Bioelectrical Impedance Analysis (BIA) in Biomedical Research: From Body Composition to Advanced Drug Screening Platforms
This article provides a comprehensive analysis of Bioelectrical Impedance Analysis (BIA) for researchers, scientists, and drug development professionals.
Bioelectrical Impedance Analysis (BIA) in Biomedical Research: From Body Composition to Advanced Drug Screening Platforms
Abstract
This article provides a comprehensive analysis of Bioelectrical Impedance Analysis (BIA) for researchers, scientists, and drug development professionals. It explores the fundamental principles of BIA technology for body composition assessment, detailing its application in clinical and research settings while addressing critical methodological considerations and validation challenges. The content further examines the transformative application of BIA principles in advanced drug screening platforms, specifically focusing on Electric Cell-substrate Impedance Sensing (ECIS) for real-time, label-free monitoring of cellular responses. By synthesizing recent validation studies and comparative analyses with reference methods like DXA, this review offers evidence-based insights for optimizing BIA implementation in both nutritional epidemiology and pharmaceutical development.
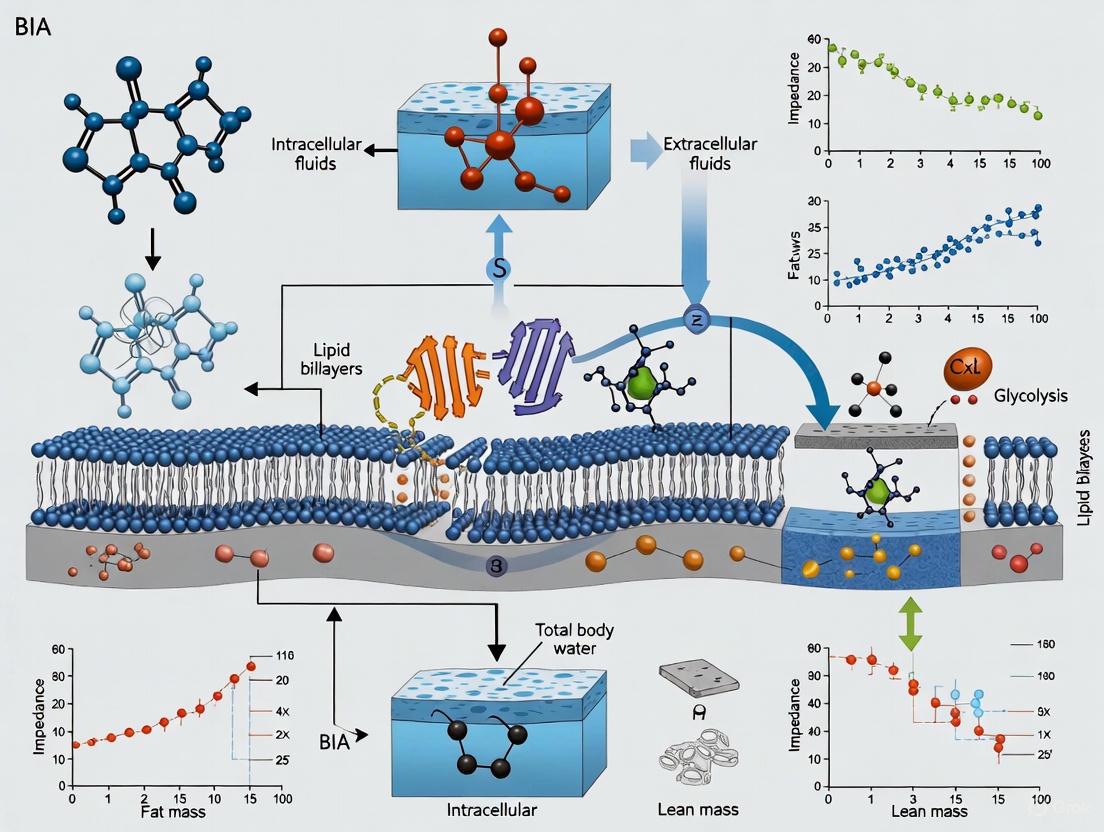
Principles and Evolution of Bioelectrical Impedance Technology
Core Biophysical Principles
Bioelectrical Impedance Analysis (BIA) estimates body composition by measuring the body's opposition to a low-level, alternating electrical current. This impedance (Z) comprises two components: resistance (R), which reflects the opposition to current flow through electrolytic fluids, and reactance (Xc), which represents the capacitive properties of cell membranes that temporarily store electrical energy [1]. The fundamental principle underpinning BIA is that different biological tissues exhibit varying electrical conductivity based on their water and electrolyte content [2].
Table 1: Fundamental Bioelectrical Parameters and Their Physiological Correlates
| Parameter | Definition | Physiological Correlate | Typical Range/Unit |
|---|---|---|---|
| Resistance (R) | Opposition to the flow of an alternating current through ionic solutions [1] | Inversely related to Total Body Water (TBW) and electrolyte content [3] | ~150-900 Ω [1] |
| Reactance (Xc) | Capacitive opposition from cell membranes and tissue interfaces [1] | Integrity and number of cell membranes [3] | Derived from R and Xc |
| Impedance (Z) | Total opposition to current flow (vector sum of R and Xc) [4] | Overall body fluid volume and composition [4] | Ohms (Ω) |
| Phase Angle (PhA) | Angular transformation of the ratio Xc/R [3] | Cellular integrity, body cell mass, and fluid distribution [3] | Degrees (°) |
Fat-free mass (FFM), which includes muscle and body fluids, is highly conductive due to its high water and electrolyte content. In contrast, adipose tissue (fat mass) and bone are poor conductors (dielectrics) because they contain little water [2]. This differential conductivity allows BIA to distinguish between body compartments. The Impedance Index (H²/R), where H is height and R is resistance, is proportional to the volume of the conductor (the body's water pool) and is used to estimate TBW and FFM, assuming a constant hydration level of 73% for FFM [1] [5].
Frequency-Dependent Current Behavior and Body Water Compartmentalization
The behavior of the electrical current in biological tissues is frequency-dependent, which allows for the differentiation of body water compartments.
- Low-Frequency Current (≤5-50 kHz): At low frequencies, the electrical current cannot penetrate the capacitive cell membranes and is therefore confined to the Extracellular Water (ECW) space [4] [1].
- High-Frequency Current (≥50-1000 kHz): At high frequencies, the current can cross cell membranes and thus passes through both the Extracellular Water (ECW) and Intracellular Water (ICW) spaces, enabling the measurement of Total Body Water (TBW) [4] [1].
This frequency-dependent permeability is the basis for Multi-Frequency BIA (MF-BIA) and Bioelectrical Impedance Spectroscopy (BIS), which provide more detailed analyses of fluid distribution than Single-Frequency BIA (SF-BIA) [4] [1].
Table 2: BIA Device Configurations and Their Capabilities
| Device Type | Frequencies | Typical Electrode Configuration | Primary Outputs | Advantages & Limitations |
|---|---|---|---|---|
| Single-Frequency BIA (SF-BIA) | 50 kHz [4] | Tetrapolar (hand-to-foot or foot-to-foot) [1] | TBW, FFM, FM [1] | Adv: Affordable, simple [4].Limit: Cannot differentiate ICW/ECW [1]. |
| Multi-Frequency BIA (MF-BIA) | 5 kHz - 1000 kHz [5] [4] | Octopolar (segmental, hand-to-foot) [5] [4] | TBW, ECW, ICW, FFM, FM, segmental data [5] [1] | Adv: Differentiates fluid compartments [4].Limit: Higher cost, proprietary algorithms [4]. |
| Bioelectrical Impedance Spectroscopy (BIS) | A spectrum of frequencies [4] [1] | Tetrapolar or Octopolar [1] | TBW, ECW, ICW, Body Cell Mass [1] | Adv: Considered most accurate for fluid volumes [4].Limit: Complex, requires specialized models [4]. |
Quantitative Validation Data
The following table summarizes key findings from recent validation studies comparing BIA devices against criterion methods like Dual-Energy X-Ray Absorptiometry (DXA) in real-world conditions.
Table 3: Validation of BIA Devices Against Criterion Methods (DXA)
| Study Comparison | Population | Key Metric | Correlation (r) | Bias (Mean Difference) | Notes |
|---|---|---|---|---|---|
| MF-BIA (InBody 770) vs. DXA [5] | 1000 healthy adults | Fat Mass (FM) | Men: 0.93Women: 0.96 | Men: -3.7 kgWomen: -1.9 kg | Modest population-level agreement in uncontrolled conditions [5]. |
| Percent Body Fat (%BF) | Men: 0.89Women: 0.92 | Men: -4.2%Women: -2.8% | |||
| Fat-Free Mass (FFM) | Men: 0.95Women: 0.94 | Men: +3.4 kgWomen: +2.0 kg | |||
| Wearable BIA (Smartwatch) vs. DXA [6] | 108 active adults | Body Fat % (%BF) | 0.93 | Not specified (MAPE*: 14.3%) | Strong correlation but significant individual error, especially for skeletal muscle% [6]. |
| Skeletal Muscle % (SM%) | 0.92 | Not specified (MAPE*: 20.3%) | |||
| Wearable BIA vs. 4-Compartment Model [7] | Healthy adults | Percent Body Fat (%BF) | Strong agreement with MF-BIA | Overestimated vs. 4C model | Wearables show promise but can overestimate %BF versus criterion methods [7]. |
*MAPE: Mean Absolute Percentage Error
Experimental Protocol for Standardized BIA Measurement
This protocol is designed for a standing hand-to-foot octopolar MF-BIA device to ensure reliable and reproducible results.
Pre-Test Participant Preparation and Conditions
Instruct participants to adhere to the following guidelines for 24 hours prior to testing [1]:
- Hydration/Fluid Intake: Consume water normally but refrain from alcohol and caffeine.
- Physical Activity: Avoid vigorous exercise for 8 hours before the test.
- Nutritional Status: Fast for a minimum of 4 hours prior to measurement.
- Clothing: Wear lightweight athletic clothing. Remove shoes, socks, and any metal jewelry.
- Contraindications: Do not test individuals with implanted electronic medical devices (e.g., pacemakers) [1].
Equipment Calibration and Setup
- Use an MF-BIA device (e.g., InBody 770) calibrated according to the manufacturer's specifications [5].
- Input participant data (height, weight, age, gender) into the device as required.
- Ensure the device is on a stable, flat surface.
Participant Positioning and Measurement Procedure
- The participant stands barefoot on the device's foot electrodes.
- Instruct the participant to:
- Grasp the hand electrodes, ensuring palms and fingers make full contact.
- Keep arms slightly abducted, extended, and not touching the torso.
- Keep legs slightly separated and not touching each other [1].
- The participant must remain still and silent during the measurement, which typically takes 1-2 minutes.
Data Recording and Analysis
- Record the raw parameters: Resistance (R), Reactance (Xc), and calculated Phase Angle (PhA) at various frequencies [4].
- Utilize the device's proprietary algorithms or validated population-specific equations to derive body composition estimates (TBW, ICW, ECW, FFM, FM) [4] [1].
- For longitudinal tracking, ensure identical pre-test conditions and device setup for all follow-up measurements.
Visualization of Core Concepts
BIA Measurement Workflow and Determinants
Electrical Conductivity of Biological Tissues
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Materials for BIA Research
| Item/Category | Specification/Example | Primary Function in BIA Research |
|---|---|---|
| Multi-Frequency BIA Analyzer | InBody 770, RJL Systems Quantum IV [5] [8] | Primary device for applying current and measuring impedance across multiple frequencies to differentiate fluid compartments [5] [4]. |
| Electrodes (if separate) | Disposable, pre-gelled ECG-type electrodes [1] | Ensure consistent electrical contact with the skin for current injection and voltage sensing in tetrapolar setups. |
| Criterion Method Equipment | DXA Scanner (e.g., GE Lunar iDXA) [5] [6] | Provides reference ("gold standard") body composition data for validating BIA device accuracy [5] [6]. |
| Calibration Verification Kit | Manufacturer-provided resistor/circuit [1] | Verifies the proper electrical calibration of the BIA device before measurements to ensure data integrity. |
| Data Management Software | REDCap, Statistical Software (R, jamovi) [6] | Securely manages participant data and performs statistical analysis of impedance parameters and validation metrics [6]. |
| Raw Bioimpedance Parameters | Resistance (R), Reactance (Xc), Phase Angle (PhA) [4] [3] | Foundational measurements for advanced analysis (e.g., BIVA) and for applying population-specific equations beyond proprietary algorithms [4]. |
Bioelectrical Impedance Analysis (BIA) represents a critical methodology in body composition research, with its evolution from simple single-frequency devices to sophisticated multi-frequency spectroscopy (BIS) systems marking significant technological advancement. This progression has substantially enhanced the precision and applicability of BIA in both clinical and research settings, particularly for drug development and nutritional intervention studies. The transition from estimating body composition as a single cylinder to segmental analysis using multiple frequencies has addressed fundamental limitations in early devices, enabling more accurate differentiation between body water compartments and tissue types [9] [10]. This development history reflects a continuous effort to improve the correlation between electrical impedance properties and biological tissues, moving from empirical population-based estimations toward individualized, direct measurements of body composition parameters including fat mass, fat-free mass, total body water, and its sub-compartments [11] [4]. For researchers and pharmaceutical professionals, understanding this technological evolution is essential for selecting appropriate assessment tools and interpreting body composition data in clinical trials and metabolic studies.
Historical Trajectory of BIA Technology
The theoretical foundations of bioelectrical impedance were established as early as 1872 with investigations into the electrical properties of biological tissues [11]. However, the modern era of BIA began in the 1960s when Thomasset conducted pioneering studies using electrical impedance measurements with subcutaneously inserted needles as an index of total body water (TBW) [11] [12]. This foundational work demonstrated the relationship between electrical conduction and body fluid volumes, establishing the fundamental principle that impedance varies inversely with body water content.
A critical breakthrough came in 1969 when Hoffer and colleagues established a correlation coefficient of 0.92 between whole-body impedance measurements and TBW, leading to the development of the impedance index (stature²/resistance), which remains a cornerstone of BIA analysis today [9] [11] [10]. This discovery validated BIA as a viable method for estimating body composition and set the stage for commercial development.
The first commercial impedance meter was introduced by RJL Systems in 1979, which applied a 50kHz current to the right half of the body via electrodes attached to the hand and foot [11] [10]. This device significantly popularized BIA methodology by offering a non-invasive, rapid, and comparatively inexpensive alternative to traditional methods like underwater weighing or skinfold calipers, which were often uncomfortable, required skilled technicians, and could not test diverse populations [10].
Throughout the 1980s, research by Lukaski, Segal, and others revealed significant limitations in single-frequency BIA technology, particularly its treatment of the human body as a uniform single cylinder [11]. This approach proved inadequate for populations with non-standard body types, prompting researchers to develop numerous empirical equations incorporating demographic variables such as age, sex, and ethnicity to improve accuracy for specific populations [11] [10]. While these equations improved population-level estimates, they remained limited for individual assessments, particularly in clinical populations or those with atypical body compositions.
A conceptual breakthrough occurred in 1992 when Kushner proposed measuring the human body as five separate cylinders (arms, legs, and torso) rather than one uniform volume [11] [10]. This approach acknowledged the varying impedance characteristics of different body segments, with Kushner further advocating for multiple frequencies to better distinguish intracellular from extracellular water [10]. This theoretical advancement paved the way for modern segmental and multi-frequency devices.
In 1996, Dr. Kichul Cha developed the first 8-point tactile electrode system with direct segmental analysis using multiple frequencies (DSM-MFBIA technology) [10]. This innovation enabled separate impedance measurements of the limbs and torso, significantly improving accuracy without relying on empirical demographic data [10]. Subsequent technological evolution has continued with the development of wearable BIA devices and smartwatch integration, making body composition tracking more accessible, though with ongoing challenges regarding accuracy and standardization [7].
Table 1: Key Historical Milestones in BIA Development
| Year | Researcher/Company | Contribution | Significance |
|---|---|---|---|
| 1962 | Thomasset | First used electrical impedance as index of TBW | Established fundamental relationship between impedance and body water [11] [12] |
| 1969 | Hoffer et al. | Demonstrated correlation (r=0.92) between whole-body impedance and TBW | Created impedance index (height²/R) still used today [9] [11] [10] |
| 1979 | RJL Systems | First commercial impedance meter | Made BIA accessible for research and clinical use [11] [10] |
| 1980s | Lukaski, Segal et al. | Identified limitations of single-frequency, single-cylinder model | Spurred development of population-specific empirical equations [11] |
| 1992 | Kushner | Proposed 5-cylinder model and multiple frequencies | Theoretical foundation for segmental and multi-frequency BIA [11] [10] |
| 1996 | Dr. Kichul Cha | Developed first 8-point electrode system with DSM-MFBIA | Enabled direct segmental measurement without empirical estimations [10] |
| 2018-2020 | AURA Devices, Samsung | Integrated BIA into wearables and smartwatches | Made body composition tracking more accessible to consumers [11] [7] |
Technical Evolution and Methodological Principles
Fundamental Electrical Principles
Bioelectrical impedance analysis operates on the principle that the human body conducts electrical current differently based on tissue composition. Impedance (Z) represents the frequency-dependent opposition to the flow of an alternating electric current and consists of two vector components: resistance (R) and reactance (Xc) [9]. Resistance constitutes the opposition to current flow primarily through electrolyte solutions in extracellular and intracellular fluids, while reactance results from capacitive properties of cell membranes that temporarily store electrical energy [9] [4]. The mathematical relationship is expressed as Z² = R² + Xc² [9].
The phase angle (PhA), derived as the arctangent of Xc/R, provides valuable information about cellular integrity and health status [9] [4]. Phase angle has gained increasing clinical significance as a marker of cellular membrane integrity and has demonstrated prognostic value in various chronic conditions including cancer, HIV, and renal failure [4]. This raw BIA parameter changes with variations in the frequency of the applied current and reflects the relative contributions of resistance and reactance to overall impedance [9].
From Single-Frequency to Multi-Frequency Technology
Traditional single-frequency BIA (SF-BIA) devices typically operate at 50 kHz and estimate body composition based on a two-compartment model that assumes the total conductive volume equals TBW, with fat-free mass (FFM) subsequently calculated assuming a constant hydration fraction of 73% [9] [5]. This approach has limitations because the percentage of TBW in FFM actually varies with age, gender, and physiological conditions, and is altered in disease states [9].
The development of multi-frequency BIA (MF-BIA) and bioelectrical impedance spectroscopy (BIS) addressed fundamental limitations of single-frequency systems. At low frequencies (<5 kHz), electrical current primarily travels through extracellular fluids, as it cannot penetrate cell membranes effectively [9] [5]. As frequency increases, the current begins to penetrate cell membranes, with high frequencies (>100 kHz) passing through both extracellular and intracellular spaces, thereby measuring TBW [9] [5]. MF-BIA exploits this frequency-dependent behavior to differentiate water compartments, while BIS measures impedance across a spectrum of frequencies to provide detailed analysis of fluid distribution [4].
Table 2: Comparison of BIA Technological Approaches
| Parameter | Single-Frequency BIA | Multi-Frequency BIA | Bioelectrical Impedance Spectroscopy (BIS) |
|---|---|---|---|
| Frequencies | Single frequency (typically 50 kHz) [4] | Multiple discrete frequencies (e.g., 5, 50, 250 kHz) [5] [4] | Spectrum of frequencies (typically 1-1000 kHz) [4] |
| Water Compartment Assessment | Estimates TBW only [9] | Differentiates ECW and ICW [5] [4] | Precisely quantifies ECW and ICW [4] |
| Body Model | Single cylinder [10] | Segmental (5 cylinders) [10] | Segmental or whole-body [4] |
| Primary Applications | Population studies, basic body composition [4] | Clinical assessment, nutritional status [4] | Dialysis, critical care, research [4] [9] |
| Limitations | Cannot differentiate fluid compartments; affected by hydration status [9] [13] | Proprietary algorithms; requires standardization [4] | Cost; requires expertise; sensitive to measurement conditions [4] |
Electrode Configuration Advancements
Electrode configuration has evolved significantly throughout BIA's development. Early devices used bipolar arrangements, either hand-to-hand or foot-to-foot, which limited accuracy by measuring only specific body segments [13] [10]. The introduction of tetrapolar configurations (separate current and voltage electrodes) improved accuracy by reducing the impact of skin-electrode interface impedance [11] [4].
Modern medical-grade devices often employ octopolar systems with eight electrodes—two for each hand and foot—enabling direct segmental analysis of arms, legs, and torso [5] [10]. This approach recognizes that body segments have different impedance characteristics due to variations in length, cross-sectional area, and tissue composition [10]. The torso presents particular measurement challenges due to its large cross-sectional area and complex composition, making segmental measurement crucial for accuracy [10].
Comparative Accuracy and Validation Studies
Single vs. Multi-Frequency Device Performance
The evolution from single-frequency to multi-frequency BIA has brought measurable improvements in accuracy and clinical utility. SF-BIA devices show reasonable accuracy for estimating TBW and body composition in healthy populations with normal hydration [9] [13]. However, their limitations become apparent in populations with altered hydration status or non-standard body composition.
Multi-frequency systems demonstrate superior performance in differentiating body water compartments. A 2025 real-world assessment of MF-BIA involving 1000 healthy adults found modest population-level agreement with DXA for total body fat mass (men: r=0.93, bias -3.7±2.6 kg; women: r=0.96, bias -1.9±1.8 kg) and fat-free mass (men: r=0.95, bias 3.4±2.8 kg; women: r=0.94, bias 2.0±2.2 kg) [5] [14]. The same study reported high test-retest reliability for MF-BIA (ICC 0.987-0.995) even in uncontrolled conditions [5].
Consumer-grade bipolar devices typically show wider limits of agreement with criterion methods. A 2008 study comparing BIA consumer devices against DXA and MRI found 95% limits of agreement for percent fat mass ranged from -6.59 to 4.61% for a tetrapolar device compared to -14.54 to 8.58% for bipolar instruments [13]. This highlights the accuracy advantage of tetrapolar configurations, which are preferred for individual assessments [13].
Special Population Considerations
BIA accuracy varies significantly across different populations, necessitating appropriate method selection. In spinal cord injury (SCI) patients, BIA has demonstrated utility despite altered body composition, with studies validating its use for monitoring obesity, nutrition, and rehabilitation progress [12]. BIA offers particular advantages in this population due to its portability and non-invasive nature, though population-specific equations may be required for optimal accuracy [12].
For athletic populations, segmental MF-BIA provides more accurate assessment of muscle distribution compared to traditional SF-BIA. The ability to measure trunk and limb composition separately is valuable for tracking training adaptations and identifying asymmetries [5] [10].
Table 3: Accuracy Comparison Across BIA Modalities
| Measurement | Single-Frequency BIA | Multi-Frequency BIA | Bioimpedance Spectroscopy |
|---|---|---|---|
| Total Body Water | Moderate agreement with reference methods (typical error ~2-3%) [9] | Good agreement (typical error ~1-2%) [5] | High agreement with dilution methods (typical error ~1-2%) [4] |
| Extracellular Water | Not measurable [9] | Good agreement with bromide dilution [4] | High agreement with bromide dilution [4] |
| Fat-Free Mass | Moderate agreement with DXA (r=0.75-0.89) [13] | Good agreement with DXA (r=0.89-0.96) [5] | Limited reported data |
| Visceral Adipose Tissue | Poor accuracy [13] | Moderate agreement (r=0.74) [5] | Limited reported data |
| Phase Angle | Available but limited prognostic value [11] | Strong prognostic value in chronic disease [4] | High precision for monitoring [4] |
Application Notes and Experimental Protocols
Standardized BIA Measurement Protocol
For research and clinical applications, standardized protocols are essential for obtaining reliable, reproducible BIA measurements. The following protocol applies to whole-body, tetrapolar MF-BIA assessment:
Pre-Test Preparation:
- Participants should fast for 4 hours prior to measurement [5]
- Avoid moderate or high-intensity exercise for 12 hours before testing [11]
- Abstain from alcohol for 24 hours and caffeine for 4 hours before testing
- Void bladder completely within 30 minutes preceding measurement
- Maintain normal hydration status; avoid intentional overhydration or dehydration
Equipment Preparation:
- Calibrate BIA device according to manufacturer specifications
- Ensure electrodes are fresh and properly stored
- Record ambient temperature and humidity
Subject Positioning:
- Position participant supine on a non-conductive surface with limbs abducted from body
- Ensure no contact between arms/legs or arms/torso
- Place electrodes on designated sites (typically right side) according to manufacturer specifications:
- Hand electrode: proximal to metacarpophalangeal joint
- Wrist electrode: at midline of posterior wrist
- Foot electrode: proximal to metatarsophalangeal joint
- Ankle electrode: at midline of anterior ankle
- Verify secure electrode contact without excess gel seepage
Measurement Procedure:
- Input required participant data (age, gender, height, weight)
- Ensure participant remains motionless during measurement
- Record resistance and reactance values at all frequencies
- Verify measurement quality through phase angle consistency
- Repeat measurement if significant movement artifact occurs
Validation Study Design Protocol
For researchers validating BIA against criterion methods, the following protocol ensures methodological rigor:
Participant Selection:
- Recruit heterogeneous sample representing target population
- Include appropriate distribution of age, BMI, and physiological characteristics
- Obtain informed consent and ethical approval
Reference Method Selection:
- DXA for fat mass, lean mass, and bone mineral content [5] [13]
- MRI for adipose tissue distribution and skeletal muscle volume [13]
- Deuterium oxide dilution for total body water [9] [7]
- Bromide dilution for extracellular water [4]
Testing Sequence:
- Perform BIA and reference methods within 2 hours
- Maintain consistent participant conditions between measurements
- Counterbalance measurement order to minimize sequence effects
Data Analysis:
- Calculate correlation coefficients (Pearson or Spearman)
- Perform Bland-Altman analysis to assess agreement
- Report bias and limits of agreement (bias ± 1.96 SD)
- Calculate intraclass correlation coefficients for reliability
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for BIA Research
| Item | Function | Specifications |
|---|---|---|
| Medical-Grade Electrodes | Ensure consistent current application and voltage detection | Pre-gelled, hypoallergenic, specific diameter according to manufacturer |
| Calibration Verification Tools | Verify device accuracy and precision | Manufacturer-provided calibration resistors with known values |
| Height Stadiometer | Measure participant height for impedance index calculation | Wall-mounted, precision of ±0.1 cm |
| Calibrated Scale | Measure body weight for body composition calculations | Digital, precision of ±0.1 kg |
| Non-Conductive Examination Table | Provide proper surface for supine measurement | Width >70 cm, length >180 cm, non-conductive material |
| Environmental Monitor | Track conditions that may affect measurements | Temperature (±0.5°C), humidity (±5%) |
| Reference Standard Solutions | Validate new BIA equations | DXA, MRI, or dilution method access for cross-validation |
The historical development from single-frequency devices to multi-frequency spectroscopy represents a paradigm shift in bioelectrical impedance analysis, transforming it from a simple screening tool to a sophisticated research methodology. This evolution has addressed fundamental limitations in body composition assessment through technological innovations including multiple frequencies, segmental analysis, and advanced electrode configurations. For researchers and pharmaceutical professionals, modern BIS provides a non-invasive, rapid, and reasonably accurate method for assessing body composition and fluid distribution in both controlled laboratory and real-world settings. While challenges remain regarding standardization, algorithm transparency, and population-specific validation, the continued refinement of BIA technology promises enhanced utility in clinical trials, nutritional intervention studies, and personalized medicine applications. Future developments will likely focus on wearable technologies, improved algorithms, and expanded applications in diverse physiological and pathological conditions.
Bioelectrical Impedance Analysis (BIA) is a widely used, non-invasive method for assessing body composition in research and clinical practice. The technique measures the body's impedance to a small, alternating electric current, from which fundamental parameters about fluid distribution and cellular health can be derived. Among these parameters, Total Body Water (TBW), Extracellular Water (ECW), and the Phase Angle (PhA) are critical biomarkers. TBW represents the body's total fluid volume, while ECW refers specifically to the fluid outside cells; their ratio (ECW/TBW) provides insights into fluid balance. PhA, derived from the arctangent of the ratio of reactance to resistance, serves as a marker of cellular integrity and body cell mass. This application note details the protocols for measuring these parameters and synthesizes current research findings to standardize their application in scientific research and drug development.
Theoretical Foundations and Biological Significance
BIA operates on the principle that the human body conducts electrical current differently based on tissue composition. Low-frequency currents primarily pass through the extracellular fluid, while high-frequency currents can penetrate cell membranes, enabling the assessment of total body water.
- Phase Angle (PhA): Calculated as PhA = arctan(Xc/R) × (180°/π), where Xc (reactance) represents the capacitive properties of cell membranes acting as capacitors, and R (resistance) is the opposition to current flow through intra- and extracellular fluids. A higher PhA indicates robust cell membranes, greater cellular integrity, and better nutritional status. It is considered a proxy for muscle quality and cellular health [15] [16].
- Extracellular Water/Total Body Water (ECW/TBW) Ratio: This ratio is a key indicator of fluid distribution. The reference range is typically 0.360–0.400 [17]. A value exceeding 0.400 suggests fluid imbalance, such as edema or subclinical inflammation, and is associated with lower muscle quality and higher adiposity [18] [17].
