ELISA for Soluble Enzyme Biomarkers in Plasma: A Complete Guide for Precision Detection in Research & Drug Development
This comprehensive guide explores the critical application of ELISA (Enzyme-Linked Immunosorbent Assay) for detecting soluble enzyme biomarkers in plasma, a cornerstone technique in translational research and therapeutic development.
ELISA for Soluble Enzyme Biomarkers in Plasma: A Complete Guide for Precision Detection in Research & Drug Development
Abstract
This comprehensive guide explores the critical application of ELISA (Enzyme-Linked Immunosorbent Assay) for detecting soluble enzyme biomarkers in plasma, a cornerstone technique in translational research and therapeutic development. Covering foundational principles, we detail optimized methodologies for robust assay execution, from sample preparation to data analysis. The article provides systematic troubleshooting strategies for common pitfalls and delves into rigorous validation frameworks and comparative analyses with emerging technologies. Designed for researchers and drug development professionals, this resource equips readers with the knowledge to implement reliable, high-quality biomarker assays that generate actionable data for disease research, diagnostics, and preclinical/clinical studies.
Understanding Soluble Enzyme Biomarkers: Why Plasma ELISA is a Gold Standard in Biomedical Research
Within plasma-based research, soluble enzyme biomarkers represent a critical class of analytes. These are enzymes, typically released from tissues via secretion or as a result of cellular injury, that circulate in biofluids and whose quantitative levels provide insights into physiological processes, disease states, and pharmacological interventions. This application note, framed within a broader thesis on ELISA-based detection, details the roles, detection strategies, and experimental protocols for these dynamic biomarkers.
Roles of Soluble Enzyme Biomarkers
- Physiology: Reflective of normal turnover and metabolic activity (e.g., circulating Lipoprotein Lipase in lipid metabolism).
- Pathophysiology: Indicators of tissue-specific damage, inflammation, or dysregulated proteolysis (e.g., Matrix Metalloproteinase-9 in cancer metastasis and cardiovascular rupture).
- Drug Response: Pharmacodynamic (PD) markers for assessing target engagement, efficacy, and mechanism-based toxicity (e.g., Angiotensin-Converting Enzyme levels following ACE inhibitor therapy).
Key Soluble Enzyme Biomarkers: Functions and Disease Associations
Table 1: Exemplar Soluble Enzyme Biomarkers in Plasma Research
| Biomarker | Primary Physiological Role | Pathophysiological Association | Drug Response Context |
|---|---|---|---|
| Matrix Metalloproteinase-9 (MMP-9) | Extracellular matrix (ECM) remodeling, wound healing. | Atherosclerotic plaque instability, cancer metastasis, inflammatory diseases. | Monitor efficacy of MMP inhibitors in oncology trials. |
| Neutrophil Elastase (NE) | Microbial killing, innate immune response. | Chronic obstructive pulmonary disease (COPD), cystic fibrosis, acute lung injury. | PD marker for NE inhibitor therapies (e.g., alpha-1 antitrypsin augmentation). |
| Angiotensin-Converting Enzyme (ACE) | Regulates blood pressure via renin-angiotensin system (RAS). | Sarcoidosis (diagnostic marker), cardiovascular disease. | Target engagement marker for ACE inhibitor drugs. |
| Dipeptidyl Peptidase-4 (DPP-4) | Inactivation of incretin hormones (GLP-1, GIP). | Type 2 diabetes, immune regulation. | Soluble DPP-4 levels may correlate with DPP-4 inhibitor (gliptin) efficacy. |
| Autotaxin (ATX; ENPP2) | Generation of lysophosphatidic acid (LPA), cell signaling. | Fibrotic diseases (NAFLD, IPF), cancer progression. | Emerging target for ATX inhibitors in fibrosis. |
Experimental Protocols
Protocol 1: Quantitative Detection of Human MMP-9 in Plasma via Sandwich ELISA
- Principle: A capture antibody specific to MMP-9 is coated onto a microplate. Plasma samples are added, and MMP-9 is bound. A detection antibody, conjugated to horseradish peroxidase (HRP), forms a sandwich complex. Signal is generated with TMB substrate.
- Detailed Methodology:
- Coating: Dilute anti-human MMP-9 monoclonal antibody to 2 µg/mL in carbonate-bicarbonate coating buffer (pH 9.6). Add 100 µL/well to a 96-well plate. Seal and incubate overnight at 4°C.
- Washing & Blocking: Aspirate and wash wells 3x with 300 µL PBS containing 0.05% Tween-20 (PBST). Block with 200 µL/well of 3% BSA in PBS for 2 hours at room temperature (RT). Wash 3x with PBST.
- Sample & Standard Incubation: Prepare recombinant MMP-9 standards in dilution buffer (1% BSA in PBST) ranging from 15.6 pg/mL to 1000 pg/mL. Dilute EDTA-plasma samples 1:10 in dilution buffer. Add 100 µL of standard or sample per well in duplicate. Incubate for 2 hours at RT with gentle shaking. Wash 5x with PBST.
- Detection Antibody Incubation: Add 100 µL/well of biotinylated anti-MMP-9 detection antibody (0.5 µg/mL in dilution buffer). Incubate 1 hour at RT. Wash 5x with PBST.
- Streptavidin-HRP Incubation: Add 100 µL/well of streptavidin-HRP conjugate (1:5000 dilution in dilution buffer). Incubate 30 minutes at RT, protected from light. Wash 7x with PBST.
- Signal Development: Add 100 µL/well of TMB substrate solution. Incubate for 15-20 minutes at RT until color develops.
- Reaction Stop & Reading: Add 50 µL/well of 2N H₂SO₄ stop solution. Measure absorbance immediately at 450 nm with 570 nm or 620 nm wavelength correction.
- Analysis: Generate a 4-parameter logistic (4PL) standard curve. Interpolate sample concentrations, applying the dilution factor.
Protocol 2: Pharmacodynamic Assessment of DPP-4 Inhibition via Plasma Activity Assay
- Principle: A fluorogenic substrate (e.g., H-Gly-Pro-AMC) is cleaved by active DPP-4 in plasma, releasing a fluorescent product. The rate of fluorescence increase is proportional to enzyme activity and can be inhibited by pre-treatment with DPP-4 inhibitor drugs.
- Detailed Methodology:
- Sample Preparation: Collect plasma in EDTA tubes from subjects pre-dose and at specified times post-dose of a DPP-4 inhibitor. Centrifuge and aliquot immediately; store at -80°C.
- Reaction Setup: In a black 96-well plate, combine 10 µL of plasma (diluted 1:5 in assay buffer) with 70 µL of assay buffer (50 mM Tris-HCl, pH 7.5). Include negative control wells with buffer only and positive control wells with known active plasma.
- Inhibition Control (Optional): Pre-incubate a separate aliquot of a control plasma sample with 10 µM sitagliptin for 30 minutes at RT to confirm specificity.
- Kinetic Measurement: Initiate the reaction by adding 20 µL of 500 µM fluorogenic substrate (final concentration 100 µM). Mix immediately by gentle plate shaking.
- Reading: Immediately measure fluorescence (excitation 360 nm, emission 460 nm) kinetically every minute for 30-60 minutes at 37°C using a plate reader.
- Analysis: Calculate the slope (Vmax) of the linear increase in fluorescence for each well. Express DPP-4 activity as relative fluorescence units (RFU) per minute per µL of plasma. Percent inhibition is calculated relative to pre-dose sample activity.
Visualizations
MMP-9 Signaling in Pathophysiology
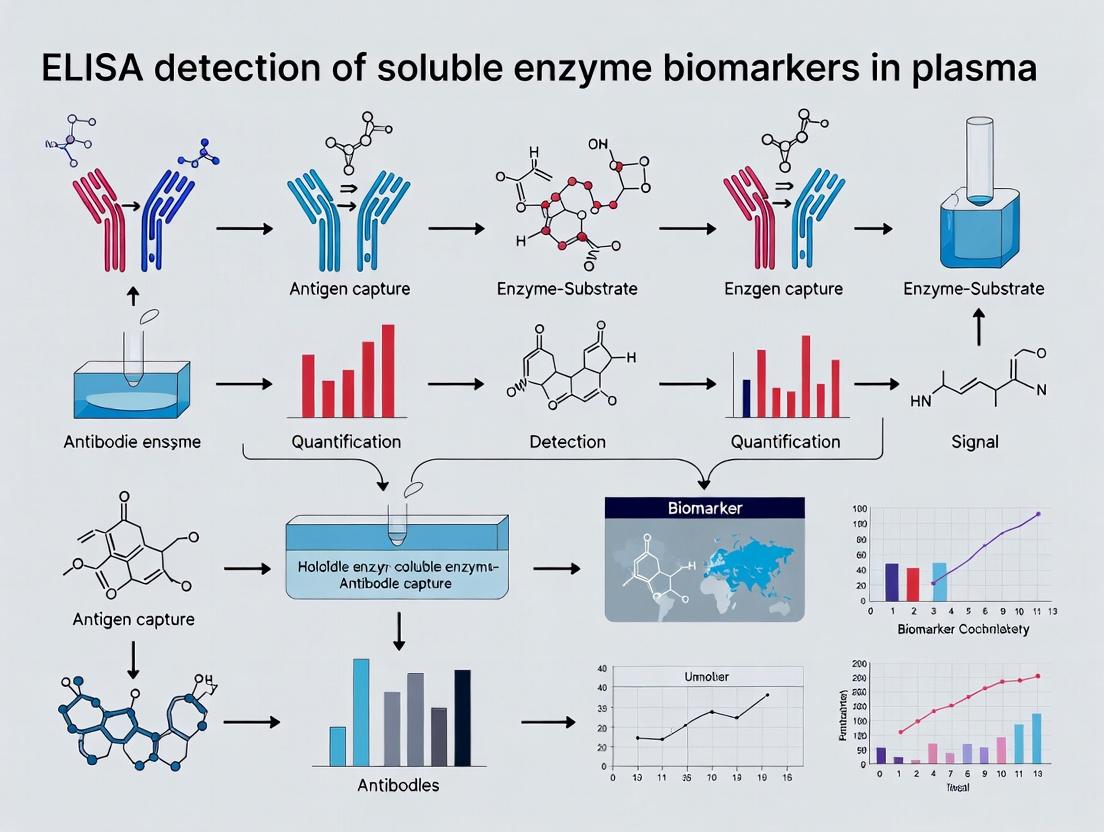
ELISA-Based Biomarker Study Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Soluble Enzyme Biomarker ELISA Research
| Item | Function / Relevance |
|---|---|
| High-Affinity Matched Antibody Pairs (Capture/Detection) | Critical for specific, sensitive sandwich ELISA development. Antibodies must recognize non-overlapping epitopes on the soluble enzyme. |
| Recombinant Enzyme Protein Standard | Quantification benchmark. Must be pure, active, and identical to the endogenous target for accurate standard curve generation. |
| Stable, Sensitive Detection System (e.g., HRP-Streptavidin + TMB) | Amplifies signal from the captured biomarker. Sensitivity is paramount for detecting low-abundance enzymes in plasma. |
| Matrix-Matched Assay Buffer (e.g., 1% BSA in PBST) | Diluent for standards and samples; reduces non-specific background by mimicking plasma protein composition. |
| Validated Plasma Collection Tubes (e.g., EDTA) | Prevents coagulation and preserves enzyme stability. Critical for pre-analytical consistency. |
| Fluorogenic Activity Assay Kits (for functional biomarkers) | Enables measurement of enzymatic activity as a direct PD readout, complementing immunodetection of antigen mass. |
| Plate Reader (Absorbance & Fluorescence) | Essential instrumentation for quantitative readout of both colorimetric (ELISA) and kinetic activity assays. |
Plasma is the acellular, liquid fraction of blood, obtained by centrifugation with an anticoagulant. Its unique composition offers distinct advantages for biomarker research within ELISA-based detection frameworks. The following tables summarize key quantitative data supporting its utility.
Table 1: Comparative Analysis of Blood-Derived Matrices for Biomarker Assays
| Matrix | Key Components | Sample Preparation | Stability Concerns | Typical Yield per Draw | Relative Interference in ELISA |
|---|---|---|---|---|---|
| Plasma | Soluble proteins, electrolytes, hormones, clotting factors (inactive) | Centrifugation post-anticoagulation | Protease activity (if not inhibited) | ~2.5 mL from 5 mL blood | Low-Medium (fibrin strands can form) |
| Serum | Soluble proteins, electrolytes, hormones, released platelet factors | Clot formation & retraction | Platelet degranulation, variable clotting time | ~2.2 mL from 5 mL blood | Medium-High (heterophilic Abs, variable composition) |
| Whole Blood | Cells, platelets, plasma | Direct lysis or fixation | Hemolysis, rapid RNA/protein degradation | N/A | Very High (cellular contents) |
Table 2: Clinical Relevance Metrics for Plasma Biomarkers in Common Diseases (Recent Meta-Analysis Data)
| Biomarker | Target Disease/Condition | Typical Plasma Conc. (Healthy) | Typical Plasma Conc. (Disease) | Correlation with Serum (R²) | Key Advantage in Plasma |
|---|---|---|---|---|---|
| Troponin I | Myocardial Infarction | < 0.04 ng/mL | > 0.4 ng/mL (acute) | 0.92 | Standardized collection; avoids platelet release artifacts. |
| C-Reactive Protein (hs) | Chronic Inflammation | 1-3 mg/L | 3-100+ mg/L | 0.98 | Stable with proper protease inhibition; reflects real-time state. |
| Neurofilament Light Chain (NfL) | Neurodegeneration | < 10 pg/mL | > 20 pg/mL | 0.85 | Strong correlation with CSF levels; accessible for longitudinal study. |
| CA-125 | Ovarian Cancer | < 35 U/mL | > 35 U/mL | 0.95 | Consistent pre-analytical variables vs. serum. |
| Chitinase-3-like-1 (YKL-40) | Fibrosis, Cancer | 20-100 ng/mL | 100-1000+ ng/mL | 0.90 | Reduced in vitro release from platelets vs. serum. |
Detailed Experimental Protocols
Protocol 1: Standardized Plasma Collection and Processing for Soluble Enzyme Biomarker ELISA
Objective: To obtain high-quality, reproducible plasma samples for the detection of soluble enzyme biomarkers (e.g., MMP-9, PSA, soluble ACE2), minimizing pre-analytical variability.
Materials: See "The Scientist's Toolkit" (Section 4).
Procedure:
- Venipuncture: Draw blood into pre-chilled vacuum tubes containing K2EDTA anticoagulant. Invert gently 8-10 times immediately.
- Transport: Keep tubes upright and maintain at 4°C. Process within 1 hour of collection for most soluble enzyme biomarkers.
- Centrifugation: Spin tubes at 1,500-2,000 x g for 15 minutes at 4°C. Use a swinging-bucket rotor for a defined plasma-platelet interface.
- Plasma Aliquotting: Using a sterile pipette, carefully aspirate the upper plasma layer, avoiding the buffy coat (white cells) and platelet layer. Transfer to a fresh polypropylene tube.
- Secondary Clearance Centrifugation (Critical for Platelet-Derived Factors): To remove residual platelets, perform a second high-speed spin of the aspirated plasma at 10,000 x g for 10 minutes at 4°C.
- Aliquot and Store: Immediately aliquot the cleared plasma into small-volume cryovials to avoid freeze-thaw cycles. Flash-freeze in liquid nitrogen or a dry-ice/ethanol bath. Store at -80°C.
Notes: For protease analysis (e.g., thrombin, kallikreins), consider specific cocktail inhibitors (e.g., AEBSF, Aprotinin) added immediately post-draw. Heparin tubes can interfere with some immunoassays.
Protocol 2: ELISA for Soluble Enzyme Biomarker in Processed Plasma
Objective: Quantify a specific soluble enzyme biomarker (e.g., soluble Dipeptidyl Peptidase-4, sDPP4) in processed plasma samples.
Materials: Commercial sDPP4 ELISA Kit (matched antibody pair), processed plasma samples, microplate washer/reader.
Procedure:
- Sample Thawing & Dilution: Thaw plasma aliquots on ice. Dilute samples 1:20 in the kit's provided sample diluent (typically PBS with a protein base). Note: Optimal dilution must be determined via pilot assay.
- Plate Preparation: Coat a 96-well microplate with 100 µL/well of capture antibody (anti-sDPP4) in coating buffer. Seal and incubate overnight at 4°C.
- Washing & Blocking: Wash plate 3x with Wash Buffer (0.05% Tween-20 in PBS). Block with 300 µL/well of blocking buffer (1% BSA in PBS) for 1 hour at room temperature (RT). Wash 3x.
- Standards & Sample Incubation: Prepare a standard curve from the recombinant sDPP4 standard (e.g., 0-10 ng/mL). Add 100 µL of standards and diluted samples per well in duplicate. Incubate for 2 hours at RT or 1 hour at 37°C. Wash 5x.
- Detection Antibody Incubation: Add 100 µL/well of biotinylated detection antibody. Incubate for 1 hour at RT. Wash 5x.
- Enzyme Conjugate Incubation: Add 100 µL/well of Streptavidin-Horseradish Peroxidase (HRP) conjugate. Incubate for 30 minutes at RT in the dark. Wash 7x thoroughly.
- Substrate Development & Stop: Add 100 µL/well of TMB substrate. Incubate for 15-30 minutes at RT in the dark. Stop the reaction with 50 µL/well of 2N H2SO4.
- Readout: Measure absorbance immediately at 450 nm with a 570 nm or 620 nm reference wavelength.
- Data Analysis: Generate a standard curve (4-parameter logistic fit) and interpolate sample concentrations. Apply the dilution factor.
Visualizations
Diagram Title: Standardized Plasma Processing Workflow for ELISA
Diagram Title: Plasma vs. Serum Generation Pathways
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Plasma Biomarker ELISA Research
| Item Name | Supplier Examples | Primary Function in Protocol | Critical Notes |
|---|---|---|---|
| K2EDTA Vacutainer Tubes | BD, Greiner Bio-One | Prevents coagulation by chelating Ca²⁺. Standard for plasma proteomics. | Preferred over heparin for downstream immunoassays; ensures consistent volume. |
| Protease Inhibitor Cocktail (PIC) | Roche, Sigma-Aldrich | Broad-spectrum inhibition of serine, cysteine, metalloproteases. Preserves biomarker integrity. | Add immediately post-draw for labile enzymes. Choose EDTA-free PIC if measuring metalloenzymes. |
| Cryogenic Vials (Polypropylene) | Corning, Thermo Fisher | Long-term storage of plasma aliquots at -80°C. Prevents sample degradation and limits freeze-thaw cycles. | Use internally-threaded vials for leak prevention. |
| Matched Antibody Pair ELISA Kit | R&D Systems, Abcam, Thermo Fisher | Provides optimized, validated capture/detection antibodies and standards for specific soluble targets. | Verify kit is validated for plasma (not just serum) to ensure matrix compatibility. |
| Recombinant Biomarker Protein Standard | PeproTech, Sino Biological | Creates the standard curve for absolute quantification in the ELISA. | Must be identical to the endogenous target for accurate interpolation. |
| Streptavidin-HRP Conjugate | Jackson ImmunoResearch, Vector Labs | High-affinity binding to biotinylated detection antibody, enabling enzymatic signal amplification. | Titer concentration to optimize signal-to-noise. |
| TMB (3,3',5,5'-Tetramethylbenzidine) Substrate | Moss, Bio-Rad | Chromogenic HRP substrate. Turns blue upon oxidation, yellow when stopped with acid. | Light-sensitive; use within specified timeframe after preparation. |
Within the context of a thesis on the detection of soluble enzyme biomarkers in plasma for drug development and clinical research, the Enzyme-Linked Immunosorbent Assay (ELISA) remains a cornerstone technology. Its power derives from the exquisite specificity of antibody-antigen interactions coupled with enzymatic signal amplification, enabling the precise quantification of low-abundance analytes in complex biological matrices like plasma. The accurate measurement of biomarkers such as matrix metalloproteinases (MMPs), neutrophil elastase, or various kinases is critical for understanding disease pathogenesis, monitoring therapeutic response, and identifying new drug targets.
Recent advancements in ELISA technology focus on improving sensitivity, multiplexing capability, and automation to meet the demands of high-throughput biomarker validation studies. The core principles, however, remain unchanged and form the foundation of robust and reproducible assay development.
Key Research Reagent Solutions
The following table details essential materials for developing a sandwich ELISA for soluble enzyme biomarkers in plasma.
| Reagent / Material | Function & Critical Notes |
|---|---|
| High-Affinity Matched Antibody Pair | A capture antibody (often monoclonal) specific to the target biomarker and a detection antibody (monoclonal or polyclonal) targeting a different epitope. Critical for specificity and sensitivity. |
| Recombinant Purified Antigen Standard | Precisely quantified protein used to generate the standard curve. Must be identical to the native biomarker for accurate quantification. |
| Blocking Buffer (e.g., 5% BSA/PBS) | Prevents non-specific binding of antibodies or plasma proteins to the coated plate, reducing background signal. |
| Plasma Sample Diluent | Optimized buffer (often containing additional protein and detergents) to maintain analyte stability and minimize matrix interference. |
| HRP or AP-Conjugated Secondary Antibody | Enzyme-linked antibody that binds the detection antibody. Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP) are common for colorimetric, chemiluminescent, or fluorescent detection. |
| High-Sensitivity Chemiluminescent Substrate | Provides amplified signal upon enzymatic conversion, offering a wider dynamic range and lower limit of detection than colorimetric substrates. |
| Low-Binding, High-Protein-Binding Capacity Microplates | Plates (typically 96-well) that efficiently adsorb capture antibody while minimizing non-specific adsorption. |
The performance of an ELISA is quantified through key parameters derived from the standard curve. The following table summarizes typical performance metrics for a research-grade plasma biomarker assay.
