strict 9:1 blood-to-anticoagulant ratio. Centrifuge for platelet-poor plasma. | -80°C |
| Lithium Heparin | Cytokines, emergency chemistry | Mix by inversion. Avoid for PCR due to heparin inhibition. | -80°C |
| PAXgene RNA | RNA stabilization | Invert 10x, incubate 2h RT before storage/processing. | -80°C (after incubation) |
Other Biofluids
- Urine: Collect mid-stream. Measure and record volume. Centrifuge at 2,000 x g for 10 min to remove cellular debris. Aliquot supernatant. Normalize analyte levels to creatinine concentration.
- Saliva: Use collection aids (Salivette). Centrifuge to separate saliva from cotton. Protease inhibitors are often required.
- Cerebrospinal Fluid (CSF): Collection is clinical. Aliquot immediately into low-binding tubes. Flash-freeze. Always note and standardize collection volume.
Sample Handling & Processing
Core Principle: Minimize time between collection and stabilization (freezing).
Table 2: Critical Time & Temperature Windows for Common Biomarkers
| Biomarker Class | Matrix | Max Hold Time RT | Max Hold Time 4°C | Processing Temp | Key Stabilizer/Inhibitor |
|---|---|---|---|---|---|
| Cytokines (e.g., IL-6, TNF-α) | Plasma/Serum | 2h | 24h | 4°C | Protease Inhibitor Cocktail |
| Phosphoproteins | Plasma, Tissue | <30 min | 2h | 4°C | Phosphatase Inhibitor Cocktail |
| Cell-Free DNA | Plasma | 2h | 24h | 4°C | EDTA (prevent nuclease activity) |
| Labile Metabolites | Plasma/Serum | <1h | 4h | 4°C | Immediate deproteinization |
| Exosomes | Plasma/Serum | 4h | 48h | 4°C (or RT) | Avoid repeated freeze-thaw |
Sample Storage & Stability
- Aliquoting: Aliquot single-use volumes to prevent repeated freeze-thaw cycles (>2 cycles is generally detrimental).
- Freezing: Rapid freeze in liquid nitrogen or dry ice before transfer to -80°C freezer. Avoid -20°C for long-term storage of most biomarkers.
- Documentation: Maintain a detailed log with freeze-thaw history.
- Shipping: Ship on dry ice in validated containers. Confirm that samples remain frozen upon receipt.
Experimental Protocol: Validating Pre-Analytical Variables for a Novel Biomarker via ELISA
Title: Protocol for Assessing the Impact of Pre-Analytical Delay on Measured Biomarker Concentration.
Objective: To determine the stability of a novel protein biomarker in human serum under varying pre-centrifugation delay times.
Materials: See "The Scientist's Toolkit" below. Method:
- Sample Collection: Draw blood from 5 healthy donors into 10 SST tubes each (50 tubes total).
- Variable Introduction: For each donor, process pairs of tubes at different pre-centrifugation delay times: 0h (immediate), 0.5h, 1h, 2h, 4h, 6h, 8h, 12h, 24h, 48h. Hold tubes upright at RT.
- Processing: At each time point, centrifuge tubes at 2,000 x g, 4°C for 15 min. Aliquot serum into 5 cryovials per time point and freeze at -80°C.
- ELISA Analysis: In a single plate to minimize inter-assay variance, thaw one aliquot from each time point for all donors. Perform a validated, quantitative ELISA according to manufacturer protocol. Run all samples in duplicate.
- Data Analysis: Calculate mean concentration for each time point. Express data as a percentage of the "0h" baseline concentration. Plot time vs. % recovery. Define stability as <15% deviation from baseline.
Visualizing the Pre-Analytical Workflow & Impact
Diagram 1: Biomarker Pre-Analytical Workflow & Error Sources
Diagram 2: Major Ex Vivo Biomarker Degradation Pathways
The Scientist's Toolkit: Essential Reagent Solutions
Table 3: Key Reagents for Pre-Analytical Stabilization
| Reagent / Material | Function in Pre-Analytical Phase | Example Application |
|---|---|---|
| Protease Inhibitor Cocktail | Broad-spectrum inhibition of serine, cysteine, metalloproteases. | Stabilizing cytokine and signaling phosphoprotein profiles in plasma/serum and tissue homogenates. |
| Phosphatase Inhibitor Cocktail | Inhibits alkaline, acid, and tyrosine phosphatases. | Preserving the phosphorylation state of target proteins in signaling studies. |
| EDTA & Citrate Anticoagulants | Chelate Ca2+ to inhibit coagulation and nuclease activity. | Plasma collection; cfDNA stabilization. |
| RNase/DNase Inhibitors | Prevent degradation of RNA/DNA. | Stabilizing cell-free RNA, transcriptomic biomarkers in biofluids. |
| Antioxidants (e.g., Ascorbic Acid) | Scavenge free radicals, prevent oxidation of labile epitopes. | Stabilizing metabolites and oxidation-prone proteins. |
| Low-Protein-Binding Tubes/Cryovials | Minimize adsorption of analyte to plastic surfaces. | Storage of all protein biomarkers, especially at low concentrations. |
| SST / Plasma Separation Tubes | Facilitate clean serum/plasma separation post-centrifugation. | Standard blood collection for most biomarker studies. |
| Stabilization Buffers (e.g., for Phosphoproteins) | Lyse cells and instantly inhibit degradation enzymes. | Snap-freezing tissue culture cells for phospho-protein ELISA. |
Within the rigorous framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technology. Its reliability for quantifying protein biomarkers directly dictates the quality of downstream data and clinical conclusions. This technical guide focuses on the foundational yet critical pre-analytical steps—coating, blocking, and washing—collectively forming an indispensable triad that establishes assay specificity, sensitivity, and reproducibility. Mastery of this triad is a prerequisite for any robust ELISA development protocol aimed at generating validation-grade data.
The Coating Step: Immobilizing the Capture Phase
Coating involves the passive adsorption of a capture molecule (typically an antibody or antigen) onto the solid phase of a microplate. This step defines the assay's target specificity.
Protocol: Optimizing Coating Conditions
- Preparation of Coating Buffer: 0.2 M carbonate-bicarbonate buffer, pH 9.6, is standard. Filter-sterilize (0.22 µm).
- Antibody/Antigen Dilution: Dilute the capture protein in coating buffer. A common starting concentration is 1–10 µg/mL. A checkerboard titration against the detection antibody is required for optimization.
- Coating: Add 100 µL/well to a high-binding polystyrene microplate. Seal and incubate overnight at 4°C (or 1–2 hours at 37°C).
- Termination: Following incubation, decant the coating solution. The plate is now ready for blocking.
Key Variables & Data
Table 1: Impact of Coating Buffer pH on Immobilization Efficiency
| Buffer pH | Relative Adsorption (%) | Recommended Use Case |
|---|---|---|
| 9.6 | 100* | Standard for most antibodies |
| 7.4 | 65 | For pH-sensitive antigens |
| 5.0 | 42 | Limited, specialized applications |
*Normalized reference value.
The Blocking Step: Sealing Non-Specific Sites
Blocking is the process of saturating unoccupied protein-binding sites on the plate surface after coating to prevent non-specific binding of subsequent reagents, a major source of high background noise.
Protocol: Effective Blocking
- Wash: After coating, wash the plate twice with 300 µL/well of Wash Buffer (e.g., PBS with 0.05% Tween 20, PBST).
- Blocking Solution: Add 300 µL/well of blocking agent. Common agents include:
- BSA (1–5% w/v in PBST): Universal, inexpensive.
- Non-fat dry milk (1–5% w/v in PBST): Cost-effective but can contain endogenous biotin/phosphatases.
- Casein (1% w/v in PBST): Excellent for phosphorylated targets, low background.
- Commercial protein-free blockers: Essential for minimizing animal-source interference.
- Incubation: Incubate for 1–2 hours at room temperature with gentle agitation.
- Prepare for Assay: Decant blocking solution. Plates can be used immediately or dried and sealed for storage at 4°C.
Table 2: Performance Comparison of Common Blocking Agents
| Blocking Agent | Background Signal | Suitability for Phospho-Specific ELISA | Risk of Interference |
|---|---|---|---|
| 1% BSA/PBST | Low | Moderate | Low (if purified) |
| 5% Non-fat Milk | Moderate | Poor | High (botin, enzymes) |
| 1% Casein/PBST | Very Low | Excellent | Low |
| Protein-Free Blocker | Low | Excellent | None |
The Washing Step: The Iterative Purification
Washing is the repeated process of adding and removing buffer to remove unbound reagents, matrix components, and non-specifically adsorbed molecules. It is performed after every incubation step.
Protocol: Consistent and Thorough Washing
- Wash Buffer: PBS or Tris-based buffer with a detergent (0.05–0.1% Tween 20). The detergent reduces hydrophobic interactions.
- Manual Method:
- Decant or aspirate liquid from wells.
- Fill each well completely with wash buffer (~300 µL) using a squirt bottle or multichannel pipette.
- Decant and forcefully tap the inverted plate on absorbent paper.
- Repeat for the prescribed number of cycles (typically 3-5 washes).
- Automated Method: Program an automated plate washer for consistent soak time, dispense volume, and aspiration height. This significantly improves reproducibility.
- Critical Step: After the final wash, firmly tap the plate to remove residual droplets before adding the next reagent.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for the Coating-Blocking-Washing Triad
| Item | Function & Rationale |
|---|---|
| High-Binding Polystyrene Plate | Optimal surface chemistry for passive protein adsorption via hydrophobic interactions. |
| Carbonate-Bicarbonate Buffer (pH 9.6) | Alkaline pH increases hydrophobicity of proteins, enhancing adsorption to plastic. |
| Bovine Serum Albumin (BSA) | A generic protein used to block remaining sites; inert for most immunoassays. |
| Tween 20 (Polysorbate 20) | Non-ionic detergent added to wash buffers to disrupt weak, non-specific binding. |
| Automated Microplate Washer | Provides unmatched consistency in wash volume, soak time, and aspiration across all wells. |
| Precision Multichannel Pipette | Enables rapid, uniform reagent addition and removal during manual processing steps. |
| Non-fat Dry Milk Blocker | A cost-effective blocking agent for general use, but unsuitable for phospho-protein assays. |
| Protein-Free (Synthetic) Blocker | Critical for assays where mammalian protein interference (e.g., from serum samples) is a concern. |
Integrated Workflow and Pathway Diagrams
Diagram 1: ELISA Foundation Triad Core Workflow
Diagram 2: Molecular Basis of Coating and Blocking
The coating, blocking, and washing triad is not a preliminary routine but the analytical bedrock of a validation-ready ELISA. Each step directly controls the signal-to-noise ratio, determining the assay's detection limit and dynamic range. In biomarker validation research, where precision and accuracy are paramount, systematic optimization and rigorous execution of this foundational triad are non-negotiable. It ensures that the observed signal is a true reflection of biomarker concentration, thereby upholding the integrity of the entire research endeavor.
Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technique in biomarker validation research, critical for drug development and clinical diagnostics. Its reliability hinges on the precise optimization of incubation dynamics—time, temperature, and reagent concentrations—which govern the kinetics of antigen-antibody interactions and enzymatic reactions. This technical guide, framed within a broader thesis on ELISA principles, provides an in-depth analysis of these core parameters to achieve maximal assay sensitivity, specificity, and reproducibility for rigorous biomarker validation.
Core Principles of Incubation Optimization
The fundamental goal is to drive the binding reactions to equilibrium efficiently without promoting non-specific binding or reagent degradation. The key interactions are:
- Primary Antibody-Antigen Binding: Governed by the association (k~a~) and dissociation (k~d~) rates, defining affinity.
- Secondary Antibody (Conjugate) Binding: Must be optimized to saturate target epitopes without causing hook effects.
- Enzyme-Substrate Reaction: A kinetic measurement where signal development must be linear and controlled.
Optimization involves balancing longer incubation times for increased sensitivity against practical throughput and potential increases in background noise.
Table 1: Optimization of Incubation Time and Temperature for a Typical Sandwich ELISA
| Parameter | Typical Range Tested | Optimal Value (Example) | Effect on Sensitivity (OD) | Effect on Background | Recommended Practice for Validation |
|---|---|---|---|---|---|
| Coating (Antigen) | 1 hr RT - O/N 4°C | O/N at 4°C | ++ (Maximizes adsorption) | + (if too long) | O/N at 4°C for consistency. |
| Blocking | 1-2 hrs at 37°C | 2 hrs at 37°C | -- (Reduces NSB) | --- (Critical) | Use protein-based blocker (BSA, casein). |
| Sample/Ab Incubation | 1 hr RT - 2 hrs 37°C | 1.5 hrs at 37°C | +++ (Main driver) | ++ (Risk of NSB) | Titrate antibody; 37°C for kinetics. |
| Conjugate Incubation | 30 min - 1.5 hrs 37°C | 1 hr at 37°C | ++ | +++ (High risk) | Use high-affinity, pre-titered conjugates. |
| Substrate Development | 5 - 30 min RT | 10 min at RT (in dark) | Controlled linear signal | + (if over-incubated) | Fixed time with precise stop. |
Table 2: Effect of Critical Reagent Concentrations on Assay Performance
| Reagent | Typical Concentration Range | Optimized Concentration Impact | Key Consideration for Sensitivity |
|---|---|---|---|
| Coating Antigen | 0.5 - 10 µg/mL in CBC | 2 µg/mL (Saturation curve) | High conc. can cause antigen aggregation. |
| Capture Antibody | 1 - 10 µg/mL in CBC | 4 µg/mL (Checkerboard) | Must pair with optimal sample incubation. |
| Detection Antibody | 0.5 - 5 µg/mL in Diluent | 1 µg/mL (Checkerboard) | High conc. increases background. |
| Enzyme-Conjugate | Manufacturer's rec. - 1:20K | 1:10,000 dilution (Titration) | Dominant source of amplification noise. |
| Sample | N/A (Biomarker-dependent) | Use within linear range of std curve | Matrix effects must be accounted for (e.g., serum). |
Detailed Experimental Protocols for Optimization
Protocol 1: Checkerboard Titration for Antibody Pair Optimization Objective: To determine the optimal working concentrations of matched capture and detection antibody pairs. Materials: Coating buffer (CBC, 0.05 M carbonate-bicarbonate, pH 9.6), PBS-T (PBS + 0.05% Tween-20), blocking buffer (1% BSA in PBS-T), antibody diluent, substrate (e.g., TMB). Method:
- Prepare serial dilutions of the capture antibody in CBC (e.g., 10, 5, 2.5, 1.25 µg/mL). Coat a 96-well plate with 100 µL/well of each dilution in columns 1-8. Incubate O/N at 4°C.
- Wash plate 3x with PBS-T. Block with 200 µL/well blocking buffer for 2 hours at 37°C.