The following diagram illustrates the relationship between raw BIA measurements, the derived key parameters, and their clinical significance in research workflows.
Research Applications and Associations
BIA-derived parameters are associated with critical health outcomes across various populations, making them valuable in nutritional research, gerontology, and chronic disease management.
Table 1: Key Research Associations of Phase Angle and ECW/TBW Ratio
| Parameter | Population | Association | Strength of Evidence (Reference) |
|---|---|---|---|
| Phase Angle (PhA) | Centrally Obese Adults | Positive correlation with Skeletal Muscle Index (SMI) and Fat-Free Mass Index (FFMI); Inverse association with Visceral Adipose Tissue (VAT) in males. | [18] |
| Older Inpatients (Convalescent) | Negative association with Activities of Daily Living (ADLs) in both sexes. | [17] | |
| Type 2 Diabetes | Significantly lower in patients with microangiopathy (nephropathy, neuropathy); negatively correlated with HbA1c changes longitudinally. | [15] | |
| Community-Dwelling Older Adults | Reduced leg PhA predicts higher incidence of functional disability over 12 years. | [16] | |
| ECW/TBW Ratio | Centrally Obese Adults | Positive association with Fat Mass Index (FMI) and VAT; inverse association with SMI. | [18] |
| Older Inpatients (Convalescent) | Negative association with ADLs in both sexes; stronger than SMI in females. | [17] | |
| General Population (BMI > 25) | Stronger correlation with hematological inflammatory markers than PhA. | [19] | |
| Community-Dwelling Older Adults | Higher ECW/ICW resistance ratio predicts higher incidence of functional disability. | [16] |
Experimental Protocols for BIA Assessment
Standardized protocols are essential for obtaining reliable and reproducible BIA data.
Pre-Test Participant Preparation and Guidelines
Instruct participants to adhere to the following conditions before assessment [18] [20]:
- Fasting: Fast for 3-4 hours prior to measurement.
- Hydration: Avoid caffeine, alcohol, or energy drinks within 24 hours. Urinate 20 minutes before the test.
- Physical Activity: Refrain from strenuous physical activity for at least 12 hours prior.
- Medication and Supplements: Withhold diuretics for 7 days prior, if possible, and disclose any medication use.
- Clothing: Wear lightweight clothing and remove metal accessories/jewelry.
Measurement Procedure
- Device Calibration: Verify calibration according to the manufacturer's specifications.
- Participant Information: Input participant's sex, age, and height accurately.
- Positioning: The participant should stand barefoot on the footplate electrodes, with arms slightly abducted from the body and grasping the hand electrodes if using a tetra-polar or octopolar device [19] [20].
- Environment: Perform measurements in a temperature-controlled room (24–26°C) to minimize environmental influence [18]. Schedule tests for the same time of day (e.g., morning or early afternoon) to control for diurnal variation.
- Data Recording: Record the raw parameters (Resistance and Reactance) in addition to the device-calculated outputs (PhA, TBW, ECW, ICW) for future reference and validation.
Device Selection and Validation
Different BIA devices employ varying technologies (e.g., single-frequency vs. multi-frequency) and electrode configurations (e.g., hand-to-foot vs. foot-to-foot), which can influence results.
Table 2: Comparison of BIA Devices for Measuring Lower Limb Muscle Mass (vs. DXA) [20]
| Device Model | Technology | Frequencies | Mean Difference (Bias vs. DXA) | Limits of Agreement (LOA) | Correlation with DXA (r) |
|---|---|---|---|---|---|
| InBody 770 | 8-point, Multi-frequency | 1, 5, 50, 250, 500, 1000 kHz | -0.625 kg | 3.8 kg | 0.928 |
| Tanita MC780MA | 8-point, Multi-frequency | 5, 50, 250 kHz | -1.613 kg | 5.1 kg | 0.925 |
| StarBIA201 | Foot-to-foot, Dual-frequency | 5, 50 kHz | -0.141 kg | 4.3 kg | 0.902 |
| InBody 270 | 4-point, Dual-frequency | 20, 100 kHz | -0.587 kg | 4.0 kg | 0.917 |
| Tanita BC418 | 8-point, Single-frequency | 50 kHz | -2.731 kg | 5.7 kg | 0.903 |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions and Materials for BIA Studies
| Item | Function/Application | Examples/Considerations |
|---|---|---|
| Validated BIA Device | Core instrument for measuring impedance. | Select based on required frequency and segmentation (e.g., InBody 770, Seca mBCA 514, Akern BIA 101). Ensure validation against criterion methods like DXA for target population [18] [5] [20]. |
| Calibration Kit/Standard | Ensures ongoing accuracy and reliability of impedance measurements. | Use manufacturer-provided calibration solutions or resistors to verify device performance before each testing session. |
| Dual-Energy X-ray Absorptiometry (DXA) | Gold standard for validating BIA-derived body composition metrics like muscle mass and fat mass. | GE Lunar Prodigy; Hologic Horizon A. Critical for device validation studies [5] [20]. |
| Ultrasound System | Provides complementary, site-specific data on muscle architecture and quality (e.g., echogenicity). | Portable A-mode (BodyMetrix) or B-mode systems. Correlates with PhA and ECW/TBW, enhancing muscle quality assessment [21]. |
| Standardized Electrodes | Ensures consistent electrical contact and signal quality. | Pre-gelled, self-adhesive electrodes placed at standard anatomical sites (wrist and ankle for traditional BIA). |
| Data Analysis Software | For statistical analysis and interpretation of BIA parameters. | SPSS, R. Used for regression and correlation analyses common in BIA research [18] [19]. |
Total Body Water, Extracellular Water, and Phase Angle are indispensable parameters derived from BIA that provide deep insights into fluid distribution, cellular health, and body composition. PhA serves as a robust indicator of cellular integrity and muscle quality, while the ECW/TBW ratio is a sensitive marker of fluid imbalance and inflammation. Their validated associations with conditions like sarcopenia, metabolic syndrome, and functional disability make them powerful tools for risk stratification and monitoring intervention efficacy in research. Adherence to standardized measurement protocols and careful selection of validated equipment, as detailed in this document, is paramount for generating high-quality, reproducible data that can reliably inform scientific and clinical decision-making.
The Impedance Index and Its Correlation with Body Composition
Bioelectrical Impedance Analysis (BIA) is a widely used, non-invasive method for assessing body composition by measuring the body's electrical impedance in response to a painless, low-intensity alternating current [4]. The fundamental principle of BIA is that impedance, comprised of resistance (R) and reactance (Xc), can be used to assess the water content of biological tissues [5]. Lean tissues, rich in electrolytes and water, conduct electrical current well (low resistance), while adipose tissue, with lower water and electrolyte content, impedes current flow (high resistance) [4].
The Impedance Index is a foundational parameter in BIA, calculated as stature (height in cm) squared divided by resistance (Z or R at 50 kHz): RI = Height² / R₅₀ [5]. This index is a strong predictor of Total Body Water (TBW) [5] and, by extension, Fat-Free Mass (FFM), based on the assumption that TBW comprises approximately 73% of FFM [5]. The relationship between the Impedance Index and body composition compartments forms the basis for most BIA predictive equations.
Key BIA Parameters and Their Physiological Correlates
Beyond the Impedance Index, BIA yields several other parameters critical for interpreting results. Resistance (R) is the opposition to the flow of an alternating current through intra- and extracellular electrolyte solutions, primarily related to total body water [4] [5]. Reactance (Xc) arises from the capacitive properties of cell membranes, which act as capacitors, storing and releasing energy; it is therefore a marker of cellular integrity and body cell mass [4]. The Phase Angle (PhA) is the geometric relationship between resistance and reactance, calculated as PhA = arctan(Xc/R) × (180/π) [4]. It is a recognized indicator of cellular health, membrane integrity, and nutritional status [22] [4]. A higher phase angle suggests robust cellular integrity, whereas a lower phase angle can indicate cell death or malnutrition [22].
Table 1: Key Raw BIA Parameters and Their Physiological Significance
| Parameter | Symbol | Physiological Correlate | Interpretation |
|---|---|---|---|
| Resistance | R | Opposition to current flow, related to total body water [4] [5] | Higher values may indicate lower TBW or higher fat mass. |
| Reactance | Xc | Capacitance of cell membranes, related to cellular integrity and mass [4] | Higher values suggest healthier cell membranes and greater body cell mass. |
| Phase Angle | PhA | Ratio of Xc to R, marker of cellular health and nutritional status [22] [4] | A higher value indicates better cellular integrity and function. |
| Impedance Index | Height²/R | A strong predictor of Total Body Water and Fat-Free Mass [5] | The primary variable used in equations to predict FFM and TBW. |
Correlation of the Impedance Index with Body Composition Compartments
The Impedance Index is the cornerstone for predicting body composition compartments. Its correlation with various body components has been extensively validated against reference methods like Dual-Energy X-ray Absorptiometry (DXA).
Fat-Free Mass (FFM) and Total Body Water (TBW)
The Impedance Index shows a very strong, positive correlation with FFM and TBW. Studies report correlation coefficients as high as r = 0.95-0.97 when comparing BIA-derived FFM to DXA measurements [23] [5]. However, it is crucial to note that BIA can exhibit systematic bias; one study found BIA overestimated FFM by 3.1 kg (+7.2%) compared to DXA in a heterogeneous Brazilian sample [23]. Another large study in healthy adults showed BIA overestimated FFM by 2.0-3.4 kg depending on sex, despite high correlation coefficients (r=0.94-0.95) [5]. This underscores the need for population-specific validation.
Fat Mass (FM)
Since BIA often estimates FM indirectly as the difference between body weight and predicted FFM, the correlation for FM is also high but inverse. The same Brazilian study found BIA underestimated FM by 2.9 kg (-13.0%) compared to DXA [23]. The large US Marine study reported correlations for percent body fat (%BF) of r = 0.89-0.92, with BIA underestimating %BF by 2.8-4.2% [5].
Sarcopenia Risk (Appendicular Skeletal Muscle Mass)
The Phase Angle, derived from R and Xc, has been studied as a potential indicator for low muscle mass. In pediatric outpatients, the Phase Angle demonstrated moderate correlations with the Appendicular Skeletal Muscle Mass Index (ASMI) and Fat-Free Mass Index (FFMI) [22]. Its Area Under the Curve (AUC) for predicting a severely low ASMI was 0.743-0.785, indicating it is a reasonable, though not definitive, indicator of sarcopenia risk [22].
Visceral Adipose Tissue (VAT)
The correlation between BIA-derived VAT and reference methods is weaker than for whole-body measures. One study found a correlation of r = 0.74 for VAT when comparing MFBIA to DXA, but the concordance was low (CCC=0.34-0.68), suggesting BIA is less accurate for this specific compartment [5].
Table 2: Summary of BIA Correlation and Agreement with Reference Methods (e.g., DXA)
| Body Composition Compartment | Correlation with Reference (r) | Typical Bias (BIA vs. Reference) | Key Findings |
|---|---|---|---|
| Fat-Free Mass (FFM) | 0.95 - 0.97 [23] [5] | Overestimation of 2.0 - 3.4 kg [23] [5] | High precision, but consistent overestimation requires calibration. |
| Fat Mass (FM) | ~0.97 [23] | Underestimation of ~2.9 kg [23] | Inverse calculation from FFM leads to systematic error. |
| Percent Body Fat (%BF) | 0.89 - 0.92 [5] | Underestimation of 2.8% - 4.2% [5] | Good for population-level trends, may lack individual accuracy. |
| Visceral Adipose Tissue (VAT) | ~0.74 [5] | Variable / Low Concordance [5] | Not recommended for precise VAT measurement in research. |
| Phase Angle vs. ASMI | Moderate [22] | AUC for predicting low ASMI: 0.74 - 0.79 [22] | A useful screening tool, but not a surrogate for muscle mass diagnosis. |
Advanced BIA Methodologies and Instrumentation
BIA technology has diversified, leading to different instrument types with varying levels of accuracy and application.
- Single-Frequency BIA (SF-BIA): Typically operates at 50 kHz. These devices are affordable and easy to use but are more sensitive to hydration status and less effective in patients with abnormal fluid distribution [4].
- Multi-Frequency BIA (MF-BIA): Uses multiple frequencies (e.g., 5, 50, 250 kHz) to differentiate between Intra- and Extracellular Water (ICW and ECW). This provides more accurate estimates of body composition, especially in clinical populations [4] [5].
- Bioelectrical Impedance Spectroscopy (BIS): Measures impedance across a spectrum of frequencies, enabling the most accurate assessment of ICW and ECW distribution [4].
- Electrode Configuration: Consumer-grade bipolar devices (hand-to-hand or foot-to-foot) are common but can lack accuracy. Tetrapolar (electrodes on hand and foot) and octopolar (multiple electrodes on limbs) configurations are preferred in clinical and research settings for whole-body or segmental analysis with greater accuracy [4].
Experimental Protocols for BIA Research
Protocol 1: Validating a BIA Device Against a Criterion Method
This protocol is designed to assess the validity and bias of a BIA device compared to a reference method like DXA.
Objective: To determine the agreement between body composition parameters (FFM, FM, %BF) measured by a BIA device and DXA in a target population.
Materials:
- BIA device (e.g., tetrapolar or octopolar MF-BIA)
- DXA scanner
- Calibrated stadiometer and scale
- Disposable electrodes, alcohol swabs, measuring tape
Procedure:
- Participant Screening & Consent: Recruit participants according to the study's inclusion/exclusion criteria. Obtain written informed consent.
- Pre-Test Standardization: Instruct participants to adhere to the following for 24 hours prior to testing:
- Avoid strenuous exercise.
- Maintain normal hydration but avoid excessive fluid intake.
- Fast for 4-12 hours.
- Avoid alcohol and caffeine.
- Void bladder completely within 30 minutes before the test.
- Anthropometry: Measure and record body weight (in light clothing) and standing height without shoes.
- DXA Scan: Perform the whole-body DXA scan according to the manufacturer's protocol and standard operating procedures.
- BIA Measurement:
- Ensure the room temperature is stable (20-25°C).
- Have the participant lie in a supine position on a non-conductive surface for at least 5 minutes prior to measurement. Arms and legs should be abducted at an angle of approximately 45° from the torso.
- Clean the skin with alcohol at electrode placement sites: on the dorsal surfaces of the hand and foot, proximal to the metacarpophalangeal and metatarsophalangeal joints, and between the distal prominences of the radius and ulna (wrist) and the medial and lateral malleoli (ankle).
- Attach disposable electrodes to the designated sites.
- Initiate the BIA measurement and record the raw parameters: Resistance (R), Reactance (Xc), and Phase Angle (PhA), along with the device's estimates for FFM, FM, and TBW.
- Data Analysis:
- Perform Pearson correlation (r) and Lin's Concordance Correlation Coefficient (CCC) to assess precision and accuracy.
- Use Bland-Altman analysis to quantify bias and limits of agreement.
- Paired t-tests can be used to evaluate systematic differences.
Protocol 2: Assessing Sarcopenia Risk Using Phase Angle
This protocol uses raw BIA parameters to evaluate cellular health as a proxy for sarcopenia risk.
Objective: To evaluate the predictive value of the Phase Angle for identifying low muscle mass in a clinical or outpatient population.
Materials:
- A BIA device capable of reporting raw R and Xc values.
- Equipment for measuring appendicular skeletal muscle mass (e.g., DXA for ASMI) if validating.
Procedure:
- Participant Preparation: Follow the same pre-test standardization as in Protocol 1.
- BIA Measurement: Conduct the BIA measurement as described in Steps 3-5 of Protocol 1. Ensure raw R and Xc values are recorded.
- Phase Angle Calculation: Calculate the Phase Angle (PhA) as: PhA = arctan(Xc / R) × (180 / π). Most modern devices calculate this automatically.
- Muscle Mass Assessment: If correlating with muscle mass, perform a DXA scan to determine the Appendicular Skeletal Muscle Mass (ASMM). Calculate the Appendicular Skeletal Muscle Index (ASMI) as ASMI = ASMM / height².
- Data Analysis:
- Perform correlation analysis between PhA and ASMI or FFMI.
- Use Receiver Operating Characteristic (ROC) curve analysis to determine the optimal Phase Angle cut-off value for predicting low muscle mass (e.g., ASMI below -1 or -2 standard deviations of a reference population) and report the Area Under the Curve (AUC), sensitivity, and specificity [22].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Equipment for BIA Research
| Item | Specification / Example | Function in Research |
|---|---|---|
| BIA Analyzer | Multifrequency, Tetrapolar/Octopolar (e.g., InBody 770, Seca mBCA) | The core instrument for measuring impedance; research-grade models provide access to raw data (R, Xc) [4] [5]. |
| Reference Method Equipment | DXA Scanner (e.g., GE Lunar iDXA, Hologic Horizon) | Criterion method for validating BIA estimates of fat mass, lean mass, and bone mass [23] [5]. |
| Anthropometric Tools | Calibrated Stadiometer, Digital Scale | For accurate measurement of height and weight, which are critical for calculating the Impedance Index and body composition indices [5]. |
| Electrodes | Disposable, Pre-gelled ECG Electrodes | To ensure consistent and high-quality electrical contact with the skin at standard anatomical sites. |
| Skin Preparation | 70% Isopropyl Alcohol Swabs | To clean skin and reduce impedance at the electrode-skin interface for a more reliable measurement. |
| Data Collection Forms/Software | Customized CRF, Database (e.g., RedCap) | To systematically record participant data, raw BIA parameters, and device outputs. |
Assumption-Based Predictive Models versus Raw Data Interpretation
Bioelectrical impedance analysis (BIA) represents a widely adopted approach in body composition assessment across clinical, research, and athletic settings. This technique operates on two fundamentally distinct interpretive frameworks: assumption-based predictive models that generate quantitative estimates of body compartments, and raw data interpretation that provides qualitative insights into tissue characteristics and hydration status. The theoretical foundation of BIA rests upon the conductive properties of biological tissues, where impedance (Z) comprises resistance (R) and reactance (Xc) [4]. Resistance reflects opposition to electrical current flow through electrolyte-rich fluids, while reactance represents the capacitive properties of cell membranes that temporarily store and release energy [24]. Understanding the applications, limitations, and appropriate contexts for each interpretive approach is essential for researchers and practitioners employing BIA methodologies.
The evolution of BIA technologies has further diversified methodological applications, with devices varying significantly in measurement frequency, electrode configuration, and analytical capabilities [4]. Single-frequency BIA (SF-BIA) typically operates at 50 kHz, while multifrequency BIA (MF-BIA) employs multiple currents across a spectrum (e.g., 1-1000 kHz) to enable differentiated assessment of fluid compartments [4]. Electrode configurations range from bipolar (hand-to-hand or foot-to-foot) to tetrapolar and octopolar systems that permit segmental analysis [4]. These technical variations directly influence the applicability of both predictive models and raw parameter interpretation across different populations and research contexts.
Predictive Models in BIA: Theoretical Framework and Applications
Foundation of Predictive Modeling in BIA
Predictive models in BIA operate through mathematical equations that convert raw electrical parameters into quantitative estimates of body composition compartments. These models typically incorporate impedance measurements alongside anthropometric variables (height, weight, sex, age) through population-specific regression equations developed against reference methods [25]. The fundamental assumption underlying most predictive models is that the human body consists of conductive (fat-free mass) and non-conductive (fat mass) components, with fat-free mass displaying relatively constant hydration (~73%) [5]. This theoretical framework enables the estimation of various body compartments including fat mass (FM), fat-free mass (FFM), total body water (TBW), and skeletal muscle mass (SMM) through device-specific proprietary algorithms [4] [25].
The development of predictive equations requires validation against criterion methods, with choice of reference standard significantly influencing model validity [25]. Common reference methods include dual-energy X-ray absorptiometry (DXA) for fat, fat-free and lean soft tissue mass; dilution techniques (deuterium oxide, sodium bromide) for total body water and extracellular water; total-body potassium for body cell mass; and magnetic resonance imaging (MRI) or computed tomography for skeletal muscle mass [25]. The population characteristics used in equation development directly impact applicability, with factors including age, geographical ancestry, health status, physical activity level, and sex necessitating careful model selection [25].
Table 1: Reference Methods for BIA Predictive Equation Development
| Body Compartment | Criterion Reference Method | Validation Approach |
|---|---|---|
| Fat Mass (FM) & Fat-Free Mass (FFM) | 4-compartment model, DXA, ADP | Cross-validation in specific populations |
| Total Body Water (TBW) | Deuterium oxide dilution | Isotopic dilution techniques |
| Extracellular Water (ECW) | Sodium bromide dilution | Isotopic dilution techniques |
| Body Cell Mass (BCM) | Total-body potassium | Gamma-ray spectrometry |
| Skeletal Muscle Mass (SMM) | MRI, CT | Imaging-based volumetric analysis |
Applications and Limitations of Predictive Models
Predictive models find extensive application in body composition assessment across diverse settings including clinical nutrition, sports science, and population health studies. In professional football, for instance, BIA-derived predictive equations specific to athletes have been developed to monitor body composition changes during training seasons [24]. Similarly, in aging research, predictive models enable screening for sarcopenia through estimation of appendicular skeletal muscle mass [20]. The practicality of these models facilitates longitudinal tracking of body composition changes in response to interventions, making them valuable tools in both research and clinical practice.
Significant limitations nevertheless constrain predictive model applications. A systematic review identified 106 distinct predictive equations, with appropriate selection dependent on device type and population characteristics [25]. Manufacturer proprietary algorithms often lack transparency, potentially incorporating undisclosed assumptions that limit clinical utility [4]. Validation studies consistently demonstrate substantial discrepancies between BIA predictions and reference standards, with one study reporting BIA overestimation of fat-free mass by 3.1 kg compared to DXA [23]. These limitations highlight the critical importance of selecting population-specific validated equations rather than relying on generic manufacturer algorithms.
Table 2: Comparative Accuracy of BIA Predictive Models Versus DXA Reference
| BIA Device Type | Population | Body Compartment | Bias (kg) | Limits of Agreement (kg) | Correlation with DXA |
|---|---|---|---|---|---|
| Tanita BC-418 | Brazilian adults & elderly [23] | Fat-Free Mass | +3.1 | -2.4 to +8.6 | r = 0.97 |
| Tanita BC-418 | Brazilian adults & elderly [23] | Fat Mass | -2.9 | -7.5 to +1.7 | r = 0.97 |
| InBody 770 | Healthy adults [5] | Fat Mass (men) | -3.7 | ±2.6 | r = 0.93 |
| InBody 770 | Healthy adults [5] | Fat Mass (women) | -1.9 | ±1.8 | r = 0.96 |
| Multiple devices [20] | Middle-aged/elderly | Lower Limb Muscle Mass | -2.7 to -0.1 | ±3.8 to ±5.7 | r = 0.90-0.93 |
Raw Data Interpretation in BIA: Principles and Applications
Theoretical Foundation of Raw Parameter Analysis
Raw bioelectrical parameters provide direct measurements of the body's electrical properties without incorporation into predictive models. The fundamental raw parameters include resistance (R), representing opposition to current flow through intra- and extracellular fluids; reactance (Xc), reflecting capacitive properties of cell membranes; and phase angle (PhA), calculated as the arctangent of Xc/R × (180°/π), representing the phase difference between voltage and current [24] [26]. These parameters serve as direct markers of tissue composition and cellular health, with PhA particularly recognized as an indicator of cell membrane integrity and body cell mass [24].
Bioelectrical Impedance Vector Analysis (BIVA) represents a prominent methodology for raw parameter interpretation, plotting resistance and reactance standardized by height on a nomogram to assess hydration and cellular condition without population-specific assumptions [4]. This approach analyzes vector position and length relative to reference confidence ellipses, with shorter vectors indicating fluid overload and longer vectors suggesting dehydration [4]. The technique has gained recognition for monitoring physiological changes in diverse populations including athletes, critically ill patients, and elderly individuals, where conventional predictive models may prove inaccurate due to non-standard hydration status or body composition [4] [24].
Research and Clinical Applications of Raw Parameters
Raw parameter analysis provides valuable insights across multiple research and clinical contexts. In critical care medicine, significantly lower phase angle values have been documented in ICU patients compared to healthy volunteers (4.5° vs. 6.1°), reflecting cellular dysfunction and nutritional status independent of fluid imbalances [27]. Similarly, non-survivors demonstrate higher extracellular water content and capillary leak index (ECW/ICW ratio), offering prognostic value in intensive care settings [27]. These applications demonstrate the clinical utility of raw parameters where predictive models may fail due to pathological conditions affecting standard body composition assumptions.
Sports science represents another domain where raw parameter analysis provides unique advantages. Studies in professional football have utilized phase angle as a marker of cellular integrity and training adaptation, with BIVA enabling assessment of hydration shifts and cellular changes without sport-specific equations [24]. Research in youth populations has further demonstrated strong associations between raw parameters and body components at molecular, cellular, and tissue levels, with resistance adjusted for stature emerging as a particularly informative marker [26]. These applications highlight the versatility of raw parameter analysis across diverse physiological states and population characteristics.
Diagram 1: Raw BIA parameter relationships with physiological interpretations. Resistance and impedance primarily reflect hydration status, reactance indicates cellular health, while phase angle serves as a marker of membrane integrity with clinical prognostic value.
Comparative Methodological Analysis: Protocols and Validation
Experimental Protocols for Predictive Model Validation
Validation of BIA predictive models requires rigorous methodological protocols employing criterion methods as reference standards. The following protocol outlines a comprehensive validation approach based on established research methodologies [23] [20]:
Participant Preparation and Standardization
- Maintain usual daily routines while avoiding alcohol consumption and strenuous exercise for ≥48 hours pre-testing
- Implement fasting conditions (including water restriction) until completion of assessments
- Standardize testing time (e.g., afternoon) to minimize diurnal variation effects
- Instruct participants to void urine 20 minutes prior to measurements for stable body water levels
Measurement Procedures
- Conduct BIA and reference method (DXA) assessments sequentially within a controlled timeframe (e.g., 90 minutes)
- Utilize calibrated BIA devices with documented electrode configurations (tetrapolar/octopolar preferred)
- For DXA reference: Position participants supine with arms extended alongside body, feet together
- Perform all measurements in temperature-controlled environments (26-28°C) with participants wearing standardized clothing
Statistical Validation Analysis
- Assess agreement using Pearson correlation coefficients (precision) and Lin's concordance correlation coefficients (accuracy)
- Evaluate mean absolute and relative differences via paired t-tests or ANOVA stratified by sex, age, and nutritional status
- Employ Bland-Altman analysis to determine bias and limits of agreement
- Develop calibration models using linear regression with randomly selected development (70%) and validation (30%) subsamples
This protocol framework has demonstrated effectiveness in identifying significant discrepancies between BIA and reference methods, enabling development of calibrated equations that improve agreement with criterion measures [23].
Experimental Protocols for Raw Parameter Applications
Raw parameter analysis employs distinct methodological approaches focused on direct electrical measurements rather than derived body composition estimates. The following protocol details standardized assessment based on established BIVA methodologies [4] [24] [27]:
Measurement Conditions and Instrumentation
- Utilize phase-sensitive BIA devices capable of measuring resistance and reactance at 50 kHz
- Employ tetrapolar electrode configurations (wrist and ankle placements) for whole-body assessment
- Position participants in a completely supine position with limbs abducted from the body
- Ensure skin preparation with alcohol cleansing at electrode placement sites
Data Collection and Analysis
- Measure resistance (R) and reactance (Xc) directly from device output
- Calculate phase angle as: PhA = arctan(Xc/R) × (180°/π)
- Standardize values by height: R/h and Xc/h (Ω/m)
- Plot individual vectors on R-Xc graphs with reference population tolerance ellipses
Interpretation Framework
- Evaluate vector position relative to reference ellipses for hydration status assessment
- Interpret longer vectors as indicating dehydration; shorter vectors suggesting fluid overload
- Analyze phase angle values against population norms: lower values indicate reduced cellular integrity/mass
- Monitor vector migration in longitudinal assessments to track physiological changes
This protocol enables qualitative assessment of hydration status and cellular health without population-specific assumptions, proving particularly valuable in clinical populations with abnormal fluid distribution or body composition [27].