Table 1: Typical Performance Metrics for a Chemiluminescent Sandwich ELISA
| Parameter | Typical Target Value | Description & Implication |
|---|---|---|
| Limit of Detection (LoD) | 0.5 - 5 pg/mL | Lowest analyte concentration distinguishable from zero. Defines assay sensitivity. |
| Lower Limit of Quantification (LLoQ) | 2 - 20 pg/mL | Lowest concentration measurable with defined precision (CV <20%) and accuracy (80-120% recovery). |
| Dynamic Range | 2 - 3 logs (e.g., 10-10,000 pg/mL) | Range over which the assay provides a linear response. Critical for measuring biomarkers across patient cohorts. |
| Intra-Assay Precision (CV) | <10% | Variation between replicates within the same plate. Measures repeatability. |
| Inter-Assay Precision (CV) | <15% | Variation between different plates/runs. Measures reproducibility. |
| Spike Recovery in Plasma | 80 - 120% | Accuracy of measuring known amounts of analyte added to plasma. Assesses matrix interference. |
| Cross-Reactivity | <1% with homologs | Measures binding to closely related proteins (e.g., other enzyme family members). Ensures specificity. |
Detailed Protocol: Sandwich ELISA for Soluble Enzyme Biomarker in Plasma
Title: Protocol for Quantification of Soluble MMP-9 in Human Plasma via Sandwich ELISA
Principle: A capture anti-MMP-9 antibody is immobilized on a plate. MMP-9 in plasma samples or standards binds, followed by a biotinylated detection antibody. Signal is amplified via Streptavidin-HRP and a chemiluminescent substrate.
Materials: As listed in Section 2, with specific matched antibody pair for MMP-9.
Pre-Assay Notes:
- Collect plasma using EDTA tubes. Centrifuge at 2000 x g for 15 min. Aliquot and store at -80°C.
- Avoid repeated freeze-thaw cycles.
- Bring all reagents to room temperature (RT) before use.
Procedure:
Day 1: Coating and Sample Preparation
- Coating: Dilute capture antibody in 0.1 M carbonate-bicarbonate coating buffer (pH 9.6) to 2 µg/mL. Add 100 µL per well to a 96-well plate. Seal and incubate overnight at 4°C.
- Prepare Standard Dilutions: Serially dilute recombinant MMP-9 standard in plasma sample diluent to create a 7-point standard curve (e.g., from 1000 pg/mL to 1.95 pg/mL). Include a diluent-only zero standard.
- Prepare Samples: Thaw plasma samples on ice. Dilute 1:10 or 1:20 in sample diluent as determined by prior optimization.
Day 2: Assay Steps
- Wash: Aspirate coating solution. Wash plate 3x with 300 µL/well of Wash Buffer (0.05% Tween-20 in PBS). Blot dry on paper towels.
- Block: Add 300 µL of Blocking Buffer (5% BSA in PBS) per well. Incubate for 2 hours at RT on a plate shaker.
- Wash: Repeat step 4.
- Add Standards & Samples: Add 100 µL of each standard, diluted sample, and appropriate controls (e.g., pooled normal plasma) per well in duplicate. Incubate for 2 hours at RT with shaking.
- Wash: Repeat step 4.
- Add Detection Antibody: Add 100 µL of biotinylated anti-MMP-9 detection antibody (diluted per manufacturer's instructions in diluent) per well. Incubate for 1 hour at RT with shaking.
- Wash: Repeat step 4.
- Add Streptavidin-HRP: Add 100 µL of Streptavidin-HRP conjugate (diluted 1:5000 in diluent) per well. Incubate for 30 minutes at RT in the dark with shaking.
- Wash: Repeat step 4.
- Signal Detection: Add 100 µL of stabilized chemiluminescent substrate per well. Incubate for 5 minutes in the dark. Measure Relative Light Units (RLU) immediately using a plate reader with integration time of 100-500 ms/well.
Data Analysis:
- Calculate the mean RLU for each standard and sample.
- Generate a 4- or 5-parameter logistic (4PL/5PL) standard curve by plotting log(MMP-9 concentration) vs. log(RLU).
- Interpolate sample concentrations from the curve.
- Multiply by the sample dilution factor to obtain the original plasma concentration.
Visualization Diagrams
Diagram 1 Title: ELISA Sandwich Assay Workflow
Diagram 2 Title: ELISA Signal Amplification Cascade
Diagram 3 Title: Key Factors in Plasma Biomarker ELISA
Key Classes of Enzyme Biomarkers Measured by Plasma ELISA (e.g., Proteases, Kinases, Metabolizing Enzymes)
Within the broader thesis on ELISA detection of soluble enzyme biomarkers in plasma, this document details application notes and protocols for three pivotal classes: proteases, kinases, and metabolizing enzymes. These proteins, often shed or released into circulation, serve as critical indicators of pathological states, including cancer, cardiovascular disease, and inflammatory disorders. Their quantification via plasma ELISA presents unique challenges due to zymogen states, endogenous inhibitors, and low abundant activity, necessitating specialized methodological approaches.
Table 1: Key Plasma Enzyme Biomarker Classes: Examples, Associations, and ELISA Considerations
| Enzyme Class | Example Biomarker | Primary Disease Association | Typical Plasma Concentration Range | Key ELISA Challenge |
|---|---|---|---|---|
| Proteases | MMP-9 (Matrix Metalloproteinase-9) | Cancer metastasis, atherosclerosis | 20 - 200 ng/mL (healthy); can exceed 500 ng/mL (disease) | Distinguishing active vs. total (pro-form + active) enzyme. |
| Proteases | Neutrophil Elastase | COPD, sepsis | < 50 ng/mL (healthy); > 200 ng/mL (acute inflammation) | Rapid complexation with α1-antitrypsin requires specific epitope targeting. |
| Kinases | CA IX (Carbonic Anhydrase IX) | Renal cell carcinoma, hypoxic tumors | < 5 ng/mL (healthy); 10 - 50 ng/mL (disease) | Shed ectodomain is target; specificity over other CA isoforms is critical. |
| Metabolizing Enzymes | Myeloperoxidase (MPO) | Cardiovascular disease, MDS | 10 - 50 ng/mL (healthy); 100 - 1000 ng/mL (ACS) | Multiple molecular forms (monomer, dimer, complexed). |
| Metabolizing Enzymes | DPP-4 (Dipeptidyl Peptidase-4) | Diabetes, liver fibrosis | 300 - 600 ng/mL (soluble form) | High basal level; detecting subtle changes requires high precision. |
Detailed Experimental Protocols
Protocol 3.1: Sandwich ELISA for Active vs. Total Protease (MMP-9)
Principle: Use of capture antibody selective for pro-domain (total MMP-9) versus neo-epitope exposed upon activation (active MMP-9).
- Coating: Coat high-binding 96-well plate with 100 µL/well of mouse anti-human MMP-9 monoclonal antibody (clone 6-6B, for total MMP-9) OR anti-MMP-9 active form antibody (clone L51/82.1) at 2 µg/mL in carbonate buffer, pH 9.6. Incubate overnight at 4°C.
- Blocking: Aspirate, wash 3x with PBS/0.05% Tween-20 (PBST). Block with 300 µL/well of 3% BSA in PBS for 2 hours at RT.
- Sample Incubation: Dilute EDTA-plasma samples 1:10 in assay diluent (PBS/1% BSA/0.05% Tween-20). Add 100 µL/well of standard, sample, or control. Incubate 2 hours at RT on orbital shaker.
- Detection: Wash 5x with PBST. Add 100 µL/well of biotinylated detection antibody (polyclonal rabbit anti-human MMP-9) at 0.5 µg/mL. Incubate 1 hour at RT. Wash 5x.
- Signal Development: Add 100 µL/well of Streptavidin-HRP (1:5000 dilution). Incubate 30 min at RT, protected from light. Wash 7x. Add 100 µL TMB substrate, incubate 10-15 min. Stop with 100 µL 2M H₂SO₄.
- Analysis: Read absorbance at 450 nm (reference 570 nm). Generate 4-parameter logistic (4PL) standard curve (0.78 - 50 ng/mL recombinant MMP-9). Report values in ng/mL.
Protocol 3.2: Sandwich ELISA for Soluble Kinase Ectodomain (CA IX)
Principle: Capture soluble CA IX ectodomain shed from tumor cell surfaces.
- Coating: Coat plate with 100 µL/well of mouse anti-human CA IX monoclonal antibody (clone M75) at 5 µg/mL in PBS overnight at 4°C.
- Blocking & Sample: Block with 5% non-fat dry milk in PBST. Dilute citrate-plasma 1:2. Incubate 100 µL/well of standard or sample for 3 hours at RT.
- Detection: Wash, then incubate with 100 µL/well of biotinylated rabbit anti-human CA IX polyclonal antibody (1 µg/mL) for 1.5 hours.
- Signal & Analysis: Follow steps 5-6 from Protocol 3.1. Use recombinant CA IX ectodomain as standard (range 0.2 - 25 ng/mL).
Protocol 3.3: ELISA for Complexed Metabolizing Enzyme (Myeloperoxidase)
Principle: Detect MPO irrespective of complexation with ceruloplasmin or other proteins.
- Coating: Coat plate with 100 µL/well of goat anti-human MPO capture antibody (polyclonal) at 4 µg/mL in coating buffer overnight.
- Blocking & Sample: Block with 2% BSA/PBS. Dilute heparin-plasma 1:100 in 1% BSA/PBST. Incubate 100 µL/well for 2 hours.
- Detection: Wash. Add 100 µL/well of mouse anti-human MPO detection antibody (clone 4A4, HRP-conjugated) at 0.1 µg/mL for 1 hour.
- Signal & Analysis: Wash, develop with TMB for 10 min, stop, and read. Use purified human MPO standard (range 3.9 - 250 ng/mL).
Diagrams of Pathways and Workflows
Sandwich ELISA Workflow for Soluble Enzymes
CA IX Shedding from Tumor to Plasma Detection
Plasma Collection Matrix Guidance by Enzyme Class
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Plasma Enzyme ELISA
| Reagent / Material | Function & Critical Consideration |
|---|---|
| High-Binding ELISA Plates | Polystyrene plates for optimal antibody adsorption. Consistency between plate lots is crucial for assay reproducibility. |
| Antibody Pair (Capture/Detection) | Monoclonal or affinity-purified polyclonal antibodies targeting non-overlapping epitopes on the target enzyme. Specificity for active form or specific isoform may be required. |
| Recombinant Purified Enzyme Standard | Quantification calibrator. Must be in the same matrix as samples (e.g., analyte-free plasma diluted) for accurate standard curve generation. |
| HRP-Streptavidin Conjugate | High-sensitivity detection system for biotinylated detection antibodies. Low non-specific binding conjugates reduce background. |
| TMB (3,3',5,5'-Tetramethylbenzidine) Substrate | Chromogenic HRP substrate. Stable, ready-to-use liquid formulations ensure consistent development kinetics. |
| Anticoagulant-Specific Plasma Collection Tubes | Choice (EDTA, Heparin, Citrate) critically impacts enzyme stability and must be standardized per biomarker. |
| Protease/Phosphatase Inhibitor Cocktails | Added immediately post-blood draw to prevent in vitro degradation or modification (esp. for proteases/kinases) in plasma. |
| Blocking Buffer (e.g., BSA, Casein) | Reduces non-specific binding. Must be optimized; BSA may contain trace enzymes (e.g., bovine ALP) that interfere. |
This Application Note details the application of enzyme-linked immunosorbent assay (ELISA) for the detection of soluble enzyme biomarkers in plasma, framed within a broader thesis on their role in translational research. Soluble enzymes, released into circulation due to cellular activity, stress, or death, provide critical insights into disease pathogenesis, progression, and therapeutic response across major disease areas.
Application Notes: Soluble Enzyme Biomarkers by Disease Area
Table 1: Key Soluble Enzyme Biomarkers and Their Clinical Research Applications
| Disease Area | Enzyme Biomarker | Primary Cellular Source | Research Context & Association | Typical Plasma Detection Range (ELISA) |
|---|---|---|---|---|
| Oncology | Carbonic Anhydrase IX (CA9) | Tumor cells (hypoxic regions) | Tumor hypoxia, metastasis, prognosis in RCC, breast cancer. | 100–5000 pg/mL |
| Oncology | Poly(ADP-ribose) Polymerase 1 (PARP1) | Nucleus/Cytoplasm (released upon cell death) | Therapy-induced cell death (e.g., PARP inhibitor efficacy), DNA damage response. | 1–50 ng/mL |
| Neurology | Neurogranin (NRGN) | Neurons (postsynaptic) | Synaptic dysfunction and degeneration in Alzheimer's disease. | 50–1000 pg/mL |
| Neurology | Glutamate Decarboxylase 65 (GAD65) | Pancreatic β-cells, Neurons | Autoimmune neuropathy, Stiff-person syndrome. | 0.1–20 IU/mL (autoantibodies) |
| Inflammation | Myeloperoxidase (MPO) | Neutrophil granules | Neutrophil activation, cardiovascular inflammation, vasculitis. | 10–200 ng/mL |
| Inflammation | Cyclooxygenase-2 (COX-2/PGES-1) | Inflammatory cells, Endothelium | Systemic inflammation, monitoring NSAID/COXIB therapeutic effects. | 50–2000 pg/mL |
| Metabolic Disorders | Dipeptidyl Peptidase-4 (DPP4) | Adipocytes, Endothelium, Immune cells | Adipose tissue inflammation, insulin resistance, type 2 diabetes. | 200–800 ng/mL |
| Metabolic Disorders | Fatty Acid Amide Hydrolase (FAAH) | Liver, CNS, Peripheral tissues | Endocannabinoid system dysregulation in obesity, NAFLD. | 2–30 ng/mL |
Detailed Experimental Protocols
Protocol 1: Quantification of Soluble PARP1 in Plasma for Therapy Response Monitoring
Objective: To measure cleaved/full-length PARP1 in human EDTA-plasma as a pharmacodynamic biomarker for DNA-damaging agents or PARP inhibitors. Materials: Human PARP1 (Cleaved/Full) ELISA Kit (e.g., Abcam, ab233565), EDTA-plasma samples, microplate washer, microplate reader. Procedure:
- Sample Prep: Centrifuge EDTA-blood at 2000 x g for 10 min at 4°C. Aliquot plasma, avoiding freeze-thaw cycles.
- Assay Setup: Reconstitute standards. Dilute plasma samples 1:5 in provided sample diluent.
- Incubation: Add 100 µL of standard or sample to pre-coated wells. Incubate 2.5 hours at RT with gentle shaking.
- Detection: Aspirate, wash 4x. Add 100 µL of biotinylated detection antibody. Incubate 1 hour. Wash, add 100 µL HRP-Streptavidin. Incubate 45 min.
- Signal Development: Wash, add 100 µL TMB substrate. Incubate 30 min in dark. Stop with 50 µL stop solution.
- Analysis: Read absorbance at 450 nm immediately. Plot standard curve (4-parameter logistic) and interpolate sample concentrations. Multiply by dilution factor.
Protocol 2: Detection of Soluble Neurogranin in Human Plasma
Objective: To quantify synaptic-derived neurogranin fragments in human plasma for neurodegenerative disease research. Materials: Human Neurogranin ELISA Kit (e.g., Roche Elecsys or commercial research kit), heparin or EDTA-plasma. Procedure:
- Sample Prep: Use platelet-poor plasma. Centrifuge at 2500 x g for 15 min, then 13,000 x g for 10 min at 4°C to remove platelets.
- Assay: Follow kit protocol for a sensitive sandwich ELISA (typically with electrochemiluminescence detection).
- Key Adaptation: Include a sample incubation step of 2 hours with detection antibody prior to adding to the plate to enhance sensitivity for low-abundance targets.
- Data Normalization: Report values as pg/mL. Correlate with total protein or albumin to control for blood-brain barrier variability.
Visualizations: Pathways & Workflows
Diagram 1: Soluble Enzyme Biomarker Release & Detection Pathway
Diagram 2: ELISA Protocol Workflow for Plasma Biomarker Quantification
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Plasma-Based Soluble Enzyme ELISA
| Item | Function & Critical Notes |
|---|---|
| High-Sensitivity ELISA Kits | Pre-optimized sandwich ELISA kits with validated antibody pairs specific for the soluble enzyme form (e.g., cleaved vs. full-length). |
| Matched Antibody Pairs | For developing in-house assays: monoclonal capture and detection antibodies targeting different epitopes on the soluble enzyme. |
| Protease Inhibitor Cocktails | Added during blood processing to prevent ex vivo degradation of labile enzyme biomarkers (e.g., for neurogranin). |
| Platelet Depletion Reagents | Critical for neurology biomarkers; prevents contamination from platelet-associated proteins. Use sequential centrifugation or filtration. |
| Recombinant Antigen Standards | Quantified, highly pure recombinant protein for generating standard curves. Must match the detected isoform. |
| Signal Amplification Systems | (e.g., Tyramide, ECL) Essential for detecting low-abundance targets (< 50 pg/mL) in the complex plasma matrix. |
| Matrix Interference Blocker | Species-specific or generic blockers (e.g., Heteroblock) to reduce nonspecific binding and heterophilic antibody interference. |
| Validated Plasma/Serum Controls | Pooled disease-state and healthy donor samples for inter-assay precision monitoring and normalization. |
Within modern drug development, biomarkers are indispensable for making quantitative, objective decisions. This article details protocols focused on the ELISA detection of soluble enzyme biomarkers in plasma, framed within the critical context of informing pharmacodynamics (PD), confirming target engagement (TE), and monitoring safety. Soluble enzymes, often released from tissues into circulation, provide a dynamic readout of biological processes, drug action, and off-target effects. The accurate measurement of their concentration or activity in plasma via ELISA offers a minimally invasive, translational strategy to bridge preclinical findings and clinical outcomes, de-risking development and accelerating candidate selection.
Table 1: Key Soluble Enzyme Biomarkers, Their Roles, and Associated Indications
| Biomarker (Enzyme) | Primary Biological Source | Role in Drug Development | Exemplary Therapeutic Area |
|---|---|---|---|
| Soluble ACE2 (sACE2) | Membrane-bound ACE2 shedding | TE/PD for renin-angiotensin system modulators & viral entry blockers; Safety for cardiovascular/renal function. | Cardiovascular, Infectious Disease |
| DPP-4 (sCD26) | T-cells, endothelial cells, hepatocytes | TE/PD for DPP-4 inhibitor class (gliptins); marker of immune activation. | Type 2 Diabetes, Immunology |
| PARP1 Fragments | Nuclear enzyme released during cell death (e.g., apoptosis) | PD for PARP inhibitor efficacy in inducing synthetic lethality. | Oncology (BRCA-mutant cancers) |
| CPS1 (Carbamoyl Phosphate Synthase 1) | Hepatocyte mitochondria | Safety biomarker for drug-induced liver injury (DILI); released upon mitochondrial damage. | All therapeutic areas (Safety) |
| Lipoprotein-Associated Phospholipase A2 (Lp-PLA2) | Inflammatory cells (macrophages, monocytes) | PD for anti-inflammatory therapies; risk biomarker for cardiovascular events. | Cardiovascular, Neurology |
Table 2: Typical Plasma Concentration Ranges & ELISA Performance Metrics
| Biomarker | Expected Plasma Range (Healthy) | Assay Dynamic Range | Critical Sample Considerations |
|---|---|---|---|
| sACE2 | 1-10 ng/mL | 0.2 - 50 ng/mL | Avoid repeated freeze-thaw; use protease inhibitors. |
| DPP-4 | 200-600 ng/mL | 5 - 2000 ng/mL | Stable in serum/plasma; EDTA plasma preferred. |
| CPS1 | Very low (≥0.5 ng/mL in DILI) | 0.1 - 30 ng/mL | Markedly elevated in hepatic injury; measure promptly. |
Detailed Experimental Protocol: Sandwich ELISA for Soluble DPP-4 in Human Plasma
Objective: To quantitatively measure soluble DPP-4 (sCD26) concentration in human EDTA plasma as a TE biomarker for DPP-4 inhibitor therapy.
I. Materials & Reagent Setup (The Scientist's Toolkit)
- Coated Microplate: 96-well plate pre-coated with mouse anti-human DPP-4 capture antibody.
- Detection Antibody: Biotinylated mouse anti-human DPP-4 antibody, specific to a different epitope.
- Standard: Recombinant human DPP-4 protein lyophilized. Reconstitute and prepare a 7-point serial dilution in Assay Diluent (range: 5-2000 ng/mL).
- Quality Controls (QCs): Prepare low, mid, and high concentration QCs in analyte-free matrix.
- Streptavidin-HRP: Conjugate for signal amplification.
- Wash Buffer: PBS with 0.05% Tween-20.
- Substrate Solution: TMB (3,3',5,5'-Tetramethylbenzidine).
- Stop Solution: 1M Sulfuric Acid.
- Plate Reader: Capable of measuring absorbance at 450 nm (reference 570 nm or 620 nm).
II. Step-by-Step Protocol
- Sample Preparation: Thaw plasma samples on ice. Centrifuge at 10,000 x g for 10 minutes at 4°C to remove precipitates. Dilute samples 1:100 in Assay Diluent.
- Plate Assembly: Add 100 µL of standards, QCs, and diluted samples to appropriate wells. Include blank wells (Assay Diluent only). Cover and incubate for 2 hours at room temperature (RT) on an orbital shaker.
- Wash: Aspirate and wash each well 4 times with 300 µL Wash Buffer.
- Detection Antibody: Add 100 µL of biotinylated detection antibody to each well. Incubate for 1 hour at RT on shaker. Wash 4 times.
- Streptavidin-HRP: Add 100 µL of Streptavidin-HRP solution to each well. Incubate for 30 minutes at RT in the dark. Wash 4 times.
- Substrate Reaction: Add 100 µL of TMB substrate. Incubate for 15-20 minutes at RT in the dark (monitor for blue color development).
- Stop & Read: Add 100 µL of Stop Solution. Read absorbance at 450 nm within 30 minutes.
- Data Analysis: Generate a 4-parameter logistic (4-PL) standard curve. Interpolate sample concentrations, applying the dilution factor.
