Emerging Biomarkers for Metabolic Syndrome and Type 2 Diabetes: From Pathophysiology to Precision Medicine
This comprehensive review synthesizes the latest advancements in biomarker science for Metabolic Syndrome (MetS) and Type 2 Diabetes Mellitus (T2DM), targeting researchers and drug development professionals.
Emerging Biomarkers for Metabolic Syndrome and Type 2 Diabetes: From Pathophysiology to Precision Medicine
Abstract
This comprehensive review synthesizes the latest advancements in biomarker science for Metabolic Syndrome (MetS) and Type 2 Diabetes Mellitus (T2DM), targeting researchers and drug development professionals. We explore the foundational pathophysiology linking these conditions, including chronic inflammation, insulin resistance, and multi-organ crosstalk. The article details established and novel biomarkers—from traditional inflammatory markers and HOMA-IR to emerging candidates like suPAR, Galectin-3, and specific metabolite panels. It critically evaluates methodological approaches in biomarker discovery, including metabolomics and multi-omics integration, while addressing key challenges in clinical validation, specificity, and standardization. Finally, we discuss the translation of these biomarkers into improved risk stratification, therapeutic monitoring, and personalized treatment strategies, framing their potential to reshape early intervention and drug development.
Unraveling the Pathophysiological Web of MetS and T2DM
The conceptual understanding of metabolic disorders has undergone a profound transformation over recent decades, evolving from a collection of distinct risk factors into sophisticated models of multisystemic dysfunction. This progression from Metabolic Syndrome (MetS) to the comprehensive Cardiovascular-Renal-Hepatic-Metabolic (CRHM) syndrome framework reflects an increasingly nuanced appreciation of the interconnected pathophysiological processes that drive disease progression across organ systems. For researchers and drug development professionals, this evolution carries significant implications for biomarker discovery, therapeutic targeting, and clinical trial design. The integration of omics technologies, advanced analytics, and population-specific considerations is reshaping our approach to these complex conditions, particularly within the context of metabolic syndrome and type 2 diabetes research. This whitepaper traces the conceptual evolution of syndrome terminology, examines the underlying pathophysiological mechanisms, and explores the biomarker and therapeutic innovations that are enabling more precise, effective interventions for these interconnected conditions.
The Historical Trajectory of Syndrome Concepts
The conceptual framework for understanding metabolic disorders has progressed through several distinct phases, each building upon previous understanding while incorporating new clinical and scientific insights.
Metabolic Syndrome: The Foundational Concept
The concept of metabolic clustering was first formally recognized in 1988 when Gerald Reaven introduced "Syndrome X," highlighting insulin resistance as a central pathological feature connecting hypertension, dyslipidemia, and hyperglycemia [1]. This cluster was subsequently operationalized in 2001 by the National Cholesterol Education Program—Third Adult Treatment Panel (NCEP-ATP III), which established diagnostic criteria requiring at least three of five components: abdominal obesity, elevated triglycerides, reduced HDL cholesterol, elevated blood pressure, and elevated fasting glucose [1]. While clinically useful for identifying at-risk individuals, this binary diagnostic approach failed to capture disease severity or the full spectrum of cardiometabolic risk [1].
Intermediate Conceptual Developments
Between 2004-2008, the Cardio-Renal Syndrome (CRS) framework emerged, categorizing five subtypes based on primary organ dysfunction and disease chronicity [2]. This recognized the bidirectional relationship between heart and kidney disorders but remained limited in scope. In 2012, the "Circulatory Syndrome" concept proposed refining MetS by incorporating markers of cardiovascular disease including renal impairment, microalbuminuria, arterial stiffness, and ventricular dysfunction [3]. This represented an important step toward a more integrated view of metabolic-cardiovascular interactions.
Contemporary Syndrome Frameworks
Table 1: Evolution of Syndrome Concepts in Metabolic Disease
| Year | Concept | Key Components | Advancements | Limitations |
|---|---|---|---|---|
| 1988 | Syndrome X [1] | Insulin resistance, hypertension, dyslipidemia | Identified insulin resistance as central defect | Limited component scope |
| 2001 | Metabolic Syndrome (NCEP-ATP III) [1] | 3 of 5 criteria: waist circumference, triglycerides, HDL-C, blood pressure, fasting glucose | Standardized clinical diagnosis | Binary diagnosis; no severity grading |
| 2004-2008 | Cardio-Renal Syndrome (CRS) [2] | 5 subtypes based on primary organ and acuity | Recognized heart-kidney interactions | Excluded liver and broader metabolic aspects |
| 2012 | Circulatory Syndrome [3] | Added renal impairment, microalbuminuria, arterial stiffness to MetS | Incorporated vascular and renal damage markers | Limited adoption in guidelines |
| 2023 | Cardiovascular-Kidney-Metabolic (CKM) Syndrome [4] | Metabolic risk factors, CKD, cardiovascular system | AHA-recognized; staging system | Underemphasized liver involvement |
| 2024-2025 | Cardiovascular-Renal-Hepatic-Metabolic (CRHM) Syndrome [4] [2] | CVD, CKD, MASLD, obesity, T2DM, dyslipidemia, hypertension | Includes hepatic system; comprehensive multiorgan view | Complex staging; emerging validation needs |
In 2023, the American Heart Association introduced Cardiovascular-Kidney-Metabolic (CKM) syndrome, defining it as "a systemic disorder characterized by pathophysiological interactions among metabolic risk factors, CKD, and the cardiovascular system leading to multiorgan dysfunction and a high rate of adverse cardiovascular outcomes" [4] [1]. This framework incorporated a staging system from stage 0 (no risk factors) to stage 4 (clinical CVD with complications) to capture disease progression [4].
Most recently in 2025, Theodorakis and Nikolaou proposed expanding CKM to CRHM syndrome to incorporate the liver's pivotal role, defining it as "a systemic disorder that leads to parallel multiorgan dysfunction driven by shared pathophysiological mechanisms, including metabolic inflammation (meta-inflammation) and dysregulation, especially insulin resistance" [4] [2]. This expansion acknowledges metabolic dysfunction-associated steatotic liver disease (MASLD) as both a driver and consequence of systemic metabolic dysfunction, completing the conceptual integration of major organ systems [4].
Pathophysiological Mechanisms and Continuum
The progression from isolated metabolic abnormalities to multisystemic dysfunction follows a recognizable pathophysiological continuum driven by core mechanistic processes.
Central Role of Adipose Tissue Dysfunction
Obesity, particularly visceral adiposity, initiates the pathological cascade through adipose tissue dysfunction characterized by impaired adipogenesis, resistance to insulin-mediated suppression of lipolysis, reduced fatty acid uptake, and excessive collagen deposition [1]. These structural and functional abnormalities promote chronic low-grade inflammation through immune cell infiltration and proinflammatory cytokine release [1]. When subcutaneous adipose storage capacity is exceeded, lipids accumulate in visceral depots and ectopic sites including liver, skeletal muscle, pancreas, and renal sinus [1].
Lipotoxicity and Organ-Specific Damage
Ectopic fat accumulation produces lipotoxicity—a toxic overload of lipids in non-adipose tissues that triggers organ-specific fibro-inflammatory responses [1]. The severity of cellular injury depends on factors including tissue resilience and the balance between inflammatory and fibrotic signaling [1]. This process contributes to insulin resistance, atherosclerosis, cardiac remodeling, hepatic inflammation (MASLD/MASH), and renal impairment [1].
Core Pathophysiological Drivers
Four interconnected pathophysiological drivers create a self-perpetuating cycle of multi-organ dysfunction in CRHM syndrome:
- Chronic Inflammation: Foundation of tissue damage through pro-inflammatory cytokines, immune activation, and fibrotic changes [2]
- Insulin Resistance: Fuels metabolic dysfunction, hyperglycemia, and lipid dysregulation [2]
- Oxidative Stress: Amplifies cellular injury through mitochondrial dysfunction and reactive oxygen species production [2]
- Endothelial Dysfunction: Impairs vascular integrity, increases arterial stiffness, and perpetuates ischemic injury [2]
These shared mechanisms explain the clinical clustering of conditions within CRHM syndrome and provide targets for therapeutic intervention.
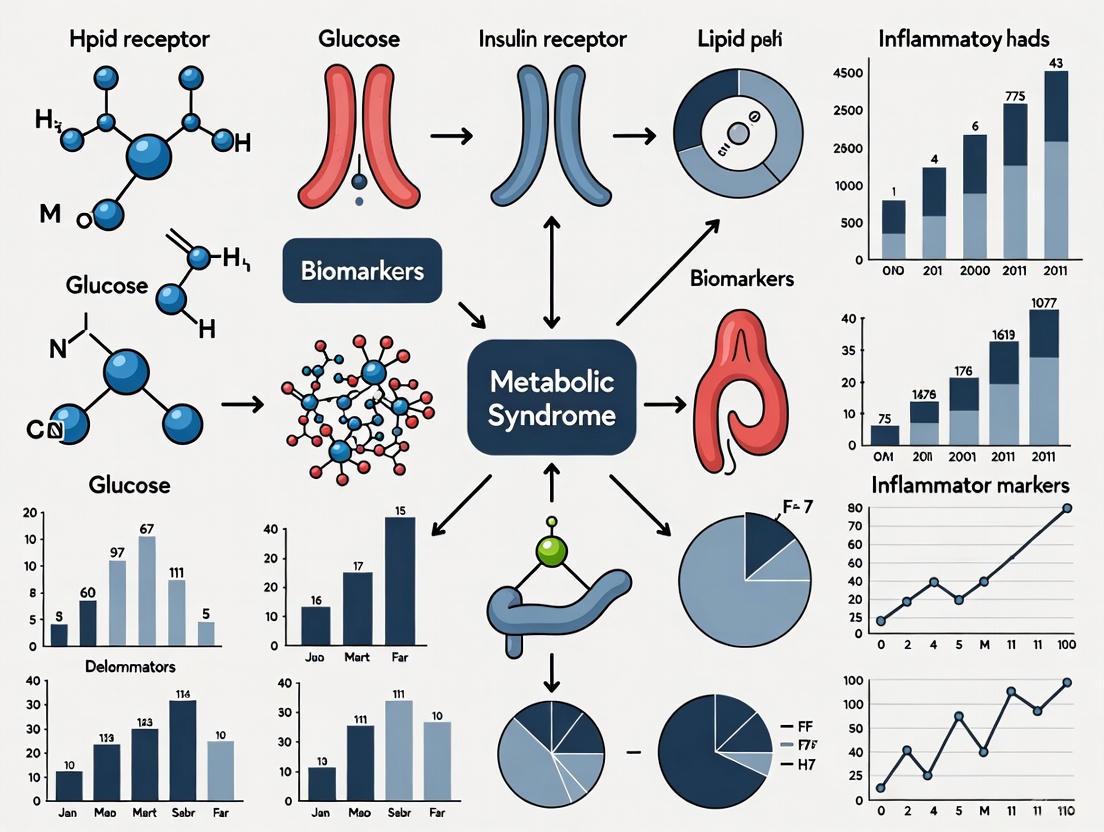
Diagram Title: Pathophysiological Pathways in CRHM Syndrome
Biomarker Advancements in Syndrome Research
The evolving syndrome concepts have driven corresponding advancements in biomarker research, particularly for metabolic syndrome and type 2 diabetes, with emerging biomarkers offering improved diagnostic, prognostic, and therapeutic monitoring capabilities.