Diagram 2: Methodological workflow for BIA predictive model development and validation, highlighting critical standardization procedures and sequential assessment phases.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BIA Methodologies
| Category | Specific Instrument/Reagent | Research Application | Technical Considerations |
|---|---|---|---|
| BIA Devices | Multi-frequency BIA (e.g., InBody 770, SECA mBCA) | Body composition assessment across fluid compartments | Multiple frequencies (1-1000 kHz) enable ICW/ECW differentiation [4] |
| BIA Devices | Single-frequency BIA (50 kHz) | Basic body composition screening | Limited to TBW estimation; requires population-specific equations [4] |
| BIA Devices | Bioelectrical Impedance Spectroscopy (BIS) devices | Precise fluid compartment analysis | Measures impedance spectrum for improved ICW/ECW modeling [4] |
| Reference Standards | Dual-Energy X-Ray Absorptiometry (DXA) | Validation of fat, fat-free, lean soft tissue mass | Considered criterion method for body composition analysis [25] |
| Reference Standards | Isotope dilution systems (deuterium oxide, sodium bromide) | Validation of TBW and ECW compartments | Criterion method for body water assessment [25] |
| Reference Standards | Magnetic Resonance Imaging (MRI) | Validation of skeletal muscle and adipose tissue | Volumetric assessment of specific tissues [25] |
| Consumables | Electrode gels and cleansing wipes | Ensuring proper electrode-skin contact | Reduce impedance artifacts from poor contact [20] |
| Consumables | Standardized clothing (gowns) | Minimizing measurement variability | Lightweight cotton (∼450g) documented [20] |
| Calibration Tools | Biological phantoms | Device calibration verification | Quality control for measurement consistency |
| Software | BIVA-specific analysis programs | Raw parameter vector analysis | Enables plotting against reference populations [4] |
Integrated Decision Framework for Method Selection
The choice between assumption-based predictive models and raw data interpretation depends on research objectives, population characteristics, and methodological constraints. Predictive models provide optimal utility in population-level assessments where specific equations have been validated against appropriate reference methods in comparable cohorts [25]. In contrast, raw parameter analysis offers advantages in clinical populations with fluid imbalances or atypical body composition, where standard predictive assumptions may prove invalid [27]. The following decision framework supports appropriate methodological selection:
Contexts Favoring Predictive Models
- Longitudinal tracking of body composition changes in stable populations
- Nutritional intervention studies requiring quantitative compartment estimates
- Athletic monitoring with sport-specific validated equations
- Epidemiological research with large sample sizes
Contexts Favoring Raw Parameter Interpretation
- Critical care settings with fluid shifts and edema
- Populations lacking validated predictive equations
- Cellular health assessment independent of body size
- Rapid screening without demographic data availability
Hybrid approaches increasingly demonstrate utility, with studies combining traditional predictive models with raw parameter analysis to enhance interpretive power [24] [26]. For example, phase angle provides complementary information when interpreted alongside conventional body composition estimates, potentially identifying confounding factors such as hyperhydration or cellular dysfunction. This integrated approach represents a promising direction for advancing BIA methodologies across research and clinical applications.
Assumption-based predictive models and raw data interpretation represent complementary analytical frameworks within bioelectrical impedance analysis, each with distinct strengths, limitations, and appropriate applications. Predictive models offer practical quantitative assessment of body composition compartments when population-specific validated equations are available, while raw parameters provide valuable insights into hydration status and cellular integrity independent of predictive assumptions. Methodological selection should be guided by research objectives, population characteristics, and available validation evidence, with emerging integrated approaches offering enhanced interpretive power. Continuing advancement in both methodologies will further strengthen the role of BIA in body composition research across diverse populations and settings.
Methodological Approaches and Translational Applications in Research and Clinic
Bioelectrical Impedance Analysis (BIA) estimates body composition by measuring how the body's tissues impede a low-level electrical current. These tissues vary in conductivity due to differences in water and electrolyte content; lean tissue, being more hydrated, is highly conductive, while fat and bone act as insulators [28]. BIA devices are classified by their electrode configuration and current path, which significantly influence measurement accuracy, clinical application, and suitability for different populations [28] [4].
The table below summarizes the core technical characteristics, applications, and key considerations for the primary BIA configurations.
Table 1: Technical Specifications and Applications of BIA Configuration Types
| Configuration Type | Technical Principle & Current Path | Primary Applications & Populations | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Hand-Held (Bipolar) | Single-frequency; current flows between hands via hand-grip electrodes [28]. | Field studies, gyms, general population screening for group-level data [4]. | High convenience and portability; rapid assessment [4]. | Only measures upper body; proprietary algorithms; lower individual accuracy; overlooks lower body and trunk composition [4]. |
| Leg-to-Leg (Bipedal) | Single-frequency; current flows between feet via footplate electrodes on a scale [28] [13]. | Home use, commercial settings, epidemiological group studies [28] [13]. | Extremely user-friendly; integrates with a weight scale [28]. | Only measures lower body; underestimates abdominal fat; significant individual error; systematic bias in visceral fat estimation [13] [29]. |
| Hand-to-Foot (Tetrapolar) | Single- or multi-frequency; current flows from hand to foot, traversing the trunk [28] [4]. | Clinical practice, research settings, nutritional assessment, and patient monitoring [4]. | More complete whole-body measurement; higher validity than bipolar devices; suitable for bedridden patients [28] [13] [4]. | Requires placement of electrodes on hand and foot; less convenient than bipedal/hand-held devices [4]. |
| Segment-Specific (Octopolar/Advanced) | Multi-frequency or spectroscopy; uses multiple electrodes (often 8) for bilateral hand-to-foot and segmental analysis [30] [31] [4]. | Research, elite sports, clinical diagnostics, and conditions with fluid imbalances (e.g., dialysis) [31] [4]. | Enables analysis of individual body segments (arms, trunk, legs); highest accuracy for fluid distribution and lean mass; sensitive to trunk changes [31] [4]. | Highest cost; requires specialized expertise; complex operation and data interpretation [31] [4]. |
Comparative Validity and Reliability of Configurations
The choice of configuration significantly impacts the accuracy and reliability of body composition data, especially for visceral fat assessment and tracking changes over time.
Table 2: Comparative Validity of BIA Configurations Against Reference Methods
| Configuration | Performance Against 4-Compartment (4C) Model/DXA | Performance in Visceral Fat Assessment | Longitudinal Validity (Tracking Changes) |
|---|---|---|---|
| Hand-Held / Leg-to-Leg (Bipolar) | Wide limits of agreement vs. 4C model. Tend to overestimate fat in lean individuals and underestimate it in obese individuals [28] [13]. Individual error rates can be very high (e.g., ±5 kg FM) [28]. | Poor agreement with CT. Leg-to-leg BIA showed significant differences, overestimating in males and underestimating in females. Limits of Agreement (LOA%) can be as high as 48.2% [29]. | Prone to misrepresent changes over time. High individual disagreement with the 4C model when measuring changes in FM and FFM [28]. |
| Hand-to-Foot (Tetrapolar) | Shows better agreement than bipolar devices. One study found a low mean bias (<1.5 %FM) and narrowest limits of agreement (-6.59 to 4.61 %FM) compared to bipolar devices [13]. | More accurate than leg-to-leg systems due to the current path encompassing the trunk, though specific data vs. CT is less available. | Generally more reliable for tracking than bipolar devices, though performance depends on the specific device and population [30]. |
| Segment-Specific (Octopolar) | Demonstrates high cross-sectional validity. One multi-device study found octopolar devices had some of the smallest constant errors (e.g., -3.5%) and high concordance (CCC=0.94) with a 4C model [30]. | The segmental approach is inherently more sensitive to changes in the trunk, where visceral fat is located [31]. | Shows the highest potential for accurately tracking body composition changes over time, with high Lin's CCC (up to 0.78) in longitudinal studies [30]. |
Experimental Protocols for BIA Assessment
Standardized protocols are critical for obtaining reliable and reproducible BIA measurements, regardless of the device configuration used.
General Pre-Test Standardization Protocol
The following conditions must be met prior to testing to ensure stable hydration and minimize confounding variables [30]:
- Fasting/Fluid Restriction: No food, fluid, caffeine, or alcohol for a minimum of 8 hours prior to the test [30].
- Exercise Abstention: No exercise or vigorous physical activity for at least 24 hours before assessment [30].
- Bladder Evacuation: Participants must void their bladder immediately before the measurement session [30].
- Hydration Standardization: For visits scheduled later in the day, instruct participants to ingest 1 litre of water between their last meal and the beginning of the 8-hour fluid abstention period [30].
- Clothing: Participants should wear light, skin-tight clothing and remove all metal jewelry, accessories, and shoes [30].
- Body Position: For standing devices, the participant must remain in an upright, standing position for at least 10 minutes before the first measurement to allow for fluid stabilization [30].
Device-Specific Measurement Protocols
Protocol A: Hand-to-Foot (Tetrapolar) & Segment-Specific (Octopolar) Configuration This protocol is for research-grade devices, often used in clinical and laboratory settings [4].
- Electrode Placement: Clean the skin with alcohol at electrode sites. For a traditional tetrapolar setup, place two signal electrodes on the dorsal surfaces of the right hand and right foot, just proximal to the metacarpophalangeal and metatarsophalangeal joints. Place the two detection electrodes at the right wrist (between the styloid processes) and the right ankle (between the malleoli) [4].
- Participant Positioning: Position the participant supine on a non-conductive surface, with limbs slightly abducted from the body to prevent contact between torso and limbs. For octopolar devices that require standing, the participant stands barefoot on the footplates and grasps the handgrips with arms extended away from the body [30] [4].
- Measurement: Initiate the device to run the impedance analysis. For segmental or octopolar devices, the device will typically cycle through multiple segments automatically [31].
- Data Recording: Record the raw impedance parameters (Resistance-R, Reactance-Xc) and Phase Angle-PhA, if available, in addition to the device's estimated body composition values [4].
Protocol B: Leg-to-Leg (Bipedal) Configuration This protocol is for consumer-grade scale-style devices [28] [13].
- Device Preparation: Ensure the scale is on a flat, hard surface. Calibrate the device according to manufacturer instructions, if required.
- Participant Preparation: The participant should be barefoot. Enter the participant's ID, height, age, and sex into the device as required.
- Positioning: The participant stands upright on the footplates, ensuring feet are clean, dry, and making full contact with the electrodes. Arms should be held away from the body.
- Measurement: The participant remains still while the device takes the measurement. The result is typically displayed within seconds.
Protocol C: Hand-Held Configuration This protocol is for upper-body-focused consumer devices [28].
- Device Preparation: Ensure the device's batteries are functional.
- Participant Preparation: Enter the participant's demographic data (height, age, sex, etc.) if the device requires it.
- Positioning: The participant holds the device with both hands, extending arms forward to ensure no contact between arms and torso. Fingers must make good contact with the electrodes.
- Measurement: The participant holds the position until the measurement is complete.
Signaling Pathways and Experimental Workflows
BIA Measurement and Data Interpretation Workflow
The diagram below outlines the logical flow from measurement to clinical interpretation, highlighting the role of raw data access for applying population-specific equations.
Decision Pathway for BIA Configuration Selection
This diagram provides a logical framework for researchers to select the most appropriate BIA configuration based on their study objectives, population, and resource constraints.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below details key materials and their functions for conducting rigorous BIA research, particularly when validating devices or developing new equations.
Table 3: Essential Materials and Reagents for BIA Research
| Item | Specification / Function in Research |
|---|---|
| Research-Grade BIA Device | An octopolar or tetrapolar multifrequency/BIS device that provides access to raw bioelectrical parameters (R, Xc, PhA). Essential for applying validated, population-specific equations [30] [4]. |
| Disposable Electrodes | Pre-gelled, hypoallergenic, single-use electrodes for tetrapolar and segmental devices. Ensure consistent skin contact and hygiene, and minimize inter-measurement variability [4]. |
| Calibration Verification Kit | A set of precision resistors and capacitors used to verify the accuracy and reliability of the BIA device's electrical measurements before data collection [31]. |
| Reference Method Equipment | Equipment for criterion methods like DXA (for fat, lean, and bone mass), Air Displacement Plethysmography (for body volume), or Deuterium Oxide Dilution (for total body water). Required for cross-validation studies and developing prediction equations [30] [23]. |
| Anthropometric Kit | A calibrated stadiometer for height and a certified digital scale for weight. These are critical inputs for all BIA prediction models [30] [23]. |
| Standardization Supplies | Skin cleaning alcohol wipes, measuring tape for waist circumference, and compression clothing for participants. These ensure standardized pre-test conditions and minimize measurement confounders [30]. |
Bioelectrical Impedance Analysis (BIA) represents a widely adopted, non-invasive methodology for assessing body composition in both research and clinical settings [4]. The technique operates on the principle that different biological tissues impede the flow of an alternating electrical current to varying degrees; lean body mass, rich in electrolytes and water, conducts electricity effectively, whereas fat mass acts as an insulator [32]. Two primary technological approaches dominate the field: Single-Frequency BIA (SF-BIA) and Multi-Frequency BIA (MF-BIA). The distinction between them is foundational, impacting the accuracy, applicability, and interpretability of results in body composition research. This application note delineates the technical specifications, underlying principles, and appropriate use cases for each technology, providing researchers and drug development professionals with evidence-based protocols for their implementation.
Technical Foundations and Key Distinctions
The core difference between SF-BIA and MF-BIA lies in the spectrum of electrical frequencies employed and the consequent depth of body composition analysis they enable.
Single-Frequency BIA (SF-BIA): Traditionally, SF-BIA devices operate at a fixed frequency of 50 kHz [4] [33]. At this frequency, the electrical current primarily traverses the extracellular water (ECW) compartment. The fundamental parameter measured is impedance (Z), a composite of resistance (R) and reactance (Xc) [33]. SF-BIA provides robust, population-level estimates of total body water (TBW), which can be used to derive fat-free mass (FFM) and, by difference with body weight, fat mass (FM) [4] [32]. Its operation is predicated on the assumption of a stable hydration status for FFM (approximately 73%), which can be a significant source of error in individuals with fluid imbalances [33] [34].
Multi-Frequency BIA (MF-BIA): MF-BIA devices utilize a range of frequencies, typically from 1–5 kHz up to 500–1000 kHz [4] [5]. This range is critical because low-frequency currents (e.g., 5 kHz) cannot penetrate cell membranes and thus primarily reflect ECW, while high-frequency currents (e.g., 200-1000 kHz) can cross cell membranes and therefore enable assessment of both intracellular water (ICW) and TBW [4] [7]. This capability allows MF-BIA to differentiate between fluid compartments, providing a more nuanced evaluation of body composition, particularly in conditions where fluid distribution is altered, such as in obesity, cachexia, or renal disease [4].
Table 1: Comparative Technical Specifications of SF-BIA and MF-BIA
| Feature | Single-Frequency BIA (SF-BIA) | Multi-Frequency BIA (MF-BIA) |
|---|---|---|
| Typical Frequencies | 50 kHz [4] | 1, 5, 50, 250, 500, 1000 kHz [5] [20] |
| Fluid Compartments Assessed | Total Body Water (TBW) [33] | Extracellular Water (ECW) & Intracellular Water (ICW) [4] |
| Primary Outputs | Fat-Free Mass (FFM), Fat Mass (FM) [4] | FFM, FM, ECW, ICW, Segmental Lean Mass [4] [5] |
| Common Electrode Configurations | Bipolar (hand-to-hand, foot-to-foot) [4] | Tetrapolar or Octopolar (hand-to-foot) [4] |
| Typical Cost & Complexity | Lower cost, consumer-grade [4] | Higher cost, research/clinical-grade [4] |
| Key Assumption | Stable FFM hydration (~73%) [33] [34] | Can account for some variation in fluid distribution [4] |
Quantitative Validation and Performance Data
The validity and reliability of BIA technologies are routinely assessed against criterion methods such as Dual-Energy X-ray Absorptiometry (DXA) and deuterium oxide dilution (D2O).
A large-scale real-world study (n=1000) comparing an octopolar MF-BIA device (InBody 770) to DXA demonstrated high reliability and modest agreement at the population level. The study reported high retest reliability for both DXA (ICC 0.990–0.998) and MF-BIA (ICC 0.987–0.995) [5]. For total body fat mass, correlations with DXA were strong (men: r=0.93, bias -3.7 kg; women: r=0.96, bias -1.9 kg), though the notable biases highlight the need for method-specific interpretation [5]. Another study focusing on lower limb muscle mass (LLMM) in an elderly cohort compared various BIA devices against DXA. The results, summarized in Table 2, show that while all devices correlated highly with DXA (r > 0.90), only some models, such as the foot-to-foot dual-frequency device (StarBIA201) and the InBody270, showed no significant fixed or proportional bias [20].
For TBW estimation, a validation study of the InBody 770 in women (n=55) found almost perfect agreement with the gold-standard D2O method (Mean Difference = 0.34 L, CCC = 0.98), supporting its use for accurate fluid assessment in research [34].
Table 2: Agreement of BIA Devices with DXA for Lower Limb Muscle Mass (LLMM) Assessment [20]
| BIA Device (Model) | Frequency Type | Correlation with DXA (r) | Mean Difference (Bias, kg) | Limits of Agreement (kg) |
|---|---|---|---|---|
| StarBIA201 | Dual-Frequency (5, 50 kHz) | 0.902 | -0.141 | ± 4.3 |
| Tanita BC418 | Single-Frequency (50 kHz) | 0.903 | -2.731 | ± 5.7 |
| InBody270 | Dual-Frequency (20, 100 kHz) | 0.917 | -0.587 | ± 4.0 |
| Tanita MC780MA | Triple-Frequency (5, 50, 250 kHz) | 0.925 | -1.613 | ± 5.1 |
| InBody770 | Six-Frequency (1, 5, 50, 250, 500, 1000 kHz) | 0.928 | -0.625 | ± 3.8 |
Advanced Analytical Approaches: BIVA and Phase Angle
Beyond the estimation of body composition masses, BIA provides raw bioelectrical parameters that are independent of predictive equations: Resistance (R), Reactance (Xc), and the derived Phase Angle (PhA).
Phase Angle (PhA): Calculated as PhA = arctan(Xc/R) × (180/π), PhA is a marker of cellular integrity and nutritional status [4] [35]. A higher PhA indicates robust cell membranes and better cellular function, and it has proven to be a prognostic indicator in various chronic diseases including cancer, HIV, and renal failure [4].
Bioelectrical Impedance Vector Analysis (BIVA): This technique bypasses predictive equations by graphically analyzing the relationship between height-adjusted R and Xc [4] [36]. The position and displacement of the resulting vector on a nomogram provide a qualitative assessment of hydration status (vector length) and cellular mass (vector direction) [36]. BIVA is particularly valuable for monitoring physiological changes over time, such as fluid shifts in athletes or patients, without the confounding factor of population-specific equations [36] [35].
Application-Based Use Case Selection
The choice between SF-BIA and MF-BIA should be guided by the research question, population, and required precision.
Appropriate Use Cases for SF-BIA: SF-BIA is well-suited for large-scale epidemiological studies in generally healthy populations with normal hydration, where cost-effectiveness and rapid assessment are priorities [4]. It is also adequate for tracking group-level changes in body composition in fitness and wellness contexts [32].
Appropriate Use Cases for MF-BIA: MF-BIA is the preferred technology in clinical research and drug development where precise monitoring of fluid shifts or muscle mass is critical. This includes studies in nephrology (dialysis patients), oncology (cachexia), cardiology (heart failure), and geriatrics (sarcopenia) [4] [20]. MF-BIA is also essential for sports nutrition research where segmental analysis of muscle mass and close monitoring of hydration status are required [36] [35].
The following decision pathway provides a visual guide for technology selection:
Detailed Experimental Protocols
Protocol 1: Whole-Body Composition Assessment using MF-BIA
This protocol is designed for research requiring comprehensive body composition data, including fluid compartment analysis [4] [5] [34].
Objective: To accurately assess total and segmental body composition, including fat mass, fat-free mass, and body water compartments (ECW and ICW), in a research cohort. Materials:
- Multi-frequency bioelectrical impedance analyzer (e.g., InBody 770, Seca mBCA)
- Calibrated stadiometer
- Standard laboratory conditions (room temperature 22–24 °C)
Pre-Test Participant Preparation:
- Fasting: Participants should fast for a minimum of 4 hours prior to testing [5] [20].
- Hydration: Avoid alcohol and caffeine for 24 hours and avoid vigorous physical activity for 12 hours before the test [20].
- Bladder Evacuation: Participants should void their bladder approximately 20 minutes before the measurement [20].
- Clothing: Participants should wear light, metal-free clothing and remove all jewelry.
Measurement Procedure:
- Participant Information: Input the participant's age, sex, and height into the BIA device.
- Positioning: For a standing octopolar device, the participant stands barefoot on the device's foot electrodes and grips the hand electrodes, ensuring arms are slightly abducted from the body [5].
- Skin Preparation: If using adhesive electrodes, the skin should be cleansed with alcohol at electrode placement sites (wrist and ankle).
- Measurement: The participant remains still during the approximately 1–2 minute measurement cycle. Ensure limbs are not touching the torso.
Data Recording and Analysis:
- Record the raw parameters: Resistance (R), Reactance (Xc), and Phase Angle at multiple frequencies.
- Document the device-generated outputs for FM, FFM, SMM, TBW, ECW, and ICW.
- For the highest accuracy, use population-specific equations if available, rather than relying solely on the device's proprietary algorithms [4].
Protocol 2: Longitudinal Monitoring with Bioelectrical Impedance Vector Analysis (BIVA)
This protocol is ideal for studies monitoring hydration and cellular health changes over time, such as in athletic training or clinical intervention studies [36] [35].
Objective: To qualitatively monitor shifts in hydration status and body cell mass in response to an intervention or training regimen, independent of predictive equations. Materials:
- A phase-sensitive, tetrapolar BIA device capable of providing raw R and Xc values at 50 kHz.
- Electrodes and skin preparation supplies.
Procedure:
- Standardization: Adhere strictly to the pre-test preparation guidelines from Protocol 1. Consistency in timing, posture, and conditions for all sequential measurements is critical [36].
- Measurement: Place electrodes on the right hand and foot following a standard tetrapolar placement. Measure R and Xc at 50 kHz.
- Calculation: Standardize R and Xc by the participant's height (R/H and Xc/H).
- Plotting: Plot the resulting vector (R/H, Xc/H) on the BIVA tolerance ellipse specific to the study population (if available) or a general reference ellipse.
Interpretation:
- Hydration: A vector longer than the 95% tolerance ellipse suggests dehydration, while a shorter vector indicates fluid overload [4] [36].
- Cell Mass: A vector located to the left and shorter may indicate loss of body cell mass, whereas a vector to the right and longer suggests an increase in cellularity [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials for BIA Research and Their Functions
| Item | Specification/Function |
|---|---|
| Multifrequency BIA Analyzer | Core device for measuring impedance across frequencies (e.g., 1–1000 kHz) to differentiate ICW and ECW [4] [5]. |
| Single-Frequency BIA Analyzer | Device for basic TBW and FFM estimation at 50 kHz; suitable for group-level analysis in healthy populations [4] [33]. |
| Adhesive Electrodes (Tetrapolar) | Single-use electrodes for precise placement on wrist and ankle; minimize skin-electrode interface artifact [4]. |
| Calibrated Stadiometer | For accurate height measurement, a critical input for standardizing impedance values and calculating body composition [5] [20]. |
| Bioimpedance Vector Analysis (BIVA) Software | Software for plotting R/H vs. Xc/H and comparing vectors to reference confidence ellipses for qualitative assessment [4] [36]. |
| Population-Specific Equations | Validated prediction equations for converting raw BIA data into body composition metrics for specific cohorts (e.g., elderly, athletes) [4] [35]. |
The selection between Single-Frequency and Multi-Frequency BIA is a critical methodological decision in body composition research. SF-BIA offers a cost-effective solution for large-scale studies in healthy populations where group-level trends are sufficient. In contrast, MF-BIA provides a more sophisticated, granular analysis of body composition, including fluid compartments and segmental lean mass, making it indispensable for clinical research, drug development, and sports science where precision and monitoring of physiological changes are paramount. Adherence to standardized protocols and consideration of advanced techniques like BIVA are essential for generating reliable and interpretable data, ultimately reinforcing the validity of research outcomes in human health and disease.
Electric Cell-substrate Impedance Sensing (ECIS) for Real-Time Cell Behavior Monitoring
Electric Cell–substrate Impedance Sensing (ECIS) is a real-time, label-free, impedance-based method used to study various cell behaviors, including cell growth, viability, migration, and barrier function in vitro [37]. This technology operates on the fundamental principles of bioelectrical impedance, measuring how cells impede the flow of a small alternating current. Within the broader field of bioelectrical impedance analysis (BIA), which encompasses well-established techniques for body composition assessment in clinical settings, ECIS represents a sophisticated in vitro application of the same core biophysical principles [38] [37].
While clinical BIA often estimates tissue-level compartments like fat-free mass and total body water, ECIS applies impedance measurement at a microscopic scale to monitor cellular activities and the integrity of cell monolayers [38] [37]. The ECIS technology distinguishes itself by using electrodes integrated into the bottom of cell culture wells, allowing cells to attach and proliferate directly on them. This setup enables highly sensitive, localized measurements of impedance across a broad frequency range (62.5 Hz to 64 kHz), providing a powerful tool for fundamental biological research and drug development [37].
Key Applications and Measurable Parameters in Cell Research
ECIS serves as a versatile platform for investigating dynamic cellular processes. Its key applications and the quantitative data it provides are summarized in the table below.
Table 1: Key Applications and Outputs of ECIS Analysis
| Application Area | Measurable Parameters | Significance in Research & Drug Development |
|---|---|---|
| Barrier Function Monitoring | Transepithelial/Transendothelial Electrical Resistance (TEER); Capacitance (C) | Quantifies integrity of cellular barriers (e.g., intestinal, blood-brain); assesses compound toxicity and protective agents [37]. |
| Cell Growth & Proliferation | Impedance (Z) over time; Cell Index | Enables label-free, real-time kinetic monitoring of cell proliferation, eliminating the need for endpoint assays [37]. |
| Cell Migration & Wound Healing | Resistance (R) fluctuations; "Wound" closure rate | Facilitates automated, reproducible wound healing assays by using electrical currents to create precise wounds in monolayers [37]. |
| Cell-Substrate Adhesion & Spreading | Changes in Impedance during initial cell attachment | Provides insights into fundamental cellular behaviors like adhesion and spreading on different substrates or under various treatments [37]. |
Detailed Experimental Protocol: Monitoring Intestinal Organoid–Derived Monolayer Barrier Functions
The following section provides a detailed methodology for applying ECIS to monitor barrier formation in physiologically relevant models, such as patient-derived intestinal organoid monolayers, which better recapitulate the cellular heterogeneity and functions of the parent tissue compared to traditional cell lines [37].
Research Reagent Solutions and Essential Materials
Table 2: Essential Materials and Reagents for ECIS with Organoid-Derived Monolayers
| Category | Item | Function / Specification |
|---|---|---|
| Biological Material | 3D intestinal organoid lines (fetal or adult tissue-derived) | Provides a physiologically relevant cell source for generating 2D monolayers [37]. |
| Core Reagents | Advanced DMEM/F12, GlutaMAX, HEPES, Penicillin-Streptomycin | Forms the base medium (Ad-DF+++) for organoid handling and culture [37]. |
| Human IntestiCult Organoid Growth & Differentiation Media | Supports the expansion and differentiation of intestinal epithelial cells [37]. | |
| Collagen Type I, Rat Tail | Coats the ECIS arrays to provide a suitable surface for cell attachment and monolayer formation [37]. | |
| L-cysteine | Used to stabilize gold electrodes on the ECIS array prior to collagen coating [37]. | |
| TrypLE Express | Enzymatically dissociates 3D organoids into single cells for seeding 2D monolayers [37]. | |
| Y27632 (ROCK inhibitor) | Improves cell viability after single-cell dissociation by inhibiting apoptosis [37]. | |
| Specialized Equipment | ECIS Z-Theta Instrument | The main hardware unit that applies the alternating current and measures impedance [37]. |
| ECIS 16-Well Array Station | Housed in the incubator, it holds the array and connects it to the instrument [37]. | |
| ECIS 8W1E or 8W10E Arrays | The consumable with integrated electrodes. 8W1E is ideal for wound healing; 8W10E (multiple electrodes) averages signals for barrier/proliferation studies [37]. | |
| Software | ECIS Zθ Software | Controls the instrument, designs experiments, and collects/analyzes real-time impedance data [37]. |
Step-by-Step Experimental Workflow
The experimental workflow for an ECIS assay using intestinal organoid-derived monolayers is a multi-stage process, as illustrated in the following diagram:
Diagram 1: ECIS Experimental Workflow
Procedure:
Preparation of the ECIS Station and Arrays:
- Place the ECIS 16-well station in a 37°C incubator at least one day before the experiment to pre-warm [37].
- Array Coating: Activate and prepare the electrode surfaces.
- Add 200 µL of 10 mM L-cysteine solution to each well of a new ECIS array and incubate for 30-45 minutes at room temperature (RT). This step stabilizes the small gold electrodes [37].
- Wash wells twice with 300 µL of sterile Milli-Q water.
- Add 300 µL of Collagen/0.1% acetic acid solution (e.g., 10 µg/cm²) to each well and incubate for 60 minutes at RT.
- Wash wells twice with 300 µL of sterile Milli-Q water. The arrays are now ready for cell seeding [37].
Preparation of Organoid-Derived Single Cells:
- Harvest and dissociate 3D intestinal organoids into a single-cell suspension using TrypLE Express enzyme. It is critical to include a ROCK inhibitor (Y27632) in the suspension medium to enhance cell survival after dissociation [37].
- Centrifuge the cell suspension and resuspend the pellet in an appropriate medium, such as Human IntestiCult Organoid Growth Medium, to the desired cell density for seeding.
Cell Seeding and Impedance Measurement:
- Seed the single-cell suspension onto the pre-coated ECIS arrays. The chosen array type (e.g., 8W1E for wound healing, 8W10E for barrier formation) depends on the experimental goal [37].
- Carefully place the seeded array into the pre-warmed station within the incubator.
- Initiate continuous, automated impedance measurements using the ECIS Zθ software. Data collection typically runs for the duration of the experiment, from initial attachment and spreading through barrier formation and any subsequent experimental interventions.
Experimental Intervention and Data Analysis:
- Once a stable, confluent monolayer with a high impedance reading (indicative of a strong barrier) is established, introduce experimental treatments (e.g., drugs, cytokines, toxins) directly into the wells.