III. Data Interpretation for Target Engagement A successful DPP-4 inhibitor will demonstrate a dose-dependent and/or time-dependent increase in plasma sDPP-4 concentration, reflecting inhibitor binding and subsequent shedding or stabilization of the soluble form. Lack of change may indicate insufficient target engagement.
Visualizations: Pathways and Workflows
Title: DPP-4 Inhibitor Mechanism and sDPP4 Biomarker Release
Title: Plasma Soluble Biomarker ELISA Workflow
A Step-by-Step Protocol: Optimizing ELISA Workflow for Plasma Enzyme Biomarker Detection
Within the context of ELISA detection of soluble enzyme biomarkers in plasma, the pre-analytical phase is the most critical determinant of reliable results. Variability introduced during blood collection, processing, and storage can irreversibly degrade biomarker integrity, leading to false positives, false negatives, and compromised data. This application note details standardized protocols to minimize pre-analytical variability and ensure the accurate quantification of labile enzyme biomarkers such as proteases, kinases, and inflammatory mediators.
Blood Collection: Minimizing Ex Vivo Activation
The choice of anticoagulant and collection protocol directly influences analyte stability.
Anticoagulant Selection
The optimal anticoagulant depends on the target biomarker. For most soluble enzyme biomarkers, EDTA is preferred for inhibiting metalloproteases. Citrate is suitable for coagulation factors, while heparin should be avoided for phosphorylation studies due to its potential to activate enzymes.
Table 1: Anticoagulant Effects on Common Enzyme Biomarkers
| Anticoagulant | Mechanism | Best For | Avoid For | Typical Concentration |
|---|---|---|---|---|
| K₂/K₃ EDTA | Chelates Ca²⁺/Mg²⁺ | Metalloprotease inhibitors, routine cytokines | Ca²⁺-dependent enzymes (e.g., some clotting factors) | 1.8 mg/mL blood |
| Sodium Citrate | Weak Ca²⁺ chelation | Coagulation cascade enzymes, complement factors | Assays sensitive to dilution | 3.2% (0.109M), 1:9 ratio |
| Lithium Heparin | Activates antithrombin | Rapid plasma separation, some metabolic enzymes | Phospho-protein/kinase studies | 15-30 IU/mL blood |
Collection Protocol
- Needle Gauge: Use 21G or larger to prevent shear stress-induced platelet activation.
- Tourniquet Time: Minimize to <1 minute. Prolonged stasis alters protein concentration and activates hemostasis.
- Fill Volume: Fill collection tubes to the correct volume to maintain the blood-to-anticoagulant ratio.
- Mixing: Gently invert tubes 8-10 times immediately after collection to ensure proper mixing.
Plasma Processing: A Time-Sensitive Protocol
Rapid and consistent processing is paramount to halt ex vivo degradation and release of intracellular enzymes.
Detailed Processing Protocol for Biomarker Stability
Objective: To isolate platelet-poor plasma (PPP) suitable for sensitive enzyme biomarker ELISA.
Materials:
- Centrifuge capable of maintaining 4°C
- Fixed-angle rotor (swing-out rotors are less effective for a tight pellet)
- Sterile polypropylene tubes (for aliquoting)
- Timer
- Cooled rack or chill block
Procedure:
- Transport: Keep collected blood tubes upright and transport at ambient temperature (unless specified otherwise) to the lab immediately. Do not chill whole blood.
- First Spin (Platelet Removal):
- Centrifuge at 1,600–2,000 x g for 15 minutes at 4°C.
- Critical: Use brakes OFF to prevent disturbing the pellet.
- Plasma Transfer:
- Using a sterile pipette, carefully transfer the top plasma layer (approximately the top 2/3) to a new polypropylene tube.
- Avoid: The buffy coat (white layer) and the top of the red blood cell pellet.
- Second Spin (Platelet-Poor Plasma):
- Centrifuge the transferred plasma at 2,500–3,000 x g for 10 minutes at 4°C.
- This step ensures removal of residual platelets, whose releaseates can contaminate samples.
- Final Aliquot Preparation:
- Transfer the doubly-centrifuged plasma into pre-chilled, labeled polypropylene cryovials.
- Aliquot volume should be sufficient for a single assay use to avoid freeze-thaw cycles (e.g., 50-200 µL).
- Place aliquots immediately on dry ice or in a -80°C freezer.
Table 2: Impact of Processing Delay on Biomarker Stability
| Biomarker Class | Recommended Max Processing Delay (Room Temp) | Key Degradation Mechanism |
|---|---|---|
| Labile Enzymes (e.g., PAI-1, DPP-4) | <30 minutes | Conformational change, autolysis |
| Phospho-Proteins | <60 minutes | Phosphatase activity |
| Cytokines/Chemokines | <2 hours | Proteolysis, adsorption |
| Matrix Metalloproteinases (MMPs) | <1 hour | TIMP binding, autocatalysis |
Storage: Maintaining Long-Term Integrity
Proper storage conditions are non-negotiable for biobanking.
Temperature Guidelines
- Short-term (<1 month): -80°C is mandatory. Never store at -20°C for enzyme biomarkers, as ice crystal formation and enzymatic activity are not fully halted.
- Long-term (>1 month): Store at -80°C in a dedicated, non-frost-free freezer. For ultimate stability, store in liquid nitrogen vapor phase (-150°C to -196°C).
Freeze-Thaw Cycles
A single freeze-thaw cycle can cause significant loss of activity for many enzymes. Aliquoting is critical.
Table 3: Effect of Freeze-Thaw Cycles on Biomarker Recovery (%)
| Biomarker | 0 Cycles | 1 Cycle | 2 Cycles | 3 Cycles |
|---|---|---|---|---|
| Active MMP-9 | 100% | 85±5% | 70±8% | 55±12% |
| Soluble Epoxide Hydrolase | 100% | 92±3% | 81±6% | 65±10% |
| Protein Kinase C (soluble) | 100% | 78±7% | 60±9% | 40±15% |
| Stable Reference Protein (e.g., Albumin) | 100% | 99±1% | 98±1% | 97±2% |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Importance |
|---|---|
| EDTA Plasma Collection Tubes | Prevents coagulation and chelates metals to inhibit metalloproteases, preserving native biomarker state. |
| Polypropylene Cryogenic Vials | Chemically inert, low protein binding, and withstands extreme temperatures without cracking. |
| Protease & Phosphatase Inhibitor Cocktails (additive) | Added immediately post-collection for exceptionally labile targets to halt ex vivo degradation. |
| Platelet Depletion Filters | For ultra-pure plasma, physically removes platelets before the first spin for platelet-derived biomarkers. |
| Temperature-Validated Freezer (-80°C) | Ensures consistent, ultra-cold storage. Frost-free freezers cause temperature fluctuations and sample degradation. |
| Cryoboxes with Color-Coding | For secure, organized sample archiving and rapid retrieval to minimize thaw time. |
| Liquid Nitrogen Dewar (Vapor Phase) | Provides the gold standard for long-term (>5 years) stability of highly labile enzymes. |
Workflow & Pathway Diagrams
Title: Plasma Processing Workflow for Biomarker Integrity
Title: Pre-Analytical Stressors Leading to Biomarker Degradation
Within plasma-based biomarker research for drug development, the detection of soluble enzyme biomarkers (e.g., MMPs, Caspases, Kinases) via ELISA is pivotal. The choice between commercial kits and in-house assays, alongside the selection of a direct or sandwich format, fundamentally impacts data quality, throughput, and cost. This guide provides a structured comparison and protocols for these critical decisions.
Comparative Analysis: Commercial Kits vs. In-House Assays
Table 1: Key Decision Factors for ELISA Format Selection
| Factor | Commercial ELISA Kits | In-House ELISA Assays |
|---|---|---|
| Development Time | Minimal (Hours to Days) | Extensive (Weeks to Months) |
| Standardization | High (Pre-optimized, lot-controlled) | Variable (Requires rigorous validation) |
| Assay Cost per Plate | High ($400 - $800) | Low ($50 - $200) |
| Initial Investment | Low (Kit cost only) | High (Antibody/Reagent procurement, validation) |
| Customization Flexibility | Low (Fixed parameters) | High (Antibody pairs, buffers, protocols) |
| Best Suited For | High-throughput screening, regulated studies, single-analyte focus | Novel biomarker discovery, high-volume testing, multi-analyte panels |
Application Note: For novel enzyme biomarkers where commercial antibodies are available but no kit exists, a validated in-house sandwich ELISA is often the only viable path. For established biomarkers in clinical trial sample analysis, FDA-approved commercial kits provide necessary standardization.
Comparative Analysis: Direct vs. Sandwich ELISA
Table 2: Technical Comparison of Direct and Sandwich ELISA Formats
| Parameter | Direct ELISA | Sandwich ELISA |
|---|---|---|
| Complexity | Low (One antibody) | High (Matched antibody pair required) |
| Time to Result | Fast (~3 hours) | Slow (~5-6 hours) |
| Specificity | Lower (Potential for non-specific binding) | High (Two epitopes required) |
| Sensitivity | Low (ng/mL range) | Very High (pg/mL range) |
| Sample Type Flexibility | High (Can detect antigens in complex matrices) | Moderate (Can be hampered by high-abundance proteins) |
| Ideal Use Case | Quick check for high-abundance antigen, antibody screening | Quantification of low-abundance biomarkers in plasma (e.g., cytokines, enzymes) |
Application Note: For soluble enzyme biomarkers in plasma, the sandwich format is almost universally superior due to its enhanced specificity and sensitivity, crucial for detecting low concentrations amidst a complex background. Direct ELISA is rarely used for quantitative plasma biomarker studies.
Experimental Protocols
Protocol 4.1: In-House Sandwich ELISA Development for a Novel Enzyme Biomarker
Objective: To quantify soluble Enzyme X in human plasma using a validated in-house sandwich ELISA.
I. Reagent Preparation
- Coating Buffer: 0.1 M Carbonate-Bicarbonate Buffer, pH 9.6.
- Wash Buffer (PBS-T): 1X PBS, 0.05% Tween-20.
- Blocking Buffer: 1X PBS, 1% BSA, 0.05% Tween-20.
- Sample Diluent: 1X PBS, 0.5% BSA, 0.05% Tween-20.
- Detection Antibody Diluent: Blocking Buffer.
- Enzyme Conjugate: Streptavidin-Horseradish Peroxidase (SA-HRP), diluted in Blocking Buffer.
- Substrate: TMB (3,3',5,5'-Tetramethylbenzidine).
- Stop Solution: 1M H2SO4.
- Capture Antibody: High-affinity monoclonal anti-Enzyme X antibody.
- Detection Antibody: Biotinylated monoclonal anti-Enzyme X antibody (different epitope).
II. Step-by-Step Procedure
- Coating: Dilute capture antibody to 2-10 µg/mL in Coating Buffer. Add 100 µL/well to a 96-well microplate. Seal and incubate overnight at 4°C.
- Washing: Aspirate wells. Wash 3x with 300 µL/well Wash Buffer using a plate washer. Blot plate on lint-free paper.
- Blocking: Add 300 µL/well Blocking Buffer. Incubate for 1-2 hours at room temperature (RT) on a plate shaker. Wash as in Step 2.
- Sample & Standard Addition: Prepare a standard curve of recombinant Enzyme X in Sample Diluent (e.g., 1000 pg/mL, 1:2 serial dilutions). Dilute plasma samples 1:10-1:50 in Sample Diluent. Add 100 µL of standard or sample per well. Incubate for 2 hours at RT on a shaker. Wash as in Step 2.
- Detection Antibody Incubation: Add 100 µL/well of biotinylated detection antibody (optimized concentration, typically 0.5-2 µg/mL). Incubate for 1-2 hours at RT on a shaker. Wash as in Step 2.
- Enzyme Conjugate Incubation: Add 100 µL/well of SA-HRP (optimized dilution, typically 1:5000-1:20000). Incubate for 30-60 minutes at RT in the dark. Wash as in Step 2.
- Signal Development: Add 100 µL/well of TMB substrate. Incubate in the dark for 5-30 minutes until blue color develops adequately.
- Reaction Stop: Add 50 µL/well of Stop Solution. Read absorbance immediately at 450 nm (reference 570 nm or 620 nm).
Protocol 4.2: Protocol for a Typical Commercial Sandwich ELISA Kit
- Note: Follow the manufacturer's instructions precisely. A generalized workflow is:
- Reconstitution: Prepare all standards, controls, and reagents as per kit insert.
- Assay: Add standards and pre-diluted samples to pre-coated wells. Incubate and wash.
- Detection: Add detection antibody, incubate and wash. Add enzyme-conjugate, incubate and wash.
- Development/Readout: Add substrate, stop, and read absorbance.
Visualizations
Title: ELISA Format Decision Flowchart
Title: Sandwich ELISA Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for In-House Sandwich ELISA Development
| Item | Function & Rationale |
|---|---|
| Matched Antibody Pair | A capture and a biotinylated detection antibody targeting non-overlapping epitopes on the target enzyme. Critical for specificity. |
| Recombinant Antigen Standard | Highly pure, quantifiable protein for generating the standard curve. Essential for accurate concentration determination. |
| High-Binding 96-Well Plates | Polystyrene plates treated for optimal antibody adsorption. Ensures consistent coating efficiency. |
| Blocking Agent (BSA or Casein) | Reduces non-specific binding by occupying unused protein-binding sites on the plate and wells. |
| Biotin-Streptavidin System | Amplification system where biotinylated detection antibody is bound by Streptavidin-HRP, enhancing signal sensitivity. |
| Chromogenic Substrate (TMB) | HRP enzyme catalyzes the conversion of TMB to a blue product, measurable spectrophotometrically. |
| Plate Washer | Provides consistent and thorough washing between steps to reduce background noise and improve precision. |
| Plate Reader (Absorbance) | Measures the optical density of the developed color reaction at 450 nm for quantification. |
This protocol details the critical steps of a sandwich Enzyme-Linked Immunosorbent Assay (ELISA) for the quantification of soluble enzyme biomarkers (e.g., MMP-9, Caspase-3) in human plasma. Within the broader thesis on "Novel Soluble Enzyme Biomarkers as Prognostic Indicators in Inflammatory Disease," robust and reproducible ELISA methodology is foundational. Accurate detection of low-abundance analytes in the complex plasma matrix is essential for correlating biomarker levels with clinical outcomes and therapeutic responses in drug development.
Key Reagent Solutions: The Scientist's Toolkit
| Reagent/Material | Function & Critical Considerations |
|---|---|
| High-Binding ELISA Plates (e.g., Polystyrene) | Provides a stable hydrophobic surface for passive adsorption of the capture antibody. |
| Coating Buffer (Carbonate-Bicarbonate, pH 9.6) | Optimal alkaline pH enhances antibody adsorption by promoting hydrophobic interactions. |
| Capture & Detection Antibodies (Matched Pair) | Target-specific monoclonal antibodies binding to distinct, non-overlapping epitopes on the biomarker. |
| Blocking Buffer (e.g., 1-5% BSA or Casein in PBST) | Saturates remaining protein-binding sites to minimize non-specific background signal. |
| Assay Diluent (Protein-based buffer, e.g., 1% BSA PBST) | Diluent for samples/standards to mimic matrix and reduce non-specific interactions. |
| Wash Buffer (PBS with 0.05% Tween 20, PBST) | Removes unbound reagents; detergent reduces hydrophobic and ionic interactions. |
| Enzyme Conjugate (e.g., Streptavidin-HRP) | Binds to biotinylated detection antibody; catalyzes colorimetric/chemiluminescent reaction. |
| TMB Substrate (3,3’,5,5’-Tetramethylbenzidine) | Chromogenic substrate for HRP; turns blue upon oxidation, stopped with acid to yellow. |
| Stop Solution (1M H₂SO₄ or HCl) | Halts enzymatic reaction, stabilizes final signal, and shifts TMB to yellow for measurement. |
Detailed Experimental Protocol
A. Coating
- Dilute the purified capture antibody in carbonate-bicarbonate coating buffer (pH 9.6) to a final concentration of 1-10 µg/mL (see Table 1).
- Dispense 100 µL per well into a 96-well microplate.
- Seal the plate and incubate overnight at 4°C (or 1-2 hours at 37°C) in a humid environment.
- Critical Note: Coating concentration and time must be optimized for each antibody pair to maximize sensitivity and dynamic range.
B. Washing (General Procedure)
- Aspirate liquid from all wells completely.
- Dispense 300 µL of wash buffer (PBST) into each well using a multichannel pipette or plate washer.
- Let it sit for 30 seconds, then aspirate completely.
- Repeat steps 2-3 for a total of three washes.
- After the final wash, invert the plate and blot firmly onto clean paper towels to remove residual buffer.
C. Blocking
- After coating and washing, add 300 µL of blocking buffer (e.g., 3% BSA in PBST) to every well.
- Seal the plate and incubate for 1-2 hours at room temperature (or overnight at 4°C).
- Wash the plate three times as described above. The plate is now ready for sample addition or can be dried, sealed, and stored at 4°C for short-term use.
D. Sample & Standard Incubation
- Prepare a dilution series of the recombinant biomarker protein in the recommended assay diluent (e.g., 1% BSA in PBST) to generate a standard curve. Include a blank (diluent only).
- Dilute plasma samples (typical starting dilution 1:2 to 1:10) in the same assay diluent to minimize matrix effects.
- Add 100 µL of each standard, sample, and blank to designated wells in duplicate or triplicate.
- Seal the plate and incubate for 2 hours at room temperature with gentle shaking.
- Wash the plate three times.
E. Detection Antibody Incubation
- Prepare the biotinylated detection antibody at the optimal concentration (determined via checkerboard titration) in assay diluent.
- Add 100 µL per well.
- Seal the plate and incubate for 1-2 hours at room temperature.
- Wash the plate three times.
F. Enzyme Conjugate Incubation
- Prepare Streptavidin-Horseradish Peroxidase (Streptavidin-HRP) conjugate at the manufacturer’s recommended dilution (typically 1:2000 to 1:10,000) in assay diluent.
- Add 100 µL per well.
- Seal the plate and incubate for 30 minutes at room temperature, protected from light.
- Wash the plate five times thoroughly to remove all unbound conjugate.
G. Detection & Development
- Prepare TMB substrate solution according to manufacturer instructions. Ensure it is at room temperature.
- Add 100 µL of TMB substrate to each well.
- Incubate at room temperature, protected from light, and monitor for color development (typically 5-30 minutes).
- Once the desired blue color develops in the mid-range standards, add 100 µL of 1M H₂SO₄ stop solution to each well in the same order as the substrate was added.
- Read the optical density (OD) immediately at 450 nm with a reference wavelength of 570 nm or 620 nm on a plate reader.
Data Presentation: Typical Optimization Parameters and Expected Results
Table 1: Example Titration Data for Capture Antibody Optimization (MMP-9 ELISA)
| Capture Ab [µg/mL] | Background OD (Blank) | OD at Mid-Range Standard (2 ng/mL) | Signal-to-Background Ratio |
|---|---|---|---|
| 0.5 | 0.05 | 0.45 | 9.0 |
| 1.0 | 0.06 | 0.85 | 14.2 |
| 2.0 | 0.08 | 1.20 | 15.0 |
| 5.0 | 0.12 | 1.25 | 10.4 |
| 10.0 | 0.18 | 1.30 | 7.2 |
Optimal concentration selected: 2.0 µg/mL for best sensitivity and high signal-to-background.
Table 2: Example Standard Curve Data for a Target Biomarker
| Standard Concentration (pg/mL) | Mean OD (450nm) | Corrected OD (Mean - Blank) |
|---|---|---|
| 0 (Blank) | 0.075 | 0.000 |
| 78 | 0.120 | 0.045 |
| 156 | 0.210 | 0.135 |
| 312 | 0.450 | 0.375 |
| 625 | 0.950 | 0.875 |
| 1250 | 1.650 | 1.575 |
| 2500 | 2.300 | 2.225 |
| 5000 | 2.650 | 2.575 |
Sensitivity (Lowest detectable concentration): <78 pg/mL. Dynamic Range: ~78-2500 pg/mL.
Visualization: ELISA Workflow and Signaling Pathway
ELISA Protocol Steps in Sequence
Biomarker Pathway from Cell to ELISA Detection
Accurate detection of soluble enzyme biomarkers in plasma via ELISA is critical for diagnostic and drug development research. However, assay accuracy is frequently compromised by matrix effects and endogenous interferences, including lipids, hemolysis, and heterophilic antibodies. This application note details optimized sample preparation protocols to mitigate these interferences, framed within a thesis on improving the reliability of plasma-based enzyme biomarker quantification.
Table 1: Impact of Common Interferents on ELISA Recovery of Target Enzyme Biomarkers
| Interferent | Concentration Level | % Recovery (Unoptimized) | % Recovery (Post-Optimization) | Recommended Mitigation Strategy |
|---|---|---|---|---|
| Lipids (Triglycerides) | >300 mg/dL | 65 ± 12% | 95 ± 5% | High-Speed Centrifugation + Dilution |
| Hemoglobin (Hemolysis) | >0.5 g/L | 58 ± 15% | 92 ± 6% | Serial Dilution with Assessor |
| Heterophilic Antibodies | High Titer | 45 ± 20% | 98 ± 4% | Blocking Agent + Target-Specific Diluent |
| Bilirubin | >20 mg/dL | 75 ± 8% | 96 ± 3% | Sample Blank Subtraction |
| Rheumatoid Factor | >100 IU/mL | 70 ± 10% | 97 ± 3% | IgG/RF Absorbent Treatment |
Table 2: Optimal Dilution Series for Common Plasma Enzyme Biomarkers
| Target Enzyme | Recommended Starting Dilution (Plasma) | Optimal Linear Range (Post-Dilution) | Diluent Composition |
|---|---|---|---|
| MMP-9 | 1:20 | 0.5 - 50 ng/mL | PBS, 0.1% BSA, 0.05% Tween-20 |
| PAI-1 | 1:10 | 1 - 100 ng/mL | Tris-Buffered Saline, 1% BSA |
| Caspase-3 | 1:5 | 0.2 - 20 ng/mL | Assay Buffer + Heterophilic Block |
| sCD40L | 1:40 | 10 - 2000 pg/mL | Commercial ELISA Diluent with Blockers |
Detailed Experimental Protocols
Protocol 3.1: High-Speed Centrifugation for Lipid Removal
Objective: To remove chylomicrons and very low-density lipoproteins (VLDL) that cause turbidity and non-specific binding.