Traditional and Emerging Circulating Biomarkers
Table 2: Biomarkers in Metabolic Syndrome and CRHM Syndrome Research
| Category | Biomarker | Association/Function | Research Utility | Considerations |
|---|---|---|---|---|
| Traditional Biomarkers | HbA1c [5] | Long-term glycemic control | Diabetes diagnosis and monitoring | Limited in certain populations |
| HOMA-IR [5] | Insulin resistance assessment | Research on insulin sensitivity | Lack of standardization | |
| CRP [2] | Systemic inflammation | Cardiovascular risk assessment | Limited specificity | |
| Emerging Circulating Biomarkers | suPAR [2] | Systemic chronic inflammation | Renal disease progression, cardiovascular risk | Stable inflammatory marker |
| GDF-15 [5] [2] | Cellular stress response, mitochondrial dysfunction | Obesity, insulin resistance, cardiovascular aging | Higher in males, older adults | |
| Galectin-3 [2] | Fibrosis and inflammation regulation | Cardiac remodeling, hepatic fibrosis, kidney disease | Multi-organ fibrosis marker | |
| Novel Omics-Based Biomarkers | miRNA-126 [2] | Vascular integrity | Endothelial dysfunction, atherosclerosis | Potential therapeutic target |
| miRNA-423-5p [2] | Heart failure progression | HF diagnosis and monitoring | Requires validation | |
| DNA methylation patterns [6] | Gene expression regulation | T2D risk prediction, early detection | Tissue-specific patterns | |
| Organ-Specific Biomarkers | ALDH3A1, CDK1, DEPDC1, HKDC1, SOX9 [5] | Glycolysis-related genes in MAFLD | MAFLD progression, immune infiltration | Hepatocyte-fibroblast-macrophage axis |
Growth differentiation factor 15 (GDF-15), a member of the TGF-β superfamily upregulated under cellular stress, has emerged as a promising biomarker with demonstrated associations with obesity, insulin resistance, and demographic factors. In a study of 2,083 participants from the Kuwait Diabetes Epidemiology Program, GDF-15 levels were significantly higher in males (580.6 vs. 519.3 ng/L, p < 0.001), participants >50 years (781.4 vs. 563.4 ng/L, p < 0.001), and those of Arab ethnicity compared to South/Southeast Asians [5]. Positive correlations were observed with BMI, waist circumference, blood pressure, insulin, and triglycerides, supporting its role as a metabolic disorder biomarker [5].
Soluble urokinase plasminogen activator receptor (suPAR) has emerged as a stable inflammatory biomarker associated with renal disease progression, cardiovascular risk, and metabolic disorders. Elevated suPAR levels correlate with CKD, atherosclerosis, and coronary artery calcification, with genetic studies linking suPAR to proinflammatory monocyte activation and vascular dysfunction [2].
Epigenetic Biomarkers and Omics Technologies
Epigenetic modifications, particularly DNA methylation, represent promising biomarker sources for T2D risk prediction and understanding disease mechanisms. DNA methylation (5-methylcytosine) at CpG sites regulates gene expression and is influenced by environmental factors including diet, chemical exposures, and chronic stress [6]. Microarray-based studies have identified epigenetic associations with T2D in blood and pancreatic β-cells, though sequencing-based approaches are increasingly advocated for improved genome-wide coverage [6].
The integration of multi-omics approaches is advancing biomarker discovery for complex metabolic conditions. In MAFLD research, integrative analysis of bulk RNA-seq, single-cell RNA-seq, and spatial transcriptomics has identified glycolysis-related key genes (ALDH3A1, CDK1, DEPDC1, HKDC1, SOX9) that discriminate MAFLD progression and interact with immune infiltration processes [5]. Single-cell analysis revealed the hepatocyte-fibroblast-macrophage axis as the predominant glycolysis-active niche, while spatial transcriptomics showed colocalization of CDK1, SOX9, and HKDC1 with the monocyte-derived macrophage marker CCR2 [5].
Experimental Models and Methodologies
Research into CRHM syndrome and its components employs diverse experimental approaches spanning basic science to clinical applications.
Biomarker Discovery and Validation Workflows
Comprehensive Protocol 1: Multi-Omics Analysis for MAFLD Biomarker Discovery
Sample Preparation and Data Generation
- Patient Cohort Selection: Recruit MAFLD patients and controls with detailed phenotyping (anthropometrics, metabolic parameters, liver histology)
- Tissue Collection: Obtain liver biopsies for bulk RNA-seq, single-cell RNA-seq, and spatial transcriptomics
- Library Preparation and Sequencing: Perform RNA sequencing using appropriate platforms (Illumina for bulk RNA-seq, 10x Genomics for single-cell RNA-seq, Visium for spatial transcriptomics)
Computational Analysis
- Differential Expression Analysis: Identify significantly dysregulated genes between MAFLD and control samples using appropriate statistical thresholds (FDR < 0.05, log2FC > 1)
- Weighted Gene Co-expression Network Analysis (WGCNA): Construct gene modules and identify glycolysis-correlated key genes
- Immune Infiltration Analysis: Utilize single-cell and spatial transcriptomics to characterize immune cell populations and interactions
- Machine Learning Application: Employ multiple models (random forest, SVM, etc.) to identify feature genes and predict MAFLD status
Experimental Validation
- External Cohort Validation: Confirm key gene expression patterns in independent patient cohorts
- In Vivo Models: Utilize methionine choline-deficient diet murine models to validate biomarker expression and functional significance
- Spatial Localization: Verify cellular colocalization of key biomarkers using immunohistochemistry and immunofluorescence [5]
Comprehensive Protocol 2: DNA Methylation Biomarker Studies for T2D
Study Design Considerations
- Population Selection: Include diverse populations, particularly Indigenous communities disproportionately affected by T2D
- Sample Type: Peripheral blood (most common), pancreatic β-cells (when available), or other relevant tissues
- Longitudinal Sampling: When possible, collect samples at multiple timepoints to establish temporal relationships
Laboratory Methods
- DNA Extraction: High-quality DNA isolation using standardized kits with quality control (spectrophotometry, fluorometry)
- Bisulfite Conversion: Treat DNA with bisulfite to convert unmethylated cytosines to uracils while preserving methylated cytosines
- Methylation Profiling:
- Microarray-Based: Illumina EPIC arrays for cost-effective genome-wide coverage of ~850,000 CpG sites
- Sequencing-Based: Whole-genome bisulfite sequencing for comprehensive coverage or targeted bisulfite sequencing for specific regions
- Validation: Pyrosequencing or targeted bisulfite sequencing for confirmation of significant CpG sites
Data Analysis
- Quality Control: Remove poor-quality probes, correct for batch effects, check for sample outliers
- Differential Methylation Analysis: Identify significantly differentially methylated positions/regions between cases and controls
- Functional Annotation: Associate methylation changes with genomic features (promoters, enhancers, gene bodies)
- Integration: Correlate methylation patterns with gene expression data when available [6]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for CRHM Syndrome Biomarker Studies
| Category | Specific Products/Platforms | Research Application | Key Features |
|---|---|---|---|
| Transcriptomics Platforms | Illumina RNA-seq [5] | Bulk gene expression analysis | Genome-wide expression profiling |
| 10x Genomics Single-Cell RNA-seq [5] | Single-cell resolution transcriptomics | Cellular heterogeneity analysis | |
| Visium Spatial Transcriptomics [5] | Tissue spatial gene expression mapping | Maintains spatial context of gene expression | |
| Epigenetics Tools | Illumina EPIC Methylation Arrays [6] | DNA methylation profiling | ~850,000 CpG sites coverage |
| Whole-genome bisulfite sequencing [6] | Comprehensive methylation analysis | Single-base resolution genome-wide | |
| Targeted bisulfite sequencing [6] | Validation of specific CpG sites | Cost-effective for specific regions | |
| Proteomics/Biomarker Assays | ELISA-based suPAR assays [2] | Quantitative suPAR measurement | High sensitivity and specificity |
| GDF-15 immunoassays [5] | GDF-15 quantification in plasma/serum | Research-use-only validated | |
| Mass spectrometry-based assays [7] | Protein/peptide quantification in diabetes | High precision and accuracy | |
| Animal Models | Methionine choline-deficient diet models [5] | MAFLD/MASH research | Recapitulates human disease features |
| High-fat diet rodent models [1] | Obesity and insulin resistance studies | Induces metabolic syndrome features | |
| Computational Tools | WGCNA R package [5] | Gene co-expression network analysis | Identifies correlated gene modules |
| Seurat/Single-cell analysis tools [5] | Single-cell RNA-seq data analysis | Comprehensive scRNA-seq processing |
Diagram Title: Biomarker Discovery Workflow for CRHM Syndrome
Diagnostic Staging and Clinical Translation
The evolution from MetS to CRHM syndrome has been accompanied by more sophisticated staging systems that enable better risk stratification and targeted interventions.
CRHM Syndrome Staging Framework
Table 4: Proposed Staging System for CRHM Syndrome
| Stage | Definition | Clinical Features | Management Focus |
|---|---|---|---|
| Stage 0 | No CRHM risk factors | No overweight/obesity, metabolic risk factors, CKD, MASLD, or CVD | Preventive lifestyle strategies |
| Stage I | Excess and/or dysfunctional adiposity | Stage Ia: Overweight (BMI ≥25 kg/m²) or high-normal waist circumference; Stage Ib: Obesity (BMI ≥30 kg/m²) or abdominal obesity; Stage Ic: Dysfunctional adiposity with prediabetes | Weight management, dietary intervention, physical activity |
| Stage II | Metabolic risk factors, CKD, or MASLD | One or more of: hypertension, hypertriglyceridemia, MetS, diabetes mellitus; Low-moderate risk CKD; MASLD with fibrosis stage F0-F1 | Risk factor control, monitoring for progression |
| Stage III | Subclinical CVD | Subclinical ASCVD or stage B HF among individuals with Stage I/II risk factors; Risk equivalents: very high 10-year cardiovascular risk, high/very high-risk CKD, MASLD with fibrosis stage F2-F4 | Intensive risk factor modification, consider organ-protective therapies |
| Stage IV | Clinical CVD | Clinical CVD (ASCVD, HF) among individuals with Stage I/II risk factors; Stage IVa: Without end-stage renal disease or cirrhosis; Stage IVb: With end-stage renal disease and/or cirrhosis | Multidisciplinary care, advanced disease management [4] |
Therapeutic Implications and Emerging Treatments
Novel therapeutic classes have demonstrated benefits across multiple organ systems in CRHM syndrome, supporting the integrated framework. Sodium-glucose cotransporter 2 inhibitors (SGLT2i), initially developed for glycemic control, have shown significant improvements in cardiovascular and renal outcomes in patients with and without diabetes [1]. Similarly, glucagon-like peptide-1 receptor agonists (GLP-1RAs) and combined gastric inhibitory polypeptide (GIP)/GLP-1 receptor agonists demonstrate multi-organ protective effects through antioxidant, anti-inflammatory, and anti-fibrotic mechanisms; enhancement of myocardial energetics; decreased neurohormonal activation; improved endothelial function; and reduced arterial stiffness [1].
These therapeutic advances align with the CRHM model by targeting shared pathophysiological pathways rather than individual disease states. Their mechanisms support the interconnected nature of cardiovascular, renal, hepatic, and metabolic systems and provide clinical validation of the syndrome concept.
Future Directions and Research Implications
The conceptual evolution from MetS to CRHM syndrome continues to shape research priorities and methodological approaches in several key areas:
Biomarker Innovation and Validation
Future biomarker development requires addressing several critical challenges. Emerging biomarkers must be validated across diverse populations, including Indigenous communities who experience disproportionate T2D burden but remain underrepresented in research [6]. For example, American-Indian young people experience more than double the burden of T2D compared to American young people overall (46.0 vs. 17.9 per 100,000) [6]. Biomarker discovery in these populations must be conducted ethically with community engagement and respect for data sovereignty.
Advanced technologies including sequencing-based DNA methylation analysis, single-cell multi-omics, and spatial transcriptomics will enable more comprehensive biomarker discovery [5] [6]. The transition from microarray to sequencing-based approaches for DNA methylation analysis provides improved genome-wide coverage and better capture of genetic and environmental complexities in T2D [6].
Precision Medicine and Population-Specific Approaches
The future of CRHM syndrome management lies in precision medicine approaches that account for individual variability in genetics, environment, and lifestyle. This requires:
- Development of integrated biomarker panels that combine traditional and novel biomarkers for improved risk stratification
- Refinement of staging systems to incorporate biomarker data for more dynamic progression monitoring
- Implementation of standardized protocols for biomarker testing and interpretation to ensure clinical utility
- Education and training for healthcare providers to effectively utilize biomarker data in clinical decision-making [5]
Interdisciplinary Research Models
Addressing the complexity of CRHM syndrome necessitates breaking down traditional silos between cardiology, nephrology, hepatology, and endocrinology. Future research should embrace:
- Integrated experimental models that capture multi-organ interactions rather than studying systems in isolation
- Clinical trial designs that evaluate outcomes across multiple organ systems simultaneously
- Collaborative research networks that bring together specialists from different disciplines
- Shared data repositories that enable comprehensive analysis of interconnected physiological systems
The conceptual evolution from Metabolic Syndrome to Cardiovascular-Renal-Hepatic-Metabolic syndrome represents a paradigm shift in understanding interconnected metabolic disorders. This progression reflects an increasingly sophisticated appreciation of the shared pathophysiological mechanisms driving multisystemic dysfunction, particularly relevant in the context of metabolic syndrome and type 2 diabetes research. The CRHM framework acknowledges the intricate interactions between cardiovascular, renal, hepatic, and metabolic systems, moving beyond organ-specific approaches to embrace a more holistic understanding of disease pathogenesis.