- Wash 3x. Add a constant concentration of target antigen (or positive control) in duplicate rows.
- Prepare serial dilutions of the detection antibody in diluent (e.g., 1:1000, 1:2000, 1:4000, 1:8000).
- After sample incubation and wash, add the detection antibody dilutions. Incubate 1 hour at 37°C.
- Wash and add conjugate (if not directly conjugated) and substrate. Stop reaction and read OD.
- Analysis: Identify the combination yielding the highest signal-to-noise ratio (Positive/Negative control OD).
Protocol 2: Kinetic Incubation Time Course for Sensitivity Objective: To establish the optimal incubation time for sample/antibody reaction at a fixed temperature. Materials: As above, plus timer. Method:
- Coat and block plate as per optimized conditions from Protocol 1.
- Prepare a dilution series of the target biomarker (standard) and a negative control.
- Add samples to plate. Place plate in 37°C incubator.
- Remove replicate sets of wells (e.g., for each standard point) at defined time points (e.g., 30, 60, 90, 120 minutes) and immediately place on ice or wash thoroughly to stop the reaction.
- Complete the remaining assay steps (detection Ab, conjugate, substrate) uniformly for all wells.
- Analysis: Plot OD vs. time for each standard concentration. The optimal time is at or just before the plateau phase for mid-range standards, ensuring maximal signal while maintaining a linear standard curve.
Visualization of Pathways and Workflows
Title: ELISA Workflow with Key Incubation Steps
Title: Sandwich ELISA Binding & Signal Amplification Pathway
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Optimizing ELISA Incubation Dynamics
| Item & Example Solution | Primary Function in Incubation Optimization |
|---|---|
| High-Affinity Matched Antibody Pairs (e.g., DuoSet or similar) | Pre-validated for sandwich ELISA; reduces optimization time and ensures specificity, directly impacting optimal concentration ranges. |
| Stable, Low-Noise Enzyme Conjugates (e.g., HRP-Streptavidin) | Provides consistent amplification; optimized dilution minimizes background during conjugate incubation. |
| Chemically Defined Blocking Buffers (e.g., Protein-free blockers) | Reduces non-specific binding (NSB) without introducing interfering proteins, crucial for sensitive biomarker detection in complex matrices. |
| Precision Microplate Coaters/Washers | Ensures even reagent distribution during coating and thorough, consistent washing between incubations to control background. |
| Controlled-Temperature Incubation Shakers | Maintains homogenous temperature and gentle mixing during sample/antibody steps, improving kinetics and reproducibility. |
| Standardized Antigen/Biomarker Reference Standards | Provides the critical benchmark for generating accurate standard curves, enabling precise quantification and assay validation. |
Within the framework of ELISA-based biomarker validation for drug development, the selection of an appropriate detection system is critical for assay sensitivity, dynamic range, and multiplexing capability. This technical guide provides an in-depth comparison of chromogenic, chemiluminescent, and fluorescent readouts, enabling researchers to make informed decisions aligned with their experimental objectives.
The validation of protein biomarkers in biological matrices relies heavily on the specificity and sensitivity of enzyme-linked immunosorbent assays (ELISAs). The detection readout, a culmination of enzymatic signal generation and measurement, fundamentally dictates the performance characteristics of the assay. This whitepaper examines the underlying chemistries, performance metrics, and practical applications of the three dominant readout modalities to guide optimal assay development.
Core Detection Chemistries and Performance Data
Table 1: Comparative Performance Characteristics of ELISA Readouts
| Parameter | Chromogenic | Chemiluminescent | Fluorescent |
|---|---|---|---|
| Typical Sensitivity (Lower Detection Limit) | ~pg/mL range | ~fg/mL - low pg/mL range | ~pg/mL range |
| Dynamic Range | 1-2 logs | 3-6 logs | 3-5 logs |
| Signal Stability | Stable (precipitated product) | Transient (requires timely reading) | Generally stable |
| Multiplexing Potential | Low | Low to Moderate (sequential) | High (multiple wavelengths) |
| Primary Instrument | Plate Absorbance Reader | Plate Luminometer | Fluorescence Microplate Reader |
| Common Enzyme Substrate Pairs | HRP/TMB, AP/PNPP | HRP/Luminol, AP/CDP-Star | N/A (Direct fluorophore) |
| Background Signal | Moderate (from plate/buffer) | Very Low | Variable (autofluorescence) |
| Quantitative Nature | Good | Excellent | Excellent |
Table 2: Common Substrates and Their Properties
| Readout Type | Enzyme | Common Substrate | Signal Generated | Quenching Solution |
|---|---|---|---|---|
| Chromogenic | Horseradish Peroxidase (HRP) | 3,3',5,5'-Tetramethylbenzidine (TMB) | Blue (450 nm), Yellow (650 nm) | 1M H₂SO₄ or HCl |
| Chromogenic | Alkaline Phosphatase (AP) | p-Nitrophenyl Phosphate (PNPP) | Yellow (405 nm) | 1M NaOH |
| Chemiluminescent | HRP | Luminol + H₂O₂ + Enhancer | Blue Light (428 nm) | None (read immediately) |
| Chemiluminescent | AP | CDP-Star / CSPD | Sustained Glow | None |
| Fluorescent | N/A (Direct) | Alexa Fluor dyes, Cyanine dyes | Emits at specific λ | None |
Experimental Protocols
Protocol 1: Standard Chromogenic ELISA (HRP/TMB)
Purpose: To detect and quantify a target antigen using a colorimetric signal.
- Coating: Coat a 96-well plate with 100 µL/well of capture antibody (1-10 µg/mL in carbonate/bicarbonate buffer, pH 9.6). Incubate overnight at 4°C.
- Blocking: Aspirate and block with 200-300 µL/well of blocking buffer (e.g., 1% BSA, 5% non-fat dry milk in PBS) for 1-2 hours at room temperature (RT).
- Sample/Antigen Incubation: Add 100 µL of sample or calibrator in assay diluent. Incubate 1-2 hours at RT.
- Detection Antibody Incubation: Add 100 µL of biotinylated or enzyme-conjugated detection antibody. Incubate 1 hour at RT.
- Enzyme Conjugate Incubation (if needed): For biotinylated antibodies, add 100 µL of Streptavidin-HRP conjugate. Incubate 30-45 minutes at RT.
- Washing: Wash plate 3-5 times with PBS + 0.05% Tween-20 between each step.
- Signal Development: Add 100 µL of TMB substrate solution. Incubate in the dark for 5-30 minutes at RT.
- Stop Reaction: Add 100 µL of 1M H₂SO₄ to stop the reaction.
- Readout: Measure absorbance immediately at 450 nm (primary) with a reference at 570 or 650 nm.
Protocol 2: High-Sensitivity Chemiluminescent ELISA
Purpose: To achieve maximal detection sensitivity for low-abundance biomarkers.
- Steps 1-6: Follow Protocol 1 (Coating through Washing).
- Signal Development: Prepare chemiluminescent substrate (e.g., luminol/peroxide + enhancer) according to manufacturer's instructions. Add 100 µL/well.
- Incubation: Incubate for 3-5 minutes at RT, protected from light.
- Readout: Read plate immediately in a luminometer, integrating signal over 100-1000 milliseconds/well. Note: Signal is transient; read plate within 30 minutes.
Protocol 3: Fluorescent ELISA (Direct Detection)
Purpose: To enable multiplexing or reduce background in complex samples.
- Steps 1-5: Follow Protocol 1, but use fluorophore-conjugated detection antibodies (e.g., Alexa Fluor 647) or a fluorogenic substrate for the enzyme.
- Washing: Perform thorough final washes to minimize unbound fluorophore.
- Signal Development (if enzymatic): Add fluorogenic substrate (e.g., QuantaRed for HRP). Incubate as recommended.
- Readout: Read plate in a fluorescence microplate reader using appropriate excitation/emission filters (e.g., Ex 650 nm / Em 665 nm for Cy5).
Visualization of Key Concepts
Signal Detection Pathway and Measurement
Enzymatic Signal Generation Cascade in ELISA
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Detection | Key Considerations |
|---|---|---|
| High-Purity Capture/Detection Antibodies | Provide specificity for the target biomarker. | Monoclonal recommended for consistency; validate pair for sandwich ELISA. |
| Enzyme Conjugates (HRP, AP) | Catalyze the conversion of substrate to detectable signal. | HRP: higher specific activity; AP: more stable but larger size. |
| Chromogenic Substrate (e.g., TMB) | Yields a colored, soluble or precipitable product upon enzyme action. | Single-component (ready-to-use) vs. two-component (stable until mixed). |
| Chemiluminescent Substrate (e.g., Luminol) | Produces light upon oxidation by the enzyme. | "Glow"-type (stable signal) vs. "Flash"-type (intense, brief signal). |
| Fluorophore Conjugates (e.g., Alexa Fluor 647) | Emit light at a specific wavelength upon excitation. | High photostability and brightness; minimal overlap in multiplex panels. |
| Blocking Buffer (BSA, Casein) | Covers nonspecific binding sites on the plate to reduce background. | Must be optimized for the specific assay; protein-free options available. |
| Plate Washer and Wash Buffer | Removes unbound reagents to minimize nonspecific signal. | Stringency is critical; Tween-20 is a common detergent additive. |
| Microplate Reader | Measures absorbance, luminescence, or fluorescence signal. | Must match detection modality; consider sensitivity and dynamic range. |
Within biomarker validation research using ELISA, the calibration (or standard) curve is the fundamental mathematical model that translates raw assay signal (e.g., absorbance) into a quantitative concentration value. Its correct construction and validation are paramount for ensuring the accuracy, precision, and reliability of pharmacokinetic, pharmacodynamic, and diagnostic data. This guide details the technical considerations for curve construction, the application of asymmetric logistic models (4PL, 5PL), and the acceptance criteria necessary for robust analytical performance within a GLP-compliant framework.
Construction of the Calibration Curve
Experimental Protocol for Standard Preparation
A precise dilution series of the analyte of known concentration is assayed alongside unknown samples. The protocol is as follows:
- Stock Solution Preparation: Reconstitute the certified reference standard in the specified matrix (e.g., assay buffer, diluted serum) to create a high-concentration stock.
- Serial Dilution: Perform a logarithmic serial dilution (typically 1:2 or 1:3) to generate 6-8 non-zero calibrator concentrations spanning the assay's claimed range. Include a blank (zero calibrator).
- Plate Layout: Run each calibrator in replicate (minimum duplicate, preferably triplicate) according to a randomized or balanced plate layout to minimize positional effects.
- Assay Execution: Process the calibrators identically to test samples through all ELISA steps (coating, blocking, sample/signal antibody incubation, washing, detection).
- Data Acquisition: Measure the instrumental response (e.g., OD at 450 nm).
Key Research Reagent Solutions
| Reagent / Material | Function in Calibration |
|---|---|
| Certified Reference Standard | Provides the analyte of known identity, purity, and concentration to establish the analytical relationship. |
| Calibrator Matrix | The biological fluid or buffer used to dilute the standard. Should closely mimic the sample matrix to minimize matrix effects. |
| ELISA Microplate | Solid phase (typically 96-well) coated with capture antibody. |
| Detection Enzyme Conjugate (e.g., HRP-Streptavidin) | Catalyzes the conversion of chromogenic substrate to generate measurable signal proportional to analyte binding. |
| Stable Chromogenic/TMB Substrate | Produces a colorimetric change upon enzyme action. Must have low background and high signal-to-noise. |
| Plate Reader (Spectrophotometer) | Precisely measures the absorbance of each well at a defined wavelength. |
Curve Fitting Models: 4PL vs. 5PL
Four-Parameter Logistic (4PL) Model
The 4PL model is symmetric around its inflection point and is defined by: [ y = D + \frac{A - D}{1 + (\frac{x}{C})^B} ] Where:
- y: Response (Signal)
- x: Analyte Concentration
- A: Minimum asymptote (background signal)
- B: Slope factor (Hill's coefficient)
- C: Inflection point (EC50/IC50)
- D: Maximum asymptote (saturation signal)
Five-Parameter Logistic (5PL) Model
The 5PL model introduces an asymmetry parameter (G) to account for skew often present in highly sensitive assays: [ y = D + \frac{A - D}{(1 + (\frac{x}{C})^B)^G} ] Where parameters A, B, C, D are as in 4PL, and:
- G: Asymmetry factor. When G=1, the model reduces to 4PL.
Model Selection and Quantitative Comparison
Calibration Curve Model Selection Workflow (100 chars)
Table 1: Characteristics of 4PL and 5PL Curve Fitting Models
| Parameter / Feature | 4PL Model | 5PL Model |
|---|---|---|
| Symmetry | Assumes symmetry around inflection point (C). | Accounts for asymmetry via parameter G. |
| Number of Parameters | 4 | 5 |
| Typical Application | Standard ELISA with symmetric sigmoidal response. | High-sensitivity assays, extended dynamic range, or asymmetric curves. |
| Computational Complexity | Lower; more stable with fewer data points. | Higher; requires more robust calibrator data (≥7 points). |
| Key Strength | Simplicity, stability, widely accepted. | Flexibility in fitting skewed data, often better accuracy at extremes. |
| Potential Limitation | May produce biased back-calculations at curve tails if asymmetry exists. | Risk of overfitting with sparse or noisy data. |
Acceptance Criteria for the Calibration Curve
A calibration curve must meet predefined acceptance criteria to be deemed valid for interpolating sample concentrations.
Table 2: Typical Acceptance Criteria for ELISA Calibration Curves
| Criterion | Typical Acceptance Limit | Rationale & Calculation |
|---|---|---|
| Coefficient of Determination (R²) | ≥ 0.990 (for 4PL/5PL) | Measures proportion of variance in signal explained by the model. ( R² = 1 - \frac{SS{res}}{SS{tot}} ) |
| Calibrator Accuracy (% Relative Error) | Within ±20% (LLOQ/UULOQ), ±15% (others) | Assesses model's fit to the calibrator data. ( RE\% = \frac{(Back-calculated Conc. - Nominal Conc.)}{Nominal Conc.} \times 100) |
| Total Error (Bias + Imprecision) | ≤ 30% | Combines systematic (bias) and random (precision) error for calibrators. |
| Curve Residuals | Random scatter, no pattern | Visual inspection of residuals vs. concentration to detect systematic misfit. |
Protocol for Assessing Curve Fit Quality
- Fit the Model: Using validated software, fit the (x=conc, y=signal) data to the selected model (4PL/5PL) using iterative least-squares algorithms (e.g., Levenberg-Marquardt).
- Back-calculate Concentrations: Use the fitted model parameters to calculate the concentration of each calibrator from its mean signal.
- Calculate Metrics: For each calibrator, compute %RE. Calculate the mean squared error (MSE) and R² for the overall fit.