- Thaw plasma samples at 4°C.
- Transfer 500 µL of plasma to a 1.5 mL microcentrifuge tube.
- Centrifuge at 18,000 x g for 25 minutes at 4°C.
- Carefully aspirate the middle clear layer (~300 µL) using a fine-tip pipette, avoiding the top lipid layer and bottom pellet.
- Proceed with optimized dilution in appropriate diluent.
Protocol 3.2: Serial Dilution for Hemolyzed Samples
Objective: To determine the optimal dilution factor that minimizes hemoglobin interference.
- Prepare a stock diluent (PBS, pH 7.4, containing 2% BSA and a commercial hemolysis interference blocker).
- Perform a serial dilution of the hemolyzed plasma sample: Neat, 1:2, 1:5, 1:10, 1:20.
- Assay all dilutions alongside a standard curve prepared in the same diluent.
- Plot measured concentration vs. dilution factor. The optimal dilution is the point where the curve plateaus (recovery becomes consistent, typically >90%).
- Re-assay all samples at this determined optimal dilution.
Protocol 3.3: Heterophilic Antibody Interference Blocking
Objective: To neutralize human anti-animal antibodies that cause false-positive or false-negative signals.
- Pre-incubate plasma samples with a commercial heterophilic blocking reagent (HBR) or a cocktail of purified animal IgGs (e.g., mouse, goat).
- Use a sample:blocker ratio of 1:1 by volume.
- Incubate for 60 minutes at room temperature on a rotating mixer.
- After pre-incubation, dilute the sample mixture further with the target-specific assay diluent to the final working dilution.
- Include a sample spiked with a known concentration of the target enzyme (spike-and-recovery control) to validate blocking efficacy.
Protocol 3.4: Dilution Linearization (Parallelism) Test
Objective: To confirm that sample dilution yields a linear response parallel to the standard curve, indicating minimal matrix effect.
- Prepare a high-concentration endogenous sample pool.
- Create a series of dilutions (e.g., 1:2, 1:4, 1:8, 1:16) in the proposed assay diluent.
- Run these dilutions on the same plate as the standard curve, which is prepared in the recommended calibrator diluent.
- Plot the measured OD or calculated concentration (if within range) against the dilution factor on a log-log scale.
- A line parallel to the ideal dilution line (slope ~1.0) indicates acceptable parallelism. Re-optimize diluent if non-parallel.
Visualizations
Title: Workflow for Plasma Sample Preparation & Interference Mitigation
Title: Mechanism of Heterophilic Antibody Interference and Blocking
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Sample Preparation
| Reagent/Material | Primary Function | Key Considerations for Use |
|---|---|---|
| Commercial Heterophilic Blocking Reagent (HBR) | Neutralizes human anti-mouse/anti-animal antibodies (HAMA) to prevent false signals. | Use at recommended concentration; pre-incubation time (30-60 min) is critical. |
| Immunoglobulin (IgG) Blocking Cocktail | Purified, non-specific animal IgGs (mouse, goat, rabbit) to saturate heterophilic binding sites. | Must be free of preservatives that might affect the assay (e.g., azide). |
| Lipid-Removing Agents (e.g., Dextran Sulfate) | Precipitates lipoproteins to reduce turbidity and non-specific binding. | Can co-precipitate some target analytes; requires validation via spike/recovery. |
| Hemolysis Interference Blocker | Contains specific reagents to minimize peroxidase-like activity of free hemoglobin. | Add directly to the assay diluent for consistent performance. |
| Matrix-Matched Calibrator Diluent | Provides a protein and salt background similar to the sample matrix for standard curve preparation. | Essential for achieving valid parallelism. Commercially available or prepared in-house (e.g., stripped plasma). |
| High-Binding, Low-Profile Microcentrifuge Tubes | For high-speed centrifugation steps to separate lipid layers. | Polypropylene tubes withstand 18,000+ x g forces. |
| Sample Diluent with High % BSA (5-10%) | Reduces non-specific adsorption of biomarkers to tube walls and improves protein stability. | Ensure BSA is IgG-free and protease-free for sensitive assays. |
| Non-ionic Detergent (e.g., Tween-20, Triton X-100) | Added to wash buffers and diluents to minimize hydrophobic interactions and non-specific binding. | Optimal concentration is typically 0.05-0.1%; higher concentrations may disrupt antibody binding. |
Within the framework of a thesis investigating the detection of soluble enzyme biomarkers (e.g., matrix metalloproteinases, serine proteases) in plasma via ELISA, the integrity of raw data acquisition is paramount. The plate reader is the critical instrument bridging the biochemical assay and quantitative analysis. This document provides detailed application notes and protocols for instrumentation calibration, validation, and data acquisition to ensure reproducible and reliable quantification of low-abundance biomarkers in complex plasma matrices.
Core Principles of Plate Reader Operation for ELISA
Modern microplate readers for ELISA detection typically function in absorbance mode, measuring the optical density (OD) of a colorimetric product (e.g., from TMB or OPD substrates). Key performance parameters for soluble biomarker detection include:
- Sensitivity/Dynamic Range: Must accommodate both high-concentration acute-phase proteins and low-concentration signaling enzymes.
- Precision: Low intra- and inter-assay variability is essential for measuring subtle, biologically relevant changes.
- Spectral Accuracy: Correct filter selection aligned with the substrate's absorbance peak (e.g., 450 nm for TMB, often with 540-590 nm reference) is required.
Calibration and Validation Protocols
Daily Operational Qualification (OQ) Protocol
Objective: Verify key instrument performance metrics prior to experimental runs. Materials:
- NIST-traceable neutral density filter set (e.g., OD 0.5, 1.0, 2.0 at 450 nm).
- Clean, blank microplate.
- Plate reader instrument software.
Procedure:
- Power on the reader and allow lamps to warm up for the manufacturer-specified time (typically 15-30 min).
- Perform an initial self-diagnostic check via the instrument software.
- Insert the neutral density filter into the designated position in a blank microplate.
- Read the plate using the absorbance mode at 450 nm (no reference wavelength).
- Acceptance Criteria: The mean measured OD for each filter must be within ±5% of the certified value. Record all data.
Table 1: Example Daily OQ Data for a 450 nm Filter
| Certified OD Value | Mean Measured OD (n=3) | Deviation (%) | Pass/Fail |
|---|---|---|---|
| 0.500 | 0.487 | -2.6% | Pass |
| 1.000 | 1.032 | +3.2% | Pass |
| 2.000 | 1.890 | -5.5% | Pass |
Monthly Wavelength Accuracy Check
Objective: Ensure optical filters/filters are transmitting light at the correct wavelength. Protocol: Use a didymium or holmium oxide filter, which has sharp, known absorption peaks. Scan absorbance across a range (e.g., 400-700 nm). The recorded peak minima must align with published standards (e.g., 452.5 nm for holmium) within ±2 nm.
Pathlength Correction for Plasma Assays
Objective: Account for variable assay volumes which can affect absorbance values. Protocol: Utilize the instrument's built-in pathlength correction feature (often based on a water absorption peak at ~900 nm) if available. For critical measurements, prepare standards in the same final volume as samples.
Protocol for Raw Data Acquisition in Plasma ELISA
Title: Optimized Raw Data Acquisition for Soluble Enzyme Biomarker ELISA from Plasma Scope: This protocol details steps from plate loading to raw data export for a sandwich ELISA quantifying a soluble protease in citrated plasma.
Materials:
- Coated and blocked ELISA plate (capture antibody specific to target biomarker).
- Plasma samples (diluted in appropriate assay buffer with protease inhibitors).
- Standards (recombinant biomarker in analyte-free matrix).
- Detection antibody (biotinylated).
- Streptavidin-HRP conjugate.
- Colorimetric TMB substrate.
- Stop solution (1M H₂SO₄ or HCl).
- Calibrated microplate reader with 450 nm (±10 nm bandwidth) filter.
Procedure:
- Plate Reader Pre-read Preparation:
- Perform Daily OQ as per Section 3.1.
- Pre-warm the reader chamber to 25°C (if temperature controlled).
- In the software, create a new absorbance protocol.
- Wavelength Setting: Primary: 450 nm. Reference: 620 nm or 540 nm (to subtract background scattering from plasma components).
- Read Mode: Endpoint.
- Orbital Shaking: Set to 3 seconds prior to read (optional, improves well homogeneity).
- Settling Time: 0 seconds.
- Dynamic Range: Set to automatic or ensure it covers 0.000 to >3.000 OD.
Plate Loading and Reading:
- After adding stop solution and ensuring no bubbles are present, gently blot the plate bottom.
- Insert the plate into the reader, aligning well A1 with the reader's home position.
- Initiate the read sequence.
- Critical: Do not adjust plate orientation after starting.
Raw Data Export and Integrity:
- Upon completion, immediately export two data files:
- Raw ODs: The 450 nm minus reference wavelength values for all wells.
- Instrument Metadata: A file containing read timestamp, instrument ID, protocol name, filter IDs, and OQ status.
- File Format: Save data as
.csv(comma-separated values) for universal compatibility. - Naming Convention: Use
YYYYMMDD_Assay_Target_InstrumentID_Raw.csv.
- Upon completion, immediately export two data files:
Data Analysis Workflow Diagram
Title: ELISA Raw Data to Concentration Workflow
Plate Reader Signal Pathway for TMB-based ELISA
Title: TMB Signal Generation Pathway in Sandwich ELISA
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Plasma Biomarker ELISA and Data Acquisition
| Item | Function & Rationale |
|---|---|
| NIST-Traceable OD Filters | Provides absolute standard for daily verification of plate reader photometric accuracy, ensuring data traceability. |
| Matrix-Matched Calibrator Diluent | A buffer spiked with immunoglobulin and lipids to mimic plasma matrix. Reduces interference in standard curve fitting. |
| High-Affinity, Cross-Absorbed Detection Antibodies | Minimizes non-specific binding to heterophilic antibodies or other plasma proteins, lowering background noise. |
| HRP Conjugate with High Specific Activity | Amplifies signal from low-abundance targets, improving assay sensitivity and dynamic range. |
| Stable, Low-Noise TMB Substrate | Provides consistent enzymatic turnover with minimal spontaneous oxidation, leading to lower background and improved precision. |
| Automated Plate Washer with Calibrated Manifold | Ensures consistent removal of unbound plasma proteins, critical for reducing non-specific signal. Must be validated for lack of cross-contamination. |
| Data Analysis Software with 5-PL Curve Fitting | Accurately models the asymmetric sigmoidal standard curves common in immunoassays, especially at upper and lower asymptotes. |
1. Introduction Within a thesis investigating soluble enzyme biomarkers in plasma via ELISA, rigorous data analysis is paramount. This protocol details the process from raw optical density (OD) values to reported concentrations, ensuring accuracy and reproducibility for drug development research.
2. Standard Curve Fitting: Protocol & Data Presentation The standard curve is the analytical backbone for quantifying unknown samples.
2.1. Experimental Protocol for Standard Preparation
- Reconstitution: Reconstitute the lyophilized protein standard with the recommended diluent to create a high-concentration stock.
- Serial Dilution: Perform a 2-fold or 5-fold serial dilution in the sample matrix (e.g., analyte-free plasma or assay buffer) to create 7-8 non-zero standard points. Include a zero concentration standard (background control).
- Plate Layout: Run all standard points in duplicate or triplicate alongside unknown plasma samples.
- Assay Execution: Process according to the specific ELISA kit protocol (coat, block, incubate with samples/detection antibodies, develop, stop).
- Data Acquisition: Read the absorbance (OD) at the appropriate wavelength (e.g., 450 nm, with 570 nm or 620 nm reference).
2.2. Curve Fitting Models The most common models are compared below:
Table 1: Common Standard Curve Fitting Models
| Model | Equation | Best For | Key Parameter |
|---|---|---|---|
| Linear | y = mx + c |
Wide, linear dynamic range. Simple. | Coefficient of Determination (R²) |
| Semi-Log (Log-Linear) | y = m*log10(x) + c |
Data where OD is linear vs. log(Conc). | R² |
| Four-Parameter Logistic (4PL) | y = d + (a-d)/(1+(x/c)^b) |
Standard ELISA sigmoidal curves. Most robust. | Asymptotes (a, d), Slope (b), EC50 (c) |
| Five-Parameter Logistic (5PL) | y = d + (a-d)/(1+(x/c)^b)^g |
Asymmetric sigmoidal curves. | Adds asymmetry factor (g) |
2.3. Fitting Procedure
- Average replicate OD values for each standard.
- Subtract the average OD of the zero standard (background) from all standard and sample readings.
- Using statistical software (e.g., GraphPad Prism, R, ELISAnalysis), plot the mean background-corrected OD (y-axis) against the known standard concentration (x-axis).
- Apply the chosen model (4PL is recommended for most ELISA). The software iteratively fits the curve to minimize the sum of squared residuals.
3. Concentration Calculation of Unknown Samples 3.1. Protocol
- Obtain the mean background-corrected OD for each unknown plasma sample.
- Using the fitted model, interpolate the concentration.
- For 4PL/5PL: Input the sample OD (y-value) into the inverse equation derived from the fit to calculate the concentration (x-value).
- Most software performs this automatically via interpolation.
- Apply the dilution factor (DF) used during sample preparation:
Final [ ] = Interpolated [ ] × DF.
3.2. Quality Control Checks
- Standard Curve R²: Acceptable fit typically requires R² > 0.99.
- Standard Recovery: Calculated concentrations of standards (from the curve) should be within 80-120% of their known value.
- QC Samples: Include internal quality control samples (high, mid, low) in each run. Their calculated concentrations must fall within pre-established acceptance ranges.
4. Data Reporting Report data comprehensively, as per journal and industry standards (e.g., MIAME, ARRIVE).
Table 2: Essential Data Reporting Elements
| Section | Required Information |
|---|---|
| Methods | ELISA kit (catalog #, vendor), curve fitting model & software, acceptance criteria for QC. |
| Results | Final standard curve equation & parameters (e.g., a, b, c, d for 4PL), R², range of quantitation (LLOQ-ULOQ). |
| Sample Data | Sample concentrations in appropriate units (e.g., ng/mL, pg/mL), expressed as Mean ± SD or SEM. |
| QC Data | Recovery data for standards and QC samples, intra- and inter-assay precision (%CV). |
5. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ELISA Biomarker Analysis
| Item | Function & Importance |
|---|---|
| Validated ELISA Kit | Pre-coated plates, matched antibody pairs, and optimized buffers specific to the target biomarker ensure specificity and sensitivity. |
| Recombinant Protein Standard | Precisely quantified standard is critical for generating an accurate calibration curve. Must be identical to the analyte. |
| Matrix (e.g., Normal Plasma) | Used for standard dilution and sample preparation to match the protein and background environment of test samples, minimizing matrix effects. |
| Precision Pipettes & Tips | Essential for accurate serial dilution of standards and reproducible sample/reagent transfer. |
| Plate Reader (Spectrophotometer) | Measures optical density (absorbance) of the assay endpoint. Must be calibrated and have appropriate filters. |
| Data Analysis Software | Specialized software (e.g., GraphPad Prism, SoftMax Pro, R) for robust nonlinear regression fitting of standard curves. |
| Low-Bind Microtubes/Plates | Minimizes analyte loss due to adsorption to plastic surfaces during sample/standard preparation. |
6. Visual Workflow and Pathway Diagrams
Title: ELISA Data Analysis Workflow from Sample to Report
Title: Logical Flow of Concentration Calculation Steps
Solving Common ELISA Challenges: Troubleshooting Guide for Enhanced Sensitivity and Specificity in Plasma
Within the context of a broader thesis on the ELISA detection of soluble enzyme biomarkers in plasma for drug development research, signal quality is paramount. Assay performance issues such as high background, low signal, and poor sensitivity directly compromise data reliability, leading to inaccurate quantification of biomarkers like MMP-9, soluble ACE, or various kinases. These issues can stem from multiple factors across the assay workflow, including sample integrity, reagent performance, and protocol execution. This document provides a structured diagnostic approach, quantitative benchmarks, and detailed protocols to identify and resolve these common problems.
Table 1: Typical Performance Metrics and Problem Indicators for Sandwich ELISAs
| Parameter | Optimal Range | High Background Indicator | Low Signal Indicator | Poor Sensitivity Indicator |
|---|---|---|---|---|
| Absorbance (Blank) | < 0.1 AU | > 0.15 AU | N/A | N/A |
| Signal-to-Noise Ratio | > 10 | < 5 | < 10 | < 10 |
| Assay Dynamic Range | 2-3 logs | Compressed | Compressed | < 1.5 logs |
| Lower Limit of Detection (LLOD) | Consistent with kit claims | Elevated | N/A | > Claimed value by 20% |
| Coefficient of Variation (CV) | < 10% (Intra); < 15% (Inter) | Often high | Often high | May be high |
| Standard Curve R^2 | > 0.99 | May be acceptable | May be acceptable | Often < 0.98 |
Table 2: Primary Causes and Investigative Actions
| Issue | Primary Causes (Sample) | Primary Causes (Reagent/Protocol) | Key Diagnostic Step |
|---|---|---|---|
| High Background | Hemolyzed/lipemic plasma; endogenous enzymes. | Inadequate wash; non-specific antibody binding; contaminated substrate. | Run sample diluent alone; check substrate before incubation. |
| Low Signal | Biomarker degradation; presence of inhibitors. | Depleted/denatured detection Ab; expired/improperly prepared substrate; short incubation times. | Spike recovery with recombinant protein; check reagent activity. |
| Poor Sensitivity | High matrix interference. | Poor antibody affinity; suboptimal conjugate dilution; improper standard reconstitution. | Standard curve in buffer vs. matrix; antibody cross-titration. |
Detailed Diagnostic and Optimization Protocols
Protocol 1: Systematic Troubleshooting Workflow
Objective: To isolate the source of signal abnormalities in a sandwich ELISA for a soluble plasma enzyme biomarker. Materials: See "The Scientist's Toolkit" below. Procedure:
- Visual Inspection: Examine all wells for uniformity. High background is often uneven if due to washing.
- Blank Analysis: Calculate the average absorbance of blank wells (sample diluent only). Values >0.15 AU suggest substrate contamination or plate washing issues.
- Standard Curve Audit: Re-plot the standard curve on a log-log scale. A poor fit (R^2 < 0.98) indicates issues with standard serial dilution, conjugate, or substrate.
- Matrix Effect Test:
- Prepare the standard curve in both the recommended assay buffer and a pooled, normal plasma sample (diluted as per protocol).
- Compare the two curves. A parallel but suppressed curve in plasma suggests matrix interference. A non-parallel curve suggests biomarker interaction with plasma components.
- Spike-and-Recovery Experiment:
- Spike a known concentration of recombinant biomarker into at least three different plasma samples at low, mid, and high points of the standard curve.
- Calculate % Recovery = (Measured Concentration – Endogenous Concentration) / Spiked Concentration * 100.
- Acceptable recovery is typically 80-120%. Low recovery suggests degradation or interference.
- Component Check: Set up a plate omitting one key component at a time (capture antibody, sample, detection antibody, conjugate). This identifies sources of non-specific binding.
Protocol 2: Optimization of Detection Antibody and Conjugate Concentrations
Objective: To maximize signal-to-noise ratio and assay sensitivity by titrating key reagents. Procedure:
- Coat plate with recommended capture antibody. Block.
- Prepare two columns of high and low biomarker concentration (standard).
- Perform a chessboard (cross) titration. Test 2-3 dilutions of the detection antibody (e.g., 1:500, 1:2000, 1:8000) in combination with 2-3 dilutions of the enzyme-conjugate (e.g., 1:1000, 1:4000, 1:16000).
- Develop and read the plate. Select the combination that yields the highest signal for the low concentration standard while maintaining a low background (blank) for the most favorable signal-to-noise ratio.
Protocol 3: Protocol for Mitigating Matrix Interference in Plasma
Objective: To reduce high background and improve sensitivity in complex plasma samples. Procedure:
- Increased Wash Stringency: Add 0.05% Tween-20 to wash buffer (if not present) and increase wash volume to 350 µL/well. Perform 5-6 wash cycles with a 30-second soak per cycle.
- Alternative Blocking: Test alternative blockers (e.g., 1% BSA, 5% non-fat dry milk, or commercial protein-free blockers) in place of the standard blocker. Incubate for 1 hour at room temperature.
- Sample Pre-treatment:
- Dilute plasma samples in assay buffer at a higher ratio than recommended (e.g., 2x further).
- Test sample pre-incubation with a non-interfering protein (e.g., 0.1% IgG) to adsorb heterophilic antibodies.
- For enzymatic biomarkers, include specific, inactive-site inhibitors in the diluent to prevent substrate turnover by the sample analyte.
- Re-run the assay with optimized conditions and re-evaluate standard curve and spike recovery.