For researchers and drug development professionals, this evolving conceptual landscape presents both challenges and opportunities. The development and validation of novel biomarkers—from traditional circulating markers to epigenetic signatures and multi-omics profiles—are essential for advancing early detection, risk stratification, and therapeutic monitoring. Emerging therapeutic classes with multi-organ protective effects provide clinical validation of the CRHM concept and offer promising avenues for intervention. As research methodologies continue to advance, embracing integrated, interdisciplinary approaches will be crucial for addressing the complex pathophysiology of CRHM syndrome and developing effective, personalized strategies for prevention and treatment.
The global rise in metabolic syndrome (MetS) and type 2 diabetes mellitus (T2DM) represents a critical public health challenge, driven by the intertwined pathophysiological forces of insulin resistance, chronic inflammation, and oxidative stress [8] [9]. These core mechanisms create a self-sustaining cycle that promotes disease progression and leads to serious complications, including cardiovascular disease, neurodegenerative disorders, and cancer [10] [11]. Understanding these interconnected pathways is paramount for developing novel biomarkers and targeted therapeutic strategies. This whitepaper provides an in-depth analysis of these mechanisms, framed within the context of advanced biomarker research for MetS and T2DM, offering a technical guide for researchers and drug development professionals.
Molecular Mechanisms of Insulin Resistance
Insulin Signaling Pathway and Disruption Mechanisms
Insulin resistance (IR) is a state of diminished responsiveness to insulin stimulation in key target tissues—primarily liver, skeletal muscle, and adipose tissue [12]. The canonical insulin signaling pathway is initiated when insulin binds to its cell-surface receptor (INSR), triggering a phosphorylation cascade that involves the recruitment and tyrosine phosphorylation of insulin receptor substrate (IRS) proteins, activation of PI3-kinase (PI3K), and subsequent activation of AKT isoforms [12].
The table below summarizes key defects in the insulin signaling pathway that contribute to insulin resistance:
Table 1: Defects in Insulin Signaling Pathways Leading to Insulin Resistance
| Signaling Component | Defect Type | Functional Consequence | Associated Tissues |
|---|---|---|---|
| Insulin Receptor (INSR) | Decreased surface content; Reduced kinase activity | Impaired insulin binding and signal initiation [12] | Liver, Muscle, Adipose |
| IRS Proteins | Reduced expression; Serine phosphorylation | Decreased PI3K binding and activation [12] | Muscle, Liver |
| PI3K | Inhibited expression/activity | Attenuated AKT activation [12] | Muscle, Liver |
| AKT | Impaired phosphorylation (Ser473) | Reduced downstream signaling [12] | Muscle, Liver |
| GLUT4 | Impaired translocation | Decreased insulin-stimulated glucose uptake [12] | Muscle, Adipose |
Experimental Models for Studying Insulin Resistance
Investigating these complex mechanisms requires robust experimental methodologies. The following protocol outlines a standard approach for assessing insulin sensitivity in vitro and in vivo.
Table 2: Core Experimental Protocol for Insulin Resistance Research
| Experimental Stage | Key Methodologies | Measured Parameters |
|---|---|---|
| 1. In Vivo Assessment | Hyperinsulinemic-Euglycemic Clamp (Gold Standard) [11] | Whole-body insulin sensitivity; Tissue-specific glucose disposal rates |
| Homeostatic Model Assessment (HOMA-IR) [11] | Fasting insulin and glucose levels to estimate IR | |
| Oral Glucose Tolerance Test (OGTT) [11] | Postprandial glucose metabolism and insulin response | |
| 2. In Vitro Models | Cell culture (e.g., L6 myotubes, 3T3-L1 adipocytes, HepG2 hepatocytes) treated with high glucose/FFA [12] | Insulin-stimulated glucose uptake; IRS/PI3K/AKT phosphorylation |
| 3. Molecular Analysis | Western Blot; Immunoprecipitation [12] | Protein expression and phosphorylation status in signaling pathways |
| 4. Advanced 'Omics | Metabolomics (NMR, Mass Spectrometry) [13] | Circulating metabolites (e.g., BCAAs, triglycerides, HDL) |
Chronic Inflammation as a Metabolic Driver
Inflammatory Pathways in Metabolic Disease
Chronic, low-grade inflammation is a cornerstone of metabolic dysfunction, characterized by persistent immune activation and elevated levels of pro-inflammatory cytokines [10] [14]. Adipose tissue, particularly in visceral obesity, acts as a primary endocrine organ, releasing adipokines, cytokines, and chemokines that sustain this inflammatory state [5] [15]. Key mediators include Tumor Necrosis Factor-alpha (TNF-α), Interleukin-6 (IL-6), and C-Reactive Protein (CRP) [14] [15].
These inflammatory molecules directly interfere with insulin signaling. TNF-α, for instance, promotes serine phosphorylation of IRS-1, rendering it a poorer substrate for the INSR and targeting it for degradation, thereby disrupting the insulin signal transduction cascade [14]. This creates a direct molecular link between inflammation and insulin resistance.
Biomarkers of Metabolic Inflammation
The table below summarizes key inflammatory biomarkers relevant to MetS and T2DM research:
Table 3: Key Inflammatory Biomarkers in Metabolic Syndrome and T2DM
| Biomarker | Cellular Origin | Pathophysiological Role | Association with IR/MetS |
|---|---|---|---|
| TNF-α | Macrophages, Adipocytes | Induces serine phosphorylation of IRS-1; Suppresses GLUT4 expression [14] | Strongly positive; levels correlate with obesity and IR [14] |
| IL-6 | Immune Cells, Adipocytes (~30%) | Hepatic CRP synthesis; Impairs insulin signaling [14] | Elevated in T2DM; predicts disease progression [14] |
| CRP | Liver (induced by IL-6) | Acute-phase reactant; Non-specific marker of inflammation [14] | Independent predictor of T2DM and CVD risk [14] |
| Leptin | Adipocytes | Regulates appetite/satiety; Pro-inflammatory at high levels [5] | Increases with adiposity (leptin resistance) [5] |
| Adiponectin | Adipocytes | Enhances insulin sensitivity; Anti-inflammatory [5] | Reduced in obesity and IR [5] |
| GDF-15 | Multiple tissues under stress | Member of TGF-β superfamily; cellular stress response marker [15] | Associated with obesity, IR, and diabetic traits [15] |
Oxidative Stress and Redox Imbalance
Oxidative stress (OS) arises from an imbalance between the production of reactive oxygen species (ROS) and the body's antioxidant defense capabilities [16]. In metabolic diseases, chronic nutrient excess (glucose and lipids) drives mitochondrial dysfunction and ROS overproduction through multiple pathways, including the polyol pathway, advanced glycation end-product (AGE) formation, and activation of protein kinase C (PKC) [16] [14].
ROS directly damage cellular components—lipids, proteins, and DNA—and act as signaling molecules that disrupt insulin action. Specifically, ROS can inhibit insulin signaling by oxidizing critical components in the pathway, further exacerbating insulin resistance [16] [14]. This establishes a vicious cycle where hyperglycemia-induced ROS impairs insulin secretion and action, leading to worsened hyperglycemia.
Biomarkers of Oxidative Stress
Clinically validated biomarkers are essential for quantifying oxidative stress. The table below details key OS biomarkers and their significance in metabolic disease.
Table 4: Established and Emerging Biomarkers of Oxidative Stress
| Biomarker Category | Specific Marker | Significance / Mechanism | Measurement Method |
|---|---|---|---|
| Lipid Peroxidation | F2-isoprostanes | Gold standard; stable peroxidation products of arachidonic acid [16] | Gas chromatography-mass spectrometry (GC-MS) |
| DNA Damage | 8-Hydroxy-2'-deoxyguanosine (8-OHdG) | Oxidative modification of guanine in DNA; marker of genomic damage [16] | ELISA, Liquid chromatography-mass spectrometry (LC-MS) |
| Antioxidant Enzymes | Superoxide Dismutase (SOD), Glutathione Peroxidase (GPX1), Catalase (CAT) | Key enzymatic defenses; their activity/levels often altered in disease [14] | Activity assays, ELISA |
| Glycated Proteins | HbA1c | Indirect marker of oxidative burden; reflects sustained hyperglycemia [5] | High-performance liquid chromatography (HPLC) |
Interplay and Amplification Loops
The pathophysiological triad of IR, inflammation, and OS does not operate in isolation. Instead, they engage in complex crosstalk and form positive feedback loops that drive metabolic decline.
- Inflammation → Oxidative Stress: Pro-inflammatory cytokines like TNF-α can activate NADPH oxidases (NOX), major enzymatic sources of ROS, thereby increasing oxidative stress [16].
- Oxidative Stress → Inflammation: ROS activate redox-sensitive transcription factors, such as Nuclear Factor-kappa B (NF-κB), which in turn upregulate the expression of pro-inflammatory genes (e.g., TNF-α, IL-6), perpetuating the inflammatory state [8] [16].
- Adipose Tissue as a Hub: Dysfunctional, expanded adipose tissue is a primary site for this crosstalk, releasing both inflammatory cytokines and non-esterified fatty acids (NEFAs). Elevated NEFAs contribute to lipotoxicity, further promoting ectopic fat deposition, mitochondrial dysfunction, ROS production, and IR in liver and muscle [12] [11].
The Researcher's Toolkit
Key Research Reagent Solutions
Advancing research in this field relies on a suite of specialized reagents and tools. The following table details essential solutions for investigating these core mechanisms.
Table 5: Essential Research Reagents for Investigating Core Metabolic Mechanisms
| Reagent / Tool Category | Specific Examples | Research Application / Function |
|---|---|---|
| Cell-Based Assay Kits | Glucose Uptake Assay Kits (e.g., fluorescent 2-NBDG) | Quantify insulin-stimulated glucose uptake in cultured cells (myotubes, adipocytes) [12] |
| ELISA Kits | Phospho-specific ELISAs (e.g., p-AKT, p-IRS-1); Cytokine ELISAs (TNF-α, IL-6, Adiponectin); OS Marker ELISAs (8-OHdG) | Measure protein phosphorylation, inflammatory markers, and oxidative damage in cell lysates, tissue homogenates, or serum/plasma [14] |
| Metabolomic Panels | NMR-based metabolomic profiling (e.g., Nightingale Health panel) | Quantify 100+ circulating metabolites (lipids, fatty acids, glycoproteins, amino acids) for network analysis [13] |
| Signal Pathway Modulators | PI3K Inhibitors (e.g., LY294002); AKT Inhibitors; TNF-α neutralizing antibodies; Nrf2 activators | Chemically probe specific nodes in insulin, inflammatory, and antioxidant signaling pathways [12] [16] |
| Animal Models | High-Fat Diet Fed Mice; ob/ob and db/db Mice; ZDF Rats | Model human MetS and T2DM to study disease progression and therapeutic interventions in vivo [8] |
Emerging Biomarkers and Therapeutic Targets
The application of omics technologies is revealing novel biomarkers and potential therapeutic targets. Branched-chain amino acids (BCAAs), total triglycerides, and large HDL cholesterol have been identified as central hubs in the T2DM risk metabolome network, with BCAA levels serving as potent early indicators in pre-T2DM individuals [13]. The inflammatory glycoprotein GlycA demonstrates female-specific risk associations [13]. Non-coding RNAs, such as serum miR-484, are also being investigated for their role in glucose metabolism and as potential diagnostic markers [15].
Emerging therapeutic strategies focus on breaking the cycles of dysfunction. These include mitochondria-targeted antioxidants (e.g., MitoQ), Nrf2 activators to restore redox balance, specific NOX isoform inhibitors, and interventions aimed at modulating the gut microbiota to reduce systemic inflammation and OS [8] [16].
Cardiometabolic diseases represent an escalating global health crisis, slowing or even reversing earlier declines in cardiovascular disease (CVD) mortality [1] [17]. The understanding of metabolic disorders has evolved dramatically from isolated disease models to a comprehensive framework recognizing intricate inter-organ communication. Cardiovascular-Renal-Hepatic-Metabolic (CRHM) syndrome has emerged as a conceptual framework describing interconnected pathophysiological mechanisms across multiple organ systems [2] [18]. While not yet a formal diagnosis, this paradigm provides valuable insights into shared disease processes and therapeutic strategies for addressing conditions that collectively intensify disease progression, elevating the risk of multi-organ dysfunction, morbidity, and mortality [2].