- The software records impedance changes in real-time, allowing for the kinetic assessment of the treatment's effect on the cell layer.
- For migration studies, the ECIS instrument can apply a lethal, high-frequency electrical current to a specific electrode, thereby "wounding" the monolayer. The subsequent impedance recovery, as cells migrate back onto the electrode, is monitored and quantified [37].
Technical Specifications and Data Interpretation
ECIS Configurations and Impedance Parameters
Understanding the hardware configuration and the fundamental electrical parameters measured by ECIS is crucial for experimental design and data interpretation.
Table 3: ECIS Technical Specifications and Measured Parameters
| Aspect | Specifications / Definitions |
|---|---|
| Measurement Principle | Application of a small, alternating current (non-invasive to cells) across electrodes and measurement of the resulting impedance [37]. |
| Frequency Range | Broad frequency spectrum, typically from 62.5 Hz to 64 kHz [37]. |
| Key Electrical Parameters | Impedance (Z): Total opposition to current flow. Resistance (R): Opposition to current from ionic solutions. Correlates with barrier integrity and cell-cell contacts. Capacitance (C): Ability of cell membranes to store charge. Correlates with the number and health of cells on the electrode. Phase Angle (φ): Phase difference between voltage and current, related to the capacitive properties of the cell layer [37]. |
| Array Types | 8W1E Array: One active electrode per well. Higher sensitivity to cell motion, ideal for wound healing and migration studies [37]. 8W10E Array: Ten active electrodes per well. Averages signals, minimizing bias from uneven cell distribution; ideal for proliferation and barrier formation studies [37]. |
Relationship Between Impedance and Biological Phenomena
The following diagram illustrates how the raw electrical measurements from ECIS translate into biologically meaningful information about the cell monolayer.
Diagram 2: From Impedance to Biological Meaning
Application in Nutritional Epidemiology and Chronic Disease Management
Bioelectrical Impedance Analysis (BIA) is a non-invasive, rapid, and widely used method for assessing body composition in both research and clinical settings. By measuring the body's opposition to a low-level, alternating electric current, BIA can provide estimates of body compartments such as fat mass (FM), fat-free mass (FFM), total body water (TBW), and its sub-compartments [4]. The fundamental parameters obtained are resistance (R), which reflects the opposition to the flow of an alternating current through intra- and extracellular electrolytic solutions, and reactance (Xc), which represents the capacitive properties of cell membranes. The phase angle (PhA), derived from the arc-tangent of the ratio of Xc to R, serves as a biomarker for cellular integrity and nutritional status [24] [39] [4].
The application of BIA has expanded significantly over the past two decades, with an annual publication growth rate of 10.1% and nearly 9,500 articles published in the last 20 years [40]. Its use spans numerous fields, with the top research areas being Nutrition and Dietetics (2,145 articles), Urology and Nephrology (883 articles), and Endocrinology and Metabolism (860 articles) [40]. Recent research hotspots have evolved from "water" to "fat," and more recently to "sarcopenia" and "phase angle" [40], underscoring its growing relevance in nutritional epidemiology and the management of chronic diseases where body composition is a critical factor.
BIA devices are categorized based on their technical operation and electrode configuration. The key distinctions are summarized in the table below.
Table 1: Key Technical Specifications of BIA Methodologies
| Feature | Single-Frequency BIA (SF-BIA) | Multi-Frequency BIA (MF-BIA) | Bioelectrical Impedance Spectroscopy (BIS) | Bioelectrical Impedance Vector Analysis (BIVA) |
|---|---|---|---|---|
| Frequencies | Single frequency (typically 50 kHz) [4] | Multiple frequencies (e.g., 5, 50, 250 kHz) [5] [4] | A spectrum of frequencies (e.g., 1–1000 kHz) [41] [4] | Typically uses 50 kHz; analysis method, not a device [40] [4] |
| Primary Applications | Estimating FM, FFM, TBW [4] | Differentiating ICW and ECW; segmental analysis [41] [4] | Accurate assessment of ICW and ECW [4] | Qualitative/semi-quantitative analysis of hydration and cell mass [24] [4] |
| Common Electrode Configurations | Bipolar (hand-to-hand, foot-to-foot) [4] | Tetrapolar or Octopolar [5] [4] | Tetrapolar [4] | Uses raw data from tetrapolar or octopolar devices [24] |
| Key Advantages | Affordable, easy to use, portable [4] | Improved accuracy for fluid distribution and lean mass [4] | Considered gold-standard for fluid compartment differentiation [4] | No reliance on predictive equations; insights into cellular health [24] [40] |
| Key Limitations | Less accurate in altered hydration; lacks raw data access in consumer models [4] | Costlier; relies on proprietary algorithms [5] [4] | Requires specialized expertise and equipment [4] | Requires specialized expertise for interpretation [4] |
BIA is a predictive method, meaning its estimates of body composition are derived from regression equations that correlate impedance measurements with reference methods like Dual-Energy X-ray Absorptiometry (DXA) or isotope dilution [23] [4]. The validity of these estimates is therefore highly dependent on the population-specificity of the underlying equations. A recent large-scale (n=1000) real-world validation of an octopolar MFBIA device (InBody 770) against DXA showed modest population-level agreement for total body FM (%BF bias: men -4.2%, women -2.8%) and FFM (bias: men +3.4 kg, women +2.0 kg) [5]. Another study (n=945) found that a Tanita BIA device overestimated FFM by 3.1 kg (+7.2%) compared to DXA [23]. These findings highlight the importance of understanding the inherent biases of specific BIA devices and the potential need for calibration equations for precise epidemiological or clinical work.
Application in Chronic Disease Management
BIA provides critical insights for the management of various chronic diseases by monitoring nutritional status, fluid shifts, and cellular health.
Chronic Kidney Disease (CKD)
BIA is extensively used in nephrology for the nutritional management of CKD patients across all stages, including pre-dialysis, hemodialysis (MHD), peritoneal dialysis, and post-transplantation [41]. In MHD patients, BIA is valuable for assessing dry weight and monitoring hydration status. Furthermore, the Phase Angle (PhA) has emerged as a significant prognostic marker. A 2025 cross-sectional study of 369 MHD patients found a strong independent association between lower PhA values and a higher risk of depressive symptoms. After full adjustment for comorbidities and nutritional markers, patients in the lowest PhA quartile had an odds ratio of 51.760 for depression compared to those in the highest quartile [39]. This suggests PhA could serve as an objective biomarker for identifying MHD patients at high risk for mental health complications.
Sarcopenia and Frailty
Sarcopenia, the age-related loss of muscle mass and function, has become a central research hotspot in the BIA field [40]. BIA is recommended by the Global Leadership Initiative on Malnutrition (GLIM) for evaluating muscle mass loss [4]. It is particularly useful in geriatrics and primary care for identifying "sarcopenic obesity," a high-risk phenotype often missed by Body Mass Index (BMI) screening alone [42]. The Skeletal Muscle Index (SMI), derived from BIA equations, and raw parameters like PhA are used to assess muscle quality and quantity. In older hospitalized patients, measures like Calf Circumference (CC), which can be informed by BIA, have been shown to be significant predictors of in-hospital complications and mortality, outperforming other frailty assessments [42].
Obesity and Metabolic Phenotyping
While BMI is commonly used, it fails to distinguish between fat and lean mass. BIA allows for direct measurement of body fat percentage (BF%) and visceral adipose tissue (VAT). This is crucial for identifying "metabolically obese normal weight" (MONW) or "skinny fat" individuals, who have a normal BMI but high body fat, a phenotype strongly associated with metabolic syndrome and cardiovascular disease [42]. Although MFBIA shows high correlation with DXA for trunk FM (r=0.92-0.93), its agreement for VAT is more modest (r=0.74), indicating a need for cautious interpretation [5].
Table 2: BIA Applications in Key Chronic Disease Areas
| Disease Area | Key BIA Parameters | Clinical and Research Utility |
|---|---|---|
| Chronic Kidney Disease (CKD) | PhA, ECW/TBW ratio, BIVA [41] [39] | Nutritional management, dry weight assessment, prognosis, and mental health risk stratification [41] [39]. |
| Sarcopenia & Frailty | SMI, FFMI, PhA, CC [40] [42] [4] | Early diagnosis of muscle loss, screening for sarcopenic obesity, predicting morbidity and mortality in the elderly [42] [4]. |
| Obesity & Metabolic Health | BF%, VAT, FFM [5] [42] | Identifying high-risk phenotypes (e.g., MONW), moving beyond BMI for better risk assessment [42]. |
| Cardiovascular Disease | BIVA, WHR, BF% [42] | Assessing fluid overload and body composition patterns associated with cardiovascular risk [42]. |
Detailed Experimental Protocols
Protocol 1: Body Composition & Phase Angle Assessment in Hemodialysis Patients
This protocol is adapted from a 2025 cross-sectional study investigating the link between PhA and depressive symptoms in MHD patients [39].
Aim: To assess the body composition and nutritional status of MHD patients and correlate these parameters with clinical outcomes such as depression. Materials: A multi-frequency, tetrapolar BIA device; standard electrodes; calibrated weighing scale; stadiometer; Patient Health Questionnaire (PHQ-9). Patient Preparation:
- Measurements must be performed before a dialysis session.
- Patients should be in a supine position for at least 5-10 minutes prior to measurement to allow for fluid redistribution.
- Ensure skin is clean and dry at electrode placement sites (hand, wrist, ankle, foot).
Procedure:
- Pre-Measurement: Confirm patient eligibility (e.g., clinical stability, no hospitalization in last 3 months). Obtain informed consent.
- Data Collection:
- Record demographic and clinical data (age, gender, dialysis vintage, comorbidities).
- Collect blood samples for serum albumin, hemoglobin, and C-reactive protein.
- Administer the PHQ-9 questionnaire to screen for depressive symptoms.
- Anthropometry: Measure standing height and post-dialysis weight for accurate input into the BIA device.
- BIA Measurement:
- Place the patient in a supine position, with limbs slightly abducted from the body.
- Attach electrodes to the dorsal surfaces of the right hand and wrist, and the right foot and ankle, following the device-specific manual.
- Initiate the BIA measurement. Ensure the patient remains still and does not talk during the procedure.
- Record the raw parameters: Resistance (R), Reactance (Xc), and the calculated Phase Angle (PhA).
- Export the derived body composition data: FFM, FM, SMI, TBW, and ECW/ICW.
- Data Analysis:
- Calculate the Extracellular Water to Total Body Water ratio (ECW/TBW).
- Analyze the association between PhA (categorized into quartiles) and PHQ-9 scores using statistical models (e.g., logistic regression), adjusting for age, sex, dialysis vintage, and serum albumin.
Protocol 2: Validating BIA against DXA in Epidemiological Cohorts
This protocol outlines the steps for validating a BIA device against DXA in a population sample, as demonstrated in a study with Brazilian adults [23].
Aim: To evaluate the agreement between BIA and DXA for measuring FFM and FM and to develop a population-specific calibration equation if necessary. Materials: BIA device (e.g., Tanita BC-618); DXA scanner (e.g., GE iDXA); calibrated scales and stadiometer. Participant Preparation:
- Participants should fast for a minimum of 4 hours and avoid vigorous physical activity for 24 hours prior to testing.
- Maintain adequate hydration but avoid excessive fluid intake immediately before the test.
- Void the bladder within 30 minutes prior to measurement.
Procedure:
- Anthropometry: Precisely measure body weight (to the nearest 0.1 kg) and height (to the nearest 0.1 cm) in light clothing without shoes.
- BIA Measurement: Conduct the BIA measurement first, following the manufacturer's instructions. For standing devices, ensure the participant's feet are clean and positioned correctly on the electrodes. Record FFM and FM estimates, and if possible, the raw impedance data (Resistance, Reactance).
- DXA Measurement: Immediately following the BIA, perform the whole-body DXA scan according to the standard operating procedures. The participant should remain in the same clothing.
- Data Collection: Collect data from a sufficiently large and heterogeneous sample (e.g., n>500, including both sexes and a range of ages and BMIs).
- Statistical Analysis:
- Assess precision using Pearson correlation (r) between BIA and DXA measures.
- Evaluate accuracy using Lin's Concordance Correlation Coefficient (CCC).
- Use paired t-tests to determine mean differences (bias) between methods.
- Perform Bland-Altman analysis to visualize the limits of agreement.
- If a significant bias is found, use linear regression to develop a calibration equation to correct BIA estimates to align with DXA values [23].
Workflow and Data Interpretation
The following diagram illustrates the logical workflow for applying BIA in nutritional epidemiology and chronic disease management, from measurement to clinical action.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for BIA Studies
| Item | Specification / Examples | Primary Function in BIA Research |
|---|---|---|
| BIA Device | Multi-frequency, Tetrapolar/Octopolar (e.g., InBody 770, RJL Quantum) [5] [4] | The core instrument for measuring raw bioelectrical parameters (R, Xc) and estimating body composition. MFBIA is preferred for clinical research. |
| Electrodes | Single-use, pre-gelled ECG electrodes [4] | To ensure consistent electrical contact and signal transmission between the device and the subject's skin. |
| Reference Method | DXA Scanner (e.g., GE iDXA, Hologic) [5] [23] | The criterion method for validating BIA-derived estimates of fat and fat-free mass. |
| Calibration Equipment | Certified weights, Stadiometer [5] | To accurately calibrate the scale within the BIA device and measure participant height, which is critical for all predictive equations. |
| Indirect Calorimeter | Metabolic cart (e.g., Vyaire CareFusion) [43] | The gold-standard method for measuring Resting Metabolic Rate (RMR), used to develop and validate BIA-based predictive equations for energy expenditure. |
| Population-Specific Equations | e.g., Campa et al. classified 106 predictive equations [4] | Software or algorithms containing validated regression equations specific to the population under study (e.g., athletes, elderly, CKD patients) to ensure accurate results. |
| Standardized Protocols | SOPs for patient preparation, positioning, and data collection [4] | Documentation to ensure measurement consistency, minimize technical error, and guarantee data reliability across operators and time. |
High-Throughput Drug Screening and Toxicity Assessment Using Impedance Biosensors
Bioelectrical Impedance Analysis (BIA) represents a sophisticated, label-free methodology for monitoring cellular responses in real-time by measuring the opposition to a small electrical current flowing through biological systems. This technique has been successfully adapted from its conventional use in body composition research, where it determines body cell mass (BCM), extracellular mass (ECM), and total body water (TBW) by analyzing impedance components [44], to advanced drug discovery applications. In the context of high-throughput drug screening, impedance biosensors function by quantifying subtle changes in cellular properties—including adhesion, morphology, and viability—when exposed to chemical compounds or potential therapeutics [45]. The technology's capacity for non-invasive, instantaneous detection of cell responses to pharmacological agents has established it as an invaluable tool for modern drug development pipelines, enabling more physiologically relevant screening compared to traditional endpoint assays [45].
The fundamental principle underpinning impedance biosensors involves applying a sinusoidal alternating current (AC) across electrode arrays and precisely measuring the resulting impedance, which comprises both resistance (R) and reactance (Xc) [45] [44]. Resistance reflects the opposition to current flow through electrolytic solutions in tissue fluids, while reactance represents the capacitive properties of cell membranes acting as electrical capacitors [1]. In controlled in vitro systems, alterations in these parameters directly correlate with critical cellular events: decreased impedance typically indicates cell death or detachment, whereas increased impedance often signifies cell proliferation, spreading, or morphological changes indicative of specific drug responses [45]. This sensitive detection mechanism provides a comprehensive functional assessment of cell status without requiring labels, dyes, or complex sample processing.
Technological Foundations of Impedance Biosensors
Basic Principles and Measurement Fundamentals
Impedance biosensors operate on the core principle of measuring a biological system's opposition to an applied alternating current (AC). The measured impedance (Z) is a complex value composed of two primary components: resistance (R), which represents the opposition to current flow through conductive paths, and reactance (Xc), which reflects capacitive effects caused by cell membranes and interface phenomena [1] [44]. When applied to cell-based assays, the technology detects changes in cell number, adhesion, morphology, and viability by monitoring how these parameters affect current flow through the system. As cells adhere and spread on electrode surfaces, they impede current flow, increasing the measured impedance. Conversely, cell detachment or death reduces impedance values [45]. This non-invasive approach enables continuous, real-time monitoring of cellular responses to pharmacological compounds, providing rich kinetic information unavailable through traditional endpoint assays.
The electrical characteristics of biological materials vary significantly based on their composition. Tissues with high water and electrolyte content, such as muscle and organs, exhibit high conductivity, while lipid-rich tissues like adipose demonstrate poor conductivity [46]. Similarly, in cell-based assays, the current flows more easily around and between cells that are poorly adhered, while well-adhered cells with extensive electrode coverage create greater impedance. The phase angle (φ), derived from the arctangent of the ratio between reactance and resistance (Xc/R), serves as a particularly sensitive indicator of cell health and adhesion status, with higher values generally correlating with improved membrane integrity and cellular function [44].
Advanced Sensor Architectures
Recent advancements in impedance biosensor technology have focused on enhancing sensitivity, throughput, and biological relevance through innovative sensor designs. Nanogroove-enhanced electrical impedance biosensors represent a significant breakthrough, incorporating nanopatterned substrates that mimic physiological conditions more accurately than traditional flat surfaces [47]. These nanogroove patterns influence cell alignment, intracellular organization, and importantly, gene expression profiles. RNA sequencing of MCF-7 cells cultured on nanopatterned substrates revealed significant differential gene expression compared to flat surfaces, suggesting that traditional cultures may induce artificial gene regulation that potentially biases drug screening results [47].
The development of the NanoIEA platform, which integrates nanopatterned membranes within 96-well plates with electrode arrays, enables real-time impedance spectroscopy for dynamic assessment of cellular behavior under chemotherapeutic drug exposure [47]. This high-throughput configuration facilitates comprehensive investigations into cellular growth and drug interactions while using physiologically relevant culture conditions. The fabrication of these platforms employs self-assembled monolayers (SAMs) and optimized imprinting parameters to create uniform large-area nanopatterns, overcoming previous challenges such as the "rabbit ears" effect and inconsistent pattern fidelity [47].
Microfluidic impedance biosensors constitute another advanced architecture, particularly valuable for single-cell analysis [48]. These systems combine miniature fluid handling channels with impedance measurement electrodes to trap, position, and analyze individual cells. The technological development of various single-cell trapping methods—including hydrodynamic traps, mechanical structures, and dielectrophoretic forces—has determined the efficiency and performance of these sensors [48]. Such systems provide unprecedented resolution for detecting heterogeneous cell responses to compounds, enabling the identification of rare cell subpopulations that might be missed in bulk measurements.
Application Notes: Implementation in Drug Screening
Platform Selection and Configuration
Implementing impedance biosensors for high-throughput drug screening requires careful consideration of platform configuration based on specific research objectives. The following table summarizes the primary impedance biosensor platforms and their appropriate applications:
Table 1: Impedance Biosensor Platforms for Drug Screening Applications
| Platform Type | Throughput | Key Features | Optimal Applications | Limitations |
|---|---|---|---|---|
| NanoIEA (Nanogroove-enhanced) | High (96-well) | Nanostructured substrates that mimic physiological conditions; real-time impedance spectroscopy | Cancer drug screening; assessment of compounds where microenvironment influences efficacy | Specialized fabrication required; potentially higher cost per well |
| Microfluidic Single-Cell | Medium to High | Single-cell trapping and analysis; reduced reagent consumption | Toxicity assessment; heterogeneous cell population studies; rare cell detection | Lower cell numbers per measurement; complex fluidic handling |
| Standard Multi-well Electrode Arrays | High (96/384-well) | Conventional electrode layouts; established protocols | Primary screening campaigns; compound library profiling | Limited physiological mimicry of cell environment |
For comprehensive screening campaigns, the nanogroove-enhanced 96-well platform provides an optimal balance between throughput and biological relevance. The nanopatterned surfaces significantly influence gene expression patterns in cultured cells, potentially yielding more clinically predictive results for anticancer drug screening [47]. This platform successfully combines advanced nanofabrication with precise real-time monitoring, addressing technical limitations in bioelectronic sensing while providing deeper insights into dynamic cellular responses [47].
Experimental Workflow and Protocol Standardization
The general workflow for impedance-based drug screening involves platform preparation, baseline measurement, compound application, continuous monitoring, and data analysis. Standardization of protocols is essential for generating reproducible, reliable data across experiments and research groups. The following diagram illustrates the core experimental workflow:
Critical standardization parameters include maintaining consistent cell culture conditions, precise seeding densities, controlled environmental factors (temperature, CO₂), and standardized data normalization procedures. For nanogroove-enhanced platforms, additional attention must be paid to the orientation and alignment of cells on patterned surfaces to ensure reproducible responses [47]. Protocol standardization significantly enhances data quality and enables meaningful cross-study comparisons.
Data Interpretation and Analysis Approaches
Impedance data from drug screening applications requires specialized analytical approaches to extract biologically meaningful information. The primary measured parameters include impedance magnitude, resistance (R), reactance (Xc), and the derived phase angle. The following table outlines key impedance parameters and their biological correlates in drug screening contexts:
Table 2: Impedance Parameters and Their Biological Significance in Drug Screening
| Parameter | Electrical Definition | Biological Correlation | Interpretation in Drug Screening | ||
|---|---|---|---|---|---|
| Impedance Magnitude ( | Z | ) | Overall opposition to current flow | Cell coverage, adhesion, and barrier integrity | Decreased: cell death/detachmentIncreased: proliferation/spreading |
| Resistance (R) | Opposition to current flow through ionic solutions | Extracellular environment and intracellular fluid conductivity | Changes in cell membrane permeabilityAlterations in cell volume | ||
| Reactance (Xc) | Capacitive opposition due to cell membranes | Cell membrane integrity and capacity | Decreased: membrane damage or compromised integrity | ||
| Phase Angle (φ) | arctan(Xc/R) | Cell membrane function and cellular health | Decreased: overall loss of cell health/viabilityIncreased: improved functional status |
Normalization of impedance data is typically performed relative to baseline measurements (time zero) or vehicle controls to account for well-to-well variability. For time-series data, parameters such as area under the curve (AUC), half-maximal effective concentration (EC₅₀), or half-maximal inhibitory concentration (IC₅₀) can be derived to quantify compound effects. For nanogroove platforms, it is essential to note that cells may exhibit different baseline impedance and response kinetics compared to conventional surfaces due to altered gene expression and adhesion patterns [47].
Detailed Experimental Protocols
Protocol 1: High-Throughput Compound Screening Using NanoIEA Platform
This protocol describes the procedure for screening compound libraries using the nanogroove-enhanced impedance biosensor platform in a 96-well format, enabling real-time, label-free assessment of compound efficacy and toxicity.
Materials and Reagents
- NanoIEA 96-well plates (nanogroove-patterned electrode arrays)
- Cell culture medium appropriate for cell line of interest
- Trypsin-EDTA solution for cell dissociation
- Dimethyl sulfoxide (DMSO)
- Compound library dissolved in DMSO at recommended stock concentrations
- Phosphate-buffered saline (PBS)
- Impedance measurement system compatible with 96-well format
Procedure
Platform Preparation
- Sterilize NanoIEA plates by UV exposure for 30 minutes per side under sterile conditions.
- Coat plates with appropriate extracellular matrix proteins if required for specific cell types (e.g., collagen for epithelial cells, fibronectin for fibroblasts).
- Wash plates twice with sterile PBS before cell seeding.
Cell Seeding and Culture
- Harvest cells during logarithmic growth phase using standard trypsinization procedures.
- Prepare cell suspension at optimal density (typically 5,000-50,000 cells/well depending on cell size and proliferation rate).
- Seed cells in NanoIEA plates, ensuring even distribution across wells.
- Allow cells to adhere and spread for 4-24 hours (duration dependent on cell type) under standard culture conditions (37°C, 5% CO₂).
Baseline Impedance Measurement
- Confirm cell adhesion and spreading by microscopic examination.
- Measure baseline impedance across all wells using the impedance measurement system.
- Set measurement parameters: frequency sweep (typically 100 Hz - 1 MHz), AC voltage amplitude (typically 10-50 mV).
- Record baseline values for normalization in subsequent analyses.
Compound Application
- Prepare compound dilutions in culture medium, ensuring final DMSO concentration does not exceed 0.1% (v/v).
- Include vehicle controls (medium with 0.1% DMSO) and positive controls (e.g., cytotoxic compound for toxicity assessment).
- Carefully replace medium in assay plates with compound-containing medium.
- Return plates to impedance measurement system within incubation chamber.
Continuous Impedance Monitoring
- Program impedance measurement system for periodic scanning (e.g., every 15 minutes for first 6 hours, then hourly for duration of experiment).
- Maintain constant environmental conditions (37°C, 5% CO₂) throughout monitoring period.
- Continue monitoring for predetermined duration (typically 24-72 hours depending on assay objectives).
Data Collection and Analysis
- Export impedance data (resistance, reactance, phase angle) for all time points.
- Normalize data to baseline measurements or vehicle controls.
- Generate time-response curves for each compound concentration.
- Calculate derived parameters (IC₅₀, AUC) using appropriate software.
Troubleshooting Notes
- High well-to-well variability: Ensure uniform cell seeding and consistent medium evaporation control.
- Erratic impedance readings: Verify electrode integrity and check for air bubbles under electrode surfaces.
- Inconsistent compound effects: Confirm compound stability in assay conditions and verify dosing accuracy.
Protocol 2: Single-Cell Toxicity Assessment Using Microfluidic Impedance Biosensors
This protocol details the procedure for single-cell resolution toxicity assessment using microfluidic impedance biosensors, enabling detection of heterogeneous responses within cell populations.
Materials and Reagents
- Microfluidic impedance chip with single-cell trapping capability
- Cell culture medium appropriate for cell line of interest
- Trypsin-EDTA solution for cell dissociation
- Test compounds dissolved at appropriate stock concentrations
- Syringe pumps or pressure-driven flow control system
- Impedance analyzer with capability for high-frequency measurements
Procedure
Chip Preparation and Priming
- Sterilize microfluidic chip by flushing with 70% ethanol followed by sterile water.
- Prime chip with cell culture medium, ensuring all air bubbles are eliminated from microchannels.
- Connect chip to fluidic control system and impedance analyzer.
Cell Loading and Trapping
- Prepare single-cell suspension at appropriate density (typically 1-5 × 10⁶ cells/mL).
- Introduce cell suspension into microfluidic chip using controlled flow rates.
- Monitor trapping efficiency microscopically, adjusting flow conditions as needed.
- Once traps are occupied, switch to maintenance flow with fresh culture medium.
Baseline Single-Cell Impedance Measurement
- Measure baseline impedance for each trapped cell across multiple frequencies.
- Record individual cell characteristics (size, shape, membrane properties) based on impedance spectroscopy.
- Establish baseline parameters for subsequent normalization.
Compound Exposure
- Prepare compound solutions at desired concentrations in culture medium.
- Switch flow from maintenance medium to compound-containing medium.
- Maintain continuous flow throughout exposure period to ensure consistent compound delivery.
Real-Time Impedance Monitoring
- Continuously monitor impedance of individual cells throughout exposure period.
- Program frequent measurement intervals (e.g., every 1-5 minutes) to capture rapid response kinetics.
- Maintain constant environmental conditions (37°C where applicable).
Data Analysis and Heterogeneity Assessment
- Analyze impedance trajectories for individual cells.
- Classify response patterns (e.g., rapid cytotoxicity, adaptive responses, resistance).
- Quantify population heterogeneity in compound responses.
- Correlate impedance changes with specific cellular events (membrane disruption, apoptosis).
Troubleshooting Notes
- Poor trapping efficiency: Optimize cell density and flow rates; verify trap dimensions match cell size.
- Cell displacement during compound application: Reduce flow rates during medium switching.
- Signal interference from debris: Pre-filter cell suspension to remove aggregates and debris.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of impedance-based drug screening requires specific reagents and materials optimized for these specialized platforms. The following table details essential components and their functions:
Table 3: Essential Research Reagents and Materials for Impedance-Based Screening
| Category | Specific Items | Function | Selection Criteria |
|---|---|---|---|
| Biosensor Platforms | NanoIEA 96-well plates [47] | Provide nanostructured surface for physiologically relevant cell culture and impedance measurement | Pattern fidelity, electrode stability, compatibility with impedance systems |
| Microfluidic single-cell chips [48] | Enable trapping and analysis of individual cells | Trap design, optical accessibility, electrode configuration | |
| Cell Culture Reagents | ECM coating proteins (collagen, fibronectin) [45] | Enhance cell adhesion to electrode surfaces | Compatibility with cell type, consistency in coating quality |
| Serum-free assay medium | Maintain cell viability while reducing background signal | Formulation support for specific cell types, low electrical conductivity | |
| Impedance Measurement | Electrolyte solutions | Provide ionic environment for current conduction | Stable conductivity, physiological compatibility |
| Reference electrodes | Ensure consistent potential measurements | Stability, low polarization, compatibility with system | |
| Compound Handling | DMSO (high purity) | Universal solvent for compound libraries | Low electrical conductivity, minimal cellular toxicity at working concentrations |
| Compound storage plates | Maintain compound integrity during screening | Low compound binding, compatibility with liquid handling systems |
Selection of appropriate extracellular matrix coatings deserves particular attention, as cell-electrode coupling significantly impacts detection sensitivity. The use of specific peptide sequences (e.g., KREDVY) that promote integrin-mediated cell adhesion can enhance signal quality by minimizing the distance between cells and electrode surfaces [45]. For nanogroove platforms, additional consideration should be given to how surface patterning influences protein adsorption and subsequent cell adhesion characteristics.