Visualizations
Title: ELISA Signal Issue Diagnostic Decision Tree
Title: Sandwich ELISA Workflow with Failure Points
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ELISA Troubleshooting
| Item | Function & Rationale |
|---|---|
| High-Binding, Low-ELISA Plates | Ensures consistent antibody coating, minimizing well-to-well variance. |
| Recombinant Target Biomarker Protein | Critical for preparing standard curves and performing spike-recovery experiments to assess interference. |
| Chromogenic TMB Substrate (Stable Peroxide/Buffer) | Sensitive, common HRP substrate. Must be prepared fresh and protected from light to prevent high background. |
| Plate Sealers | Prevent evaporation and contamination during incubations, which can cause edge effects. |
| Automated Plate Washer | Provides consistent and stringent washing, crucial for reducing background. Soak function enhances removal of unbound material. |
| Blocking Buffers (BSA, Casein, Commercial Blocker) | Reduces non-specific binding. Testing alternatives helps optimize signal-to-noise. |
| Tween-20 (or similar detergent) | Added to wash buffers (typically 0.05%) to reduce hydrophobic interactions and lower background. |
| Precision Pipettes & Calibrated Tips | Accuracy in serial dilutions of standards and reagents is fundamental to a reliable standard curve. |
| Plate Reader with Filter Matching Substrate | For TMB, read at 450 nm with a 540-650 nm reference wavelength to correct for optical imperfections. |
| Heterophilic Antibody Blocking Reagents | Commercially available reagents to mitigate false positives/background from interfering antibodies in plasma. |
1. Introduction & Context
Within the thesis framework on ELISA detection of soluble enzyme biomarkers in plasma for drug development, assay precision is paramount. High intra-assay (within-run) and inter-assay (between-run) Coefficient of Variation (CV%) compromises data reliability, obscures genuine biological variation, and hampers longitudinal study analysis. This document outlines common sources of CV variability and provides optimized protocols to enhance precision.
2. Quantitative Data Summary: Common Sources of ELISA Variability
Table 1: Typical CV% Benchmarks and Impact Factors in Plasma Enzyme Biomarker ELISA
| Variability Factor | Typical Impact on CV% | Acceptable Benchmark |
|---|---|---|
| Pipetting (manual) | Intra-assay: Increases by 5-15% | Use of calibrated, low-dead volume pipettes |
| Sample Handling | Inter-assay: Increases by >10% | Standardized freeze-thaw cycles (max 2), consistent pre-centrifugation |
| Temperature Incubation | Intra-assay: Increases by 8-20% | Use of calibrated, humidified incubators |
| Plate Washing | Intra-assay: Increases by 5-12% | Automated washer with consistent patency/volume check |
| Reagent Lot Variation | Inter-assay: Increases by >15% | Bridging studies with new lots, bulk reagent aliquoting |
| Calibration Curve Fit | Inter-assay: Influences all data | R² > 0.99, 4- or 5-parameter logistic model |
3. Experimental Protocols for Precision Enhancement
Protocol 3.1: Optimized Plasma Sample Pre-Analytical Processing Objective: Minimize pre-analytical variation for soluble enzyme biomarkers (e.g., MMP-9, LOXL2).
- Blood Draw: Use consistent anticoagulant (e.g., EDTA). Process within 30 minutes of collection.
- Centrifugation: Double-centrifuge protocol. First, 2000 x g for 15 mins at 4°C. Transfer plasma to new tube. Second, 10,000 x g for 10 mins at 4°C to remove platelets/microparticles.
- Aliquoting: Aliquot immediately into low-protein-binding microtubes. Avoid repeated freeze-thaw (>2 cycles).
- Storage: Store at -80°C. Do not use frost-free freezers.
Protocol 3.2: Standardized ELISA Run with Internal Controls Objective: Achieve intra-assay CV% < 8% and inter-assay CV% < 12%.
- Reagent Preparation: Thaw all reagents (samples, standards, detection Ab) completely and mix gently by inversion. Standardize equilibration to room temperature (e.g., 22±1°C) for 30 minutes.
- Plate Layout: Include in duplicate or triplicate:
- Freshly reconstituted standard curve.
- Test plasma samples (diluted per optimization).
- Internal Quality Control (QC) Samples: Three levels (Low, Mid, High) from a characterized pooled plasma sample, aliquoted and stored at -80°C. Include on every plate.
- Blank (diluent only).
- Pipetting: Use reverse pipetting for viscous samples and detection antibodies. Employ multi-channel pipettes with regular calibration.
- Incubation: Use a calibrated, humidified incubator. Seal plates with adhesive sealers during all incubations to prevent evaporation and edge effects.
- Washing: Use an automated plate washer. Program for 4-6 washes with a 30-second soak step. Visually confirm uniform wash buffer dispensing and aspiration.
- Signal Development: Quench reaction at the exact same optical density (OD) for the top standard across all runs (e.g., OD 2.5-3.0 for TMB).
- Data Analysis: Use a 5-parameter logistic (5PL) curve fit. Apply validity criteria: QC samples must fall within 2 SD of established mean, and standard curve R² > 0.99.
4. Visualization: Pathways and Workflows
Title: ELISA Precision Optimization Workflow Phases
Title: Root Cause Analysis for High ELISA CV% and Solutions
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for High-Precision Plasma Biomarker ELISA
| Item | Function & Rationale for Precision |
|---|---|
| Low-Protein-Binding Microtubes | Minimizes analyte adsorption to tube walls during sample storage, reducing loss and variability. |
| Calibrated, Low-Dead Volume Pipettes | Ensures accurate and reproducible liquid handling for standards, samples, and reagents. |
| Automated Microplate Washer | Provides consistent and thorough washing across all wells and all runs, reducing background noise variability. |
| Humidified Incubator (Calibrated) | Maintains stable temperature and humidity to prevent evaporation and ensure consistent reaction kinetics. |
| Commercially Prepared, Lyophilized QC Plasma Pools | Provides a stable, matrix-matched material for inter-assay monitoring and run acceptance decisions. |
| Matched Antibody Pair & Blocking Buffer Kit | Optimized reagent compatibility reduces non-specific binding, improving signal-to-noise and reproducibility. |
| Pre-Coated, High-Binding Efficiency Plates | Ensures uniform capture antibody coating lot-to-lot, a major source of inter-assay CV. |
| Stable, Liquid Substrate (e.g., TMB) | Offers consistent kinetics and sensitivity compared to freshly prepared substrates. |
Within the context of a broader thesis on the ELISA detection of soluble enzyme biomarkers in plasma, managing matrix effects is paramount. Plasma is a complex biofluid containing salts, lipids, proteins (like albumin and immunoglobulins), and metabolites that can interfere with assay accuracy by inducing false-positive/negative signals, altering antibody binding kinetics, or modifying the target analyte. This application note details current, proven sample pre-treatment techniques to mitigate these interferences, enabling reliable quantification of biomarkers such as MMP-9, soluble ACE2, or caspase-3.
Key Sample Treatment Techniques: Principles and Data
Dilution and Matrix Matching
The simplest initial approach. A sample dilution reduces interferent concentration but can also dilute the analyte below the limit of detection. Matrix matching involves preparing calibration standards in a surrogate matrix (e.g., analyte-depleted plasma or buffer with added BSA) that mimics the sample's interfering properties.
Table 1: Impact of Dilution on Recovery of MMP-9 in Human Plasma
| Dilution Factor | Nominal MMP-9 Concentration (ng/mL) | Measured Concentration (ng/mL) | % Recovery | Observed Interference Reduction |
|---|---|---|---|---|
| Neat | 10.0 | 7.2 | 72% | High (Lipid/Protein) |
| 1:2 | 5.0 | 4.3 | 86% | Moderate |
| 1:5 | 2.0 | 1.9 | 95% | Low |
| 1:10 | 1.0 | 0.95 | 95% | Minimal |
Immunoaffinity Depletion of Abundant Proteins
Removal of high-abundance proteins (e.g., albumin, IgG) using spin columns or resins with immobilized antibodies reduces non-specific binding and spectral interference. This is critical for low-abundance biomarkers.
Protocol 1.2: High-Abundance Protein Depletion Using Spin Columns
- Materials: Commercial human albumin/IgG depletion spin column, PBS wash buffer, low-salt elution buffer, plasma sample.
- Procedure:
- Condition the spin column per manufacturer's instructions (typically with 3 column volumes of PBS).
- Apply 50-100 µL of undiluted plasma to the column center.
- Centrifuge at 1000 x g for 2 minutes at 4°C. Collect the flow-through (depleted plasma).
- Wash the column with 2 column volumes of PBS and combine with the flow-through.
- The depleted plasma can now be diluted into the ELISA assay buffer. Note: The target biomarker must be validated not to bind to the depletion resins.
Precipitation and Extraction
Useful for removing lipids or concentrating samples. Acid precipitation (e.g., with perchloric acid) or organic solvent precipitation (acetone/ethanol) can remove interfering substances, though risk of co-precipitating the target analyte exists.
Table 2: Comparison of Precipitation Methods for Lipid Removal from Plasma
| Method | Target Interference | Typical Recovery of Soluble ACE2 | Key Advantage | Key Limitation |
|---|---|---|---|---|
| Polyethylene Glycol (PEG) Precipitation | Lipoproteins, IgM | 85-90% | Mild, retains protein conformation | Incomplete removal of some lipids |
| Organic Solvent (Acetone) Extraction | All lipids, some proteins | 70-80% | Efficient lipid removal | Can denature some protein biomarkers |
| Acid Precipitation (Perchloric Acid) | Macroproteins, Fibrin | 60-75% | Effective for stable, small proteins/enzymes | Harsh, unsuitable for many biomarkers |
Solid-Phase Extraction (SPE)
SPE using C18 or mixed-mode sorbents selectively captures analytes or interferents. It is highly effective for removing salts, phospholipids (a major source of ionization suppression in downstream MS), and metabolites.
Protocol 1.4: Phospholipid Removal via SPE for Plasma ELISA Samples
- Materials: 96-well mixed-mode cation-exchange SPE plate, vacuum manifold, methanol, water, 2% formic acid, elution solvent (methanol:acetonitrile 1:1 with 5% ammonium hydroxide).
- Procedure:
- Condition each well with 200 µL methanol, then 200 µL water. Do not let the sorbent dry.
- Acidify 100 µL plasma with 20 µL of 2% formic acid. Load onto the conditioned well.
- Wash with 200 µL of 5% methanol in water to remove salts and polar interferences.
- Elute the target analyte (if retained) or discard eluate (if removing interferents). For phospholipid removal, the phospholipids are retained while many protein biomarkers pass through in the load and wash. Validate per analyte.
- Lyophilize the eluent if concentration is needed and reconstitute in ELISA sample diluent.
Digestion and Denaturation
For proteolytic enzyme biomarkers, controlled denaturation can inactivate endogenous proteases that might degrade detection antibodies. Heat treatment (e.g., 56°C for 30 min) can also inactivate complement enzymes that cause interference.
Integrated Workflow for Plasma Sample Preparation
Integrated Workflow for Plasma ELISA Sample Prep
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Overcoming Plasma Interferences in ELISA
| Item & Example Product | Primary Function in Mitigating Interference |
|---|---|
| Analyte-Depleted/Stripped Plasma (e.g., Charcoal-stripped human plasma) | Serves as an ideal matrix for preparing calibration standards, eliminating the "matrix mismatch" problem. |
| Immunoaffinity Depletion Columns (e.g., Albumin & IgG Removal Spin Kits) | Rapidly removes the two most abundant plasma proteins, reducing non-specific binding and signal quenching. |
| Mixed-Mode Solid Phase Extraction (SPE) Plates (e.g., HybridSPE-PPT) | Selectively binds phospholipids and small molecule interferents while allowing protein biomarkers to pass through. |
| Stabilizing/Protease Inhibitor Cocktails (e.g., EDTA, AEBSF, Leupeptin added to collection tubes) | Preserves the integrity of the soluble enzyme biomarker by inhibiting endogenous plasma proteases pre-assay. |
| Blocking Agents for Assay Buffer (e.g., Casein, BSA, proprietary commercial blockers) | Reduces non-specific binding of plasma components to the ELISA plate well surface and detection antibodies. |
| Heterophilic Antibody Blocking Reagents (e.g., Polymeric Blocking Sera) | Binds human anti-animal antibodies (HAAA) and rheumatoid factor in plasma, preventing false-positive signals. |
Detailed Experimental Protocol: Comprehensive Sample Pre-Treatment
Protocol 4: Integrated Protocol for Sensitive Detection of Soluble Caspase-3 in Heparinized Plasma
- Objective: To accurately quantify low levels of soluble caspase-3 activity via ELISA by removing lipids, heterophilic antibodies, and abundant proteins.
Materials: Heparin plasma sample, heterophilic blocking reagent (HBR), 0.22 µm centrifugal filter (10kDa MWCO), commercial albumin/IgG depletion kit, 1x PBS, ELISA sample diluent.
Procedure:
- Initial Treatment: Mix 100 µL of plasma with 20 µL of heterophilic blocking reagent. Incubate at room temperature for 60 minutes with gentle agitation.
- Abundant Protein Depletion: Follow Protocol 1.2 using the treated sample from step 1. Collect the flow-through.
- Concentration and Buffer Exchange: Apply the flow-through to a pre-rinsed (with PBS) 10 kDa MWCO centrifugal filter. Centrifuge at 12,000 x g at 4°C until volume is reduced to ~50 µL. Discard the filtrate.
- Buffer Exchange: Add 200 µL of ELISA sample diluent to the filter and centrifuge again to ~50 µL. Repeat this dilution/centration step twice. This removes salts and exchanges the buffer into the optimal ELISA matrix.
- Final Reconstitution: Recover the final concentrated sample by inverting the filter into a clean tube and spinning at 1000 x g for 2 minutes.
- ELISA Analysis: Perform a 1:2 final dilution in ELISA diluent and assay immediately according to the kit protocol. Prepare standards in the same diluent, spiked into analyte-depleted plasma if possible.
Validation: Always perform spike-and-recovery experiments (e.g., spiking known amounts of recombinant caspase-3 into multiple plasma lots) and parallelism assays (diluting a high-concentration sample and confirming linearity) to validate the entire pre-treatment protocol.
Application Notes
Within the broader thesis focused on the detection of soluble enzyme biomarkers in plasma for diagnostic and therapeutic monitoring, the optimization of ELISA reagents and parameters is critical. The performance of a sandwich ELISA is dictated by the specificity and affinity of the matched antibody pair, the precise concentration of the detection conjugate, and the kinetics of antigen-antibody binding during incubation. Suboptimal conditions lead to high background, low signal-to-noise ratios, poor sensitivity, and unreliable quantification, which is particularly detrimental when measuring low-abundance enzymes in the complex plasma matrix. This document provides a data-driven framework for systematically optimizing these key variables to achieve robust, reproducible assays for translational research and drug development.
Antibody Pair Selection
The cornerstone of a sensitive sandwich ELISA is a well-matched antibody pair. The capture and detection antibodies must bind to distinct, non-overlapping epitopes on the target enzyme to avoid steric hindrance. For soluble enzyme biomarkers, which may exist in zymogen, active, or inhibitor-complexed forms, epitope selection is also crucial for capturing the relevant isoform.
Key Considerations:
- Epitope Mapping: Prefer monoclonal antibodies (mAbs) targeting linear epitopes distant from the enzyme's active site to avoid interference with detection.
- Affinity: Antibodies with dissociation constants (Kd) in the low nanomolar range are ideal for capturing low-concentration analytes.
- Cross-Reactivity: Verify minimal cross-reactivity with related enzymes or plasma proteins.
- Matched Pair Validation: Commercial "matched pairs" are pre-validated, but in-house pairs require checkerboard titration.
Conjugate Concentration Optimization
The enzyme-conjugated detection antibody (e.g., HRP or ALP) is a major source of signal amplification. Excessive conjugate increases background, while insufficient conjugate reduces sensitivity.
Incubation Time Optimization
Incubation times for the sample and detection antibody impact binding equilibrium. Longer incubations can increase signal but also prolong assay time and potentially increase non-specific binding.
General Trade-off: A balance must be struck between assay sensitivity, dynamic range, total runtime, and reagent cost.
Experimental Protocols
Protocol 1: Checkerboard Titration for Antibody Pair and Conjugate Optimization
Objective: To determine the optimal working concentrations for capture antibody, detection antibody, and enzyme conjugate in a single, systematic experiment.
Materials:
- Coating Buffer (0.1 M Carbonate-Bicarbonate, pH 9.6)
- Blocking Buffer (1% BSA or 5% non-fat dry milk in PBST)
- Wash Buffer (PBS with 0.05% Tween-20)
- Assay Diluent (PBS with 0.1% BSA)
- Recombinant target enzyme standard (high and low concentration)
- Candidate capture and detection antibodies
- HRP-conjugated secondary antibody (if using a non-conjugated detection Ab)
- TMB Substrate Solution
- Stop Solution (1M H2SO4 or 2M HCl)
- 96-well microplate and plate reader
Procedure:
- Capture Antibody Coating: Prepare a dilution series of the capture antibody (e.g., 10, 5, 2.5, 1.25 µg/mL) in coating buffer. Add 100 µL per well to a 96-well plate in a grid pattern. Seal and incubate overnight at 4°C.
- Washing & Blocking: Aspirate and wash wells 3x with wash buffer. Add 200 µL blocking buffer per well. Incubate for 1-2 hours at room temperature (RT). Wash 3x.
- Antigen Addition: Prepare two antigen solutions in assay diluent: a "high" concentration (near the top of the expected range) and a "low" concentration (near the limit of detection). Add 100 µL per well to the appropriate columns/rows of the checkerboard. Include blank wells (diluent only). Incubate for 2 hours at RT. Wash 3x.
- Detection Antibody Titration: Prepare a dilution series of the detection antibody (e.g., 1, 0.5, 0.25, 0.125 µg/mL) in assay diluent. If the detection Ab is directly conjugated, proceed. If not, use a fixed concentration for this step. Add 100 µL per well according to the checkerboard layout. Incubate for 1-2 hours at RT. Wash 3x.
- Conjugate Addition (if needed): If using an unconjugated detection Ab, prepare a dilution series of the enzyme-conjugated secondary antibody (e.g., 1:2000 to 1:16000). Add 100 µL per well. Incubate for 1 hour at RT, protected from light. Wash 5x.
- Signal Detection: Add 100 µL TMB substrate per well. Incubate for 5-15 minutes in the dark. Stop the reaction with 100 µL stop solution.
- Measurement: Read absorbance immediately at 450 nm (for TMB).
Data Analysis: Calculate the signal-to-noise (S/N) ratio for each condition: (Mean Signal at High Antigen) / (Mean Signal at Zero Antigen). The optimal combination is the one that yields the highest S/N ratio for the low antigen concentration while maintaining a low background and a high maximal signal for the high antigen concentration.
Protocol 2: Incubation Time Kinetic Study
Objective: To determine the optimal incubation times for antigen and detection antibody binding.
Materials: (As in Protocol 1, using optimized antibody/conjugate concentrations)
Procedure (Antigen Incubation Time):
- Coat and block the plate with optimized capture antibody concentration.
- Add the target antigen at low, mid, and high concentrations to separate wells.
- Incubate the antigen for different time points (e.g., 30 min, 60 min, 90 min, 120 min) at RT with gentle shaking.
- Wash and continue the assay using the optimized detection antibody and conjugate incubation times.
- Plot absorbance vs. antigen incubation time for each antigen concentration.
Procedure (Detection Antibody Incubation Time):
- Proceed through the antigen incubation step using the optimized time.
- Add the detection antibody and incubate for different time points (e.g., 30, 60, 90, 120 min).
- Continue with conjugate, substrate, and stopping.
- Plot absorbance vs. detection antibody incubation time.
Data Analysis: Identify the time point where the signal for the low-concentration analyte reaches a plateau (near equilibrium) without a significant increase in the background signal. This is the optimal, efficient incubation time.
Data Presentation
Table 1: Checkerboard Titration Results for MMP-9 ELISA (Sample Data) Signal-to-Noise (S/N) Ratio for Low Antigen (5 pg/mL) Concentration
| Capture Ab [µg/mL] | Detection Ab [µg/mL] | |||
|---|---|---|---|---|
| 0.125 | 0.25 | 0.5 | 1.0 | |
| 1.25 | 2.1 | 3.5 | 5.8 | 6.1 |
| 2.5 | 3.8 | 7.2 | 12.5 | 11.8 |
| 5.0 | 4.1 | 8.9 | 15.3 | 14.7 |
| 10.0 | 3.5 | 7.5 | 13.1 | 12.0 |
Optimal Condition Selected: Capture Ab at 5 µg/mL, Detection Ab at 0.5 µg/mL (S/N = 15.3).
Table 2: HRP-Conjugate Titration Optimization Background Subtracted Signal for High Antigen (1000 pg/mL)
| Conjugate Dilution | Mean OD (450 nm) | Background OD | Net Signal |
|---|---|---|---|
| 1:1,000 | 3.521 | 0.450 | 3.071 |
| 1:2,000 | 2.987 | 0.210 | 2.777 |
| 1:4,000 | 2.512 | 0.105 | 2.407 |
| 1:8,000 | 1.654 | 0.055 | 1.599 |
| 1:16,000 | 0.890 | 0.035 | 0.855 |
Optimal Condition Selected: 1:4,000 dilution (High net signal with low background).
Table 3: Incubation Time Kinetic Analysis Signal Development for Low Antigen (10 pg/mL)
| Incubation Step | Time (min) | Net OD (450 nm) | % of Max Signal |
|---|---|---|---|
| Antigen Binding | 30 | 0.255 | 68% |
| 60 | 0.345 | 92% | |
| 90 | 0.375 | 100% | |
| 120 | 0.378 | 101% | |
| Detection Ab Binding | 30 | 0.310 | 78% |
| 60 | 0.385 | 97% | |
| 90 | 0.395 | 100% | |
| 120 | 0.398 | 101% |
Optimal Conditions Selected: Antigen incubation = 90 min, Detection Ab incubation = 60 min.