This syndromic concept extends the American Heart Association's Cardiovascular-Kidney-Metabolic (CKM) syndrome model by incorporating the liver's pivotal role in systemic metabolic dysfunction [17]. The proposed CRHM syndrome is defined as "a systemic disorder that leads to parallel multiorgan dysfunction driven by shared pathophysiological mechanisms, including metabolic inflammation (meta-inflammation) and dysregulation, particularly insulin resistance" [2] [18]. This framework captures the clinical reality that conditions once managed separately—obesity, type 2 diabetes (T2DM), atherosclerotic CVD, heart failure (HF), chronic kidney disease (CKD), and metabolic dysfunction-associated steatotic liver disease (MASLD)—are interconnected disorders sharing common pathophysiological pathways [1] [17].
Pathophysiological Mechanisms of Multi-Organ Cross-Talk
The pathophysiology of CRHM syndrome is driven by multifaceted interactions of unified mechanisms, creating a self-perpetuating cycle of multi-organ dysfunction. At its core, chronic inflammation acts as the foundation, initiating tissue damage through pro-inflammatory cytokines, immune activation, and fibrotic changes [2] [19]. Insulin resistance fuels this process, worsening metabolic dysfunction, hyperglycemia, and lipid dysregulation, which further strain the cardiovascular, renal, hepatic, and metabolic systems [2]. As the condition progresses, oxidative stress amplifies cellular injury, mitochondrial dysfunction, and reactive oxygen species (ROS) production, worsening organ failure [2]. Finally, endothelial dysfunction impairs vascular integrity, increases arterial stiffness, and perpetuates ischemic injury, creating a vicious cycle of multi-organ damage [2] [19].
Central Role of Adipose Tissue Dysfunction and Inflammation
Obesity-induced adipose tissue dysfunction initiates a chronic low-grade inflammatory state, or "meta-inflammation," which plays a pivotal role in developing cardio-renal-metabolic diseases [18] [19]. As adipose tissue expands, hypoxia and cellular stress trigger adipocyte death and recruit pro-inflammatory M1 macrophages, replacing anti-inflammatory M2 macrophages [18]. This phenotypic shift exacerbates inflammation and disrupts metabolic homeostasis. M1 macrophages secrete pro-inflammatory cytokines including TNF-α and IL-6, which impair insulin receptor signaling by activating serine kinases like c-Jun N-terminal kinase (JNK) and inhibitor of kappa B kinase-beta (IKK-β) [18]. These kinases phosphorylate insulin receptor substrates (IRS), reducing glucose transporter type 4 (GLUT4)-mediated glucose uptake and promoting insulin resistance [18].
The dysfunctional adiposity and ectopic fat deposition are central drivers of this pathophysiology [1]. When subcutaneous adipose tissue storage capacity is exceeded, lipids accumulate in visceral deposits and ectopic sites including the liver, skeletal muscle, pancreas, renal sinus, and even intramyocardial compartments [1]. This ectopic fat accumulation leads to lipotoxicity—a toxic overload of lipids in non-adipose tissues—provoking organ-specific fibro-inflammatory responses that contribute to systemic metabolic dysfunction and multi-organ damage [1].
Key Signaling Pathways in Inter-Organ Communication
Mechanistic investigations have revealed that aberrant activation of several signaling pathways constitutes a complex inflammatory regulatory network facilitating inter-organ crosstalk [19]. These pathways establish positive feedback loops among the heart, kidneys, liver, and metabolic tissues, amplifying pathological processes including oxidative stress, endothelial dysfunction, and fibrosis in a cascading manner [19]. The following diagram illustrates the core inflammatory signaling pathways and their interactions in CRHM syndrome:
The NF-κB pathway serves as a master regulator of inflammation, activated by cytokines, oxidative stress, and metabolic danger signals [19]. Once activated, it triggers transcription of numerous pro-inflammatory genes, creating a feed-forward loop that sustains chronic inflammation across organ systems. The JAK-STAT pathway transmits signals from cytokine receptors to the nucleus, modulating immune cell differentiation and inflammatory responses [19]. Simultaneously, PI3K-AKT pathway dysregulation impairs insulin signaling, creating a bridge between inflammatory and metabolic disturbances [19]. These pathways facilitate coordinated damage across cardiovascular, renal, hepatic, and metabolic systems, establishing the molecular basis for CRHM syndrome progression.
Organ-Specific Pathological Consequences
Cardiovascular System
Cardiac manifestations in CRHM syndrome include atherosclerosis, coronary artery disease, heart failure with preserved ejection fraction (HFpEF), and diabetic cardiomyopathy [19] [17]. Cardiovascular damage results from endothelial dysfunction, increased arterial stiffness, cardiac lipotoxicity, fibrosis, and impaired myocardial energetics [1] [17]. MASLD independently increases cardiovascular mortality risk (hazard ratio 1.30) and non-fatal CVD events (HR 1.40) [17].
Renal System
Chronic kidney disease in CRHM syndrome develops through multiple interconnected pathways: hemodynamic changes from systemic hypertension, glomerular hyperfiltration in diabetes, inflammatory glomerular and tubulointerstitial damage, and renal sinus lipid accumulation [19] [1]. Leptin, elevated in obesity, induces glomerulosclerosis and fibrosis while promoting oxidative stress in renal tubular epithelial cells [19].
Hepatic System
MASLD represents the hepatic manifestation of metabolic dysregulation, characterized by triglyceride accumulation in hepatocytes (>5% steatosis) [17]. Progression to metabolic dysfunction-associated steatohepatitis (MASH) involves hepatocyte injury, inflammation, and fibrosis driven by lipotoxicity and inflammatory cytokines [17]. The liver contributes to systemic insulin resistance and dyslipidemia, creating bidirectional relationships with other organ systems [17].
Emerging Biomarkers for CRHM Syndrome
Traditional inflammatory markers such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) have limitations in predicting long-term disease progression in CRHM syndrome [2] [18]. Emerging biomarkers offer novel insights into systemic disease mechanisms and potential for personalized medicine approaches. The following table summarizes key traditional and emerging biomarkers with their clinical associations and research applications:
Table 1: Biomarkers for Cardiovascular-Renal-Hepatic-Metabolic Syndrome
| Biomarker Category | Specific Biomarker | Pathophysiological Role | Organ System Associations | Research Applications |
|---|---|---|---|---|
| Traditional Inflammatory Markers | CRP | Acute phase reactant, general inflammation marker | Cardiovascular risk assessment | Limited specificity for long-term outcomes [2] |
| IL-6 | Pro-inflammatory cytokine | Systemic inflammation, atherosclerosis | Therapeutic target in clinical trials [19] | |
| TNF-α | Pro-inflammatory cytokine | Insulin resistance, endothelial dysfunction | Mechanism studies [18] [19] | |
| Emerging Biomarkers | suPAR | Systemic chronic inflammation, immune activation | CKD progression, atherosclerosis, coronary artery calcification [2] [18] | Predictive marker for renal and cardiovascular outcomes [2] |
| Galectin-3 | Fibrosis and inflammation regulation | Cardiac remodeling, hepatic fibrosis, kidney disease [2] [18] | Prognostic marker in heart failure and liver disease [2] | |
| GDF-15 | Mitochondrial dysfunction, cardiovascular aging | Metabolic stress, cardiovascular events [2] [18] | Risk stratification for cardiovascular aging [2] | |
| miR-126 | Angiogenesis, vascular integrity | Endothelial dysfunction, atherosclerosis [2] | Vascular health assessment [2] | |
| miR-423-5p | Heart failure progression | Myocardial stress, cardiac remodeling [2] | Heart failure monitoring [2] | |
| Metabolic Biomarkers | TyG-BMI | Insulin resistance surrogate | CVD risk in CKM syndrome [19] | Epidemiological research [19] |
| Stress Hyperglycemia Ratio (SHR) | Glycemic variability | All-cause mortality in CKM stages 0-3 [19] | Prognostic biomarker [19] |
Promising Novel Biomarker Profiles
Soluble urokinase plasminogen activator receptor (suPAR) has emerged as a stable and predictive biomarker of systemic chronic inflammation, with strong associations with renal disease progression, cardiovascular risk, and metabolic disorders [2] [18]. Elevated suPAR levels correlate with CKD, atherosclerosis, and coronary artery calcification, with genetic studies linking suPAR to proinflammatory monocyte activation and vascular dysfunction [2] [18].
Galectin-3, a key regulator of fibrosis and inflammation across multiple organ systems, is strongly associated with cardiac remodeling, hepatic fibrosis, and kidney disease progression [2] [18]. Elevated levels predict higher mortality in heart failure and correlate with liver fibrosis severity [2].
Growth Differentiation Factor-15 (GDF-15) is implicated in mitochondrial dysfunction and cardiovascular aging, with elevated levels observed in metabolic stress and cardiac injury [2] [18]. This biomarker responds to cellular stress and inflammation across organ systems.
MicroRNAs (miRNAs) including miR-126 (vascular integrity) and miR-423-5p (heart failure progression) show promise as biomarkers with altered expression patterns correlating with atherosclerosis, insulin resistance, and cardiac dysfunction [2] [18]. These regulatory RNAs offer potential as both biomarkers and therapeutic targets.
Experimental Models and Methodologies
In Vivo Models of Multi-Organ Disease
Animal models reproducing CRHM syndrome pathophysiology typically combine genetic predispositions with dietary interventions. The following table outlines key experimental approaches for modeling CRHM syndrome:
Table 2: Experimental Models for CRHM Syndrome Research
| Model Category | Specific Model | Induction Method | CRHM Manifestations | Research Applications |
|---|---|---|---|---|
| Diet-Induced Models | High-Fat, High-Fructose, High-Cholesterol Diet | 12-24 weeks special diet | Obesity, insulin resistance, hepatic steatosis, early cardiac/renal dysfunction [20] | Disease progression studies, therapeutic interventions |
| Western Diet + NASH-inducing components | High-fat diet with added cholesterol/fructose | Progressive MASLD/MASH, renal impairment, cardiovascular changes [20] | Liver-focused CRHM investigations | |
| Genetic Models | Leptin-deficient (ob/ob) or leptin receptor-deficient (db/db) mice | Natural mutations or genetic engineering | Severe obesity, insulin resistance, hepatic steatosis, cardiomyopathy [20] | Metabolic component studies |
| ApoE-/- or LDLR-/- mice with metabolic challenge | Genetic ablation + high-fat diet | Atherosclerosis, insulin resistance, hepatic steatosis [20] | Cardiovascular-metabolic interactions | |
| Combination Models | CKM syndrome mouse model | High-fat diet + low-dose streptozotocin + unilateral nephrectomy | Insulin resistance, hyperglycemia, renal dysfunction, cardiac fibrosis [20] | Comprehensive multi-organ studies |
| Aged mice with metabolic challenge | Aging + high-fat diet | Age-related multi-organ dysfunction, insulin resistance [20] | Aging-CRHM interactions |
Essential Research Reagent Solutions
The following research reagents are critical for investigating CRHM syndrome mechanisms and evaluating therapeutic interventions:
Table 3: Essential Research Reagents for CRHM Investigation
| Reagent Category | Specific Reagents | Research Application | Experimental Function |
|---|---|---|---|
| Cell Culture Models | Primary hepatocytes, adipocytes, renal tubular epithelial cells, endothelial cells | In vitro mechanistic studies | Cell-type specific signaling studies [19] |
| Immortalized cell lines (HepG2, THP-1, HK-2) | High-throughput screening | Therapeutic candidate evaluation [19] | |
| Antibodies for Signaling Pathways | Phospho-specific antibodies (p-NF-κB, p-AKT, p-STAT3) | Western blot, immunohistochemistry | Pathway activation assessment [19] |
| Cytokine antibodies (TNF-α, IL-6, IL-1β) | ELISA, flow cytometry | Inflammatory mediator quantification [19] | |
| Fibrosis markers (α-SMA, collagen I, galectin-3) | Immunohistochemistry, Western blot | Tissue remodeling evaluation [2] [19] | |
| Molecular Biology Tools | miRNA inhibitors/mimics (miR-126, miR-423-5p) | Transfection experiments | Functional miRNA studies [2] |
| qPCR assays for emerging biomarkers (suPAR, GDF-15, Galectin-3) | Gene expression analysis | Biomarker expression profiling [2] | |
| RNA-seq libraries | Transcriptomic profiling | Global gene expression patterns [20] | |
| Metabolic Assays | Glucose uptake assays (2-NBDG) | Cellular metabolism studies | Insulin sensitivity assessment [19] |
| Mitochondrial function kits (Seahorse) | Bioenergetics profiling | Metabolic flux analysis [19] | |
| Lipid quantification kits (triglycerides, free fatty acids) | Hepatic and plasma lipid measurement | Lipotoxicity assessment [19] |
Standardized Experimental Protocol for CRHM Assessment
The following workflow provides a comprehensive methodological approach for evaluating multi-organ cross-talk in experimental models:
Week 0: Baseline Characterization
- Metabolic parameters: Body weight, fasting blood glucose, oral glucose tolerance test (OGTT), insulin tolerance test (ITT), plasma lipid profile
- Cardiovascular assessment: Blood pressure measurement (tail-cuff or telemetry), echocardiography for cardiac structure and function
- Renal function: Urine albumin-to-creatinine ratio (UACR), plasma creatinine
- Hepatic status: Plasma ALT, AST measurements
Week 4-24: Intervention Period (depending on model)
- Dietary intervention: High-fat diet (45-60% kcal from fat) + high fructose (10-20%) in drinking water
- OR genetic model maintenance with standard monitoring
- Bi-weekly metabolic parameter assessment
Week 24: Terminal Endpoint Analyses
- Tissue collection (heart, kidney, liver, adipose tissue) with division for:
- Histopathology (formalin fixation)
- Molecular analyses (flash-freezing in liquid N₂)
- Primary cell isolation (immediate processing)
- Comprehensive tissue analysis:
Therapeutic Implications and Future Directions
Emerging Therapeutic Strategies Targeting Multi-Organ Pathways
Recent advances in pharmacotherapy have revealed several drug classes with pleiotropic effects across multiple organ systems in CRHM syndrome. These therapies target shared pathophysiological pathways rather than individual disease entities, representing a paradigm shift in management approach.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors, initially developed for glycemic control, have demonstrated significant benefits across cardiovascular, renal, and metabolic domains [1] [17]. Regardless of diabetes status, empagliflozin and dapagliflozin improve outcomes in heart failure and chronic kidney disease [1]. Proposed mechanisms include antioxidant, anti-inflammatory, and anti-fibrotic effects; enhancement of myocardial energetics; decreased neurohormonal activation; improved endothelial function; promoted vasodilation; reduced arterial stiffness; and increased natriuresis [1].