Integration with Body Composition Research Principles
The application of impedance biosensors in drug screening shares fundamental principles with bioelectrical impedance analysis (BIA) used in body composition research. Both fields rely on measuring the passive electrical properties of biological systems to derive meaningful physiological information. In body composition analysis, BIA distinguishes between fat mass and fat-free mass based on their different electrical conductivities—fat-free mass, with its higher water and electrolyte content, conducts electrical current more effectively than fat mass [1] [46]. Similarly, in cell-based impedance biosensors, the technology discriminates between different cellular states based on changes in membrane integrity, cell size, and adhesion properties that alter current flow.
The BIA parameters used in body composition assessment—resistance (R), reactance (Xc), phase angle, and impedance vector analysis (BIVA)—have direct analogs in cell-based drug screening [44]. In clinical BIA, the phase angle has emerged as a robust indicator of cellular health and nutritional status, with higher values generally reflecting better cell membrane integrity and function. Similarly, in cell-based assays, the phase angle serves as a sensitive indicator of compound-induced cytotoxicity or functional enhancement. This parameter correlation enables researchers to apply interpretative frameworks from clinical BIA to in vitro drug screening contexts.
The concept of bioelectrical impedance vector analysis (BIVA), used in body composition research to assess fluid status and body cell mass [44], can be adapted for quality control in cell-based screening. By plotting resistance and reactance values in a coordinate system and comparing them to reference ranges for specific cell types under standardized conditions, researchers can identify potential artifacts or technical issues in assay performance. This approach provides a valuable quality control mechanism, ensuring that cellular responses measured during drug screening reflect genuine biological effects rather than technical variations.
Impedance biosensors have established themselves as powerful tools in high-throughput drug screening and toxicity assessment, offering unique advantages including label-free detection, real-time kinetic information, and non-invasive monitoring of cellular responses. The integration of advanced features such as nanogroove-enhanced substrates that better mimic physiological environments and microfluidic architectures enabling single-cell resolution represents significant technological progress in the field. These developments align with the growing recognition that more physiologically relevant assay systems yield more clinically predictive results in drug discovery.
The fundamental connections between impedance-based drug screening and bioelectrical impedance analysis for body composition create opportunities for cross-disciplinary methodological exchange. Interpretative frameworks developed in clinical BIA, particularly regarding phase angle significance and vector analysis approaches, can enhance data interpretation in cell-based screening contexts. Similarly, the sophisticated single-cell analysis capabilities emerging in microfluidic impedance systems may inform new approaches for cellular-level assessment in clinical BIA applications.
Future developments in impedance-based screening will likely focus on increasing physiological complexity through co-culture systems, organ-on-a-chip integrations, and more sophisticated extracellular matrix environments. Combined with advances in data analytics and machine learning for pattern recognition in impedance data, these technological improvements will further establish impedance biosensors as indispensable tools in the drug developer's arsenal, bridging the gap between conventional in vitro screening and clinical efficacy.
Addressing Technical Limitations and Optimizing Measurement Protocols
Bioelectrical Impedance Analysis (BIA) is a widely used method for assessing body composition in research and clinical settings due to its non-invasive nature, portability, and relatively low cost. The technique operates on the principle that the conduction of a low-level electrical current through body tissues differs between fat-free mass (which contains virtually all body water and electrolytes) and fat mass (which is relatively anhydrous and non-conductive). However, the very principle that makes BIA practical also renders it susceptible to several confounding factors that can significantly impact measurement accuracy. This document details the key confounding variables—hydration status, meal consumption, and physical activity—and provides standardized protocols to control for these factors in research settings, particularly those involving drug development and clinical trials.
Hydration Status
Hydration status is a primary confounding factor for BIA because the technology fundamentally measures the body's water content to estimate fat-free mass and fat mass. Fluid imbalances directly alter the electrical properties of tissues.
Table 1: Impact of Hydration Status on BIA Parameters and Pulmonary Function
| Hydration/Fluid Metric | Impact on BIA/Pulmonary Function | Population Studied | Key Findings |
|---|---|---|---|
| Impedance Ratio (IR) ≥ 0.84 | Associated with decreased FEV1 and FVC | COPD Patients (n=180) [49] | Lower FEV1, FVC, FEV1/FVC, and DLCO compared to IR < 0.84 group. IR is an independent predictor of pulmonary function. |
| Phase Angle (PhA) | Positive association with FVC | COPD Patients (n=180) [49] | Higher PhA values were linked to better pulmonary function outcomes after adjusting for confounders. |
| Extracellular Water (ECW) | Negatively associated with FEV1 | COPD Patients (n=180) [49] | Increased ECW was correlated with a decrease in forced expiratory volume. |
| Hydration Status (H²/R) | Associated with clinical symptoms | Advanced Cancer (n=125) [50] | Lower hydration (H²/R) linked to increased dehydration assessment scale scores (dry mouth, axilla, sunken eyes) and breathlessness. Higher hydration linked to edema. |
Meal Consumption
The consumption of food and beverages prior to BIA measurement can alter body water distribution and electrolyte concentration, potentially leading to misinterpretation of body composition data.
Table 2: Effects of Meal Consumption on BIA Measurements
| Study Intervention | Caloric & Macronutrient Intake | Population | Impact on Body Fat Percentage (BFP) |
|---|---|---|---|
| Routine Food/Drink Consumption [51] | 199 ± 141 kcal (59% Carb, 14% Prot, 28% Fat) | Healthy Individuals (n=43, age 30.3±13.6 y) | No significant difference in BFP before (22.43% ± 8.9%) and after (22.63% ± 9.0%) consumption (p=0.200). |
| Systematic Review of Eating Frequency [52] | N/A - Focus on meal frequency | Meta-analysis of 16 trials | Very low certainty evidence of no difference in weight change between high- and low-frequency eating patterns (MD: -0.62 kg, CI95: -2.76 to 1.52 kg, p=0.57). |
Physical Activity
Exercise induces fluid shifts through sweating and changes in blood flow, while also altering muscle energy substrates and electrolyte balance, all of which can affect impedance measurements.
Table 3: Impact of Physical Activity on Body Composition and BIA
| Exercise Intervention | Study Population | Body Composition Changes (Post-Intervention) | Additional Metabolic Findings |
|---|---|---|---|
| 16-Week Exercise Program (EP) [53] | Obese adolescent boys (n=16) | Body Fat Percentage: Decreased from 37.61% to 29.16%. C-peptide levels also decreased. | Decreased C-peptide (4.58 ng/mL vs. 2.96 ng/mL, p<0.001) and resistin (14.05 ng/mL vs. 11.06 ng/mL, p<0.001). Increased IGF-1 and GH. |
| 8-Week HIIT (WB-HIIT vs JR-HIIT) [54] | Obese young adults (n=36) | WB-HIIT: Greater Muscle Mass increase (1.5 ± 0.7 kg, p<0.01).JR-HIIT: Greater Fat Mass reduction (-2.3 ± 1.2 kg, p<0.01). | WB-HIIT produced higher excess post-exercise oxygen consumption and lipid/carbohydrate metabolism than JR-HIIT. |
| 14-16 Week Resistance Training [55] | Inactive Men (n=27) | Fat Reduction Group: Significant reduction in body fat percentage.Mass Gain Group: Effective for muscle mass gain and strength development. | Customized training protocols confirmed as beneficial for achieving specific body composition goals. |
Standardized Experimental Protocols
Pre-BIA Testing Control Protocol
This protocol establishes standardized conditions for participants undergoing BIA measurements to minimize the confounding effects of hydration, meals, and physical activity.
Duration: 24-Hour Pre-Test Control Period
- Hydration: Maintain normal hydration. Avoid deliberate over-drinking or dehydration. No alcohol or caffeine for 24 hours prior to testing due to their diuretic effects [49] [50].
- Meal Consumption: Fasting for 4-8 hours prior to the BIA test is recommended by most guidelines. Recent evidence suggests that a low-calorie meal (<200 kcal) may not significantly alter results, but standardization is key [51].
- Physical Activity: Avoid moderate to vigorous physical activity for 24 hours prior to testing. No strenuous exercise for 48 hours before the test [54] [5].
Duration: Immediate Pre-Test Procedures (At the Lab)
- Resting Period: Participants should rest in a supine position for 10-15 minutes before the test to allow for fluid stabilization [49].
- Clothing and Accessories: Participants should wear light clothing and remove all jewelry and metal objects. Feet should be bare for foot-to-foot BIA systems [54] [5].
- Environmental Conditions: Testing should be conducted in a temperature-controlled room to prevent sweating or shivering [49].
Protocol for Validating BIA against DXA
This protocol outlines a method for validating BIA device measurements against Dual-Energy X-ray Absorptiometry (DXA) as a criterion reference in a research cohort.
Step-by-Step Workflow:
- Participant Preparation: Follow the 24-hour and immediate pre-test control procedures outlined in section 3.1.
- BIA Measurement: Perform the BIA measurement first, following the manufacturer's guidelines for electrode placement (if applicable) and participant positioning.
- DXA Measurement: Immediately following the BIA measurement, perform the DXA scan according to the standard operating procedures of the facility.
- Data Collection: Record the following metrics from both devices for comparison: Fat Mass (FM), Percent Body Fat (%BF), Fat-Free Mass (FFM), and if available, Visceral Adipose Tissue (VAT) [23] [5].
- Statistical Analysis:
- Calculate Pearson correlation coefficients (r) for precision.
- Use Lin's concordance correlation coefficient (CCC) for accuracy.
- Perform a paired t-test to assess mean differences (bias) between methods.
- Use the Bland-Altman method to evaluate the limits of agreement.
Protocol for Assessing Hydration Status via MFBIA
This protocol utilizes Multi-Frequency BIA (MFBIA) to evaluate hydration status and fluid distribution, which is critical for interpreting body composition data, especially in clinical populations.
Step-by-Step Workflow:
- Equipment Calibration: Ensure the MFBIA device is calibrated according to the manufacturer's specifications.
- Participant Positioning: Position the participant supine on a non-conductive surface, arms abducted ~30° from the trunk, legs abducted ~45°. Maintain this position for 10 minutes prior to measurement [49].
- Electrode Placement: Precisely place electrodes on the hand, wrist, foot, and ankle as per the device's manual (e.g., right-hand and right-foot for a standardized tetra-polar arrangement) [49] [5].
- Measurement: Initiate the MFBIA scan. The device will typically measure resistance (R) and reactance (Xc) across multiple frequencies (e.g., 5kHz, 50kHz, 200kHz).
- Key Hydration Metrics Calculation/Acquisition:
- Impedance Ratio (IR): Calculate as IR = Impedance at 200 kHz / Impedance at 5 kHz. An IR ≥ 0.84 indicates fluid imbalance [49].
- Phase Angle (PhA): Calculated by the device as PhA = arctan(Xc/R) * (180/π). Lower values indicate cell death or malnutrition, while higher values indicate robust cellular health [49].
- Total Body Water (TBW), Extracellular Water (ECW), Intracellular Water (ICW): These are estimated by the device's proprietary equations using the multi-frequency data [49] [50].
- Edema Index: Calculate as ECW (liters) / TBW (liters). A value ≥ 0.48 suggests edema [49].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Equipment for BIA Research
| Item | Function/Application in BIA Research | Example Models / Types |
|---|---|---|
| Multi-Frequency BIA (MFBIA) Device | Gold-standard for research; allows segmental analysis and differentiation of ECW/ICW. Provides raw data (R, Xc, PhA). | InBody 770, BodyStat QuadScan 4000 [49] [5] |
| Single-Frequency BIA (SFBIA) Device | Suitable for population-level screening where high precision in fluid compartments is not required. | Tanita BC-418, Quantum IV [23] [5] |
| Dual-Energy X-Ray Absorptiometry (DXA) | Criterion method for validating BIA measurements of fat mass, lean mass, and bone density. | GE Lunar iDXA, Hologic Horizon A [23] [5] |
| Medical-Grade Electrodes | Ensure consistent electrical contact and minimize impedance at the skin-electrode interface. | Pre-gelled, self-adhesive Ag/AgCl electrodes |
| Calibration Verification Kit | Periodic verification of BIA device accuracy using electrical circuits with known impedance values. | Manufacturer-provided calibration phantoms |
| Stadiometer | Accurate measurement of height (cm), a critical input for BIA equations. | Seca 213 [5] |
| Bioelectrical Impedance Vector Analysis (BIVA) Software | A method to interpret BIA data without reliance on predictive equations, using the direct measures of R and Xc plotted on a graph. | BIVA-specific software packages |
Hydration status, recent meal consumption, and physical activity are significant and interrelated confounding factors in BIA assessment. Adherence to strict, standardized protocols before and during testing is non-negotiable for generating reliable and reproducible data in scientific research and clinical trials. While new evidence suggests some flexibility regarding fasting [51], and while modern MFBIA devices show promise for use in real-world conditions [5], controlling for these confounders remains the cornerstone of valid BIA application. The protocols provided herein offer a framework for researchers to minimize variability and enhance the accuracy of body composition evaluation in studies where precise measurement is critical.
Standardization of Measurement Protocols for Enhanced Reliability
Bioelectrical impedance analysis (BIA) has emerged as a widely adopted method for assessing body composition in both research and clinical settings, yet significant variability in measurement protocols and terminology continues to challenge the reliability and comparability of results [56]. This application note addresses the critical need for standardized methodologies to enhance the consistency and accuracy of BIA measurements within body composition research. The persistence of confusing terminology, such as the interchangeable use of "lean body mass" for fat-free mass (FFM) or lean soft tissue, further complicates accurate interpretation [56]. Recent validation studies consistently demonstrate that while BIA shows strong correlation with reference methods like dual-energy X-ray absorptiometry (DXA), significant measurement biases exist that can be mitigated through standardized approaches and population-specific calibrations [23] [5]. This document provides researchers with evidence-based protocols, technical specifications, and analytical frameworks to improve methodological rigor in BIA applications.
Quantitative Comparison of BIA Technologies and Performance
Table 1: Technical Specifications and Performance Characteristics of BIA Technologies
| Technology Type | Frequency Range | Electrode Configuration | Key Advantages | Limitations | Validation Correlation with DXA (FFM) |
|---|---|---|---|---|---|
| Single-Frequency BIA (SF-BIA) | 50 kHz fixed | Bipolar (hand-to-hand or foot-to-foot) | Affordable, user-friendly, portable [4] | Lacks raw data access, limited clinical validation, overlooks regional fat distribution [4] | r = 0.97, but overestimates FFM by 3.1 kg (+7.2%) [23] |
| Multifrequency BIA (MF-BIA) | 1-1000 kHz (typically 5, 50, 250, 500, 1000 kHz) [5] | Tetrapolar or octopolar | Enables segmental analysis, differentiates ICW/ECW, greater accuracy for fluid distribution and lean mass [4] | Higher cost, proprietary algorithms, usually requires standing position [4] | r = 0.93-0.96, bias -3.7 to -1.9 kg FM [5] |
| Bioelectrical Impedance Spectroscopy (BIS) | Spectrum of frequencies | Typically tetrapolar | Accurate hydration assessment vs. isotopic dilution [4] | Requires specialized expertise, costlier | Comparable to MF-BIA for ICW assessment [4] |
Table 2: Performance Validation of BIA Against Reference Methods Across Populations
| Study Population | Sample Size | Reference Method | BIA Technology | Agreement for FFM | Agreement for FM |
|---|---|---|---|---|---|
| Brazilian Adults & Older Adults [23] | 945 participants | DXA | Tanita BC-418 (BIA) | Overestimation of 3.1 kg (SD=2.4; +7.2%) [23] | Underestimation of 2.9 kg (2.3; -13.0%) [23] |
| US Marines [5] | 1000 participants (667 men, 333 women) | DXA | InBody 770 (MFBIA) | r = 0.95 (men), 0.94 (women); bias 3.4 kg (men), 2.0 kg (women) [5] | r = 0.93 (men), 0.96 (women); bias -3.7 kg (men), -1.9 kg (women) [5] |
| South African Children [57] | 323 children | Deuterium dilution | Bodystat 1500MDD (SF-BIA) | R² range: 58.3% (manufacturer eq.) to 89.0% (validated eq.) [57] | RMSE range: 1.1 kg (validated eq.) to 3.4 kg (manufacturer eq.) [57] |
| White Healthy Adults [58] | 211 individuals | DXA | Akern 101 & TELELAB | Minimal fixed bias with new equations vs. manufacturer equations [58] | Reduced mean bias with validated equations [58] |
Standardized Experimental Protocols
Pre-Test Subject Preparation and Environmental Controls
Hydration Status: No standardization of hydration is required for MF-BIA in real-world conditions, as MF-BIA can differentiate water compartments [5]. However, for highly controlled laboratory studies, maintain normal hydration and avoid dehydration or overhydration protocols unless specifically investigating these states [4].
Food and Beverage Intake: In real-world assessments, participants can be measured under typical daily conditions without fasting requirements [5]. For maximum standardization in controlled studies, implement a 4-hour fast prior to testing, avoiding caffeine and alcohol during this period [4].
Physical Activity: Participants should avoid strenuous exercise for 12 hours preceding measurement to prevent fluid shifts and changes in skin temperature that alter electrical properties of tissue [5].
Measurement Environment: Maintain comfortable room temperature (20-25°C) to prevent skin temperature variations. Use electrical isolation equipment if necessary to prevent interference [4].
Subject Positioning and Electrode Placement Protocol
Body Position:
- For ambulatory subjects: Use standing position with arms abducted approximately 15-30° from torso and thighs separated [4] [5].
- For bedridden patients: Use supine position with limbs abducted from torso to prevent skin surface contact [4].
- Maintain consistent positioning between measurements as changes affect fluid distribution and impedance values.
Electrode Placement:
- Octopolar Configuration: Place electrodes on bilateral dorsal hand/foot surfaces at metacarpophalangeal and metatarsophalangeal joints, and bilateral wrists/ankles between styloid processes and malleoli [4].
- Tetrapolar Configuration: Place detecting electrodes at the midpoint between the styloid process of the wrist and the ulnar tubercle on the dorsal side, and between the medial and lateral malleoli on the anterior side of the ankle [4].
- Bipolar Configuration: Ensure full palm and plantar foot contact with electrodes; apply electrolyte gel if necessary to improve conductivity [4].
Skin Preparation: Clean skin with alcohol swabs at electrode sites and allow to fully dry before electrode placement to reduce impedance at the electrode-skin interface [4].
Device Operation and Data Collection Workflow
Calibration: Perform device calibration according to manufacturer specifications before each testing session using recommended test loads or calibration cells.
Measurement Sequence:
- Input subject data (age, sex, height, weight) before measurement.
- Ensure subjects stand quietly for 3-5 minutes pre-measurement if using standing position.
- Instruct subjects to remain still during measurement with minimal talking.
- Record raw impedance parameters (resistance [R], reactance [Xc], phase angle [PhA]) in addition to calculated body composition metrics [4].
Quality Assessment:
- Check for measurement artifacts (extreme values, inconsistent segmental readings).
- Repeat measurements if values fall outside expected ranges based on population norms.
- Document any protocol deviations or unusual conditions.
Technology Selection Framework
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Materials and Equipment for BIA Research
| Item | Specification | Research Function | Protocol Considerations |
|---|---|---|---|
| Multifrequency BIA Device | Octopolar configuration, frequency range 1-1000 kHz [4] [5] | Primary body composition assessment; differentiates ICW/ECW | Select based on population (ambulatory vs. bedridden); ensure raw data access [4] |
| Reference Method Equipment | DXA, deuterium dilution, ADP, or 4C model [57] | Validation and calibration of BIA measurements | Use for developing population-specific equations [23] [57] |
| Electrodes | Single-use, pre-gelled ECG electrodes | Signal transmission and detection | Ensure consistent placement using anatomical landmarks [4] |
| Skin Preparation Supplies | 70% isopropyl alcohol swabs, abrasive pads | Reduce impedance at electrode-skin interface | Allow to fully dry before electrode placement [4] |
| Anthropometric Equipment | Calibrated stadiometer, digital scale | Accurate height and weight input for equations | Measure height to nearest 0.1 cm, weight to 0.1 kg [5] |
| Calibration Equipment | Manufacturer-supplied test loads, verification cells | Device performance verification | Perform according to manufacturer schedule and protocol [4] |
| Environmental Controls | Room thermometer, electrical isolation equipment | Standardize measurement conditions | Maintain 20-25°C; document any deviations [4] |
Data Processing and Analytical Framework
Raw Data Acquisition and Equation Selection
Essential Raw Parameters: Ensure access to resistance (R), reactance (Xc), phase angle (PhA), and impedance (Z) values rather than relying solely on proprietary body composition estimates [4]. These raw bioelectrical parameters are critical for applying validated population-specific equations and for longitudinal monitoring of physiological changes.
Predictive Equation Selection:
- Choose equations developed using appropriate reference methods (DXA for fat mass and FFM; deuterium dilution for TBW; MRI/CT for skeletal muscle mass) [4].
- Prioritize equations validated in populations with similar demographic characteristics (age, sex, ethnicity, health status) to your study cohort [57].
- Utilize recently compiled equation databases that classify predictive equations by subject characteristics [4].
Calibration and Correction Procedures:
- Develop calibration equations when using BIA in new populations, as demonstrated in Brazilian adults where: DXAFFM = 0.94420 × BIAFFM – (0.01128 × Age) + 0.20516 [23].
- Implement multivariate prediction models that incorporate BIA raw data with anthropometric variables, such as: FFM (kg) = (Sex × 4.1797) + (Stature [cm] × 0.1062) + (Resistance Index [cm²/Ω] × 0.5289) + (Body Mass [kg] × 0.1797) - (Age [yrs] × 0.0705) - 5.4286 [23].
Bioelectrical Impedance Vector Analysis (BIVA)
Methodology: Plot R and Xc standardized by height (R/H and Xc/H) on the R-Xc graph to assess hydration status and cellular integrity without relying on population-specific equations [4].
Interpretation Framework:
Application Considerations: BIVA is particularly valuable for monitoring patients with conditions affecting hydration status (renal disease, heart failure) and for tracking physiological changes in athletes [4].
Standardization of BIA measurement protocols represents a critical advancement in body composition research, addressing the substantial methodological variability that currently limits comparability across studies. The implementation of evidence-based protocols for subject preparation, positioning, electrode placement, and device operation significantly enhances measurement reliability. Furthermore, the selection of appropriate BIA technology matched to specific research questions and population characteristics, coupled with rigorous data processing using validated predictive equations, substantially improves the accuracy and clinical utility of body composition assessments. This comprehensive framework for standardized BIA implementation provides researchers with the necessary tools to generate reproducible, valid body composition data across diverse populations and research settings.
Bioelectrical impedance analysis (BIA) has emerged as a practical method for body composition assessment in research and clinical settings. Its advantages include operational simplicity, portability, and low cost compared to reference methods like dual-energy X-ray absorptiometry (DXA) [59]. However, a significant limitation of BIA lies in its indirect estimation approach, which relies on predictive equations that often assume constant proportions of fat, lean mass, and body fluids across diverse populations [59].
The development of population-specific calibration equations addresses a critical methodological need in BIA research. Generalized equations frequently demonstrate substantial bias when applied to populations with characteristics different from the original development cohort [60] [25]. Factors such as age, geographical ancestry, health status, physical activity level, and specific physiological characteristics necessitate tailored approaches to BIA equation development [25]. This document provides comprehensive application notes and experimental protocols for developing, validating, and implementing population-specific BIA calibration equations within body composition research.
Theoretical Framework and Critical Needs
Limitations of Generalized BIA Equations
The fundamental principle of BIA involves measuring the resistance (R) and reactance (Xc) of biological tissues to alternating electrical currents. These raw measurements are then converted into body composition estimates using predictive algorithms [60]. The accuracy of these algorithms depends heavily on their alignment with the physiological characteristics of the target population.
Recent research has demonstrated that generalized equations can produce significant measurement biases. In a study of Brazilian adults, BIA systematically overestimated fat-free mass (FFM) by 3.1 kg (+7.2%) and underestimated fat mass (FM) by 2.9 kg (-13.0%) compared to DXA [23]. Similarly, when assessing bone mineral content (BMC) in Korean populations, existing BIA equations showed substantial bias with mean differences up to 0.46 kg (p < 0.001) compared to DXA [59]. These inaccuracies stem from population-specific variations in body water distribution, tissue density, and segmental body proportions that generalized equations fail to capture [25].
Populations Requiring Specific Calibration Equations
Table 1: Populations Requiring Specific BIA Equations and Their Characteristics
| Population | Key Characteristics | Impact on BIA Measurements |
|---|---|---|
| Different Age Groups | Varying body water distribution, cellular integrity | Age-stratified models for BMC improved adjusted R² to 0.90 [59] |
| Various Ethnicities | Differences in body proportions, tissue density | Brazilian population required specific FFM equations to eliminate significant differences from DXA (p > 0.05) [60] |
| Overweight/Obese Individuals | Altered hydration factors, fluid distribution | Specific equations developed for overweight/obese adults showed CCC = 0.982, SEE = 2.50 kg [60] |
| Clinical Populations | Atypical fluid balance, altered body composition | Disease-specific equations needed for valid assessment [25] |
| Athletes | Higher lean mass, different hydration status | Require specific equations accounting for specialized body composition [25] |
Development of Population-Specific Equations
Experimental Protocol for Equation Development
Objective: To develop population-specific BIA predictive equations for body composition components using a criterion reference method.
Materials and Equipment:
- BIA device (specify model, manufacturer, electrode configuration)
- Reference method equipment (DXA, dilution techniques, MRI, etc.)
- Anthropometric equipment (calibrated scale, stadiometer)
- Electrode preparation supplies (alcohol wipes, abrasive pads)
- Data collection forms and secure database
Participant Preparation Protocol:
- Pre-test Instructions: Participants should abstain from alcohol and strenuous exercise for at least 48 hours prior to testing [59]. Fasting and refraining from water intake is required on the test day until completion [59].
- Bladder Emptying: Participants should empty their bladder within 30 minutes prior to testing [59].
- Clothing: Participants should wear designated laboratory attire, removing all jewelry and metal objects [60].
- Female Participants: Testing should be scheduled outside menstrual bleeding periods, with pregnancy as an exclusion criterion [59].
- Environmental Control: Measurements should be performed in a temperature-controlled room (26-28°C) [59].
Measurement Procedure:
- Anthropometry: Measure height to the nearest 0.1 cm and weight to the nearest 0.1 kg following standardized procedures [60].
- BIA Assessment:
- Clean contact surfaces (palms, soles) with electrolyte wipes [59].
- Position participant with feet apart and arms extended approximately 30° from the body [59].
- Perform triplicate measurements, recording resistance (R) and reactance (Xc) at all available frequencies.
- Note measurement conditions (time of day, device settings, electrode placement).
- Reference Method Assessment:
Statistical Analysis and Equation Development:
- Data Preparation: Calculate mean values for triplicate BIA measurements. Screen for outliers and data normality.
- Variable Selection: Include candidate predictors such as anthropometric variables (height, weight, BMI), BIA raw parameters (R, Xc, phase angle at multiple frequencies), and demographic factors (age, sex) [59].
- Model Development: Use stepwise regression or other appropriate variable selection methods to identify significant predictors from candidate variables [59].
- Model Optimization: Evaluate competing models based on adjusted R², root mean square error (RMSE), and theoretical plausibility [59].
- Validation Planning: Reserve a portion of the dataset (typically 30%) for internal validation [60].
Sample Size Considerations
A power analysis should be conducted prior to study initiation. For multiple regression approaches, a medium effect size (f² = 0.15), α = 0.05, and power of 0.80 typically require approximately 55 participants for 10 predictors [59]. Larger samples are needed for heterogeneous populations or when developing stratified equations.
Implementation and Validation Protocols
Validation Procedures for Developed Equations
Internal Validation Protocol:
- Cross-Validation: Apply developed equations to the reserved validation sample (30% of original sample) [60].
- Agreement Analysis: Assess agreement between BIA estimates and reference method using:
- Error Assessment: Calculate standard error of estimate (SEE), total error (TE), and mean absolute percentage error (MAPE).
External Validation Protocol:
- Independent Sample: Recruit new participants with identical inclusion criteria from the target population.
- Measurement Protocol: Follow identical procedures as in development phase.
- Comparison Analysis: Evaluate equation performance in the new sample using the same statistical measures.