- Visual Assessment: Generate a residual plot (residual vs. concentration or fitted value). Acceptable curves show random scatter around zero.
- Apply Criteria: Verify all metrics in Table 2 are within limits. If not, investigate potential causes (pipetting error, degraded standard, plate defect, inappropriate model).
Integration within Biomarker Validation Thesis
Calibration's Role in Biomarker Validation Thesis (100 chars)
The calibration curve is not an isolated step. Its performance directly underpins key validation parameters:
- Accuracy & Linearity: Defined by calibrator %RE.
- Sensitivity (LLOQ): The lowest calibrator meeting accuracy/imprecision criteria, determined via the curve.
- Precision: Repeatedly generated curves assess inter-assay precision of the analytical method. A robust, well-characterized calibration model is therefore the non-negotiable foundation for generating credible biomarker concentration data, enabling sound scientific conclusions in drug development research.
Within the context of biomarker validation research using ELISA (Enzyme-Linked Immunosorbent Assay) principles, the accurate quantification of analyte concentration is paramount. This technical guide details the core calculations involved, addressing the linear interpolation from a standard curve, the application of dilution factors, and the critical correction for matrix effects. These steps are fundamental for translating raw assay signals (optical density) into physiologically or pathologically relevant concentrations.
The Standard Curve: Foundation for Interpolation
The standard curve establishes the relationship between the known concentrations of a purified standard and the assay signal. A typical sigmoidal or linear (after log transformation) curve is generated.
Protocol: Generating a Standard Curve
- Serial Dilution: Prepare a high-concentration stock solution of the purified biomarker standard. Perform a serial dilution (e.g., 1:2 or 1:3) in the assay diluent to create 6-8 standard points covering the expected dynamic range, plus a zero standard (diluent only).
- Assay Execution: Analyze all standard points in duplicate alongside unknown samples using the validated ELISA protocol.
- Data Fitting: Plot the mean absorbance (y-axis) against the standard concentration (x-axis, typically log-transformed). Fit a 4- or 5-parameter logistic (4PL/5PL) regression model using specialized software (e.g., SoftMax Pro, GraphPad Prism). A weighted linear regression on log-transformed data may be used for a linear range.
Table 1: Example Standard Curve Data for Hypothetical Biomarker "X"
| Standard Point | Concentration (pg/mL) | Log10(Conc.) | Mean Absorbance (450nm) | CV (%) |
|---|---|---|---|---|
| Blank | 0.00 | - | 0.051 | - |
| Std 1 | 7.81 | 0.892 | 0.102 | 3.5 |
| Std 2 | 15.63 | 1.194 | 0.210 | 2.8 |
| Std 3 | 31.25 | 1.495 | 0.450 | 2.1 |
| Std 4 | 62.50 | 1.796 | 0.920 | 1.9 |
| Std 5 | 125.00 | 2.097 | 1.550 | 2.3 |
| Std 6 | 250.00 | 2.398 | 2.100 | 2.7 |
| Std 7 | 500.00 | 2.699 | 2.400 | 3.0 |
Interpolation of Unknown Samples
The concentration of an unknown sample is determined by interpolating its mean absorbance value onto the fitted standard curve.
Methodology:
- Calculate the mean absorbance for each unknown sample.
- Using the regression equation from the standard curve, solve for the concentration (
x) given the sample's absorbance (y). For a 4PL model, the equation is:y = d + (a - d) / (1 + (x/c)^b)where: a = minimum asymptote, b = slope factor, c = inflection point (EC50), d = maximum asymptote. - The result is the interpolated concentration in the same units as the standards (e.g., pg/mL).
Applying the Dilution Factor
Biomarker levels in biological matrices (serum, plasma, CSF) often exceed the assay's upper limit of quantification (ULOQ), necessitating pre-analytical dilution.
Calculation:
Corrected Concentration = Interpolated Concentration × Dilution Factor (DF)
Where DF = (Final Volume) / (Sample Volume). A 1:10 dilution (10 µL sample + 90 µL diluent) has a DF of 10.
Table 2: Example Dilution Factor Calculations
| Sample ID | Interpolated Conc. (pg/mL) | Dilution Performed | Dilution Factor (DF) | Final Reported Conc. (pg/mL) |
|---|---|---|---|---|
| PT-001 | 45.2 | None | 1 | 45.2 |
| PT-002 | 1125.0 (above ULOQ) | 1:10 | 10 | 11,250.0 |
| PT-003 | 8.5 | 1:2 (per protocol) | 2 | 17.0 |
Accounting for Matrix Effects
Matrix effects occur when components of the sample (e.g., lipids, proteins, salts) alter the assay's ability to detect the analyte, causing apparent recovery to deviate from 100%. This is assessed via a spike-and-recovery experiment.
Experimental Protocol: Spike-and-Recovery
- Prepare Samples:
- Matrix Spike: Spike a known, moderate concentration of the pure biomarker standard (from the standard curve) into the biological matrix of interest (e.g., 100 µL of 100 pg/mL standard into 100 µL of normal serum).
- Standard Spike: Spike the same amount of standard into the assay diluent (ideal matrix).
- Background Control: Include an unspiked sample of the matrix to measure endogenous levels.
- Assay: Run all samples in the same ELISA plate.
- Calculate Percent Recovery:
% Recovery = [ (Measured Conc. of Matrix Spike – Endogenous Conc. of Matrix) / Theoretical Spike Conc. ] × 100The Theoretical Spike Concentration is the concentration of the standard added, accounting for the dilution into the matrix.
Table 3: Example Matrix Effect Recovery Assessment
| Sample Type | Measured Conc. (pg/mL) | Expected/Theoretical Conc. (pg/mL) | % Recovery | Interpretation |
|---|---|---|---|---|
| Standard in Diluent | 98.5 | 100.0 | 98.5% | Reference |
| Normal Human Serum | 15.2 (endogenous) | - | - | Baseline |
| Spiked Normal Serum | 108.1 | 115.2 (100 pg/mL spike + 15.2) | 93.9% | Acceptable |
| Spiked Hemolyzed Serum | 85.7 | 115.2 | 74.3% | Unacceptable |
Correcting for Matrix Effects: If recovery is consistent and sub-optimal (e.g., consistently 85%), results can be corrected: Matrix-Corrected Conc. = (DF-Corrected Conc.) / (%Recovery/100). However, investigation into the cause is preferred over mathematical correction.
Biomarker Concentration Calculation Workflow
Integrated Calculation Example
A serum sample is diluted 1:20 prior to ELISA. Its interpolated concentration is 80 pg/mL. The validated average recovery for this biomarker in serum is 92%.
- Dilution Correction:
80 pg/mL × 20 = 1600 pg/mL - Matrix Effect Correction:
1600 pg/mL / 0.92 = 1739 pg/mLThe final reported concentration is 1739 pg/mL.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Biomarker Quantitation by ELISA
| Item | Function in Experiment |
|---|---|
| Matched-Pair Antibodies | Highly specific capture and detection antibodies form the core of sandwich ELISA specificity. |
| Recombinant Purified Biomarker Standard | Provides the known quantities for constructing the standard curve. Must be identical to the endogenous analyte. |
| Assay Diluent / Matrix | Buffer used for serial dilutions of standards and samples. May contain blockers (BSA, casein) to reduce nonspecific binding. |
| Standard Diluent | Optimized buffer, often protein-based, for reconstituting and diluting the standard to preserve stability and immunoreactivity. |
| Sample Diluent (for complex matrices) | Specialized buffer designed to mitigate matrix effects, often containing detergents or competitors for sample pre-treatment. |
| Stabilized Enzyme Conjugate | Detection antibody conjugated to HRP or ALP. Stability is critical for consistent signal generation. |
| Signal Generation Reagents | TMB (3,3',5,5'-Tetramethylbenzidine) substrate for HRP, or pNPP for ALP. Yields a colorimetric product proportional to analyte. |
| Stop Solution | Acid (e.g., 1M H2SO4) to halt the enzymatic reaction, stabilizing the final signal for measurement. |
| Wash Buffer Concentrate | Typically PBS or Tris-based with surfactant (Tween-20) to remove unbound materials between assay steps, reducing background. |
| Control Samples (High, Low, Negative) | Quality control materials with known ranges to monitor inter-assay precision and accuracy. |
Sandwich ELISA Signal Generation Pathway
Troubleshooting Common ELISA Pitfalls and Advanced Optimization Strategies
Within the framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technology. Its reliability is paramount for generating high-quality, reproducible data that informs drug development. However, researchers frequently encounter performance issues—specifically high background, low target signal, and high coefficients of variation (CVs)—that can compromise data integrity and derail project timelines. This guide provides a systematic, technical approach to diagnosing these common problems, grounded in core ELISA principles.
Systematic Diagnosis of ELISA Performance Issues
The first step is a structured investigation to isolate the root cause. The following flowchart outlines the diagnostic logic.
Quantitative Benchmarking of Common Issues
The table below summarizes expected performance metrics and typical deviations associated with common problems.
| Performance Parameter | Optimal Range (Typical Sandwich ELISA) | High Background Indication | Low Signal Indication | High CV Indication |
|---|---|---|---|---|
| Assay Background (Abs) | < 0.15 (for TMB substrate) | > 0.25 | N/A | N/A |
| Signal-to-Background Ratio | > 10 | < 5 | < 5 | N/A |
| Maximum Signal (Abs) | 2.5 - 3.5 (plate reader limit) | May be normal or elevated | < 1.5 | N/A |
| Intra-Assay CV | < 10% | May be elevated | May be elevated | > 12% |
| Inter-Assay CV | < 15% | May be elevated | May be elevated | > 20% |
| Standard Curve R² | > 0.99 | Often unaffected | Often unaffected | May be < 0.98 |
Detailed Diagnostic Protocols
Protocol 1: Investigating High Background
Objective: To identify sources of non-specific binding (NSB). Methodology:
- Run Control Wells: Include wells with all reagents except the target-specific capture antibody (coated with a non-immune IgG or blocking protein). Include wells without sample (assay diluent only).
- Optimize Blocking: Test different blocking buffers (e.g., 1-5% BSA, 5% non-fat dry milk, or commercial protein blockers) and increase blocking time (1-3 hours) at room temperature.
- Increase Wash Stringency: Perform additional wash cycles (e.g., increase from 3x to 5-6x). Introduce a low-concentration (0.05-0.1%) detergent (e.g., Tween-20) into the wash buffer if not already present. Perform a final rinse with PBS or deionized water.
- Evaluate Substrate: Ensure substrate is clear and colorless before use. Incubate substrate in the dark for a precise, timed period. Read plate immediately after stopping reaction.
Protocol 2: Investigating Low Target Signal
Objective: To identify reagent or incubation failures in the signal generation cascade. Methodology:
- Check Reagent Integrity: Verify antibody pair compatibility (epitope mapping). Test new aliquots of detection antibody and enzyme conjugate. Confirm conjugate activity via a titration series.
- Optimize Incubation: Increase primary (sample/analyte) incubation time to 2 hours at RT or overnight at 4°C. Ensure plates are sealed and humidified to prevent evaporation.
- Verify Antigen Integrity: Ensure the target biomarker is not degraded in the sample matrix. Use a spike-and-recovery experiment: spike a known concentration of recombinant antigen into a sample matrix and measure recovery (target: 80-120%).
- Substrate Freshness: Prepare substrate solution immediately before use. Check expiration dates.
Protocol 3: Investigating High Coefficient of Variation (CVs)
Objective: To identify sources of technical imprecision. Methodology:
- Pipette Calibration: Service and calibrate all pipettes. Use reverse pipetting for viscous samples and reagents.
- Plate Washer Validation: Manually inspect washer nozzles for clogs. Run a dye test to ensure uniform wash buffer dispensing and aspiration across all wells.
- Edge Effect Assessment: Incubate plates in a sealed, humidified chamber in the center of the incubator. Compare CVs of edge wells vs. interior wells. If edge effects are present, consider using a thermal seal or a water bath incubator.
- Reagent Homogeneity: Thoroughly vortex and centrifuge all reagent vials before use. Allow all reagents to equilibrate to room temperature (unless protocol specifies otherwise) to minimize condensation and temperature gradients.
Core ELISA Signaling Pathway
The following diagram details the fundamental biochemical cascade in a sandwich ELISA, highlighting potential failure points.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| High-Affinity, Matched Antibody Pair | Ensures specific capture and detection of the target epitope, minimizing cross-reactivity and maximizing signal-to-noise. Validated pairs are essential. |
| Recombinant Target Antigen Standard | A purified, quantified standard is critical for generating an accurate standard curve for quantification and for spike-and-recovery experiments. |
| HRP or AP Conjugates with High Specific Activity | The enzyme (Horseradish Peroxidase or Alkaline Phosphatase) drives the colorimetric reaction. High specific activity yields stronger signal. |
| Stabilized Chromogenic TMB Substrate | 3,3',5,5'-Tetramethylbenzidine (TMB) is the most common HRP substrate. Stabilized, ready-to-use formulations reduce background and improve reproducibility. |
| Low-Protein-Binding Microplates | Plates specifically treated to minimize passive adsorption of reagents reduce non-specific binding, lowering background. |
| Precision Plate Washer | Consistent and thorough washing is the single most critical step for reducing background and variability. Automated washers must be well-maintained. |
| Calibrated Multichannel & Single-Channel Pipettes | Accurate liquid handling is fundamental to achieving low intra- and inter-assay CVs. Regular calibration is mandatory. |
| Blocking Buffer (e.g., 5% BSA, Casein) | Blocks remaining protein-binding sites on the plate and on antibodies to prevent non-specific binding of subsequent reagents. |
Overcoming Hook Effect and Prozone Phenomenon in Sandwich ELISA
Within the framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technique for the specific and sensitive quantification of proteins. The sandwich ELISA format, in particular, offers high specificity by employing two antibodies targeting different epitopes on the analyte. However, the accuracy of this assay can be critically compromised by two interrelated phenomena: the Hook Effect and the Prozone Phenomenon. These effects lead to a falsely low signal at extremely high analyte concentrations, risking significant data misinterpretation in both research and clinical diagnostics. This technical guide details the underlying mechanisms and provides robust, actionable strategies to identify and overcome these limitations, thereby ensuring data integrity for critical drug development and validation workflows.
Mechanisms and Distinctions
While often used interchangeably, the Hook Effect and Prozone Phenomenon have distinct mechanistic origins.
- Hook Effect: Predominantly occurs in sandwich immunoassays. At excessively high analyte concentrations, both the capture and detection antibodies become saturated. This prevents the formation of the essential "sandwich" complex, as analyte molecules bind separately to either antibody, leading to a decrease in the measured signal.