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) and dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists provide multi-organ protection through weight loss, glycemic control, and direct cardiorenal benefits [2] [1] [17]. These agents demonstrate direct cardiac and kidney benefits even within short-term trials [21].
Nonsteroidal mineralocorticoid receptor antagonists (e.g., finerenone) target fibrosis and inflammation across organ systems, showing particular promise for renal and cardiovascular protection in CRHM syndrome [1] [21].
The following table compares the multi-organ benefits of these therapeutic classes:
Table 4: Multi-Organ Benefits of Emerging CRHM Therapies
| Therapeutic Class | Cardiovascular Benefits | Renal Benefits | Hepatic Benefits | Metabolic Benefits |
|---|---|---|---|---|
| SGLT2 Inhibitors | Reduced HF hospitalizations, improved outcomes in HFrEF/HFpEF [1] | Slowed CKD progression, reduced albuminuria [1] | Potential improvement in hepatic steatosis [17] | Glycemic control, weight reduction, blood pressure lowering [1] |
| GLP-1 Receptor Agonists | Reduced MACE, atherosclerotic events [1] | Reduced albuminuria, slowed eGFR decline [1] | Improvement in MASLD metrics [17] | Significant weight reduction, glycemic control [1] |
| GIP/GLP-1 Receptor Agonists | Cardiovascular outcome trials ongoing [2] | Renal outcomes under investigation [2] | Significant improvement in MASH histology [2] | Superior weight reduction vs. GLP-1 RAs alone [2] |
| Nonsteroidal MRAs | Reduced CV death/HF hospitalization [1] | Slowed CKD progression, reduced albuminuria [1] | Anti-fibrotic effects in liver [21] | Modest metabolic improvements [1] |
Biomarker-Guided Therapeutic Approaches
Emerging biomarkers not only aid in early detection but also guide targeted interventions in CRHM syndrome [2]. Elevated levels of specific biomarkers may support personalized therapeutic decisions:
- Elevated suPAR levels: May indicate heightened systemic inflammation favoring SGLT2 inhibitors for cardiorenal protection [2]
- Increased galectin-3: Suggests active fibrotic processes potentially responsive to nonsteroidal MRAs [2]
- Rising GDF-15: Indicates mitochondrial dysfunction and metabolic stress potentially addressed by GLP-1RAs [2]
- Altered miRNA patterns: May identify specific pathway activations for targeted therapies [2]
Future Research Directions
The complex interplay of multi-organ dysfunction in CRHM syndrome presents both challenges and opportunities for future research. Multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) combined with machine learning may better capture common underlying mechanisms and inter-organ crosstalk [20]. There is a pressing need for more inclusive clinical trials that examine contributions of multimorbidity and incorporate multi-organ endpoints [20]. Additionally, anti-inflammatory therapies specifically targeting the inflammatory co-mechanisms of atherosclerotic cardiovascular disease and chronic kidney disease represent a promising frontier [21].
The integration of emerging biomarkers into clinical trial designs may enable better patient stratification and monitoring of treatment responses. Furthermore, understanding how social determinants of health and disparities influence CRHM syndrome progression requires focused investigation [21].
The conceptual evolution from isolated metabolic disorders to the comprehensive CRHM syndrome framework reflects growing appreciation of intricate multi-organ cross-talk. This paradigm recognizes that conditions affecting the cardiovascular, renal, hepatic, and metabolic systems share common pathophysiological roots including chronic inflammation, insulin resistance, oxidative stress, and endothelial dysfunction. The emerging biomarker landscape offers promising tools for early detection, risk stratification, and personalized therapeutic approaches. Simultaneously, novel therapeutic classes with pleiotropic effects across organ systems represent a paradigm shift in management strategy. Future research integrating multi-omics technologies, comprehensive clinical trials, and disparity-focused investigations will further advance our understanding and management of these interconnected conditions. Viewing these conditions as an integrated whole rather than discrete entities fosters a more holistic management approach essential for addressing the ongoing cardiometabolic health crisis.
Metabolic syndrome (MetS) and type 2 diabetes mellitus (T2DM) represent interconnected global health challenges characterized by insulin resistance, chronic inflammation, and metabolic dysregulation. The pathophysiology of these conditions is orchestrated by complex intracellular signaling networks that integrate genetic, environmental, and metabolic cues. Among these, three signaling pathways have emerged as critical regulators and potential biomarker sources: the phosphatidylinositol-3-kinase/protein kinase B (PI3K-Akt) pathway, the mitogen-activated protein kinase (MAPK) cascade, and the Toll-like receptor 4 (TLR4) innate immune signaling axis. These pathways not only govern core metabolic processes but also exhibit cross-talk that creates a signaling network whose dysregulation propagates metabolic dysfunction across tissues. This technical review examines the molecular architecture, experimental evidence, and biomarker potential of these pathways within the context of MetS and T2DM research, providing researchers and drug development professionals with current methodological frameworks for investigating these critical signaling networks.
PI3K-Akt Signaling: Central Regulator of Metabolic Homeostasis
Pathway Architecture and Metabolic Functions
The PI3K-Akt pathway serves as the primary intracellular signaling cascade for insulin-mediated metabolic regulation, coordinating glucose uptake, lipid metabolism, and protein synthesis. Upon insulin binding to its receptor, PI3K phosphorylates membrane phosphatidylinositol lipids, generating second messengers that recruit and activate Akt through phosphorylation at Thr308 and Ser473 residues. Activated Akt then propagates metabolic signals through downstream effectors including mTOR, GSK-3β, and FOXO transcription factors, promoting GLUT4 translocation to the plasma membrane and hepatic glycogen synthesis while inhibiting gluconeogenesis and lipolysis.
Dysregulation in Metabolic Syndrome and T2DM
Insulin resistance, a fundamental defect in both MetS and T2DM, manifests as impaired PI3K-Akt signaling. Recent human tissue research reveals distinctive expression patterns in adipose depots, with visceral adipose tissue (VAT) PI3K expression showing strong positive associations with hyperinsulinemia (β = 8.802, P = 0.008) and insulin resistance (β = 7.710, P = 0.028) [22]. Similarly, VAT Akt expression correlates with hyperinsulinemia (β = 6.684, P = 0.003) and insulin resistance (β = 5.296, P = 0.027) [22]. The pathway's negative regulator, PTEN, demonstrates an inverse relationship with insulin resistance (β = -4.475, P = 0.021) in subcutaneous adipose tissue [22], highlighting its potential therapeutic targeting value.
Table 1: PI3K-Akt Pathway Gene Expression Associations with Insulin Indices in Human Adipose Tissue
| Gene | Adipose Depot | Associated Metabolic Parameter | Effect Size (β) | P-value |
|---|---|---|---|---|
| PI3K | Visceral | Hyperinsulinemia | 8.802 | 0.008 |
| PI3K | Visceral | HOMA-IR | 7.710 | 0.028 |
| Akt | Visceral | Hyperinsulinemia | 6.684 | 0.003 |
| Akt | Visceral | HOMA-IR | 5.296 | 0.027 |
| Akt | Subcutaneous | Fasting Plasma Insulin | 0.128 | 0.048 |
| Akt | Subcutaneous | Hyperinsulinemia | 4.201 | 0.008 |
| PTEN | Subcutaneous | HOMA-IR | -4.475 | 0.021 |
Experimental Assessment Methodologies
Gene Expression Analysis in Human Adipose Tissue: The cross-sectional study design provides a robust methodology for investigating PI3K-Akt pathway activity in metabolic disease [22]. Adipose tissue biopsies (50-100 mg) are obtained during elective abdominal surgery, immediately frozen in liquid nitrogen, and stored at -80°C. RNA extraction using TRIzol reagent is followed by DNase I treatment to remove genomic DNA. After quality assessment via Nanodrop spectrophotometry (A260/280 ratio) and gel electrophoresis, cDNA synthesis employs commercial kits (e.g., BIOFACT, South Korea). Quantitative real-time PCR (qRT-PCR) using SYBR-Green PCR Master Mix on platforms such as the Corbett Rotor-Gene 6000 with cycling programs established in previous studies [22]. Relative quantitation applies the comparative CT method with GAPDH as the internal control, adhering to MIQE guidelines.
Functional Pathway Interrogation: Beyond gene expression, pathway activity assessment requires phosphorylation-specific immunoblotting for Akt residues (Thr308, Ser473) and downstream targets in tissue lysates from muscle, liver, or adipose tissue. Insulin clamp studies combined with tissue biopsies represent the gold standard for correlating pathway activity with whole-body insulin sensitivity in humans.
MAP Kinase Signaling: Integrating Stress and Metabolic Responses
Pathway Diversity and Metabolic Regulation
The MAPK pathways comprise three major branches: extracellular signal-regulated kinase (ERK1/2), c-Jun N-terminal kinase (JNK), and p38 MAPK. These cascades translate extracellular stimuli into adaptive intracellular responses, with ERK typically activated by growth factors and mitogens, while JNK and p38 respond to cellular stressors including inflammatory cytokines, oxidative stress, and lipotoxicity. In metabolic tissues, MAPK signaling regulates cell proliferation, differentiation, apoptosis, and insulin sensitivity, with pathway- and context-specific outcomes.
Pathway Activation in Metabolic Dysfunction
Sustained activation of stress-responsive MAPK branches (JNK and p38) significantly contributes to insulin resistance development. In diabetic kidney disease (DKD), metformin mediates renal protection through MAPK pathway modulation, specifically engaging MAPK1 and MAPK3 (ERK1/2) [23]. Phosphoproteomic analyses reveal metformin's influence on phosphorylation states of MAPK pathway components, with carbohydrate metabolites like D-xylose identified as potential biomarkers for therapeutic monitoring [23]. The resistin/TLR4/miR-155-5p axis in hypothalamic inflammation activates JNK and p38 MAPK signaling, establishing a novel neuroinflammatory pathway that impairs whole-body glucose homeostasis [24].
