Cerebral Ischemia Unraveled
How Brain Slices Are Revolutionizing Stroke Research
The Silent Storm in the Brain
Imagine your brain as a bustling city with an intricate network of streets and communication systems. Now imagine what happens when the power grid suddenly fails—lights flicker, communication towers go silent, and transportation grinds to a halt. This is what happens during cerebral ischemia, a condition where blood flow to the brain is disrupted, starving brain cells of oxygen and nutrients. Every year, millions of people worldwide experience this biological power outage in the form of ischemic strokes, which account for approximately 70-80% of all stroke cases 2 .
Did You Know?
Ischemic strokes account for approximately 87% of all stroke cases, making them the most common type of stroke.
For decades, scientists struggled to understand the complex cascade of events that occurs during cerebral ischemia. Studying these processes in living brains presented enormous challenges—the brain's protected location inside the skull, its incredible complexity, and the ethical limitations of human research all created barriers to discovery. This is where an ingenious laboratory model has revolutionized our understanding: in vitro brain slice preparations. These remarkable thin sections of brain tissue, kept alive in laboratory dishes, have become windows through which researchers can observe the intricate drama of cerebral ischemia unfold at the cellular level 1 4 .
From Stroke to Cellular Chaos
What Happens When the Brain's Blood Supply Fails?
Cerebral ischemia occurs when blood flow to part of the brain is interrupted, typically due to a clot blocking a blood vessel. Within seconds, the affected brain region begins to starve. Neurons—the brain's information-processing cells—are especially vulnerable to oxygen deprivation. Without oxygen, they cannot produce adenosine triphosphate (ATP), the energy currency that powers virtually all cellular processes 1 9 .
- Ion balance collapse: Energy-dependent pumps fail, causing potassium to leak out and calcium to flood into cells 1 4
- Glutamate excitotoxicity: Massive amounts of glutamate are released, overstimulating neurons 2 4
- Cellular swelling: Loss of ion balance leads to water rushing into cells
- Inflammatory activation: Immune response launches, sometimes causing more harm 2 9
What makes cerebral ischemia particularly insidious is that even when blood flow is restored—a process called reperfusion—the damage often continues. This paradoxical phenomenon, known as ischemia-reperfusion injury, involves a burst of oxidative stress and inflammation that can exacerbate the initial injury 2 .
Windows into the Ischemic Brain
The Laboratory Miracle That Revolutionized Neuroscience