- Prozone Phenomenon (Antigen Excess): A broader term describing false lows due to excess analyte, historically noted in agglutination tests. In immunoassays, it occurs when the high-analyte concentration overwhelms the reagent antibodies, resulting in univalent binding (analyte bound by only one antibody) instead of the required multivalent binding, inhibiting signal generation.
Table 1: Core Characteristics of Hook and Prozone Effects
| Feature | Hook Effect (Sandwich ELISA) | Prozone Phenomenon (General) |
|---|---|---|
| Primary Cause | Saturation of both capture & detection antibodies; insufficient antibody pairing. | Extreme antigen excess relative to antibody concentration. |
| Assay Types | Primarily two-site immunometric assays (Sandwich ELISA). | Agglutination, nephelometry, turbidimetry, some immunoassays. |
| Molecular Result | Failure to form ternary "sandwich" complexes. | Formation of small, soluble immune complexes due to univalent binding. |
| Visual Clue | High-concentration sample gives signal similar to low-concentration sample. | Lack of agglutination or expected precipitation at high concentrations. |
| Solution | Sample dilution, increased antibody concentration, assay re-optimization. | Sample dilution, reagent re-balancing. |
Proactive Identification and Diagnostic Protocols
Serial Dilution Experiment
The definitive method to identify the presence of a Hook/Prozone effect is a simple serial dilution of a high-signal sample.
Protocol:
- Select a sample yielding a high absorbance value near the assay's upper limit.
- Prepare a logarithmic serial dilution (e.g., 1:10, 1:100, 1:1000, 1:10,000) of the sample using the assay's sample diluent.
- Re-assay the original sample and all dilutions in the same plate.
- Plot the measured concentration (or signal) against the dilution factor.
Interpretation: If the measured concentration increases proportionally with dilution until reaching a plateau, a Hook Effect is confirmed for the original, undiluted sample.
Table 2: Interpretation of Serial Dilution Data
| Result Pattern | Inference | Action |
|---|---|---|
| Linear increase in measured conc. with dilution | Hook Effect Present in original sample. | Report result from the linear range dilution. |
| Measured conc. remains stable across dilutions | No Hook Effect. Original result is valid. | Report original result. |
| Measured conc. decreases with dilution | Potential matrix interference or non-specific binding. | Investigate sample matrix. |
Alternative Assay Formats
Using a different assay format can provide orthogonal validation.
- Competitive ELISA: This format is inherently resistant to the Hook Effect, as high analyte concentrations produce appropriately low signals.
- ELISA with Different Antibody Pair: An alternative antibody pair with higher affinity or targeting different epitopes may shift the dynamic range.
Mitigation Strategies and Optimized Protocols
Assay Re-optimization for Extended Dynamic Range
Protocol: Titration of Capture and Detection Antibodies
- Capture Antibody Titration: Coat plates with varying concentrations of capture antibody (e.g., 0.5, 1, 2, 4 µg/mL). Use a high-concentration analyte standard and a fixed, excess concentration of detection antibody.
- Detection Antibody Titration: Using the optimal capture concentration from step 1, test varying dilutions of the detection antibody conjugate against a range of analyte standards, including a very high concentration.
- Analysis: Identify the antibody concentration combination that yields the widest linear range on the standard curve and the highest signal for the high analyte standard without plateauing or declining.
Mandatory Sample Pre-Dilution
For assays measuring biomarkers with a wide physiological range (e.g., cytokines, CRP, PSA), establishing a routine sample pre-dilution is critical. Protocol: Validate two dilution factors during assay development. Use a 1:10 or 1:100 dilution for initial screening. Any sample yielding a result >90% of the assay's upper limit should be re-tested at a higher dilution (e.g., 1:1000).
Utilization of Monoclonal vs. Polyclonal Antibodies
- Strategy: Employ a high-affinity monoclonal antibody for capture to ensure specific, saturable binding. Use a polyclonal antibody for detection, as its recognition of multiple epitopes increases the likelihood of forming a sandwich complex even at high analyte concentrations, mitigating the Hook Effect.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Hook Effect Investigation & Mitigation
| Item | Function & Rationale |
|---|---|
| High-Affinity Monoclonal Antibody Pair | Provides specific, saturable binding. Critical for defining the assay's maximum capacity. |
| Polyclonal Detection Antibody | Recognizes multiple epitopes, increasing probability of sandwich formation at high analyte levels. |
| Recombinant Antigen Standard (High Purity) | Essential for generating a reliable standard curve up to very high concentrations to map the hook region. |
| Low-Protein-Binding Microplates | Minimizes non-specific adsorption of reagents, ensuring optimal antibody availability for specific binding. |
| Precision Multichannel Pipettes & Reservoirs | Enables accurate and reproducible serial dilution workflows. |
| Plate Reader with Kinetic/Endpoint Software | Allows for data review and identification of atypical curve shapes that may indicate a hook effect. |
| Data Analysis Software (e.g., GraphPad Prism, 4/5PL fitting) | Enables nonlinear regression analysis to model and identify the descending limb of the dose-response curve. |
This guide addresses a critical challenge in the validation of biomarkers via Enzyme-Linked Immunosorbent Assay (ELISA) as part of a rigorous thesis on immunoassay principles. The accurate quantification of target analytes in complex biological matrices is paramount for diagnostic and drug development research. However, serum, plasma, cerebrospinal fluid (CSF), and tissue homogenates contain diverse interfering components that can compromise assay specificity, sensitivity, and reproducibility. This whitepaper provides an in-depth technical analysis of these interferences and offers validated experimental protocols to mitigate their effects, ensuring robust biomarker data.
Matrix effects arise from non-specific interactions between sample components and the assay system. They can cause false elevation (positive interference) or suppression (negative interference) of the signal.
Primary Sources of Interference:
- Heterophilic Antibodies and Rheumatoid Factors (RF): Endogenous antibodies that cross-link capture and detection antibodies.
- Complement Factors: Can bind to immunoglobulin Fc regions, blocking epitopes.
- Biotin: High endogenous levels in serum can interfere with streptavidin-biotin based detection systems.
- Albumin and Other High-Abundance Proteins: Non-specific binding and masking of target analytes.
- Lipids and Hemolysis (in serum/plasma): Affect sample viscosity and optical properties; hemoglobin can quench fluorescence or catalyze peroxidase reactions.
- Proteases and Enzymes (in tissue homogenates): Degrade antibodies or target analytes.
- Salt and Ionic Strength Variations (in CSF & homogenates): Affect antibody-antigen binding kinetics.
Quantitative Comparison of Interferent Concentrations
Table 1: Typical Concentration Ranges of Key Interferents Across Matrices
| Interferent | Serum | Plasma (EDTA) | CSF | Tissue Homogenate (10% w/v) | Primary Interference Type |
|---|---|---|---|---|---|
| Total Protein (g/L) | 60-80 | 60-80 | 0.15-0.45 | 5-15 (Varies widely) | Non-specific binding |
| Albumin (g/L) | 35-50 | 35-50 | 0.08-0.35 | 1-5 | Analyte masking, binding |
| Immunoglobulin G (g/L) | 8-16 | 8-16 | 0.001-0.005 | 0.1-1.0 | Heterophilic antibody source |
| Biotin (nmol/L) | 0.2-0.4 | 0.2-0.4 | ~0.02 | Variable (Diet-dependent) | Streptavidin inhibition |
| Triglycerides (mmol/L) | 0.5-2.3 | 0.5-2.3 | <0.1 | High in certain tissues | Increased viscosity, turbidity |
| Rheumatoid Factor (IU/mL) | <20 (Can be >100 in disease) | <20 | Not typically present | Not typically present | False positive signal |
| Protease Activity | Low | Low (inhibited by EDTA) | Very Low | High (Tissue-specific) | Antibody/Analyte degradation |
Experimental Protocols for Interference Assessment and Mitigation
Protocol 4.1: Spiking and Recovery Experiment
Purpose: To quantitatively determine matrix-induced signal suppression/enhancement. Materials: Analyte-free matrix (preferably stripped), native matrix samples, high-purity analyte stock, calibrator diluent, ELISA kit. Procedure:
- Prepare a series of analyte spikes at low, mid, and high concentrations within the assay's dynamic range.
- Spike the analyte into the neat matrix and into the recommended calibrator diluent (control).
- Perform the ELISA in duplicate for all spiked samples and controls.
- Calculate percent recovery:
(Measured concentration in matrix / Measured concentration in diluent) x 100%. - Acceptance Criterion: Recovery between 80-120% is typically acceptable for validation.
Protocol 4.2: Linear Dilution Test (Parallelism)
Purpose: To confirm the immunoreactivity of the endogenous analyte is identical to the calibrator. Materials: Native sample with high endogenous analyte level, assay calibrator diluent. Procedure:
- Dilute the native sample serially (e.g., 1:2, 1:4, 1:8) using the calibrator diluent.
- Run the ELISA on all dilutions.
- Plot the measured concentration (corrected for dilution factor) against the dilution factor.
- A linear, horizontal line indicates no matrix interference. Non-linearity indicates interference.
Protocol 4.3: Interference Blocking Reagent (IBR) Treatment
Purpose: To neutralize heterophilic antibody and RF interference. Materials: Sample, commercial heterophilic blocking reagent (HBR) or mixture of non-specific animal IgGs and inert polymers. Procedure:
- Incubate the sample with HBR (following manufacturer's protocol, typically a 1-2 hour pre-incubation).
- Run the treated sample alongside an untreated aliquot.
- A significant change (typically reduction) in measured concentration in the treated sample indicates presence of heterophilic interference.
Protocol 4.4: Tissue Homogenate Preparation Protocol
Purpose: To generate a consistent, clarified lysate while minimizing interference generation. Materials: Fresh/frozen tissue, homogenization buffer (e.g., PBS with 1% Triton X-100, protease inhibitors, 1mM PMSF), mechanical homogenizer (sonicator or bead mill), centrifuge. Procedure:
- Weigh tissue and add cold homogenization buffer (typically 9 mL/g tissue for 10% w/v homogenate).
- Homogenize on ice with 3-5 bursts of 10-15 seconds.
- Centrifuge at 10,000 x g for 10 minutes at 4°C.
- Collect the supernatant (clarified homogenate). Aliquot and store at -80°C. Note: Centrifugation at 100,000 x g may be required for membrane-bound targets.
Visual Workflows and Pathways
Workflow for Addressing ELISA Matrix Interferences
Mechanism of Heterophilic Interference and Blocking
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Mitigating Matrix Interferences in ELISA
| Reagent/Solution | Primary Function | Application Notes |
|---|---|---|
| Analyte-Depleted/Stripped Matrix | Provides an interference-matched background for preparing calibration standards. | Use the same matrix as test samples (e.g., stripped serum). Critical for accurate standard curves. |
| Heterophilic Blocking Reagent (HBR) | Contains inert animal immunoglobulins and polymers to saturate heterophilic antibodies. | Add during sample pre-incubation. Effective against human anti-mouse antibodies (HAMA) and RF. |
| Protease Inhibitor Cocktail | Broad-spectrum inhibition of serine, cysteine, aspartic proteases, and aminopeptidases. | Essential for tissue homogenates. Add fresh to lysis/homogenization buffer. |
| Non-Ionic Detergent (e.g., Tween-20, Triton X-100) | Reduces non-specific hydrophobic interactions by blocking plastic and coating proteins. | Standard in assay wash buffers (0.05% Tween-20). Higher concentrations (0.1-1%) in homogenization buffers. |
| Carrier Proteins (BSA, Casein) | Competes for non-specific binding sites on the microplate well and assay components. | Used in sample diluents and antibody conjugation buffers (typically 0.1-1% BSA). |
| Polymer-based Clarification Reagents | Aggregates lipids and particulates for removal via centrifugation. | Useful for lipemic or turbid serum/plasma samples prior to assay. |
| Affinity Removal Columns | Specifically removes high-abundance proteins (e.g., albumin, IgG) that may mask low-level targets. | Used for sample pre-fractionation when targeting low-abundance biomarkers in serum/plasma. |
Within the rigorous framework of biomarker validation research, the enzyme-linked immunosorbent assay (ELISA) remains a cornerstone methodology. The reliability and analytical sensitivity of any ELISA are fundamentally governed by the precise optimization of its core parameters. This whitepaper, situated within a broader thesis on ELISA principles, provides an in-depth technical guide to optimizing three interdependent pillars: antibody pair selection, blocking strategy, and incubation conditions. Success in these areas is critical for minimizing background noise, maximizing specific signal, and ensuring the generation of robust, reproducible data for pre-clinical and clinical research.
Antibody Pair Screening
The selection of a matched antibody pair (capture and detection) is the single most critical factor in developing a sensitive and specific sandwich ELISA.
Key Considerations:
- Epitope Specificity: Antibodies must bind to non-overlapping epitopes on the target antigen to form the "sandwich."
- Affinity & Avidity: High-affinity antibodies improve sensitivity and reduce incubation times.
- Cross-Reactivity: Minimal cross-reactivity with homologous proteins or matrix components is essential for specificity.
Experimental Protocol for Pair Screening:
- Plate Coating: Coat microplate wells with a range of potential capture antibodies (1-10 µg/mL in carbonate-bicarbonate buffer, pH 9.6) overnight at 4°C.
- Blocking: Block with a standard protein-based blocker (e.g., 1% BSA, 5% non-fat dry milk, or 3% BSA in PBS) for 2 hours at room temperature (RT).
- Antigen Incubation: Add a dilution series of the recombinant target antigen and a sample diluent (e.g., pooled normal serum/plasma) as a matrix control. Incubate 2 hours at RT.
- Detection Antibody Incubation: Add candidate detection antibodies, each conjugated to biotin or horseradish peroxidase (HRP), at a predetermined starting concentration. Incubate 1-2 hours at RT.
- Signal Development: If using biotinylated antibodies, add streptavidin-HRP. Develop with TMB substrate, stop with acid, and read absorbance at 450 nm.
- Data Analysis: Evaluate pairs based on signal-to-noise ratio (SNR), dynamic range, and lowest limit of detection (LLOD). The optimal pair delivers the highest SNR across the antigen dilution series.
Table 1: Quantitative Metrics for Evaluating Antibody Pairs
| Antibody Pair | LLOD (pg/mL) | Upper LOQ (ng/mL) | Signal (at 1 ng/mL) | Background (Zero Antigen) | SNR (at 1 ng/mL) | Matrix Recovery (%) |
|---|---|---|---|---|---|---|
| Capture A / Detection X | 15.2 | 5.1 | 2.850 | 0.082 | 34.8 | 102 |
| Capture A / Detection Y | 8.5 | 8.3 | 3.120 | 0.095 | 32.8 | 98 |
| Capture B / Detection X | 25.7 | 3.8 | 1.950 | 0.210 | 9.3 | 115 |
| Capture B / Detection Y | 5.1 | 10.2 | 3.450 | 0.065 | 53.1 | 105 |
Optimization of Blocking Agents
Blocking prevents non-specific adsorption of detection components to the plate and immobilized capture antibody, a major source of background.