Experimental Assessment Methodologies
Phosphoproteomic Analysis in Metabolic Tissues: Comprehensive MAPK pathway investigation requires phosphoproteomic approaches [23]. Kidney tissue homogenization is followed by protein extraction and tryptic digestion. Phosphopeptide enrichment employs TiO2 or IMAC columns before LC-MS/MS analysis on high-resolution instruments (e.g., Q-Exactive HF-X). Data processing with MaxQuant or similar platforms identifies phosphorylation sites, with differential phosphorylation analysis between experimental groups (e.g., db/db mice with/without metformin treatment). Functional enrichment analysis (KEGG, GO) reveals pathway-level alterations, with validation through immunoblotting using phospho-specific antibodies for ERK1/2 (Thr202/Tyr204), JNK (Thr183/Tyr185), and p38 (Thr180/Tyr182).
Integrated Multi-omics Approach: Network pharmacology predicts metformin-MAPK interactions, with phosphoproteomic validation in target tissues and metabolomic correlation in blood/urine samples [23]. This integrated framework identifies conserved therapeutic targets across species, enhancing translational relevance.
Table 2: MAPK Pathway Components in Metabolic Disease Models
| MAPK Branch | Metabolic Context | Activation State | Functional Consequences |
|---|---|---|---|
| ERK1/2 (MAPK1/3) | Diabetic Kidney Disease | Modulated by metformin | Renoprotective effects |
| JNK | Hypothalamic Inflammation | Activated by resistin/TLR4 | Insulin resistance, glucose intolerance |
| p38 | Hypothalamic Inflammation | Activated by resistin/TLR4 | Microglial activation, neuroinflammation |
| ERK1/2 | Skeletal Muscle | Redox-sensitive | Impacts insulin sensitivity |
| JNK | Hepatic steatosis | Activated by lipotoxicity | Promotes hepatic insulin resistance |
TLR4 Activation: Bridging Innate Immunity and Metabolic Inflammation
Pathway Mechanism and Metabolic Implications
Toll-like receptor 4 (TLR4) functions as a pattern recognition receptor that activates innate immune responses upon detecting pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). Saturated fatty acids represent relevant DAMPs in metabolic disease, initiating TLR4 signaling that converges on NF-κB and MAPK activation through adaptor proteins MyD88, IRAK1, and TRAF6. This cascade induces proinflammatory cytokine production (TNF-α, IL-6, IL-1β) that interferes with insulin signaling through serine phosphorylation of IRS proteins, establishing a molecular link between nutrient excess, inflammation, and insulin resistance.
TLR4 Signaling in Metabolic Tissues
Clinical studies demonstrate significant overexpression of TLR2 and TLR4 in PBMCs from T2DM patients compared to healthy controls (p < 0.001) [25]. Strong positive correlations exist between TLR4 and its adaptor proteins in controls: MyD88 (r = 0.79), IRAK1 (r = 0.83), and TRAF6 (r = 0.87) [25]. These correlations persist in T2DM patients, though moderately attenuated: MyD88 (r = 0.5), IRAK1 (r = 0.4), and TRAF6 (r = 0.8) [25]. In the hypothalamus, the resistin/TLR4/miR-155-5p axis drives neuroinflammation through NF-κB, JNK, and p38 MAPK signaling, with HFD consumption increasing hypothalamic resistin expression and subsequent microglial activation [24].
Experimental Assessment Methodologies
Gene Expression in Human PBMCs: Peripheral blood mononuclear cells (PBMCs) offer an accessible tissue for evaluating TLR4 pathway activity in clinical studies [25]. After overnight fasting, blood collection in EDTA-containing tubes is followed by PBMC isolation via density gradient centrifugation. RNA extraction and qRT-PCR analysis measure expression levels of TLR2, TLR4, and adaptor proteins (MyD88, IRAK1, TRAF6), with normalization to appropriate housekeeping genes. Correlation analyses between receptor and adaptor expression levels provide insights into pathway coordination in health and disease states.
Hypothalamic Neuroinflammation Models: Investigation of central TLR4 signaling requires specialized approaches [24]. Intracerebroventricular (ICV) cannulation enables direct administration of resistin or TLR4 agonists/antagonists. Hypothalamic tissue collection followed by qPCR for inflammatory markers (IL-1β, TNF-α, NF-κB, TLR4) and microglial activation markers (IBA1, CD68). Immunofluorescence staining for IBA1 in mediobasal hypothalamus assesses microglial activation status through morphological changes and staining intensity. Microglial cell lines (e.g., SIM-A9) facilitate in vitro mechanistic studies of miR-155-5p regulation and target identification.
Cross-Pathway Integration and Therapeutic Implications
Signaling Network Interdependencies
The PI3K-Akt, MAPK, and TLR4 pathways do not function in isolation but exhibit extensive cross-talk that creates a coordinated signaling network. TLR4 activation inhibits PI3K-Akt signaling through inflammatory kinase-mediated serine phosphorylation of IRS proteins, while PI3K-Akt can negatively regulate TLR4 signaling through mTOR-dependent mechanisms. MAPK pathways serve as integration points, with ERK potentially enhancing insulin signaling under certain conditions while JNK and p38 typically oppose it. This network-level understanding explains why targeted therapeutic interventions often produce pleiotropic metabolic effects.
Biomarker and Therapeutic Applications
Metabolomic approaches identify pathway-associated biomarkers with diagnostic and prognostic utility. In DKD, D-xylose emerges as a potential biomarker for metformin response, linked to MAPK pathway modulation [23]. Lysophosphatidylcholines (LPCs 14:0, 20:4) and the dipeptide Gly-His show altered plasma levels in elderly T2DM patients, reflecting underlying perturbations in lipid metabolism and inflammation [26]. Mitochondria-related genes SLC2A2, ENTPD3, ARG2, CHL1, and RASGRP1 identified through machine learning approaches predict T2DM with AUC >0.8 and correlate with immune cell infiltration patterns [27].
Established therapeutics like metformin demonstrate multi-pathway influence, modulating MAPK signaling [23] and cellular redox state in skeletal muscle [28]. Traditional Chinese medicine polyphenols target multiple pathways simultaneously, regulating gut microbiota homeostasis and affecting AMPK, PPAR, MAPK, PI3K/Akt and NF-κB pathways [8]. This multi-target approach may explain their efficacy against MetS complex pathophysiology.
Research Toolkit: Essential Methodologies and Reagents
Table 3: Essential Research Reagents and Methodologies for Pathway Analysis
| Category | Specific Reagents/Methods | Application | Technical Notes |
|---|---|---|---|
| Gene Expression | TRIzol RNA extraction, DNase I treatment, qRT-PCR with SYBR Green | Quantifying pathway components in tissues | Follow MIQE guidelines; use appropriate reference genes |
| Protein Analysis | Phospho-specific antibodies (Akt, ERK, JNK, p38), Western blot | Assessing pathway activation states | Validate antibody specificity; include total protein controls |
| Metabolomics | UPLC-MS, targeted carbohydrate metabolomics | Identifying metabolic biomarkers | Use quality control pools; randomize injection order |
| Cell Culture Models | SIM-A9 microglial cells, palmitate treatment | Studying lipotoxicity and inflammation | Use appropriate FFA:BSA ratios; control for osmolarity |
| Animal Models | db/db mice, HFD-fed mice, ICV cannulation | In vivo pathway manipulation | Monitor metabolic phenotypes; control for sex differences |
| Pathway Analysis | Network pharmacology, KEGG enrichment, phosphoproteomics | Systems-level pathway mapping | Integrate multi-omics datasets; use appropriate FDR correction |
The PI3K-Akt, MAPK, and TLR4 signaling pathways represent interconnected regulatory networks whose dysregulation propagates metabolic dysfunction in MetS and T2DM. Comprehensive investigation of these pathways requires integrated methodological approaches spanning molecular techniques, omics technologies, and physiological validation. The continuing identification of pathway-associated biomarkers and therapeutic targets holds promise for advancing personalized management of metabolic diseases, with multi-target interventions potentially offering advantages for addressing the complex pathophysiology of these conditions.
Biomarker Discovery and Analytical Techniques in Clinical Practice
In the landscape of metabolic syndrome and type 2 diabetes (T2D) research, established clinical biomarkers provide critical windows into pathophysiological processes, enabling early detection, risk stratification, and therapeutic monitoring. HbA1c, HOMA-IR, and lipid profiles represent cornerstone biochemical measurements that collectively offer insights into glycemic control, insulin sensitivity, and atherogenic dyslipidemia—the fundamental triad of metabolic dysregulation. Within drug development, these biomarkers serve essential roles across the spectrum from diagnostic and prognostic tools to pharmacodynamic response indicators and surrogate endpoints [29]. The rigorous validation of these biomarkers according to their specific context of use (COU) makes them indispensable for clinical trial design and regulatory evaluation of novel therapies targeting metabolic disorders [29].
This technical guide provides researchers and drug development professionals with a comprehensive resource on the analytical methodologies, clinical applications, and emerging innovations surrounding these established biomarkers, with particular emphasis on their integration in contemporary research frameworks and their utility in predicting hard clinical endpoints.
HbA1c: The Cornerstone of Glycemic Control Assessment
Analytical Methodology and Physiological Basis
Hemoglobin A1c (HbA1c) reflects average blood glucose levels over the preceding 2-3 months, corresponding to the red blood cell lifespan. It forms through non-enzymatic glycation of the hemoglobin beta-chain valine residue, with the rate of formation directly proportional to ambient glucose concentrations [30]. The 2025 DMSO study highlights its established role as both a diagnostic biomarker for diabetes and a monitoring biomarker for long-term glycemic control [30] [29].
Table 1: HbA1c Interpretation Standards in Clinical Practice and Research
| Category | HbA1c Range | Clinical Significance | Clinical Trial Context |
|---|---|---|---|
| Normal | <5.7% | Normal glucose homeostasis | Reference group for comparative studies |
| Prediabetes | 5.7% - 6.4% | Increased diabetes risk | Target population for prevention trials |
| Diabetes | ≥6.5% | Diabetes diagnosis | Inclusion criterion for efficacy trials |
| Treatment Target | <7.0% | Standard glycemic goal | Primary/secondary endpoint in intervention studies |
Research Applications and Correlation with Systemic Manifestations
In drug development, HbA1c serves as a primary efficacy endpoint for glucose-lowering therapies and is recognized by regulatory agencies as a validated surrogate endpoint for diabetes-related complications [29]. Recent research has expanded its contextual utility through correlations with multisystem physiological changes quantifiable via advanced imaging.
A 2024 Scientific Reports study demonstrated that HbA1c levels show significant, progressive correlations with CT-based body composition biomarkers, even in prediabetic ranges [31]. These correlations reveal the multisystem nature of metabolic syndrome and provide quantitative imaging biomarkers that may complement HbA1c in clinical trials:
- Visceral Adipose Tissue (VAT): 53% increase between normal (HbA1c <5.7%) and poorly-controlled diabetes (HbA1c >7.0%) in female cohort
- Organ Volumes: 22% increase in kidney volume and 24% increase in liver volume across the same HbA1c spectrum
- Tissue Density Changes: 6% decrease in liver density (indicating hepatic steatosis) and 21% decrease in skeletal muscle density (indicating myosteatosis)
These objective CT biomarkers demonstrate that metabolic syndrome manifestations begin in the prediabetic phase and can be quantitatively tracked alongside HbA1c in longitudinal intervention studies [31].
Standardized Management and Predictive Modeling
The clinical utility of HbA1c is enhanced through structured management programs. A 2025 study evaluating China's National Metabolic Management Center (MMC) model demonstrated significant improvements in HbA1c levels following standardized management, with the absolute HbA1c level decreasing and the rate of achieving target (<7%) significantly enhanced (P<0.05) [30].
Multivariate analysis identified independent predictors for HbA1c target achievement, which were incorporated into a predictive nomogram:
- Protective Factors: Fasting blood glucose (FBG) and hematocrit (HCT)
- Risk Factor: Albumin (ALB)
The resulting predictive model exhibited favorable discriminative ability (c-index: 0.747, 95% CI: 0.703–0.790), providing a valuable tool for identifying patients who may require more intensive interventions [30].
HOMA-IR and Surrogate Indices of Insulin Resistance
Methodological Framework and Calculation
The Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) estimates insulin resistance from fasting glucose and insulin measurements using the formula: HOMA-IR = [Fasting Insulin (µU/mL) × Fasting Glucose (mmol/L)] / 22.5 [32] [33]. While the hyperinsulinemic-euglycemic clamp remains the gold standard for direct insulin sensitivity measurement, its complexity and cost limit widespread application [34] [35] [32].