Table 2: Performance Metrics of Population-Specific BIA Equations from Recent Studies
| Population | Body Component | Reference Method | Performance Metrics | Source |
|---|---|---|---|---|
| Healthy Korean (All Ages) | Bone Mineral Content | DXA | Adjusted R² up to 0.90; Mean difference -0.02 kg (p = 0.287) | [59] |
| Brazilian Adults | Fat-Free Mass | DXA | CCC ≥ 0.93; Calibration eliminated significant difference (p > 0.05) | [23] |
| Adults with Overweight/Obesity | Fat-Free Mass | DXA | CCC = 0.982; SEE = 2.50 kg; LOA = -5.0 to 4.8 kg | [60] |
| White, Healthy Adults | Skeletal Muscle Mass | DXA | Minimal fixed bias; Reduced mean bias versus manufacturer equations | [61] |
| US Marines (Real-World) | Fat Mass | DXA | Men: r = 0.93, bias -3.7 ± 2.6 kg; Women: r = 0.96, bias -1.9 ± 1.8 kg | [5] |
Implementation Considerations
Equipment-Specific Factors: BIA predictive equations are device-specific due to differences in:
- Electrode configuration (hand-to-foot, foot-to-hand, hand-to-hand, segmental) [25]
- Current frequency (single-frequency vs. multi-frequency) [5]
- Measurement technology (tetrapolar vs. octopolar) [5] Equations developed for one device cannot be directly applied to another without cross-validation.
Real-World Application: A study assessing multi-frequency BIA in uncontrolled conditions demonstrated modest population-level agreement with DXA for total body FM (men: r = 0.93, bias -3.7 ± 2.6 kg; women: r = 0.96, bias -1.9 ± 1.8 kg) [5]. This highlights that even with population-specific equations, environmental factors affect measurement accuracy.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for BIA Equation Development
| Item | Specification | Research Function |
|---|---|---|
| Multi-Frequency BIA Device | 8-point tactile electrode system (e.g., ACCUNIQ BC380) | Provides segmental impedance measurements at multiple frequencies for comprehensive tissue characterization [59] |
| Reference Standard Device | DXA scanner (e.g., Hologic Discovery Wi) | Criterion method for body composition assessment; requires daily calibration [59] |
| Single-Frequency BIA Device | Tetrapolar configuration (e.g., RJL Quantum IV) | Validation of TBW estimates; comparison of different BIA technologies [5] |
| Anthropometric Set | Digital scale (0.1 kg precision), stadiometer (0.1 cm precision) | Accurate measurement of fundamental anthropometric variables for prediction models [60] |
| Electrode Preparation Kit | Electrolyte wipes, abrasive pads, alcohol prep | Standardizes skin-electrode interface to reduce measurement variability [59] |
| Environmental Control | Temperature monitor, standardized clothing | Maintains consistent measurement conditions to minimize environmental effects [59] |
Workflow Visualization
Figure 1: Workflow for developing and validating population-specific BIA calibration equations, illustrating the sequential process from population definition through to implementation of validated equations.
Figure 2: Logical relationships between population characteristics, data inputs, and calibration equation development, showing how population factors influence both measurement inputs and equation development.
Population-specific calibration equations significantly enhance the accuracy and applicability of BIA for body composition assessment across diverse populations. The development of these equations requires rigorous methodology, appropriate reference standards, and comprehensive validation procedures. When properly developed and implemented, population-specific equations transform BIA from a screening tool into a valid assessment method suitable for research and clinical applications. Future work should focus on developing equations for underrepresented populations and establishing standardized protocols for equation development and validation.
Bioelectrical Impedance Analysis (BIA) is a widely used, non-invasive technique for assessing body composition by measuring the body's opposition to a low-level, alternating electric current [62] [4]. The method estimates body fat, fat-free mass (FFM), and body water based on the principle that lean tissues, with their high water and electrolyte content, are highly conductive, whereas fat and bone tissues act as insulators [62]. Despite its popularity in clinical and field settings due to its portability, safety, and ease of use, BIA relies on assumptions that often do not hold true in special populations [63]. This article examines the specific limitations and considerations for applying BIA in three distinct groups: athletes, obese individuals, and pediatric patients, and provides detailed protocols to enhance measurement validity within research and clinical practice.
Fundamental Principles and General Limitations of BIA
BIA determines body composition by measuring impedance (Z), a vector sum of resistance (R) and reactance (Xc) [4] [63]. Resistance represents the opposition to the flow of an electric current through intra- and extracellular ionic fluids, while reactance reflects the capacitive properties of cell membranes and tissue interfaces [63]. These raw measurements are used in predictive equations to estimate total body water (TBW), fat-free mass (FFM), and by difference with body weight, fat mass (FM) [62] [11].
A primary limitation of conventional BIA is its reliance on population-specific regression equations that assume constant relationships between body components, such as the hydration of FFM (set at 73%) and a uniform body geometry [62] [63]. These assumptions are frequently violated in special populations, leading to significant prediction errors. Furthermore, BIA measurements are highly sensitive to subject factors including hydration status, body temperature, glycogen stores, and recent physical activity and food intake [64] [11]. For instance, dehydration can cause a 5 kg underestimation of fat-free mass, while moderate exercise prior to measurement can lead to a substantial overestimation of FFM by nearly 12 kg [11].
Table 1: General Factors Affecting BIA Measurement Validity
| Factor | Effect on BIA Measurement | Recommended Control Protocol |
|---|---|---|
| Hydration Status | Dehydration increases resistance, leading to overestimation of body fat [11]. | Measure in a consistent, euphedrated state; avoid measurements after diuretic use or excessive fluid loss [64]. |
| Recent Food/Meal Intake | Measurements taken after a meal can show lower body fat readings, with daily variations up to 4.2% [11]. | Perform measurements after a fast of 4+ hours, ideally in the morning [65]. |
| Recent Physical Activity | Moderate-high intensity exercise reduces impedance, underestimating body fat and overestimating FFM [11]. | Avoid strenuous exercise for 24 hours prior to testing [64] [11]. |
| Body Temperature | Fever or elevated skin temperature can alter fluid distribution and impedance. | Postpone measurement if the subject has a fever. |
| Ethnicity & Population | Standard equations may not be valid for all ethnicities or unique populations like athletes [64]. | Use population-specific, validated equations where available [62] [4]. |
Limitations and Applications in Athletes
The unique body composition of athletes—characterized by higher skeletal muscle mass and lower body fat—poses significant challenges for standard BIA. Predictive equations developed for the general population often fail to account for the athlete's altered tissue geometry and hydration status, leading to substantial errors. Research indicates a tendency for BIA to overestimate percentage body fat, with the error being more pronounced in African American athletes [64]. One study on bodybuilders found that BIA underestimated fat mass and overestimated fat-free mass compared to the four-compartment model, which is the criterion method [62].
The primary issue is the lack of BIA equations for athletes that have been derived and validated against the four-compartment model [62]. Furthermore, the hydration status of athletes is highly dynamic due to training, which can directly confound impedance measurements. A single-frequency BIA (SF-BIA) cannot differentiate between intracellular (ICW) and extracellular water (ECW), a limitation that is critical when monitoring athletes for dehydration or fluid shifts [63].
Protocol for BIA Assessment in Athletes
Aim: To obtain valid and reliable body composition measurements in athletes for research purposes. Materials: A phase-sensitive, multi-frequency (MF-BIA) or bioelectrical impedance spectroscopy (BIS) device with a tetrapolar or octopolar configuration is recommended [4]. Consumer-grade, hand-to-hand or foot-to-foot devices should be avoided for research purposes due to their lower accuracy and reliance on proprietary equations [4]. Procedure:
- Pre-Test Standardization: Adhere to the following conditions for 24 hours prior to testing:
- No strenuous exercise.
- Maintain consistent hydration.
- Avoid alcohol and caffeine.
- Measurement Conditions: Conduct measurements in the morning after an overnight fast (≥8 hours) and after the athlete has voided their bladder [65].
- Body Position: For tetrapolar devices, place single-use electrodes on the right hand and foot according to the manufacturer's guidelines, with the subject lying supine and limbs abducted from the body [4].
- Data Recording: Record the raw bioelectrical parameters—Resistance (R), Reactance (Xc), and Phase Angle (PA)—rather than relying solely on the device's proprietary body fat percentage output [4] [63].
- Analysis: Use the raw data with validated equations specific to athletic populations, if available. Alternatively, employ Bioelectrical Impedance Vector Analysis (BIVA) to qualitatively assess hydration status and cellular integrity without relying on invalidated equations [63].
Diagram 1: BIA protocol workflow for athletes.
Limitations and Applications in Obese Individuals
In morbidly obese individuals, several physiological and anatomical factors limit the validity of standard BIA. This population exhibits a relatively high amount of total body water (TBW) and extracellular water (ECW), which leads to an overestimation of fat-free mass and a consequent underestimation of fat mass [66]. Furthermore, the body's geometry deviates significantly from the uniform cylindrical model assumed by BIA algorithms. Central body fat distribution, particularly severe abdominal obesity, alters the path of the electrical current and can result in an overestimation of the percentage of body fat when using prediction formulas developed in normal-weight individuals [66].
Validation studies show that BIA can underestimate fat mass by 1.9 kg and overestimate fat-free mass by 1.8 kg in obese subjects compared to the four-compartment model [62]. Of greater concern are the individual error rates; in one study, BIA underestimated fat mass by 5 kg or more in 12 out of 50 participants [62]. There is currently a lack of BIA equations sufficiently validated in individuals with a body mass index (BMI) greater than 34 kg/m², making the application of standard BIA in morbid obesity problematic [66].
Protocol for BIA Assessment in Obese Individuals
Aim: To enhance the accuracy and reliability of BIA for body composition assessment in obese subjects in a research context. Materials: A multi-frequency BIA (MF-BIA) device with a tetrapolar configuration is essential. The use of foot-to-foot (bipolar) consumer scales is discouraged due to their documented inaccuracy in this population and inability to account for central fat distribution [4]. Procedure:
- Pre-Test Conditions: Follow standard pre-test guidelines (fasting, no exercise, etc.) as outlined in the general protocol.
- Positioning: For subjects with severe obesity, ensure the examination table or surface can safely support their weight. If using a standing device, ensure the footplate electrodes are appropriately spaced.
- Electrode Placement: Take care to ensure proper skin contact for electrodes. The skin may need to be cleaned with alcohol if edema is present.
- Data Interpretation: Recognize that standard equations will likely yield inaccurate results. Where possible, use raw impedance data (R and Xc) with predictive equations that have been specifically developed and cross-validated in morbidly obese populations against a reference method like the four-compartment model [66]. Bioelectrical Impedance Vector Analysis (BIVA) can be used to track qualitative changes in hydration and body cell mass over time, which may be more informative than absolute quantitative values [63].
Limitations and Applications in Pediatric Populations
The use of BIA in children is inherently challenging due to the rapid growth-related changes in height, weight, FFM, and FM [67]. Children are not simply scaled-down adults; their bodies have different proportions of water and electrolytes, and their fat-free mass is less hydrated and contains more potassium per kg than that of adults [67]. These developmental differences mean that predictive equations developed for adults are not applicable to children.
Furthermore, the validity of BIA in children is complicated by a lack of appropriate reference methods for validation and a scarcity of BIA equations that are refined for specific ethnicities and ages [67]. Despite these limitations, recent studies suggest that BIA-derived body composition and phase angle measurements are valuable for assessing nutritional status and growth in children, and may be useful for monitoring progress during nutritional interventions [67] [65].
Protocol for BIA Assessment in Pediatric Populations
Aim: To safely and effectively monitor body composition and nutritional status in children for clinical research. Materials: A phase-sensitive, multi-frequency BIA device that is validated for use in children. The device should provide access to raw bioelectrical parameters [67] [65]. Procedure:
- Pre-Test Preparation: Explain the procedure to both the child and parent/guardian to alleviate anxiety. Calibrate the device before each session [65].
- Subject Preparation: The child should be in a fasting state (≥4 hours), have an empty bladder, and be measured in lightweight clothing or underwear. Jewelry should be removed [65].
- Measurement: Conduct the measurement with the child standing barefoot on a calibrated scale (for foot-to-foot devices) or in a supine position with electrodes placed on the right hand and foot (for tetrapolar devices) [65].
- Data Analysis: Use pediatric-specific, validated BIA equations that are appropriate for the child's age, sex, and ethnicity. The Phase Angle can be used as a marker of cellular health and nutritional status [67] [65]. As with other populations, focus on tracking changes over time rather than relying on single measurements.
Table 2: Summary of Key Limitations and Research-Grade Protocols by Population
| Population | Core Limitation | Recommended Device | Key Protocol Consideration | Data Interpretation Strategy |
|---|---|---|---|---|
| Athletes | Invalid general population equations; dynamic hydration [62] [64]. | MF-BIA/BIS, Tetrapolar/Octopolar [4]. | Strict 24h pre-test standardization (no exercise, consistent hydration) [64]. | Use raw parameters (R, Xc, PhA); Employ BIVA or athletic-specific equations [63]. |
| Obese Individuals | Altered body water & geometry; underestimates fat mass [62] [66]. | MF-BIA, Tetrapolar [4]. | Ensure safe positioning; proper electrode contact with skin. | Use raw data with obesity-specific equations; BIVA for qualitative tracking [66] [63]. |
| Pediatric Patients | Rapidly changing body composition; adult equations not valid [67]. | MF-BIA validated for children. | Child-friendly explanation; fasting & empty bladder [65]. | Use pediatric, age/ethnicity-specific equations; track trends & Phase Angle [67]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for BIA Research
| Item | Function in BIA Research | Specification/Note |
|---|---|---|
| Phase-Sensitive MF-BIA/BIS Analyzer | The core instrument for measuring impedance. Provides multiple frequencies to differentiate ICW and ECW [4]. | Prefer tetrapolar or octopolar over bipolar configurations. Ensure regulatory certification for clinical use [4]. |
| Single-Use Electrodes | Ensure consistent and hygienic electrical contact with the subject. | Use pre-gelled, self-adhesive electrodes. Place on the right hand and foot per manufacturer guidelines. |
| Calibration Kit/Weight | Verifies the accuracy of the integrated scale in the BIA device. | Calibrate according to manufacturer schedule and before each testing session [65]. |
| Statistical Software (R, Python, SPSS) | For applying population-specific equations to raw data and performing longitudinal analysis. | Necessary as device proprietary outputs may use invalidated equations [4]. |
| Reference Data Tables (BIVA) | Allow for interpretation of raw vector data (R/Xc) by comparing subject results to healthy or population-specific tolerance ellipses [63]. | Critical for the "classic" BIVA method to assess hydration and cellular mass. |
| Anthroposphere-eter & Stadiometer | For accurate measurement of height and weight, which are required for most predictive equations and impedance indexing. | Use calibrated, professional-grade equipment. |
Bioelectrical Impedance Analysis offers a practical and non-invasive method for body composition assessment, but its application in special populations requires critical consideration of its inherent limitations. For athletes, obese individuals, and children, standard protocols and generalized equations are prone to significant error due to unique physiological and anatomical characteristics. To generate valid and reliable data for research and clinical practice, it is imperative to use appropriate technology (preferably multi-frequency devices with tetrapolar configurations), adhere to strict measurement protocols, and—most importantly—apply analytical strategies that move beyond the device's built-in estimations. These strategies include using raw bioelectrical parameters and leveraging population-specific equations or qualitative methods like BIVA to ensure that findings accurately reflect body composition in these distinct groups.
Bioelectrical Impedance Analysis (BIA) has evolved from a simple body composition tool into a sophisticated technology capable of integration with advanced microfluidic and imaging platforms. This evolution supports its growing role in precise clinical assessments and pharmaceutical research. Modern BIA instruments now range from consumer-grade scales to advanced multi-frequency, multi-electrode systems that provide detailed insights into fluid distribution and cellular health [4]. These advancements make BIA an ideal cornerstone technology for hybrid systems, enabling non-invasive, real-time monitoring of physiological changes critical for nutritional science, drug efficacy studies, and chronic disease management [68].
The integration of BIA with microfluidic systems allows for continuous, miniaturized biomarker monitoring, while fusion with imaging modalities enhances spatial resolution for anatomical correlation. For researchers and drug development professionals, these hybrid platforms offer a powerful approach to obtain multifaceted data from a single experimental setup. This document provides detailed application notes and experimental protocols for leveraging these advanced integrations within body composition research.
Technical Foundations of Modern BIA
Core Principles and Key Parameters
BIA estimates body composition by measuring the impedance (Z) of biological tissues to a low-intensity, safe alternating current. Impedance comprises two components: resistance (R), which reflects the opposition to current flow through intra- and extracellular fluids, and reactance (Xc), which represents the capacitive properties of cell membranes [44] [4]. The phase angle (PhA), derived from the arctangent of the Xc/R ratio, serves as a biomarker for cellular integrity and nutritional status [44] [4].
Key BIA Parameters and Their Physiological Significance:
| Parameter | Symbol | Physiological Significance | Research Application |
|---|---|---|---|
| Resistance (R) | R | Inversely related to Total Body Water (TBW) and electrolyte content [21]. | Tracking fluid shifts, edema, or dehydration [44]. |
| Reactance (Xc) | Xc | Reflects the capacitance of cell membranes; indicates cell mass and membrane integrity [44]. | Assessing cellular health, muscle quality, and nutritional status [21] [69]. |
| Phase Angle (PhA) | PhA | A prognostic marker of cell membrane function and body cell mass; calculated as arctangent (Xc/R) × (180/π) [44] [4]. | Monitoring disease progression, nutritional intervention outcomes, and muscle function [21] [69]. |
Advanced BIA Modalities
The choice of BIA modality significantly impacts the depth and accuracy of body composition data.
- Multi-Frequency BIA (MF-BIA): Uses a range of frequencies (e.g., 5 kHz to 1 MHz) to differentiate water compartments. Low-frequency currents primarily traverse the extracellular water (ECW), while high-frequency currents penetrate cell membranes, enabling assessment of both ECW and intracellular water (ICW) [5] [4]. This is superior to Single-Frequency BIA (SF-BIA) for patients with altered hydration [4].
- Bioelectrical Impedance Vector Analysis (BIVA): A method that plots raw R and Xc values, normalized for height, on a nomogram. It allows for the qualitative assessment of hydration status and body cell mass without relying on population-specific predictive equations [44] [69]. This is particularly valuable for monitoring patients with fluid imbalances or for cross-population studies where standard equations may not apply.
- Segmental BIA: Advanced octopolar devices (e.g., DSM-BIA) measure impedance across five body segments (arms, legs, trunk) independently. This provides a more detailed analysis of fluid distribution and muscle mass in specific regions, which is crucial for detecting localized edema or assessing sarcopenia [70] [4].
Integrated System Design and Workflow
The synergistic combination of BIA with microfluidics and imaging creates a powerful analytical platform. The following diagram illustrates the core architecture and experimental workflow of such a hybrid system.
Figure 1: Integrated System Workflow. The diagram outlines the parallel data acquisition from BIA, microfluidic sampling, and hybrid imaging, culminating in a centralized data fusion and analysis module.
Application Notes & Experimental Protocols
Protocol 1: Validating BIA-Muscle Quality Assessment with Ultrasound
Objective: To validate BIA-derived parameters against muscle ultrasound echogenicity for assessing muscle quality in nutritional and sarcopenia research [21].
Background: Muscle echogenicity (EG) measured by ultrasound increases with intramuscular fat infiltration and fibrosis. This protocol correlates EG with BIA raw parameters to establish a non-invasive method for muscle quality assessment.
Research Reagent Solutions:
| Item | Function/Specification | Example |
|---|---|---|
| Phase-Sensitive BIA Analyzer | Measures raw parameters (R, Xc) at 50 kHz for calculating PhA. | Akern BIA 101 or equivalent [21] [69]. |
| Ultrasound System with A-Mode Probe | For consistent measurement of muscle tissue echogenicity. | 2.5 MHz A-mode probe (e.g., BodyMetrix) [21]. |
| Adhesive Electrodes | Low-impedance electrodes for standardized BIA measurements. | Biatrodes Akern or equivalent single-use electrodes [69]. |
| Conductive Gel | Ultrasound gel for acoustic coupling during imaging. | Standard medical-grade ultrasound gel. |
| Anatomical Marking Pen | For precise and reproducible probe placement. | Surgical skin marker. |
Methodology:
- Participant Preparation: Subjects should abstain from vigorous exercise, alcohol, and caffeine for 12 hours, and fast for at least 4 hours prior to measurement to ensure stable hydration [69].
- BIA Measurement:
- Ultrasound Measurement:
- With the subject standing, mark the midpoint between the hip and knee joints on the dominant thigh.
- Apply conductive gel and place the A-mode probe perpendicular to the skin surface. Acquire multiple images of the vastus lateralis muscle.
- Use analysis software (e.g., Adipometria) to determine muscle EG.
- Data Analysis:
- Perform Pearson or Spearman correlation analysis between muscle EG and BIA parameters (R, Xc, PhA, ICW). A strong negative correlation between PhA and EG is expected, indicating that a lower phase angle (poor cellular health) is associated with higher echogenicity (worse muscle quality) [21].
Protocol 2: Real-World Body Composition Tracking with MF-BIA
Objective: To assess the reliability of Multi-Frequency BIA (MF-BIA) for measuring body composition in real-world, non-fasted conditions, relevant for long-term pharmaceutical or nutritional intervention studies [5].
Background: While tightly controlled conditions are ideal, real-world applicability is crucial. This protocol tests MF-BIA's performance against DXA without controlling for prandial or hydration status.
Methodology:
- Device Setup: Use an octopolar MF-BIA device (e.g., InBody 770) and a DXA scanner. Calibrate both devices according to manufacturer specifications [5].
- Subject Protocol: Recruit participants and instruct them to attend testing sessions at their convenience, without specific fasting or hydration instructions. Record time of last meal and drink.
- Measurement:
- Measure height and weight.
- Have the subject stand on the MF-BIA device, barefoot, holding the hand electrodes. The device will run multiple frequencies to estimate total and segmental Fat Mass (FM), Fat-Free Mass (FFM), and Visceral Adipose Tissue (VAT).
- Immediately following the BIA, perform a whole-body DXA scan.
- Data Analysis:
- Compare MF-BIA and DXA outputs for total body FM, %BF, and FFM using correlation analysis (Pearson's r), intraclass correlation coefficient (ICC), and Bland-Altman plots to assess bias and limits of agreement [5].
- Expect strong correlations for total body and trunk FM, but potentially lower agreement for VAT, highlighting the importance of method selection based on the target compartment [5].
Protocol 3: Microfluidic-BIA Interface for Sweat Biomarker Monitoring
Objective: To integrate a wearable BIA sensor with a microfluidic patch for the simultaneous monitoring of hydration status and electrolyte loss in athletes or clinical populations.
Background: Wearable BIA can track fluid shifts, while microfluidics enables continuous analysis of sweat analytes like sodium. Combining these provides a comprehensive hydration profile.
Methodology:
- System Fabrication: Develop a flexible epidermal patch incorporating:
- BIA Module: Miniaturized electrodes and circuitry to measure localized impedance at a single or multiple frequencies.
- Microfluidic System: A network of microchannels that wicks sweat from the skin to a sensing chamber. Integrate reagent-based colorimetric sensors for sodium and potassium.
- Validation:
- Affix the hybrid patch to the subject's forearm or trunk.
- Induce sweating through controlled exercise.
- Simultaneously collect BIA data (local R and Xc) and images of the colorimetric sensor via a smartphone camera.
- Compare BIA-derived hydration trends with dynamically measured electrolyte concentrations from the microfluidic channel.
The following tables consolidate key performance and correlation data from recent studies to aid in experimental design and result interpretation.
Table 1: MF-BIA vs. DXA Validity in Real-World Conditions (n=1000) [5]
| Body Composition Parameter | Sex | Correlation (r) with DXA | Bias (Mean Difference) | Concordance Correlation Coefficient (CCC) |
|---|---|---|---|---|
| Total Body Fat Mass (FM) | Men | 0.93 | -3.7 kg | - |
| Women | 0.96 | -1.9 kg | - | |
| Percent Body Fat (%BF) | Men | 0.89 | -4.2 % | - |
| Women | 0.92 | -2.8 % | - | |
| Fat-Free Mass (FFM) | Men | 0.95 | +3.4 kg | - |
| Women | 0.94 | +2.0 kg | - | |
| Trunk FM | Men | 0.92 | - | 0.86 |
| Women | 0.93 | - | 0.93 | |
| Visceral Adipose Tissue (VAT) | Men | 0.74 | - | 0.68 |
| Women | 0.74 | - | 0.34 |
Table 2: Correlation between BIA Parameters and Muscle Ultrasound Echogenicity (n=993) [21]
| BIA Parameter | Correlation Coefficient (r) with Muscle Echogenicity | Physiological Interpretation |
|---|---|---|
| Resistance (Rz) | +0.347 | Higher resistance is weakly associated with poorer muscle quality (more fat/fibrosis). |
| Intracellular Water (ICW) | -0.479 / -0.386 (L/%) | Lower ICW is moderately associated with poorer muscle quality. |
| Phase Angle (PhA) | -0.487 | A lower phase angle is moderately associated with poorer muscle quality. |
Technical Specifications and Selection Guide
Choosing the correct BIA instrument is critical for research quality. The following diagram and table guide the selection process based on research objectives.
Figure 2: BIA Instrument Selection Guide. A decision tree for selecting the appropriate BIA technology based on specific research requirements.
Table 3: BIA Instrumentation Overview for Research Applications [70] [4]
| Device Type | Key Features | Advantages | Limitations | Best Suited For |
|---|---|---|---|---|
| Single-Frequency (SF-BIA) | Single frequency (50 kHz); often bipolar (hand-to-hand/foot-to-foot). | Low cost, portable, easy to use [4]. | Less accurate with fluid imbalances; proprietary algorithms; no raw data [4]. | Large-scale epidemiological studies (group trends) [4]. |
| Multifrequency (MF-BIA) | Multiple frequencies (1kHZ-1MHz); tetrapolar/octopolar. | Differentiates ICW/ECW; more accurate for FFM; segmental analysis [5] [4]. | Higher cost; requires more standardization [4]. | Clinical research, nutritional interventions, geriatrics [5] [4]. |
| Bioimpedance Spectroscopy (BIS) | Measures impedance across a spectrum of frequencies. | Most accurate for fluid compartment analysis [4]. | Expensive; complex data analysis; less common. | Dialysis management, critical care hydration monitoring [4]. |
| Devices with BIVA Capability | Provides access to raw R and Xc parameters. | Equation-independent; direct assessment of hydration and cell mass [44] [69]. | Requires expertise to interpret vector patterns [4]. | Populations with fluid shifts (athletes, patients) or where predictive equations are invalid [69]. |
Validation Against Reference Methods and Comparative Performance Analysis
In body composition research, criterion methods are reference standards against which the validity of practical field methods, such as bioelectrical impedance analysis (BIA), is assessed. These methods provide the most accurate measurements of body fat mass (FM), fat-free mass (FFM), bone mineral content (BMC), and total body water (TBW) available in living humans. The four-compartment (4C) model, which divides the body into fat, water, mineral, and protein masses, is considered the fundamental criterion for body composition analysis because it directly addresses biological variability in these components. Dual-energy X-ray absorptiometry (DXA or DEXA) and magnetic resonance imaging (MRI) are also widely regarded as gold-standard imaging techniques, with DXA being the clinical standard for bone density and whole-body composition and MRI providing unparalleled soft tissue detail. For researchers using BIA, these criterion methods are essential for cross-validation, development of population-specific prediction equations, and establishing the clinical credibility of BIA devices. This article details the application and protocols for these gold-standard methods within a BIA research framework.
Technical Specifications and Performance of Criterion Methods
The following table summarizes the key technical attributes, measured components, and performance metrics of the primary criterion methods.
Table 1: Technical Specifications and Performance of Criterion Body Composition Methods
| Method | Measured Components | Principle of Operation | Accuracy & Precision | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Four-Compartment (4C) Model | Fat Mass, Fat-Free Mass, Total Body Water, Bone Mineral, Protein | Mathematical model combining measurements from multiple reference methods (e.g., ADP for BV, DXA for BMC, deuterium dilution for TBW). | Highest theoretical accuracy; error propagation of ~3.4-3.5% of body mass for body fat [71]. | Accounts for variability in hydration and bone mineral content; considered the ultimate criterion. | Complex, time-consuming, requires multiple sophisticated instruments. |
| Dual-Energy X-Ray Absorptiometry (DXA/DEXA) | Bone Mineral Density (BMD), Fat Mass, Lean Soft Tissue Mass (LSTM) [72] | Uses two low-energy X-ray beams to differentiate tissue types based on differential attenuation [73]. | High precision (ICC 0.990–0.998); high agreement with 4C models [5] [74]. Considered a clinical gold standard [72]. | Quick (<10 mins), low radiation, provides regional and whole-body analysis [73]. | Accuracy can be affected by body thickness, hydration status, and tissue edema. |
| Magnetic Resonance Imaging (MRI) | Skeletal Muscle Mass, Adipose Tissue (including Visceral, Subcutaneous, Intramuscular), Organs | Uses strong magnetic fields and radio waves to excite hydrogen protons, creating detailed images of soft tissues. | Extremely high resolution and accuracy for soft tissue quantification; superior for muscle quality and fat infiltration [72]. | No ionizing radiation; excellent for visualizing internal fat depots and organ-specific fat. | Very high cost, long scan times, not practical for routine body composition tracking [72]. |
| Computed Tomography (CT) | Skeletal Muscle Mass, Adipose Tissue (especially Visceral), Bone | Uses a series of X-ray images to create cross-sectional "slices" of the body. | Extremely accurate for visceral adipose tissue (VAT) quantification [72]. | Excellent for visceral fat and organ-specific fat analysis. | Very high radiation exposure; expensive; not suitable for longitudinal studies [72]. |
| Air-Displacement Plethysmography (ADP) | Body Density (BD), from which % Body Fat is derived | Measures body volume by air displacement in a sealed chamber (e.g., Bod Pod) [71]. | Solid accuracy; compared favorably to hydrodensitometry. | Quick, non-invasive, no water immersion required. | Sensitive to clothing, posture, and lung air volume; less accurate for extreme body types [72]. |
Detailed Experimental Protocols
Four-Compartment (4C) Model Protocol
The 4C model provides the most accurate body composition assessment by dividing the body into four distinct chemical components: water, mineral, protein, and fat. This model improves upon simpler models by accounting for individual variability in bone mineral and hydration status.