Mandatory Visualizations
Diagram 1: Workflow for ELISA Reagent Optimization (80 chars)
Diagram 2: Sandwich ELISA Signal Generation Steps (77 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for ELISA Optimization in Plasma Biomarker Research
| Item | Function & Rationale |
|---|---|
| High-Affinity Matched Antibody Pairs | Pre-validated pairs ensure distinct epitope binding, minimizing steric hindrance and maximizing sensitivity for the target enzyme. Critical for specificity in complex plasma. |
| Recombinant Enzyme Standard | Provides a pure, quantifiable antigen for generating a standard curve and for use in optimization protocols (checkerboard, recovery). Must be enzymatically active or representative. |
| Matrix-Matched Assay Diluent | Diluent containing inert protein (BSA) and potential protease inhibitors. Mimics plasma composition to reduce non-specific binding and stabilize labile enzyme biomarkers. |
| HRP or ALP Conjugates | Enzyme-linked secondary antibodies or streptavidin for signal amplification. Choice depends on required sensitivity and substrate compatibility. HRP-TMB is common. |
| Low-Binding Microplates | Plates with surface treatment to maximize protein (capture Ab) binding consistency and minimize passive adsorption of other reagents, improving well-to-well reproducibility. |
| Precision Multichannel Pipettes | Essential for consistent reagent delivery across optimization titrations, reducing volumetric error which is a major source of inter-assay variability. |
| Plate Washer (Automated) | Provides consistent and thorough washing to remove unbound plasma proteins and reagents, a key step in minimizing background signal. Manual washing is variable. |
| Kinetic Plate Reader | Measures absorbance (e.g., 450nm for TMB). Capable of reading multiple plates/kinetics is ideal for high-throughput optimization and validation experiments. |
In the context of ELISA detection of soluble enzyme biomarkers in plasma for drug development research, generating a reliable standard curve is fundamental for accurate quantification. Failures such as the high-dose hook effect, poor linearity, and statistical outliers compromise data integrity, leading to incorrect biomarker concentration estimates. This document provides detailed application notes and protocols to identify, troubleshoot, and resolve these common issues.
The High-Dose Hook Effect
The hook effect, or prozone effect, occurs at extremely high analyte concentrations where excess analyte saturates both capture and detection antibodies, preventing the formation of the necessary "sandwich" complex. This results in a falsely low signal, causing the standard curve to "hook" downward at high concentrations.
Protocol 1.1: Identifying the Hook Effect
Objective: To diagnose the presence of a high-dose hook effect in a sandwich ELISA. Materials: High-concentration purified biomarker standard, assay diluent, ELISA kit components. Procedure:
- Prepare the standard per kit instructions, generating the typical 7-point curve.
- Additionally, prepare 3-4 serial dilutions (e.g., 1:10, 1:100, 1:1000) of the highest concentration standard point.
- Run all samples (standard curve and extra high-dose dilutions) in duplicate on the same plate.
- Plot all measured signals against the theoretical concentration (accounting for dilution). Interpretation: If the signal from the diluted high-concentration samples is higher than that of the undiluted sample, a hook effect is confirmed.
Protocol 1.2: Resolving the Hook Effect
Objective: To establish an accurate standard curve in the presence of a hook effect. Procedure:
- Perform the identification protocol (1.1).
- Exclude the points showing signal decrease from the standard curve fit.
- Use the correctly measured signals from the diluted high-concentration samples to redefine the upper asymptote of the curve.
- Re-fit the logistic (4- or 5-parameter) curve using the remaining points. Always report samples that required dilution.
Poor Linearity and Curve Fit Issues
Poor linearity after log transformation or a low R² value indicates an improper fit, often due to assay range limitations, reagent degradation, or pipetting errors.
Protocol 2.1: Assessing and Improving Linearity
Objective: To achieve a linear log-linear plot with R² > 0.99. Materials: Freshly prepared standards, calibrated pipettes, quality-controlled reagents. Procedure:
- Re-prepare Standards: Use fresh stock and a serial dilution with a large dilution factor (e.g., 1:4 or greater) and adequate mixing between steps.
- Validate Pipettes: Calibrate micropipettes used for standard preparation.
- Check Reagents: Ensure detection antibody and enzyme conjugate are within expiration date and have been stored correctly.
- Re-run the standard curve in triplicate.
- Fit Data: Apply a 4-parameter logistic (4PL) or 5-parameter logistic (5PL) nonlinear regression model. For the linear portion, use a weighted linear regression.
Table 1: Impact of Dilution Factor on Standard Curve Linearity
| Dilution Factor | Dynamic Range Covered | Typical R² (4PL Fit) | Recommended Use |
|---|---|---|---|
| 1:2 | Narrow | 0.970-0.990 | Preliminary range-finding |
| 1:4 | Broad | 0.990-0.998 | Optimal for most assays |
| 1:10 | Very Broad | 0.995-0.999 | For analytes with wide expected range |
Managing Statistical Outliers
Outliers in standard points distort the curve fit. They must be identified objectively, not arbitrarily.
Protocol 3.1: Objective Outlier Identification Using Grubbs' Test
Objective: To statistically identify and remove significant outliers from replicate standard measurements. Procedure:
- Run the standard curve with a minimum of n=3 replicates per point.
- Calculate the mean and standard deviation (SD) for each concentration point's replicates.
- For each point, apply the Grubbs' test (G = |suspect value - mean| / SD).
- Compare the calculated G to the critical G value (for n=3, G_crit = 1.155 at α=0.05).
- If G > G_crit, the value is a statistical outlier. Remove it and recalculate the mean/SD for that point.
- Re-fit the curve using the remaining replicate values.
Table 2: Grubbs' Critical Values (α=0.05) for Common Replicate Numbers
| Number of Replicates (n) | Critical G Value |
|---|---|
| 3 | 1.155 |
| 4 | 1.481 |
| 5 | 1.715 |
| 6 | 1.887 |
| 8 | 2.126 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Robust ELISA Standard Curves
| Item | Function & Importance |
|---|---|
| High-Purity Biomarker Standard | Lyophilized recombinant protein with known concentration; essential for accurate calibration. |
| Matrix-Matched Diluent | Diluent containing analyte-free plasma or serum; minimizes matrix interference in plasma samples. |
| Stabilized Chromogenic TMB | Tetramethylbenzidine substrate with controlled reaction stop; ensures consistent color development. |
| Pre-coated ELISA Plates (Lot-Certified) | Plates with validated coating consistency; reduces inter-plate variability. |
| High-Affinity, Matched Antibody Pair | Capture and detection antibodies targeting non-overlapping epitopes; ensures specificity and sensitivity. |
| Precision Microplate Washer | Removes unbound material consistently; critical for reducing background and variability. |
| Plate Reader with Pathlength Correction | Corrects for well-to-well volume differences; improves accuracy of endpoint readings. |
Visualizations
Application Notes: Optimizing ELISA for Soluble Enzyme Biomarker Detection in Plasma
Accurate quantification of soluble enzyme biomarkers (e.g., MMPs, caspases, kinases) in plasma via ELISA is critical for translational research and drug development. Pre-analytical and analytical variability directly compromise data integrity. These Application Notes detail standardized protocols to mitigate key sources of error, ensuring reproducible and reliable results.
Pipetting Techniques for Reproducible Plasma Handling
Protocol: Precision Pipetting for Plasma Samples and Reagents
- Objective: To minimize volumetric errors during sample dilutions and reagent dispensing.
- Materials: Calibrated single- and multi-channel micropipettes, low-retention pipette tips, microplates, plasma samples, assay diluent.
- Pre-Procedure:
- Equipment Check: Verify pipette calibration certificates (<6 months old). Perform a quick gravimetric check for critical volumes (e.g., 10 µL, 100 µL).
- Thermal Equilibration: Allow plasma samples and all reagents to equilibrate to room temperature (18-25°C) for 30 minutes, protected from light. This reduces viscosity-induced errors.
- Pre-wetting: For viscous samples like plasma, pre-wet pipette tips by aspirating and dispensing the sample or diluent 2-3 times before taking the final volume.
- Procedure for Sample Dilution:
- Use the forward pipetting technique for plasma and standard curve dilutions. Depress the plunger to the first stop, immerse the tip 2-3 mm into the liquid, aspirate slowly, and dispense to the second stop against the side of the well.
- For homogeneous reagent addition (e.g., detection antibody, substrate), the reverse pipetting technique is recommended for volumes <50 µL. Depress the plunger past the first stop to the second stop, aspirate, then dispense to the first stop. The excess remains in the tip.
- For multi-channel pipetting, ensure tips are seated evenly and the pipette is held perpendicular to the plate. Aspirate and dispense using smooth, consistent plunger pressure.
- Mix diluted samples and reagents by pipetting up and down 5-7 times or using a plate shaker (500 rpm for 1 minute).
Table 1: Impact of Pipetting Technique on ELISA Coefficient of Variation (CV%)
| Technique | Use Case | Typical Intra-Assay CV% | Key Consideration |
|---|---|---|---|
| Forward Pipetting | Aqueous buffers, standards, plasma dilutions (>50 µL) | 2-5% | Must be used for viscous or foaming liquids. |
| Reverse Pipetting | Detergents, viscous detection antibodies, small volumes (<50 µL) | 1-3% | Reduces error from tip wetting; consumes more reagent. |
| Multi-Channel (Aligned) | Adding conjugate, substrate to full plates | 3-6% | Dependent on tip seal consistency and user technique. |
Plate Washer Maintenance for Consistent Washing
Protocol: Daily and Weekly Maintenance for ELISA Plate Washers
- Objective: To prevent carry-over, ensure complete well aspiration, and deliver consistent wash buffer volumes.
- Materials: Microplate washer, 70% ethanol, 10% bleach (sodium hypochlorite), distilled water, calibration plate (if available), wash buffer.
- Daily Start-Up Procedure:
- Prime the system: Run a prime/debubble cycle with distilled water followed by wash buffer.
- Visual inspection: Check all aspiration needles for clogs or bends. Manually wipe needles with a lint-free cloth moistened with distilled water.
- Perform a test wash on an empty plate. Observe for uniform dispensing, correct needle height (1-2 mm above well bottom), and complete aspiration.
- Weekly Deep-Clean & Calibration Procedure:
- Decontamination: Run a full system wash with 10% bleach (5-minute dwell), followed by 3 cycles with distilled water.
- Degreasing: Run a cycle with 70% ethanol, followed by 3 cycles with distilled water.
- Volume Calibration: Using a precision balance, weigh a clean dry plate. Program the washer to dispense a known volume (e.g., 300 µL) to all wells. Re-weigh the plate. (Mass in mg ≈ Volume in µL). Adjust washer syringe or pump settings if deviation is >5%.
- Aspiration Check: Dispense a colored solution (e.g., dilute Coomassie blue). After aspiration, visually inspect wells for residual liquid. Residual volume should be ≤5 µL per well.
Table 2: Troubleshooting Common Plate Washer Failures in ELISA
| Problem | Potential Cause | Solution |
|---|---|---|
| High Background | Incomplete aspiration, protein buildup on needles | Perform deep-clean; adjust needle height; increase wash cycles/dwell time. |
| High Well-to-Well Variability | Clogged or misaligned needles, uneven dispensing | Manually clean needles; run prime/debubble; calibrate dispense volume. |
| Low Signal | Excessive aspiration, needle touching well bottom | Raise needle height; check waste vacuum pressure. |
Reagent Stability and Storage for Biomarker ELISAs
Protocol: Validating and Monitoring Reagent Stability
- Objective: To define shelf-life and in-use stability for critical ELISA components.
- Materials: ELISA kit components (capture/detection antibodies, conjugate, standards), plasma pools, albumin, protease inhibitor cocktails.
- Procedure: Stability Testing for Critical Reagents:
- Stock Standard Aliquoting: Upon receipt, reconstitute the biomarker standard and aliquot into single-use vials. Store at ≤ -70°C. Avoid freeze-thaw cycles.
- In-Use Stability Test:
- Prepare a working aliquot of detection antibody or conjugate as per kit instructions.
- Use this aliquot over a defined period (e.g., 7 days).
- On Day 1 and Day 7, run a parallel ELISA using a stable, frozen plasma quality control (QC) sample.
- Calculate the recovery: (Mean Concentration Day 7 / Mean Concentration Day 1) * 100%. Recovery of 85-115% indicates acceptable in-use stability.
- Plasma Sample Pre-Analytical Stability: For enzyme biomarkers, add protease inhibitors to collection tubes. Test freeze-thaw stability by assaying a plasma pool after 1, 2, and 3 freeze-thaw cycles. A >15% change from cycle 1 indicates instability.
Table 3: Recommended Storage and Stability for ELISA Components
| Reagent | Recommended Storage | In-Use Stability (2-8°C) | Key Risk |
|---|---|---|---|
| Coated Plate | Sealed with desiccant, 4°C | 4 weeks (varies by kit) | Loss of capture antibody binding capacity. |
| Lyophilized Standard | Desiccated, ≤ -20°C | N/A | Hygroscopic degradation; inaccurate reconstitution. |
| Reconstituted Standard | Aliquoted, ≤ -70°C | 24 hours (if stored at 4°C) | Adsorption to vial, enzyme degradation. |
| Detection Antibody | Glycerol aliquots, ≤ -20°C | 1 week (if containing preservative) | Microbial growth, aggregation. |
| Enzyme-Conjugate | With stabilizer, 4°C | Manufacturer specified (often 4-8 weeks) | Loss of enzymatic activity. |
| Plasma Sample (for enzymes) | Aliquoted with inhibitors, ≤ -70°C | Avoid repeated thawing | Proteolysis, complex dissociation. |
The Scientist's Toolkit: Key Reagent Solutions
| Item | Function in Soluble Enzyme Biomarker ELISA |
|---|---|
| Protease Inhibitor Cocktail | Added to plasma post-collection to prevent endogenous proteolysis of the target biomarker. |
| Blocking Buffer (e.g., 5% BSA/PBS) | Blocks non-specific binding sites on the plate and plasma components, reducing background. |
| Matrix-Matched Calibrators | Standards prepared in diluted, analyte-free plasma or serum to match sample matrix and improve accuracy. |
| Low-Binding Microcentrifuge Tubes & Tips | Minimizes adsorptive loss of low-abundance biomarkers during sample processing. |
| Stable Chemiluminescent Substrate | Provides a sensitive, steady light output for enzymatic detection, crucial for dynamic range. |
| Wash Buffer with 0.05% Tween-20 | Non-ionic detergent reduces non-specific binding during wash steps. Must be freshly prepared. |
Visualization: ELISA Workflow for Plasma Enzyme Biomarkers
Title: ELISA workflow with key consistency practices.
Ensuring Data Credibility: Validation Parameters and Comparative Analysis with Alternative Biomarker Platforms
Within plasma biomarker research, the development of a FIT-for-purpose (FFP) ELISA for soluble enzyme quantification requires rigorous validation. FFP validation balances scientific rigor with practical resource allocation, ensuring data is reliable for its intended non-clinical or early clinical use. This document outlines core validation parameters—Sensitivity (LLOQ), Specificity, Accuracy, and Precision—framed within the context of detecting soluble protease enzymes (e.g., MMP-9, Caspase-3) in human plasma. These parameters establish the assay's fundamental performance characteristics, forming the basis for generating credible pharmacodynamic or diagnostic data in drug development.
Sensitivity: Lower Limit of Quantification (LLOQ)
Sensitivity is defined as the lowest analyte concentration that can be quantitatively measured with acceptable accuracy and precision (typically ±20% bias and ≤20% CV). The LLOQ is critical for detecting low-abundance enzyme biomarkers in circulation.
Protocol for LLOQ Determination:
- Prepare a dilution series of the recombinant enzyme standard in analyte-free matrix (e.g., charcoal-stripped plasma or appropriate buffer) to bracket the expected LLOQ.
- Analyze a minimum of 6 replicate samples at each low concentration level across at least three independent runs.
- Calculate the mean observed concentration, accuracy (% bias), and precision (%CV) for each level.
- The LLOQ is the lowest concentration where:
- Mean accuracy is within 80-120% of the nominal value.
- Precision (CV) is ≤20%.
- The signal-to-noise ratio is typically >5.
Table 1: Example LLOQ Determination Data for Hypothetical MMP-9 ELISA
| Nominal Conc. (pg/mL) | Mean Observed (pg/mL) | Accuracy (% Bias) | Precision (%CV) | Meets Criteria? |
|---|---|---|---|---|
| 15 | 12.3 | -18.0% | 22.5% | No (CV >20%) |
| 25 | 23.8 | -4.8% | 18.2% | Yes |
| 50 | 52.1 | +4.2% | 15.7% | Yes |
Specificity & Selectivity
Specificity is the ability to measure the analyte unequivocally in the presence of other components, such as homologous enzymes, precursors, zymogens, or matrix interferents (e.g., heterophilic antibodies).
Protocol for Interference/Selectivity Assessment:
- Cross-Reactivity: Spike high concentrations of structurally similar enzymes (e.g., MMP-2 for an MMP-9 assay) into the matrix and measure. Calculate % cross-reactivity.
- Parallelism: Serially dilute endogenous analyte from several individual plasma samples with high analyte levels. Assess if the measured concentration dilutes linearly and proportionally to the standard curve.
- Spike Recovery in Individual Matrices: Spike the analyte at low, mid, and high concentrations into at least 10 individual plasma samples from the target population. Calculate % recovery.
Table 2: Specificity and Selectivity Assessment Parameters
| Test Parameter | Experimental Approach | Acceptance Criterion (Example) |
|---|---|---|
| Cross-Reactivity | Spike 1000 ng/mL of homologous enzyme | ≤1% cross-reactivity relative to target analyte signal |
| Parallelism (Linearity) | Dilution of endogenous samples | % Bias of back-calculated concentrations ≤±25% per level |
| Spike Recovery (Selectivity) | Spike analyte into 10 individual plasma samples at 3 concentrations | Mean recovery within 80-120% for ≥80% of samples |
Accuracy
Accuracy reflects the closeness of agreement between the measured value and the true value. For FFP ELISA, it is assessed via spike/recovery experiments.
Protocol for Accuracy Assessment:
- Prepare QC samples by spiking known concentrations of the recombinant enzyme standard into the relevant plasma matrix. Use at least 3 concentrations (low, mid, high) spanning the assay range.
- Analyze each QC sample in a minimum of 5-6 replicates per run over at least 3 separate days.
- Calculate the mean observed concentration and the percent recovery for each level.
- % Recovery = (Mean Observed Concentration / Nominal Spiked Concentration) x 100
Precision
Precision describes the closeness of agreement between a series of measurements. It includes repeatability (intra-assay) and intermediate precision (inter-assay).
Protocol for Precision Assessment:
- Analyze QC samples (low, mid, high) in replicates (n=5-6) within the same run to determine repeatability.
- Analyze the same QC samples in duplicates or triplicates across a minimum of 3 independent runs performed by different analysts on different days to determine intermediate precision.
- Calculate the coefficient of variation (%CV) for each level.
- %CV = (Standard Deviation / Mean) x 100
Table 3: Combined Accuracy and Precision Data Summary
| QC Level | Nominal Conc. (ng/mL) | Intra-Assay (n=6) | Inter-Assay (3 runs, n=18) | ||
|---|---|---|---|---|---|
| Accuracy (%) | CV (%) | Accuracy (%) | CV (%) | ||
| Low | 1.0 | 92.5 | 8.2 | 94.7 | 12.1 |
| Medium | 25.0 | 102.3 | 5.1 | 98.8 | 9.8 |
| High | 75.0 | 96.8 | 4.7 | 97.5 | 7.5 |
Research Reagent Solutions Toolkit
Table 4: Essential Materials for Soluble Enzyme ELISA Validation
| Item/Reagent | Function & Rationale |
|---|---|
| Recombinant Enzyme Standard | Highly purified, quantifiable protein for generating the standard curve. Serves as the reference for all quantitative measurements. |
| Charcoal-Stripped Plasma | Depleted of endogenous biomarkers; used as an "analyte-free" matrix for preparing standard dilutions and assessing matrix effects. |
| Target-Specific Capture/Detection Antibody Pair | Monoclonal antibodies binding non-overlapping epitopes ensure assay specificity for the target enzyme. |
| Enzyme-Conjugated Streptavidin (e.g., HRP-Streptavidin) | Binds biotinylated detection antibodies, enabling signal amplification through enzymatic reaction. |
| Stable Chemiluminescent or Chromogenic Substrate | Generates measurable signal proportional to the amount of captured analyte. Critical for sensitivity. |
| Protease Inhibitor Cocktail | Added to plasma collection tubes to prevent in vitro degradation or activation of the target enzyme post-sampling. |
| Heterophilic Antibody Blocking Reagent | Reduces false-positive/false-negative signals caused by interfering antibodies in patient samples. |
Visualizations
FIT-for-Purpose Assay Validation Workflow
Sandwich ELISA Signal Generation Pathway
Assessing Dilutional Linearity, Parallelism, and Spike-Recovery in the Plasma Matrix
This application note details critical validation experiments for quantifying soluble enzyme biomarkers in plasma using ELISA. Within the broader thesis on biomarker discovery and validation for inflammatory and fibrotic diseases, establishing robust quantitative performance in the complex plasma matrix is paramount. These assays (dilutional linearity, parallelism, and spike-recovery) confirm the assay's accuracy, specificity, and freedom from matrix effects, ensuring reliable detection of biomarkers like soluble proteases, kinases, or other enzymatically active proteins implicated in disease pathogenesis.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in the Experiment |
|---|---|
| Human Plasma Matrix (Pooled) | Serves as the primary test matrix. It is essential for assessing matrix effects and establishing baseline signals. Should be screened for low endogenous levels of the target analyte. |
| Purified Target Biomarker Standard | High-purity, well-characterized recombinant or native protein. Used to generate the standard curve and as the spike for recovery and parallelism experiments. |
| Validated ELISA Kit/Components | Includes pre-coated capture antibody, detection antibody, streptavidin-HRP (if biotinylated), and substrate (e.g., TMB). Must have demonstrated specificity for the soluble enzyme biomarker. |
| Matrix-Compatible Diluent | A buffer specifically formulated to mimic plasma's pH and ionic strength while minimizing nonspecific binding and maintaining analyte stability. Often contains carrier proteins (e.g., BSA) and blockers. |
| Assay Buffer/Diluent | The standard diluent provided with the ELISA kit, used for reconstituting standards and diluting samples as per the standard protocol. |
| Sample Collection Tubes (e.g., EDTA) | Specifies the anticoagulant used for plasma collection, which can influence analyte stability and assay performance. Consistency is critical. |
| Plate Reader (Absorbance/Fluorescence) | For quantifying the final assay signal. Must be calibrated and capable of reading the appropriate wavelength (e.g., 450nm for TMB). |
Experimental Protocols
Protocol: Dilutional Linearity Assessment
Objective: To determine if a sample can be diluted within the assay's dynamic range and yield proportional results, indicating a lack of matrix interferences at the tested dilutions.