Table 2: Insulin Resistance Indices: Comparative Methodologies and Performance Characteristics
| Index | Formula | Components | AUC Range | Population-Specific Cut-offs |
|---|---|---|---|---|
| HOMA-IR | (Fasting Insulin × Fasting Glucose)/22.5 | Insulin, Glucose | 0.83-0.92 | 1.878 (Qatari population) [32] |
| TyG Index | ln[Fasting TG (mg/dL) × Fasting Glucose (mg/dL)/2] | Triglycerides, Glucose | 0.83-0.92 | 8.281 (Qatari) [32] |
| McAuley Index | exp{2.63 - 0.28ln[Insulin] - 0.31ln[TG]} | Insulin, Triglycerides | 0.83-0.92 | 7.727 (Qatari) [32] |
| TG/HDL Ratio | Triglycerides/HDL-C | Lipids only | 0.83-0.92 | 1.718 (Qatari) [32] |
| QUICKI | 1/[log(Fasting Insulin) + log(Fasting Glucose)] | Insulin, Glucose | 0.83-0.92 | 0.347 (Qatari) [32] |
Comparative Performance of IR Indices
Comprehensive validation studies enable evidence-based selection of IR indices for specific research contexts. A 2025 Frontiers in Endocrinology study compared seven surrogate IR indices in the Qatar Biobank cohort (n=7,875), reporting AUC values ranging from 0.83 to 0.92 for all indices [32]. The Triglyceride-Glucose (TyG) index emerged as the most robust measure (AUC=0.92, sensitivity=0.90, specificity=0.79), offering practical advantages in settings where insulin measurement is unavailable or cost-prohibitive [32].
The TyG index has demonstrated particular utility in specialized populations, including COVID-19 associated dysglycemia. A 2025 pilot study found the TyG index strongly associated with newly diagnosed DM in COVID-19 patients (Crude OR: 11.25, 95% CI: 2.80-76.28; Adjusted OR: 6.83, 95% CI: 1.57, 42.96) [35]. When combined with BMI, the TyG index showed improved predictive accuracy (AUC 0.86; 95% CI: 0.77-0.95) compared to standalone use (AUC 0.73; 95% CI: 0.59-0.86) [35].
Anthropometric Alternatives for Resource-Limited Settings
In resource-constrained environments, anthropometric measures provide accessible alternatives for IR assessment. A 2025 Peruvian study evaluated various anthropometric indices, finding that the Fat Mass Index (FMI) exhibited the highest diagnostic accuracy for IR (AUC: 0.80 in women, 0.81 in men) with high sensitivity (>80%) and specificity (>70%) for both sexes [34]. Sex-specific FMI cut-offs were established at 11.70 kg/m² for women and 7.52 kg/m² for men [34].
Diagram 1: HOMA-IR and TyG Index Calculation Workflow (Title: IR Assessment Methodology)
Lipid Profiles: Beyond Conventional Cholesterol Metrics
Expanded Lipid Biomarkers in Cardiovascular Risk Stratification
Conventional lipid panels (TC, LDL-c, HDL-c, TG) provide foundational cardiovascular risk assessment, but emerging evidence supports the superior predictive value of composite metrics, particularly in diabetic dyslipidemia. Non-HDL-c (total cholesterol minus HDL-c) encompasses all atherogenic apolipoprotein B-containing lipoproteins, including LDL, VLDL, IDL, and remnant particles [36].
A 2025 Ghanaian cross-sectional study among T2D patients demonstrated that non-HDL-c significantly outperformed remnant cholesterol (RC) in predicting atherosclerotic cardiovascular disease (ASCVD) risk, with higher AUC (0.78 vs. 0.62), sensitivity, and specificity [36]. Non-HDL-c showed significant associations with elevated hs-CRP and resistin levels, while RC demonstrated weaker, non-significant associations [36].
Methodological Considerations for Lipid Biomarker Implementation
Table 3: Advanced Lipid Biomarkers in Metabolic Syndrome and T2D Research
| Biomarker | Calculation | Predictive Value | Advantages | Research Context |
|---|---|---|---|---|
| Non-HDL-c | Total Cholesterol - HDL-c | Superior to RC for ASCVD risk (AUC: 0.78) [36] | Comprehensive atherogenic burden assessment | Primary predictive biomarker in T2D cohorts |
| Remnant Cholesterol (RC) | Total Cholesterol - LDL-c - HDL-c | Moderate predictive value (AUC: 0.62) [36] | Captures triglyceride-rich lipoproteins | Secondary risk stratification |
| TG/HDL Ratio | Triglycerides / HDL-c | Strong association with IR [32] | Simple calculation, no additional costs | Insulin resistance assessment, epidemiological studies |
| LDL-c | Friedewald formula: Total Cholesterol - HDL-c - (Triglycerides/5) | Traditional primary target [36] | Established treatment target | Regulatory endpoints for lipid-lowering therapies |
The TyG index, while primarily an IR measure, also reflects atherogenic dyslipidemia and has demonstrated strong association with ASCVD risk in diabetic populations, particularly when combined with other biomarkers such as BMI [35].
Integrated Biomarker Applications in Clinical Research
Predictive Modeling and Machine Learning Approaches
Advanced computational approaches enhance the predictive utility of established biomarkers by integrating them with clinical and lifestyle parameters. A 2025 machine learning study developed an IR prediction model using 34 lifestyle-related questionnaire features and 17 biochemical markers from 16,411 nondiabetic individuals [33]. The LightGBM model demonstrated superior performance (AUC: 0.8456, accuracy: 0.7542, sensitivity: 0.6639, specificity: 0.7642) [33].
Top predictive features identified through Shapley Additive Explanations analysis included:
- BMI
- Fasting blood glucose
- HDL-cholesterol
- Triglycerides
- Creatinine
- Alanine aminotransferase
- Sex
- Total bilirubin
- Age
- Albumin/globulin ratio [33]
This model successfully stratified diabetes risk in validation cohorts, with high-risk individuals showing a 5.1-fold increased diabetes incidence (4.6% vs. 0.9%) over 5 years [33].
Biomarker Applications in Therapeutic Development and Response Prediction
Biomarkers play critical roles throughout the drug development pipeline, from target identification to post-marketing surveillance. HbA1c serves as a validated surrogate endpoint for glycemic efficacy, while HOMA-IR and specific lipid parameters provide mechanistic insights into drug effects on insulin sensitivity and cardiovascular risk [29].
In GLP-1 receptor agonist studies, baseline biomarkers predict therapeutic response. A 2025 52-week prospective study identified that responders to GLP-1RA therapy (≥5% weight loss) exhibited distinct baseline characteristics, including elevated BMI, waist circumference, hepatic steatosis indices, fat mass, and insulin levels, along with reduced muscle-to-fat and muscle-to-visceral adipose tissue ratios [37]. Additionally, female gender, younger age, shorter disease duration, and non-use of metformin prior to enrollment significantly associated with treatment response [37].
Diagram 2: Biomarker Integration in Metabolic Research (Title: Biomarker Integration Framework)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Analytical Platforms for Biomarker Quantification
| Category | Essential Items | Specifications/Examples | Research Application |
|---|---|---|---|
| Blood Collection & Processing | Serum separator tubes, EDTA tubes, Centrifuges | Standard venipuncture equipment | Pre-analytical sample processing |
| Glucose Metabolism | Hexokinase GLUC3 kit (Roche), HbA1c TINIA Gen. 3 kit | Enzymatic colorimetric methods | HbA1c and fasting glucose quantification |
| Insulin Measurement | Elecsys Insulin kits (ECLIA), C-peptide kits | Electrochemiluminescence immunoassays | HOMA-IR, HOMA2 calculations |
| Lipid Profiling | Enzymatic colorimetric kits for TG, HDL-c, LDL-c | Homogeneous enzymatic assays | Conventional and advanced lipid panels |
| Body Composition | DXA scanners, CT imaging, Bioimpedance analyzers | SECA anthropometric tools, Holtain calipers | Fat mass index, visceral fat assessment |
| Data Analysis | HOMA2 calculator, R statistical packages, Machine learning algorithms | Custom scripts for TyG, McAuley indices | Insulin resistance indices calculation |
Established clinical biomarkers—HbA1c, HOMA-IR, and lipid profiles—remain foundational tools in metabolic syndrome and T2D research, with evolving applications in predictive modeling, therapeutic development, and personalized medicine. The integration of these biochemical measures with emerging biomarkers from medical imaging, anthropometry, and molecular profiling enables multidimensional assessment of metabolic health. As regulatory science advances, these biomarkers continue to serve critical roles in drug development, from patient stratification to efficacy assessment, with proper validation and context-specific implementation remaining paramount for their meaningful application in both research and clinical practice.
The rising global prevalence of metabolic syndrome and type 2 diabetes mellitus (T2DM) necessitates advanced biomarkers for early detection, risk stratification, and monitoring of complications. Traditional biomarkers often lack specificity for capturing the underlying inflammatory and fibrotic processes that drive disease progression. This whitepaper provides an in-depth technical analysis of three emerging biomarkers—soluble urokinase plasminogen activator receptor (suPAR), Galectin-3, and Growth Differentiation Factor-15 (GDF-15)—within the context of metabolic disease research. We summarize current clinical evidence, detail standardized experimental protocols, visualize key signaling pathways, and catalog essential research tools to facilitate their investigation and validation in preclinical and clinical settings.
Biomarker Profiles and Clinical Significance
Soluble Urokinase Plasminogen Activator Receptor (suPAR)
suPAR, the soluble form of the membrane-bound urokinase plasminogen activator receptor, is a glycoprotein involved in inflammation, immune activation, and fibrinolysis. Elevated serum suPAR levels reflect chronic inflammatory states and have emerged as a significant predictor for the development and progression of metabolic diseases [38] [39].
Key Clinical Associations:
- Diabetes and Prediabetes Risk: Elevated baseline suPAR concentrations are independently associated with an increased risk of developing type 2 diabetes [39].
- Cardiovascular Disease in T2DM: suPAR levels are significantly higher in T2DM patients with cardiovascular disease (CVD) compared to those without CVD and healthy controls. One study reported levels of 2500.72 ± 12.36 ρg/mL in T2DM with CVD versus 2255.32 ± 10.15 ρg/mL in T2DM without CVD, and 229.00 ± 14.48 ρg/mL in healthy controls [38].
- Diabetic Nephropathy: suPAR predicts the development of microalbuminuria, an early sign of diabetic kidney disease. Subjects in the highest suPAR quartile had a 5.3-fold increased risk of new-onset microalbuminuria compared to the lowest quartile [39].
- Atherosclerosis and Thrombosis: suPAR is positively associated with increased carotid plaque thickness and enhanced ADP-induced platelet aggregation, linking it to macrovascular complications in both type 1 and type 2 diabetes [40].
Galectin-3
Galectin-3 is a β-galactoside-binding lectin widely expressed by immune cells, including macrophages. It plays a multifunctional role in inflammation, autoimmunity, apoptosis, and chemotaxis, and is implicated in tissue fibrosis and remodeling [41] [42].
Key Clinical Associations:
- Type 2 Diabetes: Circulating Galectin-3 levels are significantly elevated in T2DM patients compared to healthy controls and are positively correlated with fasting plasma glucose, HbA1c, and high-sensitivity C-reactive protein (hs-CRP) [41] [42].
- Cardiovascular Remodeling: Galectin-3 is strongly associated with structural-functional changes in the heart and vessels. It correlates with parameters of left ventricular hypertrophy and increased intima-media thickness of the common carotid artery in hypertensive and diabetic patients [42].
- Insulin Resistance: Galectin-3 induces cellular insulin resistance by directly interacting with the insulin receptor and impairing insulin signaling in adipose tissue, liver, and muscle [41].
- Risk Stratification: The ratio of Galectin-3 to adiponectin has been identified as a superior biomarker for assessing diabetes risk, especially in older populations (age ≥50 years) [43].
Growth Differentiation Factor-15 (GDF-15)
GDF-15 is a stress-responsive cytokine and divergent member of the transforming growth factor-β (TGF-β) superfamily. It is highly expressed in cardiomyocytes, adipocytes, and macrophages under pathological conditions and is recognized as a marker of metabolic stress and tissue injury [44] [45].
Key Clinical Associations:
- Obesity and Insulin Resistance: Serum GDF-15 levels are elevated in obese individuals and T2DM patients, correlating with BMI, body fat, glucose levels, and C-reactive protein [44].
- Diabetic Complications: Elevated GDF-15 is an independent predictor for peripheral artery disease (PAD) in diabetic patients. One study found a mean level of 2521.5 pg/mL in diabetic patients with PAD and associated high levels with an ABI < 0.9 [45]. It is also linked to diabetic nephropathy and retinopathy [44] [45].