How do researchers study these complex processes? Enter in vitro brain slice preparations—an elegant experimental model that has transformed our understanding of cerebral ischemia. Typically harvested from rodents, these thin (200-400 micrometer) sections of brain tissue are maintained alive in specialized chambers that provide oxygen and nutrients 1 3 .
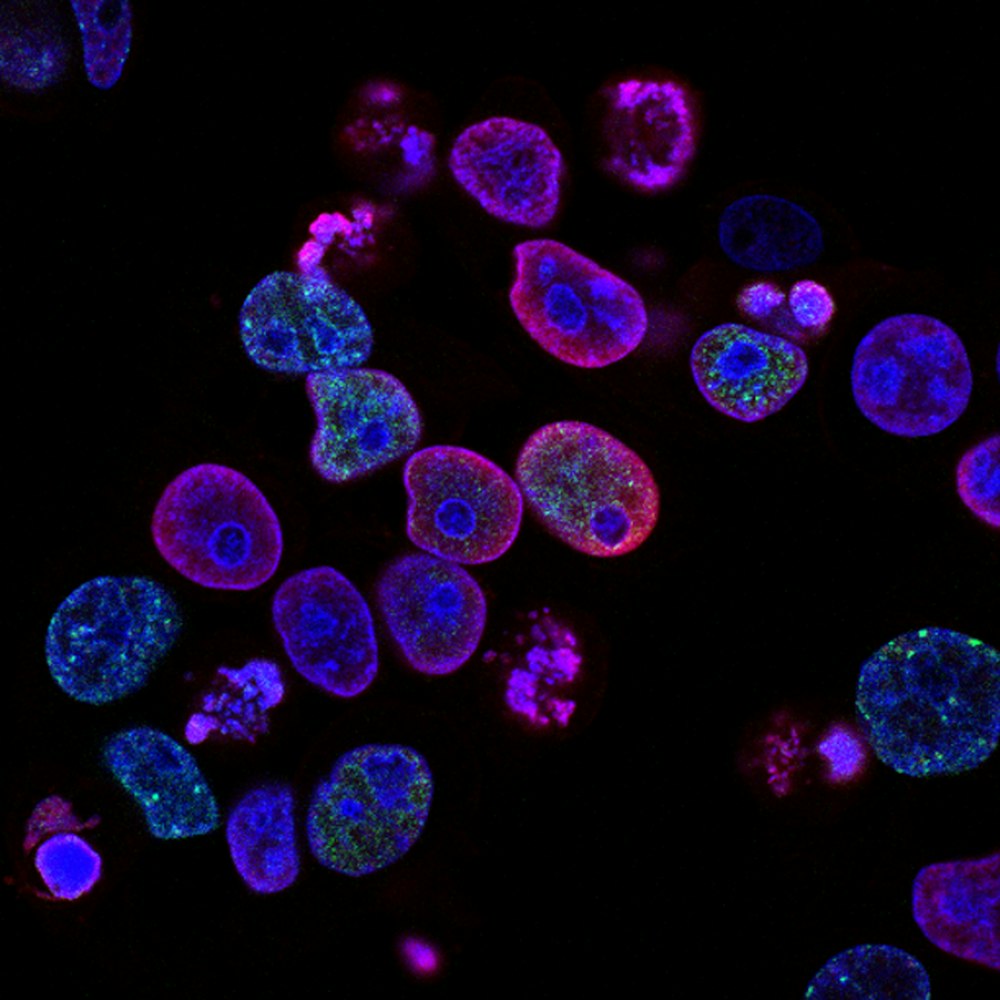
The beauty of this model lies in its balance of complexity and controllability. Unlike isolated cells in a dish, brain slices preserve much of the brain's three-dimensional architecture and many of the connections between different cell types. Neurons, astrocytes, microglia, and other brain cells continue to interact much as they would in an intact brain 3 . At the same time, researchers have precise control over the slice's environment—they can precisely manipulate oxygen and glucose levels, add drugs or protective compounds, and directly monitor cellular responses with unprecedented clarity 1 4 .

| Advantage | Description | Research Benefit |
|---|---|---|
| Preserved architecture | Maintains cellular organization and connections of living brain tissue | Allows study of cell-to-cell interactions and network effects |
| Environmental control | Precise manipulation of oxygen, glucose, and drug concentrations | Enables isolation of specific mechanisms and pathways |
| Direct observation | Cellular responses can be visualized in real-time using imaging techniques | Provides dynamic view of ischemic processes as they unfold |
| High-throughput potential | Multiple slices can be prepared from a single brain and tested in parallel | Accelerates research pace and drug screening capabilities |
| Reduced animal use | One animal provides tissue for multiple experiments | Addresses ethical concerns and reduces research costs |
Unveiling Ischemia's Secrets Through Hippocampal Slices
Methodology: Simulating Ischemia in the Laboratory
One of the most informative uses of brain slice technology has been the study of ischemia in the hippocampus—a brain region critical for memory formation and exceptionally vulnerable to ischemic damage 1 4 . Let's walk through a typical experiment that has yielded crucial insights into cerebral ischemia:
Slice Preparation
Researchers remove the brain from an anesthetized rat or mouse and rapidly dissect out the hippocampus. Using a precise cutting instrument called a vibratome, they slice the tissue into thin sections.
Simulating Ischemia
To simulate ischemia, researchers replace the normal artificial cerebrospinal fluid (aCSF) with a solution lacking both oxygen and glucose.
Monitoring Responses
Using electrodes placed directly onto neurons, researchers can record electrical activity before, during, and after the simulated ischemia.
Results and Analysis: The Ischemic Cascade Unmasked
Through countless iterations of this basic experiment, researchers have pieced together the detailed sequence of events that occurs during cerebral ischemia:
Energy failure (within minutes)
ATP levels plummet as oxygen and glucose are deprived.