Common Blocking Agents & Mechanisms:
- Protein-Based (Inert): BSA, casein, non-fat dry milk. They physically occupy hydrophobic binding sites.
- Protein-Based (Serum): Normal serum from the host species of the detection antibody. It blocks anti-species immunoglobulin interactions.
- Non-Protein-Based: Synthetic polymers (e.g., PBS-Tween 20, Synblock). They reduce non-specific binding without introducing interfering biomolecules.
Experimental Protocol for Blocking Comparison:
- Coat plates with optimal capture antibody.
- Blocking: Divide plates and block with different candidate solutions (see Table 2) for 2 hours at RT.
- Perform the ELISA protocol using a high matrix sample (e.g., 50% serum) and a zero antigen control (matrix only).
- Compare the background signal and the SNR for a low-concentration antigen spike in matrix.
Table 2: Performance of Common Blocking Agents
| Blocking Solution | Composition | Background (OD 450nm) | Signal (Low Antigen Spike) | SNR | Risk of Interference |
|---|---|---|---|---|---|
| 1% BSA / PBS | 1% Bovine Serum Albumin in PBS | 0.075 | 0.320 | 4.3 | Low (if IgG-free) |
| 5% NFDM / PBS | 5% Non-Fat Dry Milk in PBS | 0.055 | 0.290 | 5.3 | High (may contain biotin) |
| 3% BSA / 5% Serum / PBS | 3% BSA + 5% Normal Serum* | 0.030 | 0.350 | 11.7 | Medium |
| 1% Casein / PBS | 1% Hammarsten Casein in PBS | 0.065 | 0.300 | 4.6 | Low |
| Commercial Block Buffer | Proprietary polymer blend | 0.040 | 0.310 | 7.8 | Low |
*Serum species should match the detection antibody host (e.g., goat serum for a goat detection antibody).
Optimization of Incubation Conditions
Time and temperature govern the kinetics of antigen-antibody binding, directly impacting assay sensitivity and throughput.
Key Variables:
- Temperature: Room temperature (RT, ~22-25°C) vs. 37°C. Higher temperature accelerates kinetics but may increase non-specific binding.
- Duration: Must be sufficient to reach equilibrium binding for maximum sensitivity.
- Agitation: Orbital shaking can improve binding efficiency and reduce incubation times by 25-50%.
Experimental Protocol for Kinetics Profiling:
- Set up a standard ELISA with a mid-range antigen concentration.
- For the antigen incubation step, test combinations of time (30, 60, 120, 180 min) and temperature (RT, 37°C), with and without agitation (~500 rpm).
- Plot the signal development over time for each condition to identify the point of diminishing returns.
Table 3: Impact of Incubation Conditions on Assay Performance
| Condition (Antigen Step) | Time to 90% Max Signal | Final Max Signal (OD) | Intra-Assay CV (%) | Recommended Use Case |
|---|---|---|---|---|
| RT, Static | 180 min | 2.85 | 8.2 | Standard protocol, overnight possible |
| RT, Agitated | 90 min | 2.95 | 6.5 | Improved precision, faster runtime |
| 37°C, Static | 75 min | 2.70 | 10.5 | Fast turnaround, potential for higher background |
| 37°C, Agitated | 45 min | 2.98 | 5.1 | High-throughput, optimized assays |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| High-Purity BSA (IgG-Free) | A standard blocking and diluent protein; IgG-free grade prevents interference from bovine immunoglobulins. |
| Normal Sera (Multiple Species) | Used in block/diluent buffers to block heterophilic and anti-species antibody interferences. |
| Monoclonal Antibody Pairs (Matched) | Pre-validated pairs guaranteed to recognize distinct epitopes, reducing development time. |
| HRP/TMB Detection System | A sensitive, ready-to-use chromogenic system (enzyme + substrate) for signal generation. |
| Streptavidin-Poly-HRP Conjugates | Provides significant signal amplification (>1 HRP:1 biotin) versus traditional streptavidin-HRP. |
| Stabilized Coating Buffer (pH 9.6) | Ensures consistent, high-efficiency passive adsorption of capture antibodies to polystyrene plates. |
| Commercial ELISA Block/Stabilizer | Optimized, ready-to-use buffers designed to minimize background in complex matrices. |
| Microplate Shaker/Incubator | Provides controlled agitation and temperature for kinetically optimized incubations. |
Visualizations
Diagram 1: Sandwich ELISA Optimization Workflow
Diagram 2: Key Antibody-Antigen Interactions & Interferences
Improving Sensitivity (LOD/LOQ) and Dynamic Range for Low-Abundance Biomarkers
Within the framework of a thesis on ELISA principles for biomarker validation research, the accurate quantification of low-abundance biomarkers presents a significant analytical challenge. The limit of detection (LOD) and limit of quantification (LOQ) define the lowest concentrations that can be reliably detected and measured, respectively, while the dynamic range determines the span of concentrations over which accurate measurements can be made. For biomarkers present at picogram or femtogram per milliliter levels—common in early disease detection, neurological studies, and pharmacodynamics—conventional ELISA formats often fall short. This technical guide explores advanced methodologies to push these analytical boundaries, ensuring robust data for critical research and drug development decisions.
Core Strategies for Enhanced Sensitivity
Signal Amplification Systems
Moving beyond traditional enzyme-substrate systems (e.g., HRP/TMB) is paramount. Recent innovations employ catalytic nanoparticle labels, DNA-amplified detection, and enhanced chemiluminescence.
Detailed Protocol: DNA-Amplified ELISA (Immuno-PCR)
- Conjugate Preparation: Link a specific oligonucleotide (e.g., a 60-80 base single-stranded DNA) to a detection antibody (polyclonal or monoclonal) using a heterobifunctional crosslinker (e.g., SMCC).
- Standard ELISA: Perform the capture and sample incubation steps as in a standard sandwich ELISA.
- Detection Incubation: Incubate with the DNA-labeled detection antibody. Wash stringently.
- DNA Amplification & Detection: Use the conjugated DNA as a template for real-time quantitative PCR (qPCR) with SYBR Green or a TaqMan probe. The resulting Ct value or fluorescence intensity correlates with the amount of captured biomarker.
Improved Assay Kinetics and Surface Chemistry
Optimizing the solid phase is critical for capturing rare analytes.
- High-Affinity Capture Molecules: Use recombinant monoclonal antibodies with sub-nanomolar affinity, affibodies, or aptamers.
- Oriented Immobilization: Employ Protein A/G, anti-Fc, or biotin-streptavidin systems to present capture antibodies in a uniform, accessible orientation.
- Low-Binding Surfaces: Use plates with specialized polymer coatings to minimize nonspecific adsorption (NSB), effectively lowering background noise.
Pre-Analytical Enrichment and Sample Prep
- Immunodepletion: Remove top 12-14 high-abundance serum proteins (e.g., albumin, IgG) using spin columns or magnetic beads to reduce masking effects.
- Immunoaffinity Enrichment: Use magnetic beads conjugated with the target-specific capture antibody to "pull down" the biomarker from a large sample volume (e.g., 1 mL) and elute it into a small assay volume (e.g., 50 µL), achieving a 20-fold pre-concentration.
Experimental Protocols
Protocol 1: Single Molecule Counting (SMC) ELISA using Planar Waveguide Technology
- Plate Coating: Coat a planar waveguide microplate with high-affinity capture antibody (2 µg/mL, 100 µL/well) overnight at 4°C.
- Blocking: Block with a proprietary protein-free buffer containing stabilizing agents for 2 hours.
- Sample/Biomarker Incubation: Add samples and standards diluted in assay buffer. Incubate for 3 hours with shaking.
- Detection Antibody Incubation: Add a biotinylated detection antibody for 1 hour. Wash.
- Labeling: Incubate with streptavidin-conjugated fluorescent dye (e.g., phycoerythrin) for 30 minutes. Wash.
- Reading & Analysis: Scan the waveguide surface with a laser excitation source. Individual fluorescent immunocomplexes are counted as discrete events by a CCD camera. The count per unit area is directly proportional to analyte concentration.
Protocol 2: Electrochemiluminescence (ECL)-Based Immunoassay
- Bead Coating: Covalently couple capture antibodies to magnetic, conductive beads (e.g., carbon-coated).
- Assay Assembly: In a multi-array plate, mix sample, capture beads, and a detection antibody labeled with a Ruthenium (Ru) complex. Incubate to form a sandwich.
- Magnetic Separation: Apply a magnet to immobilize beads and wash.
- Signal Generation: Place the plate in an ECL reader containing Tripropylamine (TPA) buffer. Apply an electrical potential. The Ru label on beads in proximity to the electrode undergoes a redox reaction with TPA, emitting photons at ~620 nm.
- Measurement: A photomultiplier tube (PMT) counts the emitted photons. The key advantage is near-zero background, as the signal is triggered electrically only from labels on the bead surface.
Table 1: Comparison of Advanced ELISA Platform Performance for Low-Abundance Biomarkers
| Platform/Technique | Typical LOD Improvement vs. Std. ELISA | Effective Dynamic Range | Key Principle | Best for |
|---|---|---|---|---|
| Enhanced Chemiluminescence (CL) | 5-10 fold | 3-4 logs | Ultra-sensitive substrate with signal enhancers | High-throughput labs, standard plate readers |
| Electrochemiluminescence (ECL) | 10-100 fold | 5-6 logs | Electrical triggering of luminescence, low background | Multiplexing, low background critical |
| Immuno-PCR (DNA-Amplified) | 100-1000 fold | 4-5 logs | PCR amplification of DNA reporter tag | Ultimate sensitivity, specialized equipment |
| Single Molecule Counting (SMC) | 100-1000 fold | 4 logs | Digital counting of individual immunocomplexes | Ultra-low abundance, requires specific reader |
| Plasmonic ELISA (Nanozyme) | 50-200 fold | 3-4 logs | Nanoparticle catalysts generate precipitate | Colorimetric readout, high sensitivity |
Table 2: Impact of Pre-Analytical Enrichment on Assay Sensitivity
| Enrichment Method | Sample Volume Input | Elution Volume | Concentration Factor | Expected LOD Improvement* | Notes |
|---|---|---|---|---|---|
| High-Abundance Protein Depletion | 20 µL | 20 µL | None (clean-up) | 2-5 fold | Reduces interference, not concentration. |
| Magnetic Bead Immunoaffinity | 500 µL - 1 mL | 50 µL | 10-20 fold | ~10 fold | Target-specific, can multiplex. |
| Solid Phase Extraction (SPE) | 100 µL | 20 µL | 5 fold | ~5 fold | General for peptides/small molecules. |
*Improvement is multiplicative with a sensitive detection platform.
Visualizations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for High-Sensitivity Biomarker Assays
| Item | Function & Rationale | Example/Notes |
|---|---|---|
| High-Affinity, Low-Lot-Variation Antibody Pairs | Critical for specificity and LOD. Recombinant monoclonals ensure consistency. | Validate via surface plasmon resonance (SPR) for KD < 1 nM. |
| Low-Binding Microplates | Minimizes NSB of proteins and detection reagents, lowering background noise. | Plates with polymer (e.g., polyvinyl alcohol) or modified polystyrene coatings. |
| Signal Generation: Ultra-Sensitive ECL Substrate | Provides amplified luminescent signal with high signal-to-noise ratio for plate readers. | Commercial kits with enhanced luminol/peroxide formulations + enhancers. |
| Signal Generation: Ruthenium-labeled Detection Ab | Tag for ECL systems; stable, allows for electrical triggering of signal. | Often custom-conjugated or available in kit form from platform providers. |
| Magnetic Beads for Enrichment | Solid support for immunocapture from large volumes. Enables efficient washing. | Tosylactivated or carboxylated beads for covalent antibody coupling. |
| DNA Labeling Kit (for Immuno-PCR) | Creates stable antibody-DNA conjugates without disrupting immunoreactivity. | Heterobifunctional crosslinkers (e.g., SMCC) or click chemistry kits. |
| Protein-Free Blocking & Assay Buffers | Reduces background from non-specific binding of conjugate to blocking proteins. | Based on polymers, carbohydrates, or engineered protein fragments. |
| Precision Liquid Handling System | Essential for reproducibility when working with small volumes and concentrated samples. | Positive-displacement or air-displacement pipettes with <2% CV. |
Within the broader thesis on ELISA principles for biomarker validation, the optimization of precision—both intra-assay (within-run) and inter-assay (between-run)—is foundational. Reproducible data is the bedrock of credible research, essential for clinical diagnostics, drug development, and regulatory submission. This guide details technical strategies to minimize assay variability and achieve robust, reliable results.
Fundamental Concepts: Precision in ELISA
Intra-Assay Precision measures the repeatability of results within a single plate or run under identical conditions and time. It is affected by pipetting technique, reagent homogeneity, and plate washing. Inter-Assay Precision measures the reproducibility across different runs, operators, days, or lot numbers of reagents. It is influenced by environmental conditions, reagent stability, calibration, and instrument performance. The coefficient of variation (%CV) is the key metric: %CV = (Standard Deviation / Mean) × 100.
Quantitative Precision Benchmarks
Acceptable precision thresholds depend on the assay stage and application.
Table 1: Typical Precision Performance Targets for Biomarker ELISA
| Precision Type | Development Phase | Target %CV | Key Influencing Factors |
|---|---|---|---|
| Intra-Assay | Assay Development | <10% | Pipetting error, plate effects, incubation timing. |
| Intra-Assay | Validated Method | <8% | Optimized protocol, automated liquid handling. |
| Inter-Assay | Assay Development | <15% | Reagent lot variation, day-to-day operator difference. |
| Inter-Assay | Validated Method | <12% | Standardized SOPs, calibrated equipment, QC samples. |
| Total Precision (Overall) | GLP/GCP Context | <20%* | Sum of all random error sources. *FDA/EMA guidelines often recommend ≤20-25% for ligand-binding assays. |
Experimental Protocols for Precision Assessment
Protocol 3.1: Intra-Assay Precision Experiment
Objective: To determine within-plate variability. Materials: A single plate, one lot of all reagents, one operator. Method:
- Prepare a minimum of three replicates each of at least three analyte concentrations (low, mid, high QC samples) across the plate. A 5-8 replicate per level is recommended.
- Perform the entire ELISA protocol according to the standard operating procedure (SOP).
- Calculate the mean, standard deviation (SD), and %CV for each concentration level across its replicates. Analysis: The mean %CV across all levels represents the intra-assay precision.
Protocol 3.2: Inter-Assay Precision Experiment
Objective: To determine between-run variability over time. Materials: Multiple plates, multiple reagent lots (if applicable), multiple operators/days. Method:
- Over at least 3-5 independent runs (different days), assay the same set of low, mid, and high QC samples in replicates (e.g., duplicates or triplicates) per run.