3.1.1 Principle and Workflow
The 4C model is derived from the following foundational equation, which uses measurements obtained from other criterion methods:
Fat Mass = 2.748 * BV - 0.699 * TBW - 1.129 * BMC - 2.051 * Body Mass
Where BV is Body Volume, TBW is Total Body Water, and BMC is Bone Mineral Content [74]. The protocol involves a sequential measurement of body mass, body volume, total body water, and bone mineral content.
3.1.2 Step-by-Step Procedure
- Body Mass (BM) Measurement: Measure body mass to the nearest 0.01 kg using a calibrated electronic scale, with the participant wearing minimal, light clothing.
- Body Volume (BV) Measurement: Determine body volume using Air-Displacement Plethysmography (ADP).
- Procedure: The participant, wearing a tight-fitting swim cap and minimal clothing (or standardized compression apparel), sits inside the ADP chamber.
- The chamber door is sealed, and the system measures the displaced air volume.
- The test is typically performed in duplicate, with the participant asked to perform a normal breathing protocol and remain still.
- Total Body Water (TBW) Measurement: Assess TBW using the deuterium oxide (D₂O) dilution technique.
- Procedure: Collect a baseline urine or saliva sample from the participant.
- Administer a pre-weighed oral dose of D₂O.
- Allow a 3-4 hour equilibration period for the isotope to distribute throughout the body's water compartments.
- Collect a post-dose urine or saliva sample.
- Analyze the isotope enrichment in the samples using isotope ratio mass spectrometry to calculate TBW.
- Bone Mineral Content (BMC) Measurement: Obtain BMC from a whole-body DXA scan, following the protocol outlined in Section 3.2.
- Calculation: Input the measured values for BM, BV, TBW, and BMC into the 4C equation to calculate fat mass and fat-free mass.
The following diagram illustrates the integrated workflow of the 4C model:
Dual-Energy X-Ray Absorptiometry (DXA) Protocol
DXA is valued for its speed, low radiation dose, and ability to provide regional body composition data, making it ideal for assessing muscle-fat asymmetry and bone health concurrently [75] [73].
3.2.1 Pre-Scan Preparation and Positioning
- Participant Instructions: Participants should fast for 4-12 hours, be adequately hydrated, and avoid strenuous exercise for 24 hours prior. They must remove all metal objects and wear a hospital gown or light, metal-free clothing [73].
- Pregnancy Screening: Pre-menopausal female participants must be screened for pregnancy; a negative test is required before scanning [75] [73].
- Positioning: The participant lies supine on the DXA table. To flatten lumbar lordosis for a spine scan, a positioning block is placed under the knees. For a hip scan, the femur is internally rotated using a positioning brace to elongate the femoral neck. The arms are slightly separated from the trunk, and the feet are secured in dorsiflexion to maintain position [73].
3.2.2 Scan Acquisition and Analysis
- System Calibration: Perform a daily quality assurance scan using the manufacturer's phantom to calibrate the instrument.
- Whole-Body Scan: The scanning arm passes over the participant from head to feet, typically taking 6-10 minutes. The participant must remain motionless.
- Regional Analysis: Using the manufacturer's software (e.g., GE encore), the whole-body image is analyzed. Standard regions of interest (arms, legs, trunk) are defined automatically and manually adjusted by a trained technician to ensure anatomical accuracy, using bony landmarks [75].
- Data Output: The software provides values for total and regional fat mass, lean soft tissue mass, bone mineral content (BMC), and bone mineral density (BMD).
Table 2: Key Anatomical Landmarks for DXA Regional Analysis
| Body Region | Proximal Landmark | Distal Landmark | Lateral Landmarks |
|---|---|---|---|
| Arm | Humeral head, inferior to acromion | Distal to radial and ulnar styloid processes | Through the glenohumeral and radioulnar joints. |
| Leg | Inferior to the femoral neck (greater trochanter) | Distal to the tibial and fibular malleoli | Through the femoral and tibiofibular joints. |
| Trunk | Inferior to the chin | At the iliac crests, superior to the pelvis | Along the lateral aspects of the ribs and pelvis, excluding the arms. |
| Anterior/Posterior Thigh (Research) | 80% of distance from lateral epicondyle to greater trochanter [75] | Lateral epicondyle of the femur [75] | Down the shaft of the femur (medial) and outside the leg area (lateral) [75]. |
Magnetic Resonance Imaging (MRI) Protocol
MRI is the gold standard for quantifying specific adipose tissue depots and assessing muscle morphology without ionizing radiation.
3.3.1 Image Acquisition
- Participant Positioning: The participant lies supine in the MRI scanner. To standardize visceral fat measurement, arms are extended above the head. Coils are placed over the abdomen or the specific body region of interest.
- Sequence Selection: A T1-weighted fast spin-echo sequence is typically used due to its high signal-to-noise ratio and excellent contrast between adipose (bright) and non-adipose (dark) tissues.
- Slice Thickness and Gap: For abdominal analysis, a series of contiguous axial slices (e.g., 10 mm thickness with 0 mm gap) are acquired from the xiphoid process to the top of the iliac crest. For whole-body composition, the entire body is scanned in sequential segments.
3.3.2 Image Analysis and Quantification
- Software-Based Segmentation: Analyze images using specialized software (e.g., SliceOmatic, HippoFat). The analyst manually or semi-automatically traces the boundaries of different tissue compartments on each axial image.
- Tissue Compartment Identification:
- Subcutaneous Adipose Tissue (SAT): The adipose tissue located between the skin and the outer abdominal wall muscles.
- Visceral Adipose Tissue (VAT): The adipose tissue located inside the abdominal cavity, surrounding the organs.
- Skeletal Muscle (SM): Major muscle groups are identified based on anatomical location and cross-sectional area.
- Volume Calculation: The cross-sectional area (cm²) of each tissue in every slice is calculated by the software. The volume (cm³) is then determined by multiplying the area by the slice thickness. Total tissue mass is derived by multiplying the total volume by the assumed density of the tissue (e.g., 0.92 kg/L for fat, 1.04 kg/L for muscle).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Reagents for Criterion Body Composition Assessment
| Item | Function/Application | Example Specifications |
|---|---|---|
| Dual-Energy X-ray Absorptiometry (DXA) System | Gold-standard measurement of areal bone mineral density (BMD), fat mass, and lean soft tissue mass. | GE Lunar iDXA (or equivalent from Hologic, Norland) with encore software [75]. |
| Air-Displacement Plethysmography (ADP) System | Measurement of total body volume (BV) for 4-compartment and body density models. | Bod Pod system, requires calibration with a cylinder of known volume [71]. |
| Deuterium Oxide (D₂O) | Tracer for the isotope dilution measurement of total body water (TBW) in 4C models. | 99.9% atom purity, dose typically 0.05-0.1 g per kg body mass [74]. |
| Isotope Ratio Mass Spectrometer | Analysis of deuterium enrichment in biological samples (urine, saliva) for TBW calculation. | High-precision instrument capable of measuring small differences in isotope ratios. |
| Magnetic Resonance Imaging (MRI) Scanner | Gold-standard quantification of adipose tissue depots (VAT, SAT) and skeletal muscle volume. | 1.5T or 3.0T scanner with dedicated body and surface coils [72]. |
| Anthropometric Kit | For basic measurements and supplementary data: height, weight, circumferences. | Calibrated stadiometer, electronic scale, non-stretchable tape measure. |
| Positioning Aids (Foam Pads, Straps) | Standardize participant positioning during DXA and MRI scans to ensure measurement reliability and reproducibility. | Medical-grade foam pads, tibia positioning block, hip positioning brace [75] [73]. |
BIA Validation Framework Against Criterion Methods
The primary application of criterion methods in BIA research is to validate the accuracy and reliability of BIA devices and their predictive equations. The following diagram outlines a standard validation workflow:
Key Validation Steps:
- Participant Cohort: Recruit a sample that represents the target population for the BIA device (e.g., athletes, elderly, clinical patients). A large sample size (n > 100) improves generalizability [5].
- Concurrent Testing: Perform BIA and the criterion method (e.g., DXA, 4C model) in quick succession, ideally within 1-2 hours, under standardized conditions (fasting, euhydration, no recent exercise) [5].
- Data Collection: For BIA, prioritize devices that provide access to raw parameters (Resistance-R, Reactance-Xc, Phase Angle-PhA). This allows researchers to apply and develop population-specific equations rather than relying on the manufacturer's proprietary algorithms [4].
- Statistical Analysis:
- Use Pearson's correlation (r) and Lin's Concordance Correlation Coefficient (CCC) to assess the strength and agreement of the relationship between BIA and the criterion.
- Employ Bland-Altman plots to visualize the mean bias (average difference between methods) and the 95% limits of agreement, identifying any systematic over- or under-estimation by the BIA device [5].
- Calculate the Standard Error of Estimate (SEE) and Root Mean Square Error (RMSE) to quantify the average error of the BIA prediction.
This structured validation framework ensures that BIA can be deployed with known and acceptable margins of error for specific research or clinical purposes.
Accurate body composition assessment is critical in clinical research and pharmaceutical development. While Dual-Energy X-Ray Absorptiometry (DXA) is widely considered a reference method, Bioelectrical Impedance Analysis (BIA) offers a portable, cost-effective alternative. This application note synthesizes findings from recent validation studies (2024-2025) quantifying the agreement between BIA and DXA across diverse populations and measurement components, providing researchers with structured data and standardized protocols for method selection and implementation.
Table 1: Agreement for Fat Mass (FM) and Fat-Free Mass (FFM) Assessment
| Population | Sample Size | BIA Device | DXA Device | Parameter | Agreement Metric | Key Finding | Citation |
|---|---|---|---|---|---|---|---|
| Adults with Obesity | 28 | InBody S10 | GE Lunar Prodigy Primo | FM & FFM | ICC (Supine): Excellent | Supine posture showed narrowest LOA; seated posture poorest, especially with high WC. | [76] |
| Adults (22-92 years) | 1,116 | InBody 770 | GE Lunar iDXA | Relative ALM | Mean Bias: +0.25 kg/m² | Strong correlation (R²=0.88); consistent overestimation by BIA across ages. | [77] |
| Mixed BMI (Retrospective) | 3,655 | Bodystat QuadScan 4000 | Lunar Prodigy Advance | FM | CCC: 0.94 | High correlation, but BIA underestimated FM in most BMI classes >18.5. | [78] [79] |
| Children with SMA | 57 | InBody S10 | Hologic Horizon W | FM & MM | CCC: 0.95-0.96 | BIA underestimated FM, overestimated MM; good agreement for nutritional evaluation. | [80] |
| Pediatric Obesity | 28 Studies | Various | Various | FM | Trend: Systematic Underestimation | BIA consistently underestimated BF% and FM vs. DXA in overweight/obese children. | [81] |
Table 2: Agreement for Bone and Skeletal Muscle Parameters
| Population | Sample Size | BIA Device | DXA Device | Parameter | Agreement Metric | Key Finding | Citation |
|---|---|---|---|---|---|---|---|
| Healthy Taiwanese Adults | 318 | StarBIA-201 | GE Lunar Prodigy | Whole-Body BMD | r = 0.737, Bias: -0.053 g/cm² | BIA underestimated BMD; useful for screening but not interchangeable. | [82] |
| Healthy Korean Population | 302 | ACCUNIQ BC380 | Hologic Discovery Wi | Bone Mineral Content (BMC) | Adjusted R²: Up to 0.90 | Age-stratified optimized models showed negligible bias vs. DXA. | [59] |
| Adult Cohort | 353 | Foot-to-Hand BIA | DXA | Skeletal Muscle Mass (SMM) | Bias (New Eq.): -0.01 kg | Novel phase-angle equation showed excellent accuracy vs. Janssen equation (+3.65 kg bias). | [83] |
| Various (Device Comparison) | 77 | Six BIA Devices | DXA | % Body Fat | ICC Range: 0.25 - 0.73 | Multi-frequency BIA devices demonstrated superior reliability vs. single-frequency. | [84] |
Detailed Experimental Protocols from Key Studies
Protocol: Posture Impact in Obesity (2024)
This study evaluated the critical effect of patient posture on BIA measurement accuracy in obesity [76].
- Population: 28 adults (mean age 61.4 ± 6.9 years, BMI 38.6 ± 5.0 kg/m²).
- Experimental Workflow:
- Key Procedures:
- Subject Preparation: Minimum 8-hour fast, 24-hour avoidance of moderate-to-vigorous physical activity.
- BIA Measurements: Conducted using the InBody S10 in three postures (supine, standing, seated) with electrode placement per manual.
- WC Stratification: Participants divided by median WC (118.3 cm) to analyze impact of body shape.
- DXA Reference: Whole-body DXA scan performed in supine position on the same day.
- Statistical Analysis: Intraclass Correlation Coefficient (ICC) and 95% Limits of Agreement (LOA) calculated for FM and FFM.
Protocol: Lean Mass Agreement Across Lifespan (2025)
This large-scale study validated BIA for appendicular lean mass (ALM) assessment across adults aged 22-92 [77].
- Population: 1,116 healthy adults (55% female) from the Copenhagen Sarcopenia Study.
- Experimental Workflow:
- Key Procedures:
- Anthropometry: Height and weight measured to the nearest 0.1 cm/kg in light clothing.
- BIA Measurement: Conducted using InBody 770 (multi-frequency, 8-electrode) per manufacturer's instructions.
- DXA Reference: Whole-body scan performed on GE iDXA; analysis with Encore software v16.0.
- Data Processing: ALM calculated as sum of lean soft tissue from arms and legs. Relative ALM derived as ALM/height².
- Statistical Analysis: Linear regression (R²) and Bland-Altman analysis for bias and LOA.
Protocol: Bone Mineral Density Validation (2024)
This study evaluated a novel BIA device for whole-body bone mineral density (BMD) measurement [82].
- Population: 318 healthy Taiwanese adults (145 male, 173 female), aged 19.4-84.0 years.
- Key Procedures:
- Device: StarBIA-201, a foot-to-foot BIA device.
- Testing Protocol: Participants stood barefoot on device platform for BIA measurement.
- Reference Standard: DXA scan using Lunar Prodigy system.
- Analysis: Paired t-test, Pearson correlation (r), and Bland-Altman plots with trend analysis.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials and Equipment for BIA-DXA Validation Studies
| Item | Specification/Model Examples | Critical Function in Research |
|---|---|---|
| Multi-Frequency BIA | InBody 770, InBody S10, Bodystat QuadScan 4000, ACCUNIQ BC380 | Measures impedance at multiple frequencies to differentiate intra/extracellular water and estimate body composition. Segmental devices (e.g., InBody) show better agreement with DXA [84] [81]. |
| DXA System | GE Lunar (iDXA, Prodigy), Hologic Discovery Wi, Hologic Horizon | Gold-standard reference for body composition, providing measures of fat mass, lean mass, and bone mineral content/density. |
| Ethanol Wipes | 70% Isopropyl Alcohol | Ensures clean skin at electrode sites to minimize impedance and measurement error. |
| Calibration Phantoms | DXA Spine Phantom, BIA Calibrator | Daily quality control and assurance for both DXA and BIA devices to ensure measurement precision and longitudinal consistency. |
| Anthropometry Kit | Stadiometer, Digital Scale, Non-Stretchable Tape | Provides accurate height, weight, and waist circumference data for normalization and analysis. |
| Phase Angle Equation | Novel SMM Equation [83] | Enhances estimation of skeletal muscle mass from raw BIA parameters (reactance, phase angle), improving accuracy over generic equations. |
Critical Factors Influencing Agreement
The level of agreement between BIA and DXA is not static but is influenced by several key variables that researchers must control or account for:
- Posture: The supine position demonstrates the highest agreement with DXA, while the seated position shows the poorest, especially in individuals with high waist circumference where limb-trunk contact disrupts current flow [76].
- Body Mass Index (BMI): Agreement varies across BMI categories. BIA tends to underestimate Fat Mass and overestimate Fat-Free Mass in overweight and obese adults (BMI > 25) compared to DXA [78] [79]. This trend of FM underestimation is also consistent in pediatric obesity [81].
- Device Technology: Multi-frequency, segmental BIA analyzers (e.g., InBody models) consistently demonstrate superior reliability and narrower limits of agreement with DXA compared to single-frequency or simpler devices [84] [81].
- Population-Specific Equations: The accuracy of BIA is heavily dependent on the predictive equations used. Optimized, population-specific equations for parameters like Skeletal Muscle Mass [83] and Bone Mineral Content [59] can significantly reduce bias versus DXA, whereas generalized equations may introduce significant error.
Bioelectrical Impedance Analysis (BIA) is widely utilized in body composition research due to its non-invasive nature, portability, and cost-effectiveness. However, its accuracy is compromised by systematic biases, specifically the overestimation of Fat-Free Mass (FFM) and concomitant underestimation of Fat Mass (FM), particularly when compared to reference methods like Dual-Energy X-ray Absorptiometry (DXA). These biases stem from fundamental assumptions in BIA technology and are exacerbated by population-specific factors such as obesity, fluid imbalances, and the use of non-validated predictive equations. This document delineates the quantitative evidence for these biases, details standardized protocols for mitigating them, and provides visual frameworks to guide researchers in validating BIA methodology for specific cohorts, ensuring data integrity in clinical and pharmaceutical development settings.
Quantitative Evidence of Systematic Biases
Extensive validation studies across diverse populations consistently demonstrate that BIA tends to overestimate FFM and underestimate FM compared to criterion methods. The following table summarizes key findings from recent research.
Table 1: Documented Systematic Biases in BIA Compared to Reference Methods
| Population Studied | Reference Method | Bias in Fat-Free Mass (FFM) | Bias in Fat Mass (FM) | Citation |
|---|---|---|---|---|
| Women with Overweight/Obesity (Postpartum) | DXA | Overestimation: +1.2 kg (2 weeks pp), +0.7 kg (6 months pp) | Underestimation: -0.7 kg (2 weeks pp), -0.3 kg (6 months pp) | [85] |
| Healthy, Physically Active Adults | DXA | Overestimation: +3.4 kg (men), +2.0 kg (women) | Underestimation: -3.7 kg (men), -1.9 kg (women) | [5] |
| Patients with Obesity (Cohort of 2134) | DXA | Overestimation: Ranged from +2.18 kg to +8.28 kg across different equations | Underestimation: Ranged from -1.91 kg to -7.41 kg across different equations | [86] |
| Breast Cancer Patients | DXA | Overestimation: +4.1 kg (mean across 18 equations) | Not explicitly stated (inferred from FFM overestimation) | [87] |
These discrepancies are critical for researchers to consider during data interpretation. The bias can lead to an underestimation of the effectiveness of an intervention designed to reduce fat mass or preserve lean mass. Furthermore, the error is not consistent and is influenced by factors such as the degree of obesity, hydration status, and the specific predictive equation used by the BIA device [86] [87].
Experimental Protocols for Bias Assessment and Mitigation
To ensure the validity of BIA data in research, the following protocols provide a framework for method validation and standardized measurement.
Protocol 1: Validation of BIA against a Criterion Method
This protocol is designed to characterize the magnitude and direction of bias in a specific study population.
1. Objective: To determine the agreement between BIA-derived body composition estimates (FFM and FM) and a reference standard (DXA) within a defined cohort. 2. Materials: * Criterion method: Dual-Energy X-ray Absorptiometry (DXA) scanner. * Bioelectrical Impedance Analyzer (multi-frequency devices are preferred for enhanced compartment differentiation). * Calibrated digital scale and stadiometer. * Data collection forms and statistical software (e.g., SPSS, R). 3. Procedure: * Participant Preparation: Schedule participants after an overnight fast (≥12 hours). Instruct them to avoid strenuous exercise, alcohol, and diuretics (e.g., caffeine) for at least 24 hours prior. Adhere to a euhydrated state and void the bladder immediately before testing. * Measurement Order: Conduct BIA and DXA measurements sequentially on the same day, ideally in a randomized order to avoid systematic error. The time between measurements should be minimized. * BIA Measurement: * Ensure the participant is in a supine position for at least 10 minutes prior to measurement to allow for fluid stabilization. * Place electrodes on the hand, wrist, foot, and ankle according to the manufacturer's guidelines on the dominant side of the body. * Record resistance (R), reactance (Xc), and phase angle (PhA) in addition to the device's calculated FFM and FM. * DXA Measurement: * Perform a whole-body scan following the manufacturer's standard operating procedure. * Ensure participants remove all metal objects and wear lightweight clothing. 4. Data Analysis: * Use paired t-tests to assess mean differences between methods. * Employ Bland-Altman analysis to plot the differences between BIA and DXA against their means, establishing limits of agreement and checking for proportional bias. * Calculate Pearson's correlation coefficient (r) and Concordance Correlation Coefficient (CCC) to evaluate strength and precision of agreement.
Protocol 2: Standardized BIA Operation for Longitudinal Monitoring
This protocol ensures consistency in BIA measurements for tracking body composition changes over time, crucial for clinical trials.
1. Objective: To obtain reliable and reproducible BIA measurements for longitudinal assessment of body composition changes. 2. Pre-test Controls: * Time of Day: Conduct all follow-up measurements at the same time of day (± 1 hour) as the baseline measurement to control for diurnal variation. * Hydration & Diet: Strictly enforce pre-test fasting and fluid intake controls as defined in Protocol 1. * Exercise: Mandate a 24-hour period without vigorous exercise before testing. * Clothing: Use the same lightweight clothing for each measurement, or use a hospital gown. 3. Device and Operator Consistency: * Use the same BIA device model for all measurements throughout the study. * Calibrate the device daily according to manufacturer instructions. * Where possible, the same trained operator should perform all measurements to minimize inter-observer variability. 4. Data Recording: * Document raw bioelectrical parameters (R, Xc, PhA) in addition to derived body composition values. This allows for post-hoc analysis and the application of alternative, population-specific equations if needed [60].
The following workflow diagram illustrates the logical sequence for implementing these protocols in a research setting.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for BIA Body Composition Analysis
| Item | Function/Application in Research |
|---|---|
| Dual-Energy X-ray Absorptiometry (DXA) | Considered the gold-standard criterion method for validating BIA-derived estimates of FM, FFM, and bone mineral content in a research context. It provides a three-compartment model. |
| Multi-Frequency BIA (MF-BIA) Device | The preferred tool for research. The use of multiple current frequencies (e.g., 1 kHz, 50 kHz, 250 kHz) allows for better differentiation between extracellular (ECW) and total body water (TBW), improving FFM estimation accuracy. |
| Single-Frequency BIA (SF-BIA) Device | A common, lower-cost tool. Suitable for large-scale field studies but with recognized limitations in accuracy, especially in populations with abnormal fluid balance. |
| Bioelectrical Impedance Vector Analysis (BIVA) | A technique that uses the raw parameters Resistance (R) and Reactance (Xc) normalized for height, plotted on a tolerance ellipse. It provides a qualitative assessment of hydration and body cell mass independent of predictive equations. |
| Population-Specific BIA Equations | Validated predictive equations (e.g., Roubenoff for general obesity, Gray for adolescents) are critical reagents. Using equations derived from a different population is a major source of systematic bias. |
| Standardized Electrolyte Wipes | Used to clean the skin (palms and soles) before electrode placement, ensuring low skin impedance and improving measurement reproducibility. |
Understanding the root causes of these systematic errors is essential for robust research design.
1. Hydration Status and Fluid Compartments: BIA fundamentally estimates body water compartments, from which FFM is derived assuming a constant hydration fraction of 73%. This assumption is frequently violated in populations such as athletes, the elderly, and individuals with obesity, who may exhibit variations in the extracellular water to total body water (ECW/TBW) ratio. An elevated ECW/TBW ratio, common in inflammatory states or edema, leads to a systematic overestimation of FFM [85] [86].
2. Limitations of Predictive Equations: BIA devices utilize proprietary or published equations that incorporate variables like height, weight, sex, age, and impedance to predict FFM. A primary source of bias is the application of an equation developed in one population (e.g., healthy, normal-weight adults) to a demographically or clinically distinct population (e.g., adolescents with severe obesity or breast cancer patients). Studies consistently show that population-specific equations significantly improve accuracy [88] [89] [60]. For instance, the Roubenoff equation has been recommended for patients with obesity, while the Gray and Hamilton equations showed superior performance in obese adolescents [86] [88].
3. Device-Specific and Segmental Factors: Technological factors introduce variability. Single-frequency (SF-BIA) devices are more susceptible to hydration artifacts than multi-frequency (MF-BIA) devices, which can better account for fluid shifts [5]. Furthermore, segmental BIA devices, which model the body as five cylinders (trunk, arms, legs), are anticipated to be more reliable than whole-body models, particularly for assessing trunk composition [85] [5].
The following diagram illustrates the interconnected logical relationships between the sources of bias and their ultimate effect on research data.
In body composition research, validating new measurement techniques against established reference methods is a fundamental practice. Bioelectrical impedance analysis (BIA) has emerged as a practical, non-invasive, and cost-effective alternative to more complex body composition assessment methods like dual-energy X-ray absorptiometry (DXA) [4]. However, introducing new BIA devices or predictive equations requires rigorous statistical validation to ensure measurement reliability and accuracy. Three statistical methodologies form the cornerstone of method comparison studies: Bland-Altman analysis for assessing agreement between two quantitative measurement techniques, Lin's Concordance Correlation Coefficient (CCC) for evaluating precision and accuracy relative to a perfect concordance line, and Receiver Operating Characteristic (ROC) analysis for determining the diagnostic accuracy of classification tests [90] [91] [92]. This article provides detailed application notes and experimental protocols for implementing these statistical approaches within the context of BIA validation studies, enabling researchers to conduct robust method comparison analyses.
Theoretical Foundations
Bland-Altman Analysis
The Bland-Altman plot, also known as the difference plot, is a graphical method for comparing two measurement techniques [93] [94]. In this approach, the differences between paired measurements from two methods are plotted against their averages, with horizontal lines drawn at the mean difference (bias) and the limits of agreement, defined as the mean difference ± 1.96 times the standard deviation of the differences [93] [95]. This method allows researchers to visualize systematic bias, identify proportional bias, and assess the range within which 95% of differences between the two methods are expected to lie [94]. The interpretation hinges on whether the limits of agreement are clinically acceptable, which is a contextual determination based on the specific application domain [95].
Lin's Concordance Correlation Coefficient (CCC)
While conventional correlation coefficients like Pearson's r measure the strength of a linear relationship between two variables, they fail to capture systematic differences or deviations from perfect agreement [92]. Lin's CCC (ρc) remedies this limitation by evaluating both precision (how far observations deviate from the best-fit line) and accuracy (how far the best-fit line deviates from the 45° line of perfect concordance) [90] [92]. The resulting coefficient ranges from -1 to 1, with values closer to 1 indicating better agreement. Unlike Bland-Altman analysis which focuses on differences, Lin's CCC provides a single metric summarizing overall agreement while accounting for both systematic and random error components.
Receiver Operating Characteristic (ROC) Analysis
ROC analysis evaluates the performance of diagnostic tests in classifying subjects into categorical groups [91]. By plotting sensitivity (true positive rate) against 1-specificity (false positive rate) across all possible test cut-off points, the ROC curve visually represents the trade-off between these competing metrics [91]. The area under the ROC curve (AUC) provides an overall measure of diagnostic accuracy, ranging from 0.5 (no better than chance) to 1.0 (perfect discrimination) [91]. In body composition research, ROC analysis helps establish optimal cut-off values for BIA-derived parameters to identify conditions like obesity, sarcopenia, or metabolic syndrome.
Application in BIA Validation Studies
Comparative Analysis of BIA Against Reference Methods
Recent validation studies have employed these statistical approaches to evaluate BIA devices against reference standards like DXA. A 2024 study comparing the CUN-BAE equation with BIA in Southern Indian populations demonstrated significant absolute agreement, with mean body fat percentage values of 28.91 ± 8.94 (BIA) versus 29.22 ± 8.63 (CUN-BAE) [90]. The researchers utilized Bland-Altman plots, intraclass correlation coefficients, and concordance correlation coefficients to establish comparable efficacy between the methods [90].
Similarly, a 2022 study examining a handheld BIA device (Omron HBF-306C) against DXA in Veterans with COPD found strong concordance for fat mass (ρc = 0.95) but only moderate concordance for percent body fat (ρc = 0.67) and fat-free mass (ρc = 0.74) [92]. The study further employed Bland-Altman analysis, revealing a mean difference of 2.7 ± 3.2 kg for fat mass between BIA and DXA [92]. These findings highlight the importance of multi-faceted statistical validation, as agreement may vary across different body composition parameters.