Ion gradient collapse
The sodium-potassium pump fails, leading to membrane depolarization.
Glutamate release
Massive amounts of glutamate are released, overactivating NMDA and AMPA receptors.
Calcium overload
Calcium floods into neurons, activating destructive enzymes.
Oxidative stress
Restoration of oxygen (reperfusion) generates an explosion of damaging free radicals.
Protective Strategies: Insights from Intervention Studies
Brain slice studies have been invaluable for testing potential protective strategies against ischemic damage. For example:
| Intervention Category | Example Compounds | Mechanism of Action | Protective Effect |
|---|---|---|---|
| Glutamate antagonists | MK-801, AP5 | Block NMDA receptors, reduce excitotoxicity | 40-60% reduction in neuronal death |
| Calcium blockers | Nimodipine, Verapamil | Inhibit calcium influx, prevent calcium overload | 25-50% protection, depending on timing |
| Antioxidants | Vitamin E, Edaravone | Scavenge free radicals, reduce oxidative stress | 30-55% reduction in lipid peroxidation |
| Anti-inflammatories | Minocycline, IL-1RA | Modulate immune response, reduce inflammation | 35-65% protection, especially in reperfusion |
| Combination therapies | Caffeine + melatonin | Multiple targets, synergistic effects | 50-75% protection, most promising approach |
The Tools for Discovery
The incredible insights gained from brain slice studies depend on a sophisticated toolkit of research reagents and technologies. Here are some of the essential components that make this research possible:
| Reagent/Category | Specific Examples | Function in Research |
|---|---|---|
| Slice maintenance solutions | Artificial CSF, choline-based slicing solution | Maintain tissue viability, reduce slicing damage |
| Viability indicators | Propidium iodide, MTT assay | Assess cell death and metabolic function |
| Ion indicators | Fura-2 (calcium), SBFI (sodium) | Measure intracellular ion concentrations |
| Electrical recording | Patch-clamp electrodes, multi-electrode arrays | Monitor neuronal activity and connectivity |
| Oxygen-glucose deprivation systems | Nitrogen chambers, glucose-free media | Simulate ischemic conditions in controlled manner |
| Genetic tools | Viral vectors, transgenic animals | Manipulate gene expression in specific cell types |
Beyond the Slice: Future Directions and Implications
From Rodents to Humans: The Challenge of Translation
While rodent brain slices have provided invaluable insights, researchers must always consider the crucial differences between rodent and human brains. Approximately 70 million years of evolution separate humans from rodents, resulting in significant differences in gene expression, immune signaling, and brain organization 7 . These differences may explain why many neuroprotective compounds that showed promise in rodent studies have failed in human clinical trials.
Therapeutic Testing
Brain slice models have become valuable platforms for drug screening and therapeutic testing. For example, researchers can test whether a compound can protect against ischemic damage or enhance recovery after simulated ischemia.
Personalized Medicine
The combination of brain slice models with induced pluripotent stem cell (iPSC) technology may open new avenues for personalized medicine. Researchers could potentially create brain organoids from individual patients.
Small Slices, Big Insights
In vitro brain slice preparations may seem like a humble scientific tool, but they have revolutionized our understanding of cerebral ischemia. By providing a window into the complex cellular and molecular events that occur during ischemic injury, these thin sections of brain tissue have helped researchers identify potential therapeutic targets and test promising intervention strategies.
Research Impact
Brain slice models have contributed to over 10,000 scientific publications on cerebral ischemia, dramatically advancing our understanding of stroke mechanisms.
Though challenges remain—particularly in translating findings from rodents to humans—the continued refinement of brain slice technologies offers hope for future breakthroughs. As we refine our ability to maintain human brain tissue in the laboratory and develop more sophisticated monitoring techniques, these preparations will continue to yield insights into one of medicine's most devastating conditions.
The silent storm of cerebral ischemia may always be a formidable foe, but thanks to these remarkable laboratory models, we are better equipped than ever to understand its mechanisms and develop strategies to protect the brain from its devastating effects.