- Use the same SOP but allow for normal variations (new reagent aliquots, different calibrator preparations, different operators).
- For each QC level, pool all results from all runs. Calculate the overall mean, SD, and %CV. Analysis: The %CV for each pooled QC level represents the inter-assay precision.
Optimization Strategies
Minimizing Intra-Assay Variability
- Pipetting: Use calibrated, positive displacement pipettes for viscous samples/reagents. Implement reverse pipetting for surfactants.
- Mixing: Ensure all reagents and samples are thoroughly mixed and centrifuged before use.
- Incubation: Use plate sealers, maintain consistent temperature, and ensure plate shaker speed is standardized.
- Washing: Employ automated plate washers. Validate wash efficiency and consistency across all wells.
Minimizing Inter-Assay Variability
- Reagent Management: Use large, single lots of critical reagents (e.g., antibody pairs). Aliquot and store at optimal temperatures.
- Calibration Curve: Include a full standard curve in every run. Monitor curve fit parameters (R², EC50).
- Quality Control (QC) Samples: Include defined QC samples (low, mid, high) in every run. Plot on Levey-Jennings charts to monitor trend and shift.
- SOPs & Training: Use detailed, step-by-step SOPs. Ensure all operators are trained and demonstrate proficiency.
Visualizing Precision Optimization Workflow
Diagram Title: ELISA Precision Assessment & Optimization Cycle
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagent Solutions for Precision Optimization
| Item | Function & Role in Precision | Optimization Tip |
|---|---|---|
| Matched Antibody Pair | Capture and detection specificity. High-affinity antibodies reduce background and variability. | Source from a single, large lot. Characterize affinity (KD) before use. |
| Calibrator Standard | Creates the reference curve for quantification. Inaccuracy here propagates to all samples. | Use an internationally recognized reference material if available. Prepare fresh aliquots. |
| Quality Control (QC) Samples | Monitor run-to-run performance. Critical for inter-assay precision. | Use pooled patient samples or spiked matrix at low, mid, high concentrations. |
| Plate Coating Buffer | Immobilizes capture antibody. Inconsistent coating leads to variable signal. | Optimize pH and ionic strength (e.g., Carbonate-Bicarbonate buffer, pH 9.6). Use fresh. |
| Blocking Buffer | Covers non-specific sites. Reduces background noise and improves signal-to-noise ratio. | Compare proteins (BSA, casein). Use sufficient volume and incubation time. |
| Detection Enzyme Conjugate | Generates measurable signal (colorimetric, chemiluminescent). Lot-to-lot variation is critical. | Titrate for optimal dilution. Use stabilized, ready-to-use formulations if possible. |
| Wash Buffer | Removes unbound material. Inconsistent washing is a major source of high CVs. | Include a mild detergent (e.g., 0.05% Tween-20). Use automated washers for uniformity. |
| Substrate | Enzyme reaction component. Signal generation must be stable and linear. | For HRP, use single-component TMB. For AP, use pNPP. Protect from light. |
| Stopping Solution | Halts enzyme reaction. Timing affects final optical density (OD). | Add in the same order as substrate addition, with consistent timing. |
Establishing Assay Validity: Meeting Regulatory Standards and Comparing Platforms
Within biomarker validation research, particularly using Enzyme-Linked Immunosorbent Assay (ELISA) principles, a rigorous validation framework is non-negotiable. This technical guide details the core analytical parameters—Specificity, Precision, Accuracy, Sensitivity, and Robustness—that underpin credible, reproducible, and translatable data. Adherence to this framework ensures that biomarker assays meet the stringent requirements for preclinical and clinical decision-making in drug development.
The identification and quantification of biomarkers via ELISA is foundational to modern therapeutic research. However, the utility of any biomarker is contingent upon the analytical validity of the assay used to measure it. This guide delineates the key validation parameters, framing them as essential checkpoints within a broader thesis on developing fit-for-purpose ELISAs. These parameters collectively ensure that an assay reliably detects the intended analyte (e.g., a cytokine, autoantibody, or therapeutic protein) amidst a complex biological matrix, providing data that is accurate, precise, and sensitive enough to inform research hypotheses and development go/no-go decisions.
Deconstructing the Key Validation Parameters
Specificity
Specificity confirms that the assay signal is generated solely by the target analyte. For sandwich ELISAs, this depends on the unique binding of two antibodies.
- Experimental Protocol (Cross-Reactivity): Spike known concentrations of structurally similar interferents (e.g., homologs, metabolites, related proteins) into the sample matrix. Run the ELISA. Calculate the apparent concentration measured for each interferent relative to its actual concentration. Less than 5% cross-reactivity is typically required for a specific assay.
- Experimental Protocol (Parallelism): Serially dilute a native sample (e.g., serum) with a high concentration of the analyte and a calibrator spiked into the assay matrix. Plot the dose-response curves. Parallelism (similar slopes) indicates the immunoassay recognizes the native and recombinant forms equivalently, supporting specificity in the biological context.
Precision
Precision is the closeness of agreement between repeated measurements. It is stratified into:
- Intra-assay Precision (Repeatability): Variability within a single plate/run.
- Inter-assay Precision (Intermediate Precision): Variability across different days, operators, or lots of reagents.
- Experimental Protocol: Analyze at least three analyte concentrations (low, mid, high QC samples) with a minimum of 5 replicates per level in one run (intra-assay) and over at least 3 separate runs (inter-assay). Express as Coefficient of Variation (%CV).
Accuracy
Accuracy reflects how close the measured value is to the true value. It is often assessed through recovery experiments.
- Experimental Protocol (Spike/Recovery): Spike a known quantity of pure analyte into the native sample matrix at multiple levels across the assay range. Measure the concentration via ELISA. Calculate % Recovery = (Measured Concentration / Expected Concentration) * 100.
Sensitivity
Sensitivity defines the lowest amount of analyte that can be reliably distinguished from zero. The key metrics are the Limit of Detection (LOD) and Limit of Quantification (LOQ).
- Experimental Protocol (LOD & LOQ): Measure a zero standard (blank matrix) at least 20 times. LOD is typically calculated as the mean blank signal + 3 standard deviations. LOQ is the mean blank signal + 10 standard deviations, and must be validated by demonstrating a %CV ≤ 20% (or a predefined criterion) at that concentration.
Robustness
Robustness is the capacity of the assay to remain unaffected by small, deliberate variations in method parameters, indicating reliability under normal operational changes.
- Experimental Protocol: Introduce minor, deliberate changes (e.g., incubation time ±5%, temperature ±2°C, reagent preparation time variance, different microplate washer settings). Assess the impact on key performance outputs (e.g., OD values of QC samples, calculated concentrations).
Table 1: Target Acceptance Criteria for Key Validation Parameters in a Fit-for-Purpose Biomarker ELISA
| Parameter | Sub-Parameter | Typical Acceptance Criterion | Example Experimental Outcome* |
|---|---|---|---|
| Specificity | Cross-Reactivity | ≤ 5% for key interferents | Interferent X: 2.1% cross-reactivity |
| Parallelism | % Bias < 20% across dilutions | Mean bias: 12% (Slope ratio: 0.95) | |
| Precision | Intra-assay (%CV) | ≤ 10-15% (LLOQ); ≤ 10% (other) | LQC: 8.2% CV; HQC: 6.5% CV |
| Inter-assay (%CV) | ≤ 15-20% (LLOQ); ≤ 15% (other) | LQC: 12.4% CV; HQC: 9.8% CV | |
| Accuracy | % Recovery | 80-120% of expected value | Mean recovery across levels: 102% |
| Sensitivity | Limit of Blank (LoB) | Not applicable (derived value) | Meanblank = 0.045 OD, SDblank = 0.005 |
| LOD | Meanblank + 3*SDblank | 0.060 OD (0.5 pg/mL) | |
| LOQ | Meanblank + 10*SDblank; CV ≤20% | 0.095 OD (1.0 pg/mL), CV=18% | |
| Robustness | Parameter Variation | % Change in QC value < 15% | Incubation time ±5 min: Max 8% change |
*Example data is illustrative.
Table 2: Example Precision Profile Data from an Interleukin-6 ELISA Validation
| QC Level | Nominal Conc. (pg/mL) | Intra-assay (n=10) | Inter-assay (n=5 runs) | ||
|---|---|---|---|---|---|
| Mean (pg/mL) | %CV | Mean (pg/mL) | %CV | ||
| Low | 15 | 15.8 | 11.5 | 16.2 | 14.1 |
| Medium | 100 | 98.5 | 7.2 | 101.3 | 9.8 |
| High | 400 | 390.2 | 5.1 | 405.6 | 8.3 |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Biomarker ELISA Validation
| Item | Function in Validation |
|---|---|
| Matched Antibody Pair (Capture/Detection) | The core reagents defining specificity. Must be characterized for affinity and lack of cross-reactivity. |
| Recombinant Purified Target Antigen | Used for generating the standard curve, spiking for recovery experiments, and specificity challenges. |
| Well-Characterized Biological Matrix | Pooled, analyte-depleted matrix (e.g., serum, plasma, CSF) for preparing calibrators and QCs to mimic real samples. |
| Validated Assay Buffer System | Includes blocking agents and stabilizers to minimize non-specific binding and maintain analyte integrity. |
| High-Sensitivity Detection System | e.g., HRP-Streptavidin with ultra-sensitive chemiluminescent substrate to achieve required LOD/LOQ. |
| Precision QC Samples | Low, mid, and high concentration samples in matrix, aliquoted and stored for longitudinal precision testing. |
| Interferent Stocks | Solutions of potential cross-reactants (e.g., homologous proteins, common matrix components like biotin, lipids). |
Visualizing the Validation Workflow and Relationships
ELISA Validation Parameter Workflow
Validation Experiment Flow
Linearity, Dilutional Parallelism, and Spike-and-Recovery Experiments
Within the rigorous framework of biomarker validation research using Enzyme-Linked Immunosorbent Assay (ELISA), establishing the accuracy and reliability of quantitative measurements is paramount. Three cornerstone analytical experiments—Linearity, Dilutional Parallelism, and Spike-and-Recovery—serve as critical pillars for assessing assay performance in complex biological matrices. These experiments collectively verify that an assay measures the analyte of interest without interference from the sample matrix itself, ensuring data integrity for preclinical and clinical decision-making in drug development.
Core Principles and Experimental Methodologies
Linearity
Linearity evaluates the assay's ability to produce results that are directly proportional to the concentration of the analyte across the declared working range. It confirms the calibration curve is valid.
Protocol:
- Prepare a high-concentration stock of the purified analyte in the assay's diluent/buffer.
- Serially dilute the stock to generate at least 5-7 concentrations spanning the entire claimed range of the assay (e.g., from the Lower Limit of Quantification (LLOQ) to the Upper Limit of Quantification (ULOQ)).
- Run each dilution in replicate (minimum n=2, ideally n=3-4) within a single assay run.
- Plot the observed concentration (or mean signal) against the expected concentration.
- Perform linear regression analysis. Acceptance criteria typically require a coefficient of determination (R²) ≥ 0.99 and the slope to be close to 1 (e.g., 0.90-1.10).
Dilutional Parallelism
Dilutional Parallelism assesses whether an endogenous analyte in a real biological matrix (e.g., serum, plasma, tissue homogenate) behaves identically to the purified calibrator standard when serially diluted. It detects matrix effects that could cause non-proportional recovery.
Protocol:
- Select 3-5 individual donor samples with endogenous analyte concentrations near the ULOQ.
- Spike these samples with a known amount of recombinant analyte if endogenous levels are insufficient ("spike-in").
- Perform serial dilutions (e.g., 1:2, 1:4, 1:8, etc.) of each matrix sample using the assay's prescribed diluent.
- Assay each dilution and the neat sample.
- Calculate the measured concentration for each dilution, correcting for the dilution factor.
- The percent recovery at each dilution is calculated as: (Measured Concentration / Expected Concentration) * 100%.
Acceptance Criteria: Recovery should be within 80-120% (or a lab-defined range) across all dilutions, and the dilution-response curve should be parallel to the standard curve.
Spike-and-Recovery
Spike-and-Recovery experiments determine the accuracy of the assay by measuring the recovery of a known quantity of purified analyte ("spike") added to a sample matrix. It quantifies the impact of matrix interference.
Protocol:
- Prepare a "blank" matrix sample (ideally from multiple individual donors) expected to have low or no endogenous levels of the analyte. If unavailable, use a matrix stripped of the analyte.
- Prepare three different spike concentrations (low, mid, high) within the assay's dynamic range using purified analyte.
- Spike the matrix samples with the analyte solutions. Include a control of the spike in assay diluent (no matrix).
- Assay all samples (spiked matrix, unspiked matrix, spike in diluent) in replicate.
- Calculate Percent Recovery: *Recovery % = [ (Measured concentration in spiked matrix – Measured concentration in unspiked matrix) / Theoretical spike concentration ] * 100%.
Acceptance Criteria: Mean recovery is generally acceptable within 70-130% for complex matrices, with tighter limits (e.g., 80-120%) for more refined assays.
Table 1: Typical Acceptance Criteria and Results for Core Validation Experiments
| Experiment | Key Metric | Target/Acceptance Criteria | Example Outcome (Mean ± SD) |
|---|---|---|---|
| Linearity | Coefficient of Determination (R²) | ≥ 0.990 | 0.998 ± 0.002 |
| Slope of Linearity | 1.00 ± 0.10 | 1.03 ± 0.04 | |
| Dilutional Parallelism | % Recovery across dilutions | 80 – 120% | 95% ± 8% (range: 84-108%) |
| Coefficient of Variation (CV) of recoveries | < 20% | 12% | |
| Spike-and-Recovery | % Recovery (Low Spike) | 70 – 130% | 88% ± 10% |
| % Recovery (Mid Spike) | 80 – 120% | 102% ± 6% | |
| % Recovery (High Spike) | 80 – 120% | 97% ± 5% | |
| Inter-donor CV of recovery | < 25% | 15% |
Visualizing Experimental Workflows and Relationships
Title: ELISA Matrix Validation Experiment Decision Flow
Title: Spike Recovery & Dilution Parallelism Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for ELISA Matrix Validation Experiments
| Item | Function in Validation | Critical Specification/Note |
|---|---|---|
| ELISA Kit / Matched Antibody Pair | Core capture and detection of the target analyte. | Ensure specificity for the target biomarker; check cross-reactivity. |
| Recombinant Purified Analyte Standard | Used to generate standard curve, for spiking, and linearity dilutions. | High purity and confirmed activity; should be identical to endogenous form. |
| Matrix-Matched Diluent / Assay Buffer | Diluent for standards and samples. | Optimized to minimize matrix interference; often contains blockers (BSA, casein). |
| Analyte-Depleted or "Blank" Matrix | Negative control for spike-and-recovery. | Ideally pooled from multiple donors with undetectable endogenous analyte. |
| Native Biological Samples | For parallelism studies. | Should be from relevant species and disease state; use individual donors (n≥3-5). |
| Microplate Washer & Reader | For automated washing and absorbance detection. | Calibrated and maintained for consistent performance. |
| Precision Pipettes & Liquid Handler | For accurate serial dilutions and reagent dispensing. | Regularly calibrated; use low protein-binding tips for analyte. |
| Data Analysis Software | For regression analysis, curve fitting, and statistical calculation. | Use 4- or 5-parameter logistic (4PL/5PL) for standard curves. |
The systematic execution of linearity, dilutional parallelism, and spike-and-recovery experiments forms an indispensable triad in the ELISA biomarker validation process. These tests move beyond simple standard curve assessment to rigorously interrogate how the assay performs in the complex, variable environment of real-world samples. For researchers and drug development professionals, data from these experiments provides the foundational confidence that observed concentration changes reflect true biology, not methodological artifact, thereby supporting robust scientific conclusions and translational decisions.