Procedure:
- Sample Preparation: Prepare a high-concentration plasma sample (expected to be above the assay's upper limit of quantification - ULOQ) from a disease-state donor pool.
- Serial Dilution: Perform a serial dilution (e.g., 1:2, 1:4, 1:8, 1:16, 1:32) of the high-concentration sample using the matrix-compatible diluent. Ensure the final dilution falls within the assay's standard curve range.
- Assay Execution: Analyze all diluted samples alongside the standard curve in the same ELISA plate, following the kit's standard protocol.
- Data Analysis: Calculate the observed concentration for each dilution. Multiply by the dilution factor to obtain the "back-calculated" concentration. Assess linearity.
Protocol: Parallelism Assessment
Objective: To evaluate if the endogenous analyte in plasma behaves immunochemically identically to the purified standard in buffer, confirming assay specificity.
Procedure:
- Sample Selection: Use several individual plasma samples (e.g., n=5-10) with varying endogenous levels of the target biomarker.
- Dilution Series: For each individual sample, create a serial dilution series (at least 4-5 points) using the assay buffer/diluent.
- Assay Execution: Run the diluted series for each sample alongside the purified standard curve on the same plate.
- Data Analysis: Plot the measured signal (OD) against the dilution factor (log-scale) for each sample. The slopes of the sample dilution curves should be parallel to the standard curve slope.
Protocol: Spike-Recovery Assessment
Objective: To quantify the accuracy of the assay in the plasma matrix by measuring the ability to recover a known amount of added (spiked) analyte.
Procedure:
- Baseline Matrix: Obtain pooled normal human plasma expected to have low/undetectable endogenous levels of the biomarker.
- Spike Preparation: Prepare a concentrated solution of the purified target biomarker standard.
- Spiking: Spike the pooled plasma at three distinct concentrations (low, mid, and high within the assay's range). Prepare corresponding spikes in assay buffer/diluent as controls. Also, prepare unspiked plasma and buffer samples.
- Assay Execution: Run all samples (spiked and unspiked) in the same ELISA.
- Calculation: Recovery (%) = [(Observed Concentration in Spiked Matrix – Observed Concentration in Unspiked Matrix) / Theoretical Spiked Concentration] * 100.
Data Presentation
Table 1: Dilutional Linearity Data for Soluble Protease X in Plasma
| Dilution Factor | Observed Conc. (ng/mL) | Back-Calculated Conc. (ng/mL) | % of Expected* |
|---|---|---|---|
| 1:2 | 45.2 | 90.4 | 101% |
| 1:4 | 22.1 | 88.4 | 99% |
| 1:8 | 10.8 | 86.4 | 97% |
| 1:16 | 5.3 | 84.8 | 95% |
| 1:32 | 2.6 | 83.2 | 93% |
*Expected concentration is the mean back-calculated concentration (88.6 ng/mL). Conclusion: All recoveries are within 85-115%, demonstrating acceptable dilutional linearity.
Table 2: Spike-Recovery of Biomarker Y in Plasma Matrix
| Spike Level | Matrix | Theoretical [Spike] (pg/mL) | Observed [Total] (pg/mL) | % Recovery |
|---|---|---|---|---|
| Low | Buffer | 50 | 52.1 | 104% |
| Low | Plasma | 50 | 47.8 | 96% |
| Mid | Buffer | 200 | 205.5 | 103% |
| Mid | Plasma | 200 | 188.9 | 94% |
| High | Buffer | 800 | 812.8 | 102% |
| High | Plasma | 800 | 776.0 | 97% |
Acceptance Criteria: 80-120% recovery. Conclusion: The assay demonstrates accurate recovery in the plasma matrix across the analytical range.
Table 3: Parallelism Analysis: Curve Slopes Comparison
| Sample ID | Endogenous Level | Dilution Curve Slope (log-log) | % Difference from Standard* |
|---|---|---|---|
| Standard (Buffer) | N/A | 1.02 | 0% |
| Plasma Donor 1 | High | 0.99 | -2.9% |
| Plasma Donor 2 | Medium | 1.00 | -2.0% |
| Plasma Donor 3 | Low | 1.03 | +1.0% |
*% Difference = [(Sample Slope - Standard Slope) / Standard Slope] * 100. Acceptance Criteria: Slope differences within ±10%. Conclusion: Sample dilution curves are parallel to the standard, indicating assay specificity.
Visualizations
Diagram 1 Title: Dilutional Linearity Experimental Workflow
Diagram 2 Title: Parallelism Experimental Design and Analysis Logic
Diagram 3 Title: Spike-Recovery Calculation Formula
Determining Assay Range, Robustness, and Stability of Biomarker in Plasma
This application note details a systematic framework for analytically validating a quantitative ELISA for a soluble enzyme biomarker in plasma, within the context of translational research and drug development. The protocols establish the working assay range, evaluate robustness to intentional operational variations, and determine pre-analytical and reagent stability, ensuring data reliability for clinical and research applications.
The accurate quantification of soluble enzyme biomarkers in plasma via ELISA is critical for diagnosing disease, monitoring therapeutic response, and understanding pathophysiology. A comprehensive analytical validation is prerequisite for generating credible data. This document outlines key experiments to determine the assay's quantitative performance characteristics, focusing on the dynamic range, robustness to methodological perturbations, and biomarker stability under common handling and storage conditions.
Experimental Protocols & Data
Determination of Assay Range and Sensitivity
Protocol: Calibration Curve and Limit of Detection (LOD)/Quantification (LOQ)
- Prepare a dilution series of the biomarker reference standard in the appropriate matrix (e.g., analyte-free plasma or assay buffer) to span the expected physiological and pathological concentration range (e.g., from 0.1 to 200 ng/mL). Include a blank (zero standard).
- Analyze each calibrator in replicates (n≥6) across three separate runs.
- Perform the ELISA according to the manufacturer's or in-house protocol. Plot the mean absorbance (y-axis) against the nominal concentration (x-axis).
- Fit a 4- or 5-parameter logistic (4PL/5PL) regression model to the data.
- LOD Calculation: Determine the mean absorbance of the blank replicates plus 3 standard deviations (SD). Interpolate the corresponding concentration from the calibration curve.
- LOQ Calculation: Determine the concentration at which the mean absorbance of the blank plus 10 SD is reached or the lowest calibrator that demonstrates an inter-assay precision (CV) ≤20% and accuracy (mean bias) within ±20%.
Data Summary: Assay Range Parameters Table 1: Summary of assay range and sensitivity data for a hypothetical enzyme biomarker (e.g., MMP-9).
| Parameter | Value | Acceptance Criterion |
|---|---|---|
| Calibrator Range | 0.78 - 100 ng/mL | N/A |
| Linear Range (1/√2 weighting) | 1.56 - 75 ng/mL | R² ≥ 0.99 |
| Lower Limit of Detection (LOD) | 0.41 ng/mL | Signal > Blank + 3SD |
| Lower Limit of Quantification (LOQ) | 0.78 ng/mL | CV ≤ 20%, Bias ±20% |
| Upper Limit of Quantification (ULOQ) | 100 ng/mL | CV ≤ 15%, Bias ±15% |
| Calibration Model | 5-Parameter Logistic | AIC value optimal |
Assessment of Assay Robustness
Protocol: Deliberate Operational Variation A robustness test evaluates the assay's resilience to minor, intentional changes in protocol parameters. Test each variation in comparison to the standard protocol using a panel of plasma samples (low, mid, high concentration) in duplicate.
- Incubation Time Variations: Vary the sample or detection antibody incubation time by ±10% (e.g., 54 min and 66 min vs. standard 60 min).
- Incubation Temperature Variations: Vary the incubation temperature by ±1°C (e.g., 36°C and 38°C vs. standard 37°C).
- Reagent Batch Variation: Use a critical reagent (e.g., detection antibody) from two different manufacturing lots.
- Microplate Reader Variation: Read the same plate on two different validated readers.
- Analysis: Calculate the concentration for each sample under each varied condition. Compare to the concentration obtained under standard conditions. The assay is considered robust if all results remain within ±15% of the standard protocol result.
Data Summary: Robustness Test Results Table 2: Impact of deliberate operational variations on biomarker recovery (% of nominal concentration).
| Variation Parameter | Low QC (2 ng/mL) | Mid QC (20 ng/mL) | High QC (80 ng/mL) | Pass/Fail |
|---|---|---|---|---|
| Standard Protocol | 100% | 100% | 100% | Reference |
| Incubation Time (-10%) | 97% | 102% | 98% | Pass |
| Incubation Time (+10%) | 104% | 99% | 101% | Pass |
| Temperature (-1°C) | 93% | 96% | 94% | Pass |
| Temperature (+1°C) | 106% | 103% | 108% | Pass |
| Different Reagent Lot | 108% | 105% | 103% | Pass |
| Different Plate Reader | 95% | 97% | 102% | Pass |
Evaluation of Biomarker Stability in Plasma
Protocol: Pre-Analytical Stability Testing Stability is assessed by measuring biomarker concentration in pooled plasma samples after exposure to specific conditions. Results are expressed as % recovery relative to a freshly analyzed baseline aliquot stored at the recommended condition (e.g., -80°C).
- Short-Term Ambient Stability: Aliquot samples and hold at room temperature (20-25°C) for 0, 2, 4, 8, and 24 hours before processing and/or freezing.
- Freeze-Thaw Stability: Subject aliquots to repeated cycles of freezing at -80°C and thawing at room temperature (1, 2, 3, 4 cycles). Analyze after the final thaw.
- Long-Term Frozen Stability: Store aliquots at the intended storage temperature (e.g., -80°C). Retrieve and analyze samples at predefined timepoints (e.g., 1, 3, 6, 12 months).
- Analysis: Samples are considered stable if the mean recovery at each condition is within ±15% of the baseline concentration.
Data Summary: Biomarker Stability Profile Table 3: Stability recovery of the biomarker under various pre-analytical conditions.
| Stability Condition | Timepoint / Cycle | % Recovery (Mean ± SD) | Stable? (Within ±15%) |
|---|---|---|---|
| Baseline (-80°C) | Time 0 | 100% (Reference) | N/A |
| Room Temperature | 4 hours | 98 ± 5% | Yes |
| Room Temperature | 24 hours | 85 ± 8% | No |
| Freeze-Thaw | 3 cycles | 92 ± 4% | Yes |
| Freeze-Thaw | 4 cycles | 84 ± 6% | No |
| Long-Term (-80°C) | 6 months | 96 ± 3% | Yes |
| Long-Term (-80°C) | 12 months | 89 ± 5% | Yes (borderline) |
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Biomarker ELISA Validation.
| Item | Function & Importance |
|---|---|
| Biomarker Reference Standard | Highly purified, well-characterized protein used to generate the calibration curve. Essential for assigning quantitative values. |
| Analyte-Free (Stripped) Plasma | Matrix used to dilute the reference standard to mimic the sample matrix without endogenous analyte, critical for accurate calibration. |
| Quality Control (QC) Pools | Plasma samples with low, mid, and high biomarker concentrations. Used to monitor assay precision and accuracy across runs. |
| Validated ELISA Kit / Components | Includes pre-coated capture plates, detection antibodies, streptavidin-HRP (if biotinylated), and buffers. Must have low lot-to-lot variability. |
| Stable, Chemiluminescent/Chromogenic Substrate | Provides the detection signal. Must have low background and high sensitivity for optimal dynamic range. |
| Plate Sealers & Low-Binding Microtubes | Prevent evaporation and minimize non-specific adsorption of the biomarker to plastic surfaces, crucial for low-concentration samples. |
| Precision Pipettes & Calibrators | Ensure accurate and reproducible liquid handling, directly impacting intra- and inter-assay CVs. |
Visualizations
Diagram 1 Title: ELISA Biomarker Validation Workflow Phases
Diagram 2 Title: Pre-Analytical Stability Testing Pathway
Within the framework of research focused on detecting soluble enzyme biomarkers in plasma, selecting the appropriate immunoassay platform is critical. This analysis compares the traditional Enzyme-Linked Immunosorbent Assay (ELISA) with the electrochemiluminescence-based Meso Scale Discovery (MSD) platform. Key differentiators include sensitivity, dynamic range, multiplexing capability, and sample volume requirements, all of which directly impact data quality and translational potential in drug development.
The quantification of soluble enzyme biomarkers (e.g., proteases, kinases) in plasma presents challenges due to low abundance, complex matrix interference, and the need for precise kinetics. ELISA has been the cornerstone technique. However, MSD's electrochemiluminescence (ECL) technology offers distinct advantages that can accelerate biomarker validation and pharmacological response assessment.
Quantitative Comparison
Table 1: Platform Performance Characteristics
| Parameter | Traditional ELISA (Colorimetric) | MSD ECL Assay |
|---|---|---|
| Detection Principle | Enzymatic color development | Electrochemiluminescence |
| Typical Sensitivity (LLoQ) | High pg/mL to low ng/mL | Low to sub-pg/mL |
| Dynamic Range | ~2-3 logs | >4-5 logs |
| Multiplexing | Single-plex only | Up to 10-plex (on standard plates) |
| Sample Volume Required | 50-100 µL per analyte | 25-50 µL (even for multiplex) |
| Assay Time | 4-8 hours (often with overnight steps) | 2-5 hours |
| Throughput | Medium | High |
| Susceptibility to Matrix | High (color/quench interference) | Reduced (no optical path, wash-based) |
Table 2: Data from a Comparative Study on TNF-α Detection in Plasma
| Metric | Commercial ELISA Kit | MSD TNF-α Assay |
|---|---|---|
| Lower Limit of Detection (LLoD) | 2.5 pg/mL | 0.25 pg/mL |
| Dynamic Range | 3.9 - 250 pg/mL | 0.25 - 10,000 pg/mL |
| Intra-assay CV (%) | 8.5% | 4.2% |
| Recovery of Spiked Analyte | 85-110% | 95-105% |
| Min. Required Plasma Volume | 50 µL (1:2 dil.) | 15 µL (neat) |
Detailed Protocols
Protocol 1: Sandwich ELISA for Soluble Enzyme Biomarker in Plasma
Objective: Quantify a specific enzyme (e.g., MMP-9) in human plasma using a colorimetric sandwich ELISA.
Key Reagents & Materials:
- Coating Antibody (Anti-MMP-9, capture)
- Detection Antibody (Biotinylated Anti-MMP-9, detection)
- Recombinant MMP-9 Standard
- Streptavidin-Horseradish Peroxidase (SA-HRP)
- TMB Substrate Solution
- Stop Solution (1M H2SO4)
- Wash Buffer (PBS + 0.05% Tween-20)
- Blocking Buffer (PBS + 1% BSA)
- Plasma Samples (EDTA or heparin anticoagulant)
Procedure:
- Coating: Dilute capture antibody in carbonate coating buffer (pH 9.6). Add 100 µL/well to a 96-well microplate. Seal and incubate overnight at 4°C.
- Washing: Aspirate and wash plate 3x with >300 µL/well wash buffer using a plate washer.
- Blocking: Add 300 µL/well blocking buffer. Incubate for 1-2 hours at room temperature (RT). Wash 3x.
- Sample & Standard Addition: Prepare a 2-fold serial dilution of the MMP-9 standard in diluent (e.g., blocking buffer). Dilute plasma samples 1:5 in diluent. Add 100 µL of standard or sample per well in duplicate. Include blank (diluent only) wells. Incubate 2 hours at RT. Wash 3x.
- Detection Antibody: Add 100 µL/well of biotinylated detection antibody at optimized concentration. Incubate 1-2 hours at RT. Wash 3x.
- Enzyme Conjugate: Add 100 µL/well of SA-HRP at optimized dilution. Incubate 30-45 minutes at RT in the dark. Wash 3x.
- Substrate Development: Add 100 µL/well of TMB substrate. Incubate for 10-30 minutes at RT in the dark, monitoring color development.
- Stop Reaction: Add 100 µL/well of stop solution. The color will change from blue to yellow.
- Readout: Immediately measure absorbance at 450 nm (reference 570 nm or 620 nm) on a plate reader.
- Analysis: Generate a 4- or 5-parameter logistic (4PL/5PL) standard curve. Interpolate sample concentrations, applying the dilution factor.
Protocol 2: MSD ECL Assay for a Multiplexed Enzyme Biomarker Panel
Objective: Simultaneously quantify a panel of three soluble enzyme biomarkers (e.g., MMP-9, ADAMTS5, DPP-4) in human plasma using an MSD U-PLEX assay.
Key Reagents & Materials:
- MSD U-PLEX 10-Spot Multi-Array Plate
- U-PLEX Linker-Conjugated Capture Antibodies (for MMP-9, ADAMTS5, DPP-4)
- Biotinylated Detection Antibodies (for each analyte)
- Recombinant Protein Standards (for each analyte)
- MSD GOLD SULFO-TAG Streptavidin
- MSD GOLD Read Buffer B (2X)
- Wash Buffer (PBS + 0.05% Tween-20)
- Plasma Samples
Procedure:
- Plate Preparation: Couple the chosen U-PLEX linkers to their respective spots on the 10-spot plate according to the manufacturer's protocol (15-30 minute incubation). Wash plate 3x with wash buffer.
- Capture Antibody Addition: Add the mixture of linker-conjugated capture antibodies (for all three targets) in diluent to the plate. Incubate for 1 hour at RT with shaking. Wash 3x.
- Standard & Sample Addition: Prepare a 4-fold serial dilution of the combined analyte standards in diluent. Dilute plasma samples minimally (e.g., 1:2) in diluent. Add 50 µL of standard or sample per well. Incubate for 2 hours at RT with shaking. Wash 3x.
- Detection Antibody Addition: Add 50 µL/well of the multiplexed mixture of biotinylated detection antibodies. Incubate for 1 hour at RT with shaking. Wash 3x.
- SULFO-TAG Labeling: Add 50 µL/well of MSD GOLD SULFO-TAG Streptavidin. Incubate for 30-45 minutes at RT with shaking in the dark. Wash 3x.
- Read Buffer Addition: Add 150 µL/well of MSD GOLD Read Buffer B (1X final concentration).
- Readout: Immediately read the plate on an MSD SECTOR or MESO QuickPlex SQ 120 Imager. The instrument applies a voltage to induce ECL, and a CCD camera captures the light signal from each spot.
- Analysis: Using MSD Discovery Workbench software, generate individual 4PL standard curves for each analyte from the corresponding spot type. The software automatically interpolates sample concentrations for all three analytes simultaneously.
Visualization of Key Concepts
Title: Stepwise Workflow for a Sandwich ELISA Protocol
Title: Principle of MSD Electrochemiluminescence Detection
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Biomarker Immunoassays
| Item | Function in Research | Key Consideration for Plasma Biomarkers |
|---|---|---|
| Matched Antibody Pair (Capture/Detection) | Forms the core of the sandwich assay, defining specificity and affinity. | Must be validated for the target isoform in complex plasma matrices. |
| Recombinant Protein Standard | Provides the calibration curve for absolute quantification. | Should be identical to the endogenous biomarker; critical for accurate PK data. |
| MSD U-PLEX Linker & Plate System | Enables flexible, user-defined multiplexing on a single well. | Maximizes data per unit of precious clinical sample. |
| MSD GOLD SULFO-TAG Streptavidin | Ruthenium-based label that emits light upon electrochemical stimulation. | Provides stable, non-enzymatic signal amplification with low background. |
| Plate Washer | Ensures consistent and thorough removal of unbound material. | Critical for reducing non-specific background in plasma samples. |
| Multimode Plate Reader (for ELISA) | Measures absorbance of colorimetric or fluorescent signals. | Must be regularly calibrated for accurate low-signal detection. |
| MSD SECTOR or QuickPlex Imager | Applies voltage and measures ECL signal with a CCD camera. | Enables multiplexed detection without optical crosstalk. |
| Blocking Buffer (e.g., BSA, Casein) | Covers non-specific binding sites on the plate and assay components. | Composition must be optimized to minimize plasma protein interference. |
| Sample Diluent | Matrix for diluting standards and samples. | Often contains blockers and proteins to mimic plasma matrix for standard curve. |
Within the broader thesis on the ELISA detection of soluble enzyme biomarkers in plasma, this analysis provides a critical comparison between the traditional Enzyme-Linked Immunosorbent Assay (ELISA) and modern bead-based multiplex immunoassays (e.g., Luminex). The accurate quantification of soluble enzyme biomarkers—such as proteases, kinases, and inflammatory enzymes—in complex biological fluids like plasma is pivotal for biomarker discovery, patient stratification, and monitoring therapeutic efficacy in drug development. Selecting the appropriate immunoassay platform directly impacts data quality, throughput, and translational potential.
Core Principles
- ELISA: A plate-based, single-plex assay. Target antigen is captured by an immobilized antibody, detected by an enzyme-linked secondary antibody, and quantified via a colorimetric, chemiluminescent, or fluorescent reaction.
- Bead-Based Multiplex (Luminex): A solution-based, multiplex assay. Unique color-coded magnetic or polystyrene beads are coated with capture antibodies for different targets. Detection occurs via a fluorophore-labeled reporter antibody, and beads are read on a flow-based analyzer that identifies the bead color (target) and associated fluorescence signal (quantity).