Table 1: Statistical Agreement Between BIA and Reference Methods in Recent Studies
| Study Population | Comparison | Statistical Method | Key Findings | Citation |
|---|---|---|---|---|
| Southern Indians (n=351) | CUN-BAE vs. BIA | Bland-Altman, ICC, CCC | Significant absolute agreement for BF%; comparable efficacy for detecting MetS | [90] |
| Veterans with COPD (n=50) | Handheld BIA vs. DXA | Lin's CCC, Bland-Altman | Excellent concordance for fat mass (ρc=0.95); moderate for BF% (ρc=0.67) and FFM (ρc=0.74) | [92] |
| Children (n=443) | BIA vs. DXA | Correlation analysis, ICC, Lin's CCC, Bland-Altman | Strong correlations (r=0.853-1.000) but BIA overestimated BMC (62.7-66.5%) and underestimated BF% (-8.9 to -0.8%) | [96] |
| CRC patients (n=43) | BIA vs. DXA | Linear regression, Bland-Altman | Strong linear relationships (R²=0.94-0.98) but large equation-dependent discrepancies in FFM estimates (-11.0 to 6.8 kg) | [97] |
Factors Influencing BIA Validity
The performance of BIA devices varies considerably based on several technical and biological factors. Device specifications, including single-frequency versus multi-frequency technology, electrode configuration (bipolar, tetrapolar, or octopolar), and the predictive equations employed significantly impact measurement accuracy [4]. Additionally, population characteristics such as age, sex, ethnicity, health status, and body composition extremes influence validity, as demonstrated by stronger BIA-DXA correlations in obese versus non-obese subjects (ρ = 0.96 vs. 0.84 for fat mass) [92]. Hydration status represents another critical factor, as BIA estimates body composition based on the conductive properties of water-rich tissues [96] [4].
Experimental Protocols
Protocol for BIA Method Comparison Studies
Table 2: Essential Research Reagents and Equipment
| Item | Specifications | Function/Purpose | Examples/References |
|---|---|---|---|
| Reference Standard Device | DXA, ADP, or 4-compartment model | Gold-standard body composition assessment for validation | GE Lunar iDXA (DXA); Hologic QDR-4500A (DXA) [96] [92] |
| BIA Device Under Investigation | Specify frequency, electrode configuration, model | Test method for comparison against reference | Tanita BC-622 (single-frequency); Omron HBF-306C (handheld) [96] [92] |
| Anthropometric Equipment | Stadiometer, calibrated scale | Accurate height and weight measurements | Electronic height-weight scale (AD-6351) [96] |
| Data Collection Forms | Standardized templates | Consistent data recording across participants | Customized case report forms |
| Statistical Software | R, SPSS, MedCalc, GraphPad Prism | Implementation of statistical analyses | MedCalc for Bland-Altman plots [93] |
Study Design and Participant Preparation
Employ a cross-sectional design with simultaneous measurements using both methods to minimize temporal variation [90] [92]. Recruit participants representing the target population for the BIA device, ensuring appropriate sample size (typically n≥50 based on similar studies) [92]. Exclude individuals with conditions potentially affecting measurement accuracy (pacemakers, severe edema, pregnancy) [92]. Standardize testing conditions by requiring participants to: fast for at least 4 hours prior to assessment; avoid strenuous exercise for 12 hours; abstain from alcohol and caffeine for 24 hours; void immediately before measurements; and wear light clothing without metal objects [96] [92].
Measurement Procedures
Conduct reference method measurements first according to manufacturer protocols and established guidelines [96]. For DXA, perform quality control checks using manufacturer phantoms, position participants supine with arms slightly separated from body, and ensure minimal clothing [92]. For BIA, follow device-specific protocols regarding electrode placement, body position, and environmental conditions [96] [92]. With handheld devices like the Omron HBF-306C, ensure proper grip with arms extended forward [92]. With foot-to-foot devices, position participants standing upright with bare feet on electrodes [4]. Conduct triplicate measurements with repositioning to assess intra-method variability [92].
Data Management
Record all raw measurements systematically, including potential covariates (age, sex, ethnicity, health status) [90] [92]. Calculate derived body composition parameters (fat mass, fat-free mass, percentage body fat) using consistent equations across methods. For BIA devices using proprietary equations, document the equation version and consider collecting raw impedance data (resistance, reactance) when possible to enable application of alternative predictive equations [4].
Statistical Analysis Protocol
Data Preparation
Organize paired measurements from both methods in a structured dataset. Check for normality of differences using Shapiro-Wilk test or QQ plots when implementing parametric Bland-Altman analysis [94]. Address outliers through diagnostic checks rather than automatic removal.
Bland-Altman Analysis Implementation
Calculate differences between paired measurements (Method A - Method B) and their averages [(Method A + Method B)/2] [94]. Compute mean difference (bias) and standard deviation of differences. Determine limits of agreement as bias ± 1.96 × SD of differences [93] [95]. Create scatter plot with differences on Y-axis and averages on X-axis. Add horizontal lines for bias and limits of agreement. Visually inspect for proportional bias (correlation between differences and averages) and heteroscedasticity (systematic change in variability across measurement range) [95]. For non-normally distributed differences, use non-parametric percentiles for agreement limits [93].
Lin's CCC Implementation
Calculate Lin's CCC using statistical software with corresponding 95% confidence intervals [92]. Interpret values as follows: <0.90 = poor, 0.90-0.95 = moderate, 0.95-0.99 = substantial, >0.99 = almost perfect agreement. Compare with Pearson's correlation to distinguish precision from accuracy components.
ROC Analysis Implementation
For diagnostic performance assessment, create binary classification based on reference standard (e.g., obesity defined by DXA percent body fat) [91]. Calculate sensitivity and specificity at multiple BIA cut-off points. Plot ROC curve with sensitivity against 1-specificity. Determine AUC with 95% confidence interval. Identify optimal cut-off point using Youden's index (sensitivity + specificity - 1) or clinical requirements [91].
Data Interpretation Guidelines
Integrated Analysis Approach
No single statistical method provides a complete picture of method agreement. Implement all three approaches complementarily: Bland-Altman analysis quantifies measurement differences and establishes agreement intervals; Lin's CCC evaluates overall concordance while accounting for systematic error; and ROC analysis determines diagnostic performance when categorical classifications are needed [90] [91] [92]. Consider clinical context when interpreting statistical results, as statistically significant differences may not be clinically relevant, and vice versa [95].
Bland-Altman Interpretation
Assess mean difference (bias) for systematic measurement error. If consistent across measurement range, consider applying a fixed correction factor [94]. Evaluate limits of agreement width relative to clinically acceptable difference thresholds [93] [95]. Identify proportional bias if differences correlate with measurement magnitude, potentially requiring ratio-based Bland-Altman analysis or regression-based limits of agreement [93]. Detect heteroscedasticity if variability changes with measurement magnitude, possibly necessitating data transformation or percentage difference analysis [93].
Lin's CCC Interpretation
Compare Lin's CCC with Pearson's correlation coefficient. Similar values suggest minimal systematic error, while substantially lower CCC indicates accuracy issues despite good precision [92]. Consider values ≥0.95 as demonstrating excellent agreement for most body composition applications, though specific thresholds may vary by parameter and population [92].
ROC Analysis Interpretation
Interpret AUC values as follows: 0.5-0.7 = poor discrimination; 0.7-0.8 = acceptable; 0.8-0.9 = excellent; >0.9 = outstanding [91]. Select optimal cut-points based on clinical context: higher sensitivity for "rule-out" tests; higher specificity for "rule-in" tests; or maximize both using Youden's index [91]. Report corresponding likelihood ratios to facilitate clinical application across different prevalence settings [91].
Table 3: Troubleshooting Common Issues in Method Comparison Studies
| Issue | Detection Method | Potential Solutions |
|---|---|---|
| Proportional Bias | Significant correlation between differences and averages in Bland-Altman plot | Use regression-based limits of agreement; plot percentage differences; apply ratio Bland-Altman method [93] |
| Heteroscedasticity | Increasing variability with measurement magnitude in Bland-Altman plot | Express differences as percentages; apply logarithmic transformation; use regression-based limits of agreement [93] |
| Systematic Bias | Mean difference significantly different from zero | Apply fixed correction factor if bias consistent across range [95] |
| Non-Normal Differences | Shapiro-Wilk test p<0.05; non-random pattern in QQ plot | Use non-parametric percentiles for limits of agreement; transform data [93] [94] |
| Outliers | Points outside limits of agreement in Bland-Altman plot | Verify data entry errors; assess clinical plausibility; report with and without outliers [95] |
Bland-Altman analysis, Lin's CCC, and ROC analysis provide complementary statistical frameworks for comprehensive method comparison in BIA validation studies. When implemented according to the protocols outlined herein, these approaches enable robust assessment of new BIA devices and equations against reference standards. The growing diversity of BIA technologies, including single-frequency, multi-frequency, and segmental devices, necessitates continued rigorous validation using these statistical methods to ensure appropriate application in clinical and research settings [4]. By adhering to standardized measurement protocols and implementing integrated statistical analyses, researchers can generate high-quality evidence regarding BIA performance across diverse populations and clinical contexts.
The Phase Angle (PhA), derived from Bioelectrical Impedance Analysis (BIA), is a direct measurement calculated from the relationship between resistance (R) and reactance (Xc). Resistance represents the opposition to an alternating current caused by bodily fluids, while reactance reflects the capacitive properties of cell membranes. PhA, calculated as arctangent (Xc/R) and expressed in degrees, serves as a non-invasive biomarker for assessing cellular health, membrane integrity, and body composition in both research and clinical settings [98] [99]. This parameter indicates the ability of cells to store energy and reflects the distribution of water between intra- and extracellular compartments. A higher Phase Angle suggests greater cellular integrity and function, whereas lower values are associated with cell death or dysfunction, making it a valuable prognostic tool in nutritional assessment and disease management [99].
The clinical relevance of Phase Angle extends across various populations, from healthy adults to those with chronic conditions. Research demonstrates its utility in evaluating nutritional status, disease prognosis, and functional outcomes. In the context of a broader thesis on BIA for body composition research, understanding Phase Angle provides critical insights beyond conventional fat and lean mass measurements, offering a window into cellular-level physiological processes [100] [101].
Quantitative Data Synthesis: Phase Angle Associations Across Populations
Table 1: Correlations Between Phase Angle and Body Composition Parameters in Centrally Obese Adults [100]
| Body Composition Parameter | Males (Correlation Coefficient) | Females (Correlation Coefficient) | P-value |
|---|---|---|---|
| Skeletal Muscle Index (SMI) | B = 0.257 | B = 0.251 | < 0.001 |
| Fat-Free Mass Index (FFMI) | Significant positive association | Significant positive association | < 0.001 |
| Visceral Adipose Tissue (VAT) | B = -0.082 | Not significant | 0.017 |
Table 2: Phase Angle Reference Values and Associations in Diverse Cohorts
| Study Population | Sample Size | Mean Phase Angle | Key Correlations | Citation |
|---|---|---|---|---|
| Iranian Adults (Healthy) | 239 (85M, 154F) | Men: 6.2° ± 0.6°Women: 5.3° ± 0.6° | Positive with weight, BMI, WC, FFM, muscle mass, bone mass, visceral fat | [99] |
| Cancer Patients with Locomotive Syndrome | 190 (133M, 57F) | Not specified | Significant negative correlation with LS stage (rₛ = -0.507) | [101] |
| General Adult Population (Reference) | 4,367 total | Percentiles established | Decrement rates: Males: -0.03°/year (33-51 yrs), -0.05°/year (>51 yrs)Females: -0.03°/year (37.2-57.9 yrs) | [102] |
Experimental Protocols for Phase Angle Measurement
Standardized BIA Measurement Protocol
Objective: To obtain accurate and reproducible Phase Angle measurements using a multi-frequency bioelectrical impedance analyzer.
Equipment Setup:
- SECA mBCA 514 Medical Body Composition Analyzer or equivalent multi-frequency BIA device
- Standard electrode placements for tetrapolar measurement
- Calibrated stadiometer for height measurement
- Calibrated scale for body weight
Pre-Test Participant Preparation:
- Participants should fast for 3-4 hours prior to measurement
- Avoid caffeine, alcohol, or energy drinks within 24 hours of testing
- Refrain from strenuous physical activity for at least 12 hours before assessment
- Maintain normal hydration status without overhydration or dehydration
- Testing should be conducted in a temperature-controlled environment (24-26°C)
Measurement Procedure:
- Confirm participant meets inclusion/exclusion criteria (e.g., no pacemakers, metal implants, or clinically evident edema)
- Record participant demographics including age, sex, and clinical history
- Measure height and weight using standardized protocols
- Position participant in a standing position, barefoot, without metal accessories
- Ensure proper electrode contact according to manufacturer specifications
- Perform impedance measurement with participant remaining motionless
- Record resistance (R) and reactance (Xc) values directly from the device
- Calculate Phase Angle using the formula: PhA = arctangent (Xc/R) × (180/π)
Quality Control:
- Perform periodic device calibration according to manufacturer guidelines
- Conduct inter-rater reliability assessments (target ICC >0.90)
- Implement periodic cross-checks throughout the study period
- Standardize measurement timing to minimize diurnal variation (preferably morning to early afternoon) [100]
Protocol for Validating BIA Against Reference Methods
Objective: To establish the validity of BIA-derived Phase Angle and body composition measurements against criterion methods such as Dual-Energy X-Ray Absorptiometry (DXA).
Equipment:
- Multi-frequency BIA device (e.g., InBody 770, Tanita BC-418)
- DXA scanner (e.g., GE iDXA)
- Standard anthropometric equipment
Procedure:
- Recruit participants representing the target population demographics
- Perform BIA measurements following the standardized protocol above
- Conduct DXA scans according to manufacturer guidelines on the same day
- Ensure participants wear similar clothing (light athletic wear) for both assessments
- Maintain consistent positioning between measurements
- Extract DXA values for fat mass, fat-free mass, and regional body composition
- Analyze agreement between methods using correlation coefficients, concordance correlation coefficients (CCC), and Bland-Altman analysis [5] [23]
Statistical Analysis:
- Calculate Pearson correlation coefficients (r) for precision
- Determine Lin's concordance correlation coefficients (CCC) for accuracy
- Assess mean absolute and relative differences using paired t-tests
- Develop calibration equations using linear regression when systematic biases are identified [23]
Visualization of Bioelectrical Impedance Vector Analysis (BIVA)
BIVA Interpretation Diagram: This visualization represents the bioelectrical impedance vector analysis method, showing how vector position on the resistance-reactance graph corresponds to hydration status and body cellularity across four diagnostic quadrants. [98] [102]
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Essential Materials for BIA Research on Phase Angle
| Item | Specification/Model | Research Function | Protocol Notes |
|---|---|---|---|
| Multi-Frequency BIA Analyzer | SECA mBCA 514; InBody 770 | Measures resistance (R) and reactance (Xc) at multiple frequencies (1-1000 kHz) | Enables direct calculation of Phase Angle and ECW/TBW ratio [100] [5] |
| Reference Method Equipment | DXA (e.g., GE iDXA) | Criterion method for validating BIA body composition estimates | Provides accurate assessment of fat mass, lean mass, and bone density [5] [23] |
| Single-Frequency BIA | Quantum IV (RJL Systems) | Comparison for TBW estimation against MFBIA | Uses 50 kHz frequency; electrodes at wrist and ankle [5] |
| Bioelectrical Electrodes | Skintak electrodes or equivalent | Ensure consistent electrical contact for impedance measurement | Standard placement: base of middle toe, above ankle joint, base of middle finger, above wrist joint [98] |
| Anthropometric Equipment | Calibrated stadiometer, flexible tape measure | Accurate height and waist circumference measurement | Essential for standardized indices (SMI, FFMI, FMI) [100] [99] |
| Data Analysis Software | SPSS, R Statistical Computing | Statistical analysis of correlation and regression models | R package ggplot2 recommended for creating publication-quality graphs [100] |
Clinical and Research Applications of Phase Angle
The clinical validity of Phase Angle extends beyond basic research into practical healthcare applications. In cancer populations, Phase Angle shows significant negative correlation with locomotive syndrome stage (rₛ = -0.507, p < 0.001) and has been identified as an independent factor associated with mobility decline (OR = 0.361, 95% CI: 0.221-0.588) [101]. This demonstrates its utility as a simple screening tool for functional decline in clinical settings.
In hepatic cirrhosis, Phase Angle values below 5.4° serve as predictive markers for poor prognosis, with BIVA effectively identifying hydration and cellularity status in these patients who often present with fluid balance disturbances [98]. For central obesity management, Phase Angle demonstrates distinct patterns, positively associating with skeletal muscle indices (B = 0.257 in males, B = 0.251 in females) while showing inverse relationships with visceral adipose tissue in males (B = -0.082) [100].
The integration of Phase Angle assessment into clinical workflows provides a rapid, non-invasive method for evaluating cellular health that complements traditional anthropometric and laboratory measures. Recent reference studies have established percentile curves for Phase Angle across adult populations, enabling more precise interpretation of individual measurements in both research and clinical contexts [102].
Conclusion
Bioelectrical Impedance Analysis represents a versatile technology with expanding applications from clinical body composition assessment to sophisticated drug discovery platforms. While BIA provides a practical, non-invasive method for body composition analysis, evidence confirms significant discrepancies compared to reference methods like DXA, necessitating population-specific calibration and standardized protocols. The translational potential of BIA principles in ECIS systems offers revolutionary approaches for real-time, label-free drug screening and toxicity assessment. Future directions should focus on developing more accurate predictive models for diverse populations, establishing comprehensive reference data for raw parameters like phase angle, and advancing integrated systems that combine impedance measurement with other analytical modalities. For researchers and drug development professionals, these advancements promise enhanced precision in both nutritional epidemiology and pharmaceutical development, solidifying BIA's role as a critical tool in biomedical research.
References
- 1. Bioelectric impedance analysis [https://www.measurement-toolkit.org/anthropometry/objective-methods/bioelectric-impedence-analysis]
- 2. Bioelectrical Impedance Analysis (BIA) [https://www.scienceforsport.com/bioelectrical-impedance-analysis-bia/?srsltid=AfmBOoo5c-1vaoeBlgCLQ5eC02rLfCq28Do_tyET8Kubxx3tDfAFuK8_]
- 3. The science of bioelectrical impedance-derived phase angle [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316808/]
- 4. Bioelectrical impedance analysis instruments: how do they ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12337901/]
- 5. Real-world assessment of Multi-Frequency Bioelectrical ... [https://www.nature.com/articles/s41430-025-01664-4]
- 6. Wearables for health monitoring: body composition ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2025.1644082/full]
- 7. The evolution of bioimpedance analysis: From traditional ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900724002508]
- 8. Association between bioelectrical impedance analysis ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06963-9]
- 9. Bioelectrical Impedance: A History, Research Issues, and ... [https://www.ncbi.nlm.nih.gov/books/NBK233766/]
- 10. InBody Technologies – InBody BWA (Body Water Analyzer) [https://inbodybwa.com/learn/inbody-technologies/]
- 11. Bioelectrical impedance analysis [https://en.wikipedia.org/wiki/Bioelectrical_impedance_analysis]
- 12. Bioelectrical Impedance Analysis for Historical Evaluation ... [https://www.mdpi.com/2673-4605/10/1/3]
- 13. Accuracy of Bioelectrical Impedance Consumer Devices for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6452160/]
- 14. Real-world assessment of Multi-Frequency Bioelectrical ... [https://pubmed.ncbi.nlm.nih.gov/40957934/]
- 15. Phase Angle Evaluated by a Bioimpedance Analysis Is ... [https://www.jmaj.jp/detail.php?id=10.31662%2Fjmaj.2025-0071]
- 16. Segmental phase angle and the extracellular to ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900725000279]
- 17. Extracellular water-to-total body water ratio and its ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900725002837]
- 18. Association between phase angle and ECW/TBW ratio with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518083/]
- 19. Phase angle and water cell distribution as inflammation ... [https://www.nature.com/articles/s41598-025-98430-0]
- 20. Comparison study of bioelectrical impedance analyzers for ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1546499/full]
- 21. Association between bioelectrical impedance analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392491/]
- 22. Bioelectrical impedance analysis for measuring body ... [https://pubmed.ncbi.nlm.nih.gov/40241085/]
- 23. Body composition measures assessed by bioelectrical ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1689031/full]
- 24. Bioelectrical Impedance Analysis in Professional and Semi ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568126/]
- 25. High-standard predictive equations for estimating body ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05272-x]
- 26. Raw bioelectrical impedance parameters as informative ... [https://www.sciencedirect.com/science/article/pii/S0261561425001724]
- 27. Comparison of Bioelectrical Impedance Analysis (BIA) [https://www.mdpi.com/2075-1729/14/1/27]
- 28. Bioelectrical Impedance Analysis (BIA) [https://www.scienceforsport.com/bioelectrical-impedance-analysis-bia/?srsltid=AfmBOop8hV-J5M5mR7J9QbCo-Nr2HnRlH4D7EemKnx3YVVoleoI5A2xD]
- 29. Discrepancies between leg-to-leg bioelectrical Impedance ... [https://www.nature.com/articles/s41598-017-08991-y]
- 30. Assessing the reliability and cross-sectional and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10404482/]
- 31. Development of a Segmental Bioelectrical Impedance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6891272/]
- 32. A Comprehensive Guide to Bioelectrical Impedance ... [https://www.habdirect.com/a-comprehensive-guide-to-bioelectrical-impedance-analysis-bia/]
- 33. The Theory and Fundamentals of Bioimpedance Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4118362/]
- 34. Validity of Body Composition Estimates in Women ... [https://www.mdpi.com/1424-8220/25/16/5037]
- 35. Bioelectrical Impedance Analysis in Professional and Semi ... [https://www.mdpi.com/2075-4663/13/10/348]
- 36. Bioelectrical Impedance Vector Analysis (BIVA) in Sports ... [https://www.sciencedirect.com/science/article/pii/S1452398125002986]
- 37. Monitoring Intestinal Organoid–Derived Monolayer Barrier ... [https://en.bio-protocol.org/en/bpdetail?id=4947&type=0]
- 38. Bioelectrical Impedance Analysis (BIA) for the Assessment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10675768/]
- 39. Investigating the association of bioelectrical impedance ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1662484/full]
- 40. Evolution of research trends and emerging hotspots in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203698/]
- 41. Application of Bioelectrical Impedance Analysis in ... [https://pubmed.ncbi.nlm.nih.gov/37764725/]
- 42. Editorial: Body composition assessment and future disease ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1617729/full]
- 43. New Bioelectrical Impedance-Based Equations to Estimate ... [https://www.mdpi.com/2409-9279/8/3/53]
- 44. A practical guide to bioelectrical impedance analysis using the ... [https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-10-35]
- 45. Cellular Impedance Biosensors for Drug Screening and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3205117/]
- 46. Bioelectrical Impedance Analysis (BIA) [https://www.scienceforsport.com/bioelectrical-impedance-analysis-bia/?srsltid=AfmBOoo8etaPsRlsOGYasw5Q0zGNqiASM91zBe0cZCdDNPW0R_B-6QtM]
- 47. High-Throughput 96-Well Nanogroove-Enhanced Electrical ... [https://pubmed.ncbi.nlm.nih.gov/40534247/]
- 48. A Review of Advanced Impedance Biosensors with ... [https://www.mdpi.com/2079-6374/11/11/412]
- 49. The impact of hydration and fluid distribution on pulmonary... status [https://www.nature.com/articles/s41598-022-05192-0?error=cookies_not_supported&code=f9e188bf-0ffd-452e-a50b-662f9551dbde]
- 50. Non-invasive technology to assess hydration in advanced... status [https://pubmed.ncbi.nlm.nih.gov/39160544/]
- 51. Consuming a low-calorie amount of routine food and drink ... [https://www.sciencedirect.com/science/article/abs/pii/S0899900721002884]
- 52. The effects of eating frequency on changes in body ... [https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-023-01532-z]
- 53. Exercise improves body composition, physical fitness, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11735414/]
- 54. The effects and post-exercise energy metabolism ... [https://www.nature.com/articles/s41598-025-98590-z]
- 55. Effects of resistance training with and without post-exercise ... [https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-025-01256-6]
- 56. Methodological standards for body composition—an expert ... [https://www.sciencedirect.com/science/article/pii/S0002916525002771]
- 57. Validation of anthropometric and bioelectrical impedance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587244/]
- 58. Development and validation of new bioimpedance ... [https://www.sciencedirect.com/science/article/abs/pii/S2405457725003717]
- 59. Bioelectrical impedance analysis of bone mineral content ... [https://www.nature.com/articles/s41598-025-08304-8]
- 60. Development and cross-validation of predictive equations ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1499752/full]
- 61. Development and validation of new bioimpedance ... [https://pubmed.ncbi.nlm.nih.gov/40523473/]
- 62. Bioelectrical Impedance Analysis (BIA) [https://www.scienceforsport.com/bioelectrical-impedance-analysis-bia/]
- 63. Bioelectrical impedance vector analysis (BIVA) in sport and exercise: Systematic review and future perspectives | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197957]
- 64. Use of bioelectrical impedance analysis measurements as an evaluation for participating in sports - PubMed [https://pubmed.ncbi.nlm.nih.gov/8780365/]
- 65. Bioelectrical Impedance Analysis as a Helpful Tool in ... [https://www.mdpi.com/2571-841X/8/1/15]
- 66. Limitations and validation of bioelectrical impedance ... [https://pubmed.ncbi.nlm.nih.gov/15809537/]
- 67. Body composition during growth in children: limitations and ... [https://pubmed.ncbi.nlm.nih.gov/26039314/]
- 68. Exploring Bio-Impedance Sensing for Intelligent Wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109311/]
- 69. Bioelectrical impedance vector analysis in older adults [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1640407/full]
- 70. Bioelectrical Impedance Analysis: BIA Measurement and ... [https://www.withings.com/us/en/health-insights/about-bioelectrical-impedance-analysis?srsltid=AfmBOoq66K50xNGxbj16fKOuAFlBq1QN7Wyr1kd_Nrkl8A9XqNBhimaE]
- 71. Exploratory approach to speculate on body composition ... [https://www.nature.com/articles/s41598-025-20293-2]
- 72. DEXA Scan for Body Composition: Best Method in 2025 [https://revolutionhealth.org/blogs/news/dexa-for-body-composition-in-2025]
- 73. Dual-Energy X-Ray Absorptiometry - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK519042/]
- 74. Visual body composition assessment methods: A 4- ... [https://www.sciencedirect.com/science/article/abs/pii/S0261561422003491]
- 75. Accuracy and Reliability of Assessing Lateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5370193/]
- 76. Fat and fat‐free mass measurement agreement by dual‐ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10928253/]
- 77. High agreement between lean mass assessed by Dual ... [https://www.medrxiv.org/content/10.1101/2025.02.03.25321573v2.full-text]
- 78. Comparison of body composition assessment by DXA and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6042744/]
- 79. Comparison of body composition assessment by DXA and BIA ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0200465]
- 80. A comparative analysis of body composition assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9715747/]
- 81. Bioelectrical Impedance Analysis Versus Dual X-Ray ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192207/]
- 82. Comparison of whole body bone mineral density ... [https://www.nature.com/articles/s41598-024-80721-7]
- 83. Development and validation of a phase-sensitive ... [https://pubmed.ncbi.nlm.nih.gov/40903338/]
- 84. Agreement Between Six Bioelectrical Impedance Analysis ... [https://www.journalofexerciseandnutrition.com/index.php/JEN/article/view/206]
- 85. Relative validity of bioelectrical impedance analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11836777/]
- 86. Accuracy of bioimpedance equations for measuring body ... [https://www.sciencedirect.com/science/article/abs/pii/S026156142200276X]
- 87. Bioelectrical Impedance Analysis Overestimates Fat-Free ... [https://pubmed.ncbi.nlm.nih.gov/31769074/]
- 88. Development and Validation of Bioelectrical Impedance ... [https://www.sciencedirect.com/science/article/pii/S0022316622166769]
- 89. Fat-free mass prediction equations for bioelectric impedance ... [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-015-0476-7]
- 90. Agreement between equation‐derived body fat estimator and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11492144/]
- 91. Sensitivity, Specificity, Receiver-Operating Characteristic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556590/]
- 92. Performance of bioelectrical impedance analysis ... [https://www.nature.com/articles/s41598-022-05887-4]
- 93. Bland-Altman plot - MedCalc Statistical Software Manual [https://www.medcalc.org/en/manual/bland-altman-plot.php]
- 94. Bland-Altman Plot [https://real-statistics.com/reliability/interrater-reliability/bland-altman-analysis/bland-altman-plot/]
- 95. Interpreting results: Bland-Altman [https://www.graphpad.com/guides/prism/latest/statistics/bland-altman_results.htm]
- 96. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10576075/]
- 97. Validity of bioelectrical impedance analysis in estimation ... [https://www.sciencedirect.com/science/article/pii/S0261561416313693]
- 98. Bioelectrical impedance vector analysis evaluates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7772738/]
- 99. as an indicator of nutritional status: a cross-sectional... Phase angle [https://jhpn.biomedcentral.com/articles/10.1186/s41043-025-01060-5]
- 100. Frontiers | Association between phase and ECW/TBW ratio with... angle [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1638075/full]
- 101. Usefulness of the Phase in Evaluating Locomotive Syndrome in... Angle [https://pubmed.ncbi.nlm.nih.gov/40507742/]
- 102. New bioelectrical impedance vector references and phase ... [https://www.sciencedirect.com/science/article/pii/S0261561423002510]