Within the thesis on ELISA principles for biomarker validation research, establishing robust assay performance is only the first step. The reliability of any biomarker measurement is fundamentally dependent on the integrity of the analyte from sample collection to analysis. This guide details the critical practice of stability assessments, a series of controlled experiments designed to evaluate how storage conditions affect biomarker concentration and detectability. The goal is to define standardized handling protocols that ensure data generated by ELISA and other immunoassays accurately reflects in vivo biology rather than ex vivo degradation.
Core Stability Study Designs
Stability is evaluated under conditions mimicking pre-analytical variables. Key experiments include:
- Freeze-Thaw Stability: Assesses the effect of repeated cycling between frozen and thawed states.
- Short-Term (Bench-Top) Stability: Defines the allowable time a sample can remain at ambient or processing temperatures (e.g., 4°C, room temperature).
- Long-Term Stability: Determines the maximum safe storage duration at the recommended long-term temperature (e.g., -80°C).
- Post-Preparative Stability: Evaluates the integrity of prepared samples or reagents (e.g., assay calibrators, ready-to-use lysates) in the storage conditions used during an analytical run.
Experimental Protocols for Key Assessments
Protocol 1: Freeze-Thaw Stability Assessment
- Objective: To determine the number of freeze-thaw cycles a biomarker can withstand before significant degradation.
- Methodology:
- Pool quality control (QC) samples (high, mid, low concentration) in sufficient volume.
- Aliquot the pooled QC samples into multiple vials.
- Subject aliquots to 1, 2, 3, 4, and 5 freeze-thaw cycles. One set of aliquots serves as the "zero-cycle" baseline, analyzed fresh without freezing.
- For each cycle, thaw samples completely at room temperature or in a refrigerator (as per intended use), then re-freeze at the target storage temperature (e.g., -80°C) for a minimum of 12 hours.
- After completing the designated cycles, analyze all samples in a single, randomized ELISA run to minimize inter-assay variation.
- Calculate the mean measured concentration for each cycle group. Stability is confirmed if the mean recovery for all cycles is within ±15% (or a pre-defined acceptance criteria) of the baseline (zero-cycle) mean.
Protocol 2: Short-Term Temperature Stability
- Objective: To establish the allowable hold time for samples at various processing temperatures.
- Methodology:
- Prepare fresh QC sample pools (high, mid, low).
- Aliquot into multiple vials and store them at the test conditions: Room Temperature (e.g., 20-25°C), Refrigerated (2-8°C), and optionally on wet ice (0-4°C).
- Remove and analyze replicate aliquots at predefined time points (e.g., 0, 1, 2, 4, 8, 24, 48 hours). The "0-hour" time point is analyzed immediately.
- Store a reference set of aliquots at -80°C immediately upon preparation.
- Analyze all time-point samples and the -80°C reference samples in the same ELISA run.
- Plot concentration vs. time. The stability threshold is the time point at which the mean recovery falls outside the pre-defined acceptance range (e.g., 85-115%) compared to the -80°C reference.
Table 1: Common Stability Study Types and Acceptance Criteria
| Study Type | Test Conditions | Key Measurement | Typical Acceptance Criteria |
|---|---|---|---|
| Freeze-Thaw | -80°C to Thaw Temp, repeated cycles | Mean Recovery per Cycle | 85% - 115% of baseline (Cycle 0) |
| Short-Term | 2-8°C, RT (20-25°C) | Mean Recovery per Time Point | 85% - 115% of reference (-80°C) |
| Long-Term | -80°C, -20°C | Trend over months/years | 85% - 115% of initial (T=0); statistical trend analysis |
| Post-Preparative | Autosampler temp (e.g., 4-10°C) | Mean Recovery over run duration | 85% - 115% of initial prepared state |
Table 2: Example Stability Data for a Hypothetical Cytokine (IL-6) in Plasma
| Condition | Time/Cycle | Mean Conc. (pg/mL) | % Recovery vs. Baseline | Stable? (85-115%) |
|---|---|---|---|---|
| Baseline (Ref) | T=0 at -80°C | 150.0 | 100% | N/A |
| 2-8°C Stability | 24 hours | 147.2 | 98.1% | Yes |
| 48 hours | 141.5 | 94.3% | Yes | |
| 72 hours | 124.1 | 82.7% | No | |
| Freeze-Thaw | Cycle 1 | 148.8 | 99.2% | Yes |
| Cycle 3 | 142.5 | 95.0% | Yes | |
| Cycle 5 | 126.3 | 84.2% | Yes (marginal) |
Visualization of Stability Assessment Workflow
Diagram Title: Stability Assessment Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Biomarker Stability Studies
| Item | Function in Stability Assessments |
|---|---|
| Validated ELISA Kit | Provides the critical immunoassay component with known performance characteristics for accurate biomarker quantification. |
| Matrix-Matched Quality Control (QC) Pools | Samples (high, mid, low conc.) prepared in the same biological matrix (e.g., human serum) as test samples. Essential for realistic stability simulation. |
| Protease & Phosphatase Inhibitor Cocktails | Added during sample processing to halt enzymatic degradation and preserve labile biomarkers (e.g., phospho-proteins). |
| Low Protein-Binding Microtubes & Plates | Minimizes analyte adsorption to plastic surfaces, preventing loss of low-abundance biomarkers during storage and handling. |
| Controlled-Temperature Storage | Programmable freezers (-80°C, -20°C), refrigerators (2-8°C), and cold rooms. Critical for precise environmental control. |
| Stability-Specific Sample Aliquot Tubes | Cryogenic vials with silicone O-rings for secure, long-term storage; pre-labeled for tracking time points/cycles. |
| Data Analysis Software | Tools like SoftMax Pro, PLA, or R for statistical analysis of recovery data and trend determination. |
In the critical pathway of biomarker validation, the enzyme-linked immunosorbent assay (ELISA) has long been the foundational workhorse. Its principles—antigen immobilization, specific antibody binding, and enzymatic signal amplification—form the conceptual bedrock for most modern immunoassays. However, the evolving demands of precision medicine and systems biology, which require the measurement of low-abundance biomarkers in small sample volumes, have driven the development of advanced platforms. This guide deconstructs the core trade-offs between the traditional ELISA and three key technologies—Meso Scale Discovery (MSD), Luminex, and Simoa—framed within the essential context of selecting the optimal tool for rigorous biomarker validation research.
Technology Comparison: Core Principles & Quantitative Metrics
Table 1: Platform Comparison for Biomarker Validation
| Feature | ELISA | MSD (Electrochemiluminescence) | Luminex (xMAP) | Simoa (Single Molecule Array) |
|---|---|---|---|---|
| Core Detection Principle | Colorimetric/fluorimetric absorbance | Electrochemiluminescence | Fluorescence (laser-excited beads) | Fluorescence (digital counting of single molecules) |
| Typical Sensitivity (LLoQ) | pg/mL (10⁻¹² g/mL) | fg–pg/mL (10⁻¹⁵–10⁻¹² g/mL) | pg/mL (10⁻¹² g/mL) | fg/mL (10⁻¹⁸–10⁻¹⁵ g/mL) |
| Multiplexing Capacity | Single-plex | Low- to mid-plex (∼10 plex) | High-plex (∼50–500 plex) | Single-plex to low-plex (∼6 plex) |
| Throughput (Samples/Day) | High (96/384-well) | High (96/384-well) | Very High (96-well, bead-based) | Medium (96-well, automated) |
| Dynamic Range | 2–3 logs | 4–6 logs | 3–4 logs | 3–4 logs |
| Sample Volume Required | 50–100 µL | 25–50 µL | 25–50 µL | < 25 µL |
| Key Advantage | Cost-effective, standardized, high throughput | Excellent sensitivity & range, low background | High multiplexing, sample sparing | Exceptional sensitivity, digital detection |
Table 2: Suitability for Research Phases
| Research Phase | Primary Need | Recommended Platform(s) | Rationale |
|---|---|---|---|
| Discovery Screening | High multiplexing | Luminex, Large MSD Panels | Maximize biomarker candidate identification from minimal sample. |
| Analytical Validation | Sensitivity, precision, robustness | ELISA, MSD, Simoa | ELISA for established markers; MSD/Simoa for low-abundance targets. Requires rigorous QC. |
| Clinical Assay Translation | Standardization, throughput, cost | ELISA, MSD | Well-understood protocols, suitable for clinical lab environments. |
| Ultra-Sensitive Detection | Quantifying trace levels (e.g., neurology) | Simoa | Unmatched sensitivity for cytokines, neuronal biomarkers in plasma/serum. |
Detailed Experimental Protocols
Protocol 1: Standard Sandwich ELISA for Biomarker Validation
- Coating: Dilute capture antibody in carbonate-bicarbonate buffer (pH 9.6). Add 100 µL/well to a 96-well microplate. Incubate overnight at 4°C.
- Washing: Aspirate and wash plate 3x with 300 µL/well of PBS containing 0.05% Tween-20 (PBST).
- Blocking: Add 200 µL/well of blocking buffer (e.g., 5% BSA or casein in PBS). Incubate 1–2 hours at room temperature (RT). Wash 3x with PBST.
- Sample & Standard Incubation: Add 100 µL of diluted sample or calibrator (in assay buffer) per well. Incubate 2 hours at RT with shaking. Wash 3–5x.
- Detection Antibody Incubation: Add 100 µL/well of biotinylated detection antibody (in assay buffer). Incubate 1–2 hours at RT. Wash 3–5x.
- Streptavidin-Enzyme Conjugate: Add 100 µL/well of streptavidin-HRP (diluted in assay buffer). Incubate 30 minutes at RT in the dark. Wash 3–5x.
- Signal Development: Add 100 µL/well of TMB substrate. Incubate 5–30 minutes at RT in the dark.
- Stop & Read: Add 50 µL/well of stop solution (e.g., 1M H₂SO₄). Read absorbance immediately at 450 nm with a reference at 620 nm.
Protocol 2: Simoa (Digital ELISA) Workflow for Ultra-Sensitive Detection
- Immunocomplex Formation: Mix sample with biotinylated capture antibody and detector antibody labeled with β-galactosidase (β-Gal) in solution. Incubate to form immunocomplexes.
- Streptavidin Bead Capture: Add streptavidin-coated paramagnetic beads to the mixture. Biotinylated immunocomplexes bind to beads.
- Washing & Sealing: Wash beads and resuspend in a resorufin β-D-galactopyranoside (RGP) substrate solution. The bead suspension is loaded into a disc containing ∼216,000 microwells. Beads are drawn into wells via centrifugation, with most wells receiving 0 or 1 bead.
- Sealing & Imaging: An oil layer is added to isolate each well. If a bead in a well carries an enzyme label, RGP is converted to fluorescent resorufin. A high-resolution fluorescence camera images the array.
- Digital Counting: Wells with fluorescence signal above a threshold are "on" (positive). The average enzymes per bead (AEB) is calculated from the ratio of positive wells to total bead-containing wells, enabling digital quantification.
Visualizations: Technology Workflows & Selection Logic
ELISA Sandwich Assay Protocol Steps
Immunoassay Platform Selection Logic
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Immunoassay Development
| Item | Function | Critical Consideration for Platform Choice |
|---|---|---|
| Matched Antibody Pairs | Capture and detect target analyte with high specificity. | Epitope non-overlap is paramount. MSD/Simoa often require special screening for optimal pairing. |
| Low-Binding Microplates | Solid phase for assay construction (ELISA, MSD). | Plate composition (e.g., polystyrene, polypropylene) affects antibody binding and background. |
| Magnetic Beads | Solid phase for Luminex (color-coded) and Simoa (paramagnetic). | Bead size, surface chemistry, and magnetic properties are platform-specific. |
| Electrochemiluminescent Labels (MSD) | Ruthenium chelates emit light upon electrochemical stimulation. | Requires specific MSD assay buffer and read buffer for optimal signal. |
| β-Galactosidase Enzyme Label (Simoa) | Enzyme for converting substrate in digital ELISA. | Must be conjugated to detection antibody without compromising activity. |
| Streptavidin-Biotin System | Universal amplification system for linking detection components. | High-quality, purified streptavidin conjugates (HRP, beads) reduce non-specific binding. |
| Assay Diluent/Blocking Buffer | Matrix for samples/standards; reduces non-specific binding. | Must mimic sample matrix (e.g., serum, CSF). Optimization is critical for sensitivity. |
| Calibrator Standards | Known quantities of recombinant analyte for generating standard curve. | Must be highly pure and in the same matrix as diluent for accurate quantification. |
Within the critical framework of biomarker validation research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technology for the quantitative measurement of biomarkers in biological matrices. The reliability of this data is paramount, directly impacting clinical decision-making and drug development. This guide details the alignment of ELISA-based biomarker assay development and validation with the harmonized principles of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), the Clinical and Laboratory Standards Institute (CLSI), and the U.S. Food and Drug Administration (FDA). Adherence to these guidelines ensures assays are fit-for-purpose, robust, and generate data acceptable for regulatory submission.
Guideline-Specific Considerations for ELISA Biomarker Assays
ICH Guidelines
The ICH Q2(R2) guideline on "Validation of Analytical Procedures" and the ICH E6(R3) guideline on "Good Clinical Practice" provide the foundational principles for assay validation and the conduct of clinical trials.
- ICH Q2(R2): Emphasizes the validation of the analytical procedure itself. For quantitative biomarker ELISAs, this involves establishing precision, accuracy, linearity, range, limit of quantification (LOQ), and robustness. The guideline is principles-based, requiring a justification of the selected validation tests and acceptance criteria based on the assay's intended use.