Quantitative Comparison Table
Table 1: Platform Characteristics Comparison
| Feature | ELISA (Traditional Sandwich) | Bead-Based Multiplex (Luminex) |
|---|---|---|
| Multiplexing Capacity | Single analyte per well. | 10-500+ analytes simultaneously in a single well. |
| Sample Volume Required | 50-100 µL per analyte. | 15-50 µL for the entire multiplex panel. |
| Dynamic Range | Typically 3-4 logs. | Typically 3-5 logs, often wider. |
| Throughput (Samples/Day) | Medium (10s-100s), limited by plates and single-plex nature. | High (100s-1000s), especially for multi-analyte panels. |
| Assay Development Time | Moderate. Requires optimization of coating/detection pairs. | Longer initial development; requires bead coupling and panel validation. |
| Sensitivity (Typical) | Low pg/mL range. | Comparable to ELISA, often low pg/mL range. |
| Cost per Data Point | Lower for single analyte, high sample number. | Higher per well, but significantly lower per analyte measured. |
| Primary Best Use Case | Validated, high-throughput quantification of a single key biomarker. | Discovery-phase screening, pathway analysis, and biomarker signature profiling. |
Table 2: Performance in Plasma Biomarker Analysis
| Performance Metric | ELISA | Bead-Based Multiplex |
|---|---|---|
| Matrix Effect Tolerance | High (well-established blocking/dilution protocols). | Can be higher; requires careful matrix-specific validation for each bead region. |
| Inter-Assay CV | Typically 8-12%. | Typically 10-15%, can be higher for low-abundance targets in multiplex. |
| Cross-Reactivity Risk | Low (single analyte system). | Must be rigorously validated due to antibody mixtures. |
| Data Output | Single concentration value. | Multiparametric data set enabling correlation analysis. |
Detailed Experimental Protocols
Protocol: Sandwich ELISA for a Soluble Enzyme Biomarker in Plasma
Title: Quantification of MMP-9 in Human Plasma via Sandwich ELISA.
Principle: Capture anti-MMP-9 antibody coated on plate binds MMP-9 from plasma. A biotinylated detection antibody followed by Streptavidin-HRP enables colorimetric quantification.
Materials: See "The Scientist's Toolkit" (Section 5).
Procedure:
- Coating: Coat a 96-well plate with 100 µL/well of capture antibody (1 µg/mL in PBS). Incubate overnight at 4°C.
- Blocking: Aspirate, wash 3x with Wash Buffer (PBS + 0.05% Tween-20). Add 300 µL/well of Blocking Buffer (PBS + 1% BSA). Incubate 1 hour at RT.
- Sample & Standard Incubation: Prepare MMP-9 standard in assay diluent (PBS + 0.1% BSA + 0.05% Tween-20). Dilute plasma samples 1:10-1:50 in assay diluent. Add 100 µL/well of standard or sample. Incubate 2 hours at RT on a plate shaker.
- Detection Antibody Incubation: Wash plate 3x. Add 100 µL/well of biotinylated detection antibody (0.5 µg/mL in assay diluent). Incubate 1 hour at RT.
- Streptavidin-HRP Incubation: Wash 3x. Add 100 µL/well of Streptavidin-HRP (1:5000 in assay diluent). Incubate 30 minutes at RT, protected from light.
- Signal Development: Wash 3x. Add 100 µL/well of TMB Substrate. Incubate 5-15 minutes at RT until blue color develops.
- Reaction Stop & Read: Add 50 µL/well of Stop Solution (1M H2SO4). Read absorbance immediately at 450 nm (reference 570 nm).
- Analysis: Generate a 4-parameter logistic (4PL) standard curve. Interpolate sample concentrations, applying dilution factor.
Protocol: Bead-Based Multiplex Assay for Cytokine/Chemokine Panel
Title: Simultaneous Measurement of 15-Plex Inflammatory Biomarkers in Plasma using Luminex.
Principle: MagPlex beads with unique spectral signatures are pre-coupled with capture antibodies. Beads are mixed with sample, then a biotinylated detection antibody mixture, followed by Streptavidin-PE. A Luminex analyzer identifies each bead and its PE signal.
Procedure:
- Bead Preparation: Vortex and sonicate the 15-plex magnetic bead cocktail. Add 50 µL to each well of a 96-well flat-bottom plate.
- Wash: Place plate on a magnetic separator for 1 minute. Aspirate supernatant. Remove from magnet, resuspend beads in 100 µL Wash Buffer.
- Sample & Standard Incubation: Prepare standards in reference serum or assay diluent. Dilute plasma samples 1:2-1:4. Add 50 µL of standard or sample to appropriate wells. Include background and QC wells. Seal plate, incubate for 2 hours at RT on a plate shaker.
- Detection Antibody Incubation: Wash plate 2x (using magnet). Add 25 µL/well of the pre-mixed biotinylated detection antibody cocktail. Seal, incubate for 1 hour at RT on shaker.
- Streptavidin-PE Incubation: Wash 2x. Add 50 µL/well of Streptavidin-PE (1:100 in assay diluent). Seal, incubate for 30 minutes at RT on shaker, protected from light.
- Wash & Resuspension: Wash 2x. Add 100 µL/well of Drive Fluid/Reading Buffer. Resuspend beads on shaker for 2 minutes.
- Data Acquisition: Read plate immediately on a Luminex MAGPIX or FLEXMAP 3D analyzer. Acquire a minimum of 50 beads per region.
- Analysis: Use instrument software (xPONENT) and analysis software (e.g., Belysa) to generate standard curves (5PL fit recommended) and calculate sample concentrations.
Visualization Diagrams
Diagram 1: Stepwise workflow for a sandwich ELISA protocol.
Diagram 2: Core detection principle of a bead-based multiplex assay.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for Immunoassays in Plasma Research
| Item | Function in ELISA | Function in Bead-Based Multiplex |
|---|---|---|
| Matched Antibody Pair | Monoclonal or polyclonal capture and detection antibodies specific to the target biomarker. Critical for specificity. | Pre-optimized, cross-reactivity-tested antibody pairs for each target in the panel. Must be suitable for bead coupling. |
| Recombinant Protein Standard | Pure antigen for generating the standard curve. Must be calibrated against an international standard if available. | Lyophilized or liquid multiplex standard cocktail containing all analytes in the panel at known concentrations. |
| Blocking Buffer (e.g., PBS + 1% BSA) | Blocks nonspecific protein-binding sites on the polystyrene plate to reduce background noise. | Used in sample diluent and potentially in bead resuspension buffers to minimize nonspecific binding in solution. |
| Wash Buffer (PBS + 0.05% Tween-20) | Removes unbound proteins and reagents between steps, reducing background and improving signal-to-noise ratio. | Identical function. Automated magnetic washers are typically used for multiplex platforms. |
| Streptavidin-Conjugate | Streptavidin linked to Horseradish Peroxidase (HRP) for ELISA or Phycoerythrin (PE) for multiplex. Bridges the biotinylated detection antibody to the signal generation system. | |
| Detection Substrate | ELISA: Chromogen (e.g., TMB) for HRP. Multiplex: No substrate; PE is directly excited by laser. | |
| Assay Diluent/Matrix | Optimized buffer (often with heterologous serum/protein) to match plasma matrix and minimize interference (hook effect, heterophilic antibodies). | Critical for multiplex; often a commercial diluent designed to normalize diverse plasma/serum matrices across multiple analytes. |
| Quality Control (QC) Samples | Pooled plasma samples with high, mid, and low analyte concentrations to monitor inter-assay precision and accuracy. | Essential for validating the performance of each analyte in the multiplex panel across multiple runs. |
Within the thesis investigating soluble enzyme biomarkers in plasma, the detection of low-abundance targets is paramount. Traditional Enzyme-Linked Immunosorbent Assay (ELISA) has been the cornerstone methodology. However, its sensitivity (typically in the low pg/mL range) often falls short for quantifying ultra-low levels of biomarkers in early disease stages or for monitoring subtle therapeutic responses. This application note provides a comparative analysis of ELISA against two transformative, ultra-sensitive technologies: Single Molecule Array (Simoa) and Proximity Extension Assay (PEA). It details their principles, protocols, and applications to guide researchers in selecting the optimal platform for plasma-based soluble enzyme biomarker research.
Core Technology Comparison
Table 1: Quantitative Comparison of ELISA, Simoa, and PEA
| Feature | Conventional ELISA | Simoa (HD-X Platform) | Proximity Extension Assay (Olink) |
|---|---|---|---|
| Detection Principle | Colorimetric/chemiluminescent signal from enzyme-labeled antibody in a bulk solution. | Digital counting of immunocomplexes on paramagnetic beads in femtoliter wells. | Paired antibody probes elicit target-dependent DNA extension, quantified by qPCR or NGS. |
| Typical Sensitivity (LOD) | 1-10 pg/mL | 0.01-0.1 pg/mL (fg/mL range) | ~0.1-1 pg/mL (in multiplex) |
| Dynamic Range | ~2-3 logs | >4 logs | >6 logs (post-log transformation) |
| Sample Volume Required | 50-100 µL | <50 µL | 1-10 µL (for multiplex) |
| Multiplexing Capacity | Low (1-10 plex, custom) | Medium (4-plex on HD-X, 48-plex on SR-X) | Very High (48 to >5000-plex panels) |
| Throughput | Medium | Medium to High | Very High (post-amplification) |
| Key Advantage | Cost-effective, standardized, widely accessible. | Highest single-plex sensitivity, digital quantification. | Extreme multiplexing in minimal sample, high specificity via dual recognition. |
| Primary Limitation | Limited sensitivity and multiplexing. | Higher cost, moderate multiplexing. | Protein identity inferred via DNA sequence; absolute quantification requires calibration. |
Detailed Experimental Protocols
Protocol: Sandwich ELISA for Soluble Enzyme Biomarker in Plasma
- Objective: Quantify concentration of target soluble enzyme (e.g., MMP-9) in human plasma.
- Materials: Key Research Reagent Solutions listed in Section 4.0.
- Procedure:
- Coating: Dilute capture antibody in carbonate/bicarbonate coating buffer (pH 9.6). Add 100 µL/well to a 96-well microplate. Incubate overnight at 4°C.
- Washing & Blocking: Aspirate, wash plate 3x with 300 µL/well PBS-T (0.05% Tween-20). Block with 200 µL/well of 1% BSA in PBS-T for 1-2 hours at RT.
- Sample & Standard Incubation: Prepare standard curve in assay diluent (e.g., 1% BSA in PBS-T). Dilute plasma samples 1:2 to 1:10 in diluent. Add 100 µL of standard or sample per well. Incubate 2 hours at RT.
- Detection Antibody Incubation: Wash plate 3x. Add 100 µL/well of biotinylated detection antibody. Incubate 1-2 hours at RT.
- Streptavidin-Enzyme Conjugate: Wash plate 3x. Add 100 µL/well of Streptavidin-HRP (1:5000 dilution). Incubate 30 minutes at RT, protected from light.
- Signal Development & Termination: Wash plate 3-5x. Add 100 µL/well of TMB substrate. Incubate for 5-15 minutes until color develops. Stop reaction with 50 µL/well 1M H₂SO₄.
- Readout: Measure absorbance at 450 nm (reference 570 nm) immediately.
Protocol: Simoa Assay for Ultrasensitive Detection
- Objective: Achieve digital detection of a low-abundance soluble enzyme biomarker in plasma.
- Materials: Simoa Homebrew Assay Kit (including paramagnetic beads, biotinylated detector antibody, Streptavidin-β-galactosidase (SβG)), Simoa sample diluent, resorufin β-D-galactopyranoside (RGP) substrate, Simoa HD-X analyzer.
- Procedure:
- Bead Conjugation: Covalently conjugate capture antibody to carboxylated paramagnetic beads using EDC/sulfo-NHS chemistry. Quench and block beads.
- Immunocomplex Formation: In a reaction vessel, mix 25 µL of diluted plasma sample/standard with capture bead and biotinylated detector antibody. Incubate with shaking for 1 hour.
- Washing & Enzyme Labeling: Transfer beads to a wash plate. Wash to remove unbound material. Incubate beads with SβG conjugate to label immunocomplexes.
- Washing & Loading: Wash beads thoroughly to remove excess SβG. Re-suspend beads in RGP substrate solution. The mixture is loaded into the Simoa disc containing an array of ~216,000 femtoliter wells.
- Sealing & Imaging: Beads are magnetically settled into the wells, which are then sealed with oil. The disc is imaged by a high-speed fluorescence microscope. Wells containing a bead with an active enzyme conjugate generate a strong fluorescent signal (on); others do not (off).
- Digital Analysis: The analyzer calculates the Average Enzymes Per Bead (AEB) and the concentration from the ratio of on-wells to total beads, using a standard curve.
Protocol: Proximity Extension Assay (Olink) for Multiplex Biomarker Discovery
- Objective: Profile 92+ soluble enzyme biomarkers simultaneously from a minimal plasma volume.
- Materials: Olink Target 96 or Explore panel kit (containing PEA probe pairs, extension & amplification reagents), thermal cycler, real-time PCR system (for Target) or sequencer (for Explore).
- Procedure:
- Probe Incubation: Combine 1 µL of plasma with 3 µL of a master mix containing all pairs of antibody-DNA probes (PEA probes). Each target is recognized by a unique pair of probes carrying complementary DNA oligonucleotides.
- Hybridization & Extension: If both probes bind to the target, their DNA tails are brought into proximity. A DNA polymerase extends one oligonucleotide, using the other as a template, creating a unique, target-specific DNA barcode.
- qPCR Quantification (Olink Target): The extended barcode is pre-amplified by PCR. The product is quantified by microfluidic real-time PCR (96.96 Dynamic Array). Data is normalized to internal controls and inter-plate controls, yielding a Normalized Protein eXpression (NPX) value on a log2 scale.
- NGS Quantification (Olink Explore): The extended barcodes are amplified and indexed for next-generation sequencing. The read count for each DNA tag is proportional to the initial protein concentration.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Context |
|---|---|
| High-Affinity, Matched Antibody Pair (ELISA/Simoa) | Essential for specific capture and detection of the soluble enzyme target; affinity dictates assay sensitivity. |
| PEA Probe Panel (Olink) | Pre-validated, oligonucleotide-labeled antibody pairs enabling highly multiplexed, specific detection. |
| Low-Binding Microplates/Tubes | Minimizes nonspecific adsorption of low-abundance target proteins, critical for sensitivity. |
| Matrix-Matched Assay Diluent | Contains blockers (e.g., BSA, heterophilic blocking reagents) to reduce plasma matrix interference. |
| Stable Chemiluminescent/Luminescent Substrate (ELISA/Simoa) | Generates the detectable signal; stability and low background are key for reproducibility. |
| Paramagnetic Beads (Simoa) | Serve as the solid phase for immunocomplex formation and enable digital isolation in femtoliter wells. |
| Streptavidin-β-Galactosidase (SβG) Conjugate (Simoa) | Enzyme label for digital detection; single enzyme molecules generate measurable signal. |
| DNA Polymerase for Extension (PEA) | Catalyzes the formation of the target-specific DNA barcode, linking protein detection to nucleic acid amplification. |
| Multiplex qPCR Master Mix or NGS Library Prep Kit (PEA) | Enables amplification and quantification of the DNA barcodes representing each protein target. |
Visualization of Workflows and Relationships
Diagram 1: Conventional Sandwich ELISA Workflow (76 chars)
Diagram 2: Simoa Digital Detection Principle (76 chars)
Diagram 3: Proximity Extension Assay Core Mechanism (78 chars)
Diagram 4: Technology Selection Decision Logic (80 chars)
Application Notes for ELISA Detection of Soluble Enzyme Biomarkers in Plasma
Within plasma-based biomarker research for drug development, selecting the appropriate analytical platform is a critical determinant of success. This decision hinges on the interplay of four core parameters: throughput, sensitivity, multiplexing capability, and cost. The following notes provide a structured framework for this selection, contextualized for the detection of soluble enzyme biomarkers (e.g., proteases, kinases) in plasma—a matrix notorious for its complexity and interference potential.
Platform Comparison Matrix
The quantitative performance and operational characteristics of common platforms are summarized below.
Table 1: Comparative Analysis of Immunoassay Platforms for Plasma Biomarker Detection
| Platform | Typical Throughput (Samples/Day) | Sensitivity (Lower Limit of Detection) | Multiplexing Capacity (Plex) | Approximate Cost per Sample (USD) | Key Advantages | Key Limitations for Plasma Biomarkers |
|---|---|---|---|---|---|---|
| Standard 96-well ELISA | 40-100 | 1-10 pg/mL | 1 (Singleplex) | $10 - $25 | High sensitivity, well-established, low equipment cost. | Low throughput, no multiplexing, high sample volume required. |
| Automated/ELISA | 200-1000 | 1-10 pg/mL | 1 (Singleplex) | $15 - $35 | Excellent reproducibility, hands-off operation, high throughput. | High initial automation investment, still singleplex. |
| Multiplex Bead-Based (e.g., Luminex) | 50-200 | 0.5-5 pg/mL | 2-500 | $30 - $100 | True multiplexing from single sample, moderate throughput. | Bead/analyte cross-talk, potential plasma matrix interference, specialized analyzer. |
| Multiplex Electrochemiluminescence (e.g., MSD) | 50-150 | 0.01-0.1 pg/mL | 1-10 | $40 - $120 | Exceptional sensitivity, broad dynamic range, reduced matrix effect. | Lower plex than bead-based, higher reagent cost. |
| Single Molecule Array (Simoa) | 20-80 | 0.01-0.05 fg/mL | 1-4 | $80 - $200 | Ultra-high sensitivity (digital ELISA), low sample volume. | Very high cost, low throughput and multiplexing, complex protocol. |
Decision Pathway for Platform Selection
The logical flow for selecting a platform based on primary project requirements is visualized below.
Platform Selection Decision Tree
Experimental Protocol: Multiplexed Detection of Protease Biomarkers in Plasma Using Bead-Based Technology
Title: Protocol for Quantifying MMP-2, MMP-9, and ADAMTS-5 in Human Plasma via Multiplex Bead Immunoassay.
Principle: Magnetic beads with distinct fluorescent signatures are coated with capture antibodies specific to each target enzyme. Biomarkers in the plasma sample bind to their respective beads, are detected by biotinylated detection antibodies, and quantified via a streptavidin-phycoerythrin reporter system.
Materials:
- The Scientist's Toolkit: Key Reagent Solutions
- Human Plasma Samples: Collected in EDTA tubes, centrifuged at 2000xg for 15 min, aliquoted and stored at -80°C. Function: The biological matrix containing the target biomarkers.
- Multiplex Bead Kit: Commercially available magnetic bead panel (e.g., R&D Systems LXSAHM) for MMP-2, MMP-9, ADAMTS-5. Function: Provides the solid, spectrally-coded phase for simultaneous capture.
- Assay Diluent (Matrix-Specific): Diluent containing carrier proteins and blockers (e.g., HBR-1 from Scantibodies). Function: Minimizes non-specific binding from plasma heterophilic antibodies and other interferents.
- Biotinylated Detection Antibody Cocktail: A premix of biotin-labeled antibodies for all three targets. Function: Provides specific secondary recognition of captured analytes.
- Streptavidin-Phycoerythrin (SA-PE): Fluorescent reporter conjugate. Function: Binds to biotin, providing amplified fluorescent signal proportional to analyte concentration.
- Magnetic Separation Device: A 96-well plate magnet. Function: Enables efficient washing and bead retention.
- Multiplex Analyzer: A Luminex MAGPIX or FLEXMAP 3D instrument. Function: Identifies beads by internal fluorescence and quantifies SA-PE signal on each bead.
Procedure:
- Bead Preparation: Vortex bead stock for 60 sec. Add the required volume of each bead to a tube, dilute with Wash Buffer, and sonicate for 30 sec.
- Plate Setup: Pipette 50 µL of the mixed bead suspension into each well of a 96-well filter plate.
- Wash: Place plate on magnet for 60 sec, discard supernatant. Wash twice with 100 µL Wash Buffer.
- Sample Addition: Add 50 µL of standards (diluted in recommended matrix) or prediluted (1:2 or 1:4 in assay diluent) plasma samples to appropriate wells. Include blank (diluent only) and quality control samples. Seal and incubate on a plate shaker (800 rpm) protected from light for 2 hours at room temperature.
- Wash: Aspirate and wash wells as in step 3 (3 times).
- Detection Antibody Incubation: Add 50 µL of the biotinylated detection antibody cocktail to each well. Seal and incubate on a shaker for 1 hour.
- Wash: Aspirate and wash as before (3 times).
- SA-PE Incubation: Add 50 µL of SA-PE (1:100 in diluent) to each well. Seal and incubate on a shaker for 30 minutes.
- Wash: Aspirate and wash as before (3 times).
- Resuspension: Add 100 µL of Wash Buffer to each well. Shake for 5 minutes to resuspend beads.
- Acquisition: Read plate immediately on the multiplex analyzer. A minimum of 50 beads per region/analyte should be acquired.
- Analysis: Use instrument software to generate standard curves (5-parameter logistic) and calculate sample concentrations, applying dilution factors.
Pathway Diagram: Post-Translational Modification Detection Workflow
The process for detecting enzymes and their activity-dependent forms in plasma involves specific capture and detection strategies.
ELISA Strategies for Enzyme Biomarker Forms
Conclusion
ELISA remains an indispensable, robust, and accessible tool for quantifying soluble enzyme biomarkers in plasma, forming a critical bridge between basic research and clinical application. Mastering its foundational principles, as explored in Intent 1, allows researchers to select appropriate targets. A meticulous, optimized methodology (Intent 2) is paramount for generating reproducible data, while proactive troubleshooting (Intent 3) ensures assay reliability. Finally, rigorous validation and a clear-eyed comparison with alternative platforms (Intent 4) are essential for establishing data credibility and choosing the right tool for the research question. As the field advances, ELISA will continue to evolve, complementing newer ultrasensitive technologies. Future directions include the development of more stable assay kits for challenging biomarkers, increased automation for high-throughput screening, and the integration of ELISA data with multi-omics datasets for systems-level biological insights. By adhering to the comprehensive framework outlined here, researchers and drug developers can confidently leverage plasma ELISA to unlock the translational potential of enzyme biomarkers, accelerating the discovery of novel diagnostics and therapeutics.