- ICH E6(R3): While focused on clinical trial conduct, it underscores the importance of using validated systems and procedures for generating reliable data, directly implicating the need for validated biomarker assays.
CLSI Guidelines
CLSI provides granular, practical guidance for laboratory testing. Key documents include:
- CLSI EP05-A3: Evaluation of Precision of Quantitative Measurement Procedures.
- CLSI EP06-A2: Evaluation of Linearity of Quantitative Measurement Procedures.
- CLSI EP07-A2: Interference Testing in Clinical Chemistry.
- CLSI EP09-A3: Measurement Procedure Comparison and Bias Estimation Using Patient Samples.
- CLSI EP17-A2: Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures.
These documents offer specific experimental protocols and statistical methods for establishing assay performance characteristics.
FDA Guidance
FDA guidance documents, such as "Bioanalytical Method Validation Guidance for Industry" (May 2018) and "Fit-for-Purpose Assay Development for Biomarker Qualification," provide a regulatory perspective. They stress:
- Tiered Approach: The level of validation rigor depends on the context of use (e.g., exploratory vs. decision-making).
- Specific Parameters: Detailed expectations for stability (bench-top, freeze-thaw, long-term), matrix effects, and selectivity.
- Documentation: Comprehensive documentation of procedures, validation data, and acceptance criteria.
The following table synthesizes core validation parameters, their definitions, and typical acceptance criteria derived from ICH, CLSI, and FDA expectations for a quantitative ELISA biomarker assay intended for pharmacokinetic or pharmacodynamic assessments.
Table 1: Core Validation Parameters for Quantitative Biomarker ELISA Assays
| Parameter | Definition | Typical Acceptance Criteria (Example) | Primary Guideline Reference |
|---|---|---|---|
| Precision | Closeness of agreement between a series of measurements. | Intra-assay (Repeatability): CV ≤ 15% (20% at LLOQ). Inter-assay (Intermediate Precision): CV ≤ 20% (25% at LLOQ). | ICH Q2(R2), CLSI EP05, FDA BMV |
| Accuracy (Trueness) | Closeness of agreement between test result and accepted reference value. | Mean recovery of 85-115% (80-120% at LLOQ) for spiked quality control (QC) samples. | ICH Q2(R2), CLSI EP09 |
| Linearity | Ability to obtain results proportional to analyte concentration. | R² ≥ 0.99, residuals within ±15% of expected. | ICH Q2(R2), CLSI EP06 |
| Range | Interval between upper and lower concentration for which method has suitable precision, accuracy, and linearity. | Defined by LLOQ and ULOQ, validated by QCs across range. | ICH Q2(R2) |
| Lower Limit of Quantification (LLOQ) | Lowest analyte concentration reliably quantified with acceptable precision and accuracy. | Signal ≥5x blank signal; Precision (CV) ≤20%; Accuracy 80-120%. | FDA BMV, CLSI EP17 |
| Selectivity / Specificity | Ability to measure analyte unequivocally in presence of interfering components (e.g., hemolysis, lipids, cross-reactants). | Accuracy within ±20% of nominal for spiked samples in at least 80% of individual matrices tested. | ICH Q2(R2), CLSI EP07 |
| Matrix Effect | Direct or indirect alteration in response due to components in the sample other than the analyte. | Normalized matrix factor CV ≤ 15% across lots. | FDA BMV |
| Stability | Chemical stability of analyte under specified conditions. | Accuracy within ±15% of nominal for all QCs. | FDA BMV |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters (e.g., incubation time/temp, reagent lot). | All results meet pre-defined acceptance criteria. | ICH Q2(R2) |
Experimental Protocols for Core Validation Experiments
Protocol 1: Precision (Repeatability and Intermediate Precision) per CLSI EP05-A3
Objective: To evaluate the within-run (repeatability) and between-run/between-day/between-analyst (intermediate precision) variance of the ELISA method.
Materials: A minimum of two concentration levels (e.g., Low and High QC) prepared in the target biological matrix (e.g., serum). Three independent preparations of each QC level.
Procedure:
- Over 5 separate analytical runs, analyze each of the 3 independent preparations per QC level in duplicate.
- Runs should incorporate intended sources of variation (e.g., different days, different analysts, different reagent lots if applicable).
- Calculate the mean concentration and coefficient of variation (CV%) for the replicates within each run (repeatability) and across all runs and preparations (total variance, used to estimate intermediate precision).
Protocol 2: Linearity of Dilution and Parallelism per CLSI EP06-A2
Objective: To confirm that sample dilution in the assay matrix yields results proportional to concentration (linearity) and that the endogenous analyte behaves immunologically similar to the reference standard (parallelism).
Materials: A high-concentration endogenous sample (e.g., disease state pool) and the reference standard spiked into the same analyte-free matrix.
Procedure:
- Prepare a series of serial dilutions (e.g., 1:2, 1:4, 1:8, etc.) of both the endogenous sample and the spiked standard, using the assay's recommended dilution buffer/matrix.
- Analyze all dilutions in a single ELISA run.
- Plot measured concentration (or optical density) vs. expected concentration/dilution factor.
- Assess linearity via linear regression (R², slope). Assess parallelism by comparing the regression slopes of the endogenous sample and the spiked standard (e.g., % difference should be within ±15%).
Protocol 3: Selectivity and Matrix Effect Evaluation per CLSI EP07-A2 & FDA BMV
Objective: To assess interference from common matrix components and variability across individual matrix sources.
Materials: Individual matrix samples (e.g., serum from at least 10 healthy and 10 target disease donors). Interferent stocks (e.g., bilirubin, hemoglobin, lipids). A spiking solution of the biomarker analyte.
Procedure:
- Selectivity: Spike a low and high concentration of analyte into each individual matrix sample. Also prepare unspiked controls. Calculate recovery in each lot. Acceptance: ≥80% of individual lots show recovery within ±20% of nominal.
- Interference: Spike a known concentration of analyte into a pooled matrix. Add potential interferents at high physiological concentrations. Compare measured concentration to a control with no interferent added. Acceptance: Recovery within ±15% of control.
- Matrix Factor (for ligand-binding assays): Post spiking at low and high levels into multiple individual matrices, the normalized matrix factor (MF) is calculated. Acceptance: CV of normalized MF across matrix lots is ≤15%.
ELISA Biomarker Validation Workflow
Signaling Pathway Impact on Biomarker Selection
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Robust Biomarker ELISA Development & Validation
| Item | Function in Biomarker Assay | Critical Considerations for Validation |
|---|---|---|
| Capture & Detection Antibody Pair | Forms the immunoassay's core, defining specificity and sensitivity. Must recognize distinct, non-overlapping epitopes. | Document source, clone, lot number. Test for cross-reactivity and parallelism. Critical reagent stability must be established. |
| Reference Standard | Highly purified analyte used to construct the calibration curve. Serves as the basis for all quantitative measurements. | Source, purity, and certificate of analysis (CoA) are paramount. Should be traceable to a primary standard if available. Stability data required. |
| Matrix-matched Calibrators & QCs | Calibrators and Quality Control samples prepared in the same biological matrix as study samples (e.g., human serum). | QCs at Low, Mid, High concentrations anchor each run. Must demonstrate commutability with endogenous analyte. |
| Assay Buffer System | Provides optimal pH, ionic strength, and protein background to minimize non-specific binding and matrix interference. | Optimization is key. Must be validated for selectivity across individual matrix lots. |
| Detection System (e.g., HRP-Streptavidin) | Amplifies the specific signal for readout. Enzymatic (HRP, AP) or fluorescent tags are common. | Enzyme activity and conjugate stability must be monitored. Lot-to-lot consistency is critical for precision. |
| Blocking Agent | Reduces non-specific binding of antibodies or sample proteins to the solid phase (plate). | Common agents: BSA, casein, non-fat dry milk. The chosen agent must not interfere with antibody-antigen binding. |
| Signal Generation Substrate | Reacts with the detection enzyme to produce a measurable colorimetric, chemiluminescent, or fluorescent signal. | Must be fresh and protected from light. Reaction kinetics (linear range) must be characterized. |
Successful validation of an ELISA for biomarker quantification is a deliberate, evidence-driven process framed by the complementary guidelines of ICH, CLSI, and the FDA. By integrating the principle-based approach of ICH, the detailed experimental protocols of CLSI, and the regulatory expectations of the FDA, researchers can develop a fit-for-purpose, robust, and defensible assay. This alignment ensures the generation of high-quality, reliable data that supports informed decision-making in both clinical research and drug development, ultimately contributing to the advancement of personalized medicine and therapeutic efficacy.
The transition of an enzyme-linked immunosorbent assay (ELISA) from a Research-Use-Only (RUO) tool to a clinically accepted diagnostic is a critical pathway in translational medicine. This journey encapsulates the rigorous validation of a biomarker from initial discovery to a reliable measurement of clinical status. ELISA, with its foundational principles of specificity, sensitivity, and quantitative output, serves as the archetypal platform for this evolution. This whitepaper delineates the technical, regulatory, and validation milestones required, positioning the process within the broader thesis of biomarker validation for drug development and clinical decision-making.
The Validation Pathway: Technical and Regulatory Stages
The path from RUO to clinical-grade in vitro diagnostic (IVD) is defined by increasing levels of stringency. The following table summarizes the core distinctions and requirements at each phase.
Table 1: Comparative Analysis of RUO, ASR, and IVD ELISA Assays
| Aspect | Research-Use-Only (RUO) | Analyte-Specific Reagent (ASR) | FDA-Cleared/Approved IVD |
|---|---|---|---|
| Primary Purpose | Exploratory research, hypothesis generation. | Lab-developed test (LDT) component. | Clinical diagnosis, monitoring, or prognosis. |
| Regulatory Oversight (FDA, USA) | Minimal; labeled "For Research Use Only. Not for use in diagnostic procedures." | Class I-III medical device; controls labeling but not performance. | Premarket review (510(k), De Novo, or PMA). |
| Claim Support | No clinical performance claims required. | Performance claims determined by the laboratory (CLIA). | Specific, validated indications for use and claims. |
| Validation Burden | Analytical performance (precision, sensitivity) often assessed internally. | Laboratory must perform full analytical & clinical validation per CLIA. | Manufacturer must provide extensive analytical & clinical validation data. |
| Manufacturing Controls | Good Laboratory Practice (GLP) common. | Quality System Regulation (QSR) compliance required. | Strict adherence to Quality Management System (QMS), e.g., ISO 13485. |
| Traceability & Stability | Lot-specific data may be limited. | Requires established traceability and stability data. | Extensive lot-to-lot consistency, calibration traceability, and shelf-life studies. |
Core Experimental Protocols for Clinical Validation
The following methodologies are foundational for advancing an ELISA from RUO to clinical-grade.
Protocol 1: Comprehensive Analytical Sensitivity (LoB, LoD, LoQ) Determination
Objective: To establish the limit of blank (LoB), limit of detection (LoD), and limit of quantification (LoQ) according to CLSI EP17-A2 guidelines.
Materials: Assay buffer (negative matrix), low-concentration analyte samples, routine precision materials.
Procedure:
- LoB: Measure replicate (n≥20) aliquots of a blank sample (matrix without analyte). Calculate the mean and standard deviation (SD). LoB = Meanblank + 1.645(SDblank).
- LoD: Prepare samples with analyte concentration near the expected LoD. Measure at least 20 replicates per sample over multiple days. LoD = LoB + 1.645(SDlow concentration sample).
- LoQ: Determine the lowest concentration where the total error (bias + 2*SD) meets predefined acceptability criteria (e.g., ≤20% CV). This requires testing multiple low-level samples across the assay range.
Protocol 2: Method Comparison and Clinical Concordance Study
Objective: To compare the candidate clinical ELISA against a reference method or clinical truth.
Materials: A minimum of 100-150 well-characterized clinical specimens spanning the assay's measuring range and including disease/relevant control states.
Procedure:
- Test all specimens in duplicate using both the candidate assay and the comparator method.
- Perform statistical analysis: Calculate Pearson/Spearman correlation, perform Deming or Passing-Bablok regression analysis, and generate Bland-Altman difference plots.
- For diagnostic accuracy, establish a receiver operating characteristic (ROC) curve. Calculate the area under the curve (AUC), optimal cutoff (using Youden's index), and associated sensitivity, specificity, and predictive values against a clinical gold standard (e.g., biopsy, confirmed diagnosis).
Key Signaling Pathways and Workflows
Diagram 1: The Path from RUO to IVD
Diagram 2: Sandwich ELISA Principle & Workflow
The Scientist's Toolkit: Essential Reagent Solutions
Table 2: Key Research Reagent Solutions for Clinical-Grade ELISA Development
| Reagent/Material | Function & Clinical-Grade Critical Attribute |
|---|---|
| Clinical-Grade Capture/Detection Antibodies | High specificity and affinity clones; produced under GMP/ISO 13485 with full traceability (hybridoma sequence, purification records). Must demonstrate lack of cross-reactivity against homologous interferents. |
| Calibrators & Reference Standards | Quantified analyte in defined matrix, traceable to an international standard (e.g., WHO IS). Critical for establishing the assay's master calibration curve and ensuring longitudinal consistency. |
| Matched Diluent/Assay Buffer | Optimized for specific sample matrix (serum, plasma, CSF). Contains blockers to minimize non-specific binding and matrix effects, ensuring accuracy across diverse patient samples. |
| Stable Enzyme Conjugates | Consistent enzyme-to-antibody ratio (e.g., HRP, ALP). Rigorous batch testing for activity and stability is required to maintain uniform signal generation over the shelf life. |
| Validated Sample Collection Tubes | Specifies acceptable anticoagulants (e.g., EDTA, heparin), tube materials, and stability conditions (time/temperature) to prevent pre-analytical analyte degradation or alteration. |
| Control Materials (Positive, Negative, QC) | Third-party or internally validated controls spanning medical decision points. Essential for daily run acceptance and monitoring assay performance (Levey-Jennings charts). |
| Microplate with Certificate of Analysis | Plates with high and consistent binding capacity, low background fluorescence, and lot-specific performance data to ensure uniform coating efficiency. |
Conclusion
ELISA remains a cornerstone technology for biomarker validation, balancing accessibility, robustness, and quantitative rigor. Success hinges on a deep understanding of foundational principles, meticulous execution and optimization of the methodology, proactive troubleshooting, and rigorous validation against contemporary standards. While emerging technologies offer advantages in multiplexing and sensitivity, a well-validated ELISA provides the gold-standard reliability required for critical preclinical and clinical decision-making. Future directions involve greater harmonization of validation protocols, integration with digital tools for data analysis, and the development of more standardized, recombinant reagents to reduce variability. Ultimately, mastering ELISA validation is essential for translating promising biomarkers from discovery into trustworthy tools that can advance personalized medicine and therapeutic development.