- Protective Metabolic Effects: Despite its association with disease states, GDF-15 appears to play a protective role by decreasing food intake, reducing body weight and adiposity, and improving glucose tolerance in animal models [44].
Table 1: Summary of Key Clinical Associations for Novel Biomarkers in Metabolic Disease
| Biomarker | Primary Biological Role | Association with T2DM & Metabolic Syndrome | Key Diabetic Complications Linked |
|---|---|---|---|
| suPAR | Inflammation, immune activation, fibrinolysis | Predicts incident T2DM; elevated in T2DM patients [38] [39] | Cardiovascular disease [38], Nephropathy (microalbuminuria) [39], Atherosclerosis [40] |
| Galectin-3 | Inflammation, fibrosis, insulin resistance signaling | Elevated in T2DM; correlates with HbA1c and HOMA-IR [41] [42] | Cardiac remodeling [42], Macrovascular disease [41] |
| GDF-15 | Cellular stress response, metabolic regulation | Elevated in obesity and T2DM; correlates with insulin resistance [44] [45] | Peripheral artery disease [45], Nephropathy, Cardiovascular events [44] |
Table 2: Characteristic Circulating Levels in Health and Disease States
| Biomarker (Units) | Healthy/Normative Range | T2DM (No Complications) | T2DM (With Complications) | Key References |
|---|---|---|---|---|
| suPAR (pg/mL) | ~229 [38] | 2255.32 ± 10.15 [38] | 2500.72 ± 12.36 (with CVD) [38]; >3701 (Q4, with microalbuminuria) [39] | |
| Galectin-3 (μg/L) | Information missing | Information missing | Information missing | [41] [42] |
| GDF-15 (pg/mL) | 200 - 1200 [45] | Information missing | 2521.5 (mean, with PAD) [45] |
Pathophysiological Mechanisms and Signaling Pathways
suPAR in Podocyte Injury and Diabetic Nephropathy
A primary mechanism linking suPAR to diabetic nephropathy involves direct injury to podocytes. Elevated circulating suPAR binds to and activates β3-integrin on the surface of podocytes. This activation disrupts the actin cytoskeleton, leading to podocyte effacement and a loss of glomerular permselectivity, which results in albuminuria. In diabetic states, the expression of SMPDL3b is high, skewing suPAR-mediated injury toward a pro-apoptotic phenotype in podocytes, further exacerbating renal damage [39].
Figure 1: suPAR Signaling in Podocyte Injury. suPAR binding to β3-integrin on podocytes leads to cytoskeletal disruption and foot process effacement. In diabetes, high SMPDL3b expression shifts this injury toward apoptosis.
Galectin-3 in Insulin Resistance and Fibrosis
Galectin-3 contributes to metabolic dysfunction via two primary pathways. First, it promotes systemic insulin resistance; Galectin-3 secreted from macrophages can directly bind to the insulin receptor on target tissues (adipose, liver, muscle), impairing key steps in the insulin signaling pathway (e.g., IRS-1 phosphorylation) [41]. Second, it drives tissue fibrosis and cardiovascular remodeling. Galectin-3 is a potent activator of macrophages and fibroblasts, stimulating the deposition of collagen and other extracellular matrix proteins, which leads to myocardial fibrosis and arterial stiffening [41] [42].
Figure 2: Galectin-3 in Metabolic Dysfunction. Galectin-3 impairs insulin signaling, inducing resistance, and activates profibrotic pathways leading to cardiovascular remodeling (LVH: Left Ventricular Hypertrophy, IMT: Intima-Media Thickness).
GDF-15 as a Stress-Induced Metabolic Regulator
GDF-15 is broadly induced in response to cellular stress, inflammation, and tissue injury. Its expression is upregulated by transcription factors like p53 and EGR-1 in response to cytokines (IL-1β, TNF-α), anoxia, and metabolic stress [44]. While persistently high circulating levels are a robust marker of disease burden, GDF-15 appears to have protective metabolic functions. It acts centrally in the brainstem and area postrema to reduce appetite and body weight. Furthermore, it activates cytoprotective signaling pathways in tissues (e.g., PI3K/AKT and SMAD) to counterbalance stress and injury [44].
Figure 3: GDF-15 as a Stress-Responsive Cytokine. Cellular stressors induce GDF-15 expression, which functions as a biomarker of disease severity while also eliciting protective metabolic and cellular responses.
Experimental Protocols and Methodologies
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA is the standard method for quantifying suPAR, Galectin-3, and GDF-15 in serum or plasma.
Detailed Protocol for suPAR/GDF-15 Measurement [38] [45]:
- Coating: A microtiter plate is pre-coated with a capture antibody specific to the target analyte (e.g., suPAR, GDF-15).
- Sample Addition: Standards (of known concentration) and prediluted patient samples are added to the wells and incubated. Any target antigen present binds to the immobilized capture antibody.
- Washing: Wells are washed to remove unbound substances.
- Detection Antibody Addition: A biotin-conjugated detection antibody specific to the target is added and incubated, forming an antibody-antigen "sandwich."
- Washing: Another wash step removes unbound detection antibody.
- Enzyme Conjugate Addition: Avidin conjugated to Horseradish Peroxidase (HRP) is added and binds to the biotin on the detection antibody.
- Washing: A final wash removes unbound enzyme conjugate.
- Substrate Addition: A Tetramethylbenzidine (TMB) substrate solution is added. HRP catalyzes a color change in the substrate.
- Reaction Stop: The enzyme-substrate reaction is stopped by adding a sulfuric acid solution.
- Quantification: The optical density (color intensity) of each well is measured spectrophotometrically at 450 nm. The analyte concentration in unknown samples is determined by interpolation from the standard curve.
Table 3: Key Commercial ELISA Kits and Reagents
| Biomarker | Exemplary Kit (Supplier) | Sensitivity | Detection Range | Sample Type |
|---|---|---|---|---|
| suPAR | ELK2317 / 2318 [38] | 36 pg/mL | 78.13 - 5000 ρg/mL | Serum |
| Galectin-3 | Bender Med Systems [42] | Information missing | Information missing | Serum |
| GDF-15 | R&D Systems [45] | 2.2 pg/mL | Information missing | Plasma, Serum |
Assessment of Functional Correlates in Clinical Studies
To establish clinical relevance, biomarker levels are correlated with phenotypic and functional measures.
- Diabetic Nephropathy: Urinary Albumin-to-Creatinine Ratio (UACR) is measured in spot urine collections to define microalbuminuria (UACR 30-300 mg/g) [39] [40].
- Peripheral Artery Disease (PAD): The Ankle-Brachial Index (ABI) is measured using a VaSera VS-1500N or similar device. An ABI < 0.9 is diagnostic for PAD [45].
- Arterial Stiffness: The Cardio-Ankle Vascular Index (CAVI) is derived from pulse wave velocity and blood pressure measurements using the same device, providing an index of arterial stiffness independent of blood pressure [45].
- Cardiovascular Remodeling: Echocardiography is performed to determine Left Ventricular Mass Index (LVMI), and carotid ultrasound is used to measure Intima-Media Thickness (IMT) [42].
- Insulin Resistance: The Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) is calculated as: (Fasting Insulin (mcU/mL) × Fasting Glucose (mmol/L)) / 22.5 [42].
Table 4: Key Reagents and Tools for Biomarker Research
| Reagent / Tool | Specific Example | Research Application / Function |
|---|---|---|
| Quantitative ELISA Kits | Human suPAR ELISA (ELK2317) [38]; Human GDF-15 ELISA (R&D Systems) [45] | Gold-standard for precise quantification of biomarker levels in biological fluids. |
| Validated Antibodies | Anti-Galectin-3 (for Western Blot) [46]; Anti-uPAR (for ELISA capture/detection) [38] | Detection of biomarkers in immunoassays and immunohistochemistry. |
| Cell-Based Assays | Podocyte cell lines; Macrophage cell lines | In vitro modeling of suPAR-integrin signaling [39] or Galectin-3-induced insulin resistance [41]. |
| Animal Models | High-Fat Diet (HFD) induced obese mice [41] [46]; Genetic knockout models (e.g., Gal-3 KO) [41] | Investigation of biomarker function in disease pathogenesis and validation as therapeutic targets. |
| Pharmacological Inhibitors | TD139 (Galectin-3 inhibitor) [41] | Tool for probing the functional role of a specific biomarker in pathological processes. |
suPAR, Galectin-3, and GDF-15 represent a promising new class of biomarkers that provide critical insights into the inflammatory and fibrotic pathways underlying metabolic syndrome and type 2 diabetes. Their ability to predict the risk of developing diabetes and its devastating microvascular and macrovascular complications positions them as valuable tools for refining patient stratification in research and future clinical practice. Further large-scale prospective studies and the development of standardized assays are essential to fully translate these biomarkers from research tools into clinical assets that can guide personalized prevention and treatment strategies.
Metabolomics and lipidomics, comprehensive studies of small molecules and lipids in biological systems, have emerged as indispensable tools for decoding the complex pathophysiology of metabolic syndrome and type 2 diabetes mellitus (T2DM) [47] [48]. As the final downstream products of biological processes, metabolites provide a direct snapshot of physiological activity and disease-induced perturbations [49] [50]. The global burden of T2DM, projected to affect 783 million people by 2045, has intensified the search for novel biomarkers that can enable early detection, risk stratification, and personalized therapeutic interventions [47] [49]. Nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry (MS) have become the principal analytical platforms driving this research, each offering complementary capabilities for identifying and quantifying metabolic signatures associated with insulin resistance, β-cell dysfunction, and diabetic complications [51] [52].
This technical guide examines the foundational methodologies, experimental protocols, and applications of NMR and MS-based metabolite profiling, with specific focus on their utility in T2DM biomarker discovery. We present standardized workflows, comparative analytical specifications, and illustrative pathway diagrams to equip researchers with practical frameworks for implementing these technologies in metabolic disease research.
Core Analytical Technologies: NMR and MS
Nuclear Magnetic Resonance (NMR) Spectroscopy
NMR spectroscopy exploits the magnetic properties of atomic nuclei to identify and quantify metabolites in complex biological samples [47]. When placed in a strong magnetic field, nuclei with spin (such as ^1H, ^13C) absorb and re-emit electromagnetic radiation at frequencies characteristic of their molecular environment [53]. This phenomenon enables non-destructive analysis of biofluids and tissues with high reproducibility across laboratories [47].
Technical Specifications and Methodologies: Modern high-field NMR systems (e.g., 600-800 MHz) provide sufficient resolution to identify approximately 400 metabolites per spectrum [47] [51]. A typical 1D ^1H NMR experiment for serum metabolomics employs the Carr-Purcell-Meiboom-Gill (CPMG) pulse sequence to suppress macromolecule signals and enhance detection of low-molecular-weight metabolites [51]. For T2DM research, NMR has proven particularly valuable in quantifying energy metabolites (glucose, pyruvate, lactate), amino acids, and lipoprotein subclasses [51] [52].
Table 1: Key NMR Technical Parameters for Metabolite Profiling
| Parameter | Typical Specification | Application in T2DM Research |
|---|---|---|
| Magnetic Field Strength | 600-800 MHz | Higher fields (800 MHz) enhance resolution for complex biofluids [51] |
| Sample Volume | 100-500 μL | Suitable for precious clinical samples [47] |
| Temperature | 298K (25°C) | Standardized for reproducibility [51] |
| Spectral Width | 12-15 ppm | Covers entire metabolite chemical shift range [53] |
| Relaxation Delay | 1-5 seconds | Allows complete nuclear spin relaxation [51] |
| Scan Numbers | 64-256 scans | Balances signal-to-noise with acquisition time [51] |
Mass Spectrometry (MS) Platforms
Mass spectrometry measures the mass-to-charge ratio (m/z) of ionized metabolites, offering exceptional sensitivity and specificity for detecting compounds at trace concentrations [47] [49]. MS-based metabolomics typically couples separation techniques (liquid chromatography, gas chromatography) with mass analyzers to resolve complex biological mixtures [53].
Technical Specifications and Methodologies: Liquid chromatography-MS (LC-MS) dominates T2DM metabolomic studies due to its versatility in analyzing both polar and non-polar metabolites [49]. Reverse-phase C18 columns separate lipids and hydrophobic metabolites, while hydrophilic interaction liquid chromatography (HILIC) optimizes separation of polar compounds like amino acids and organic acids [50]. Gas chromatography-MS (GC-MS) provides superior resolution for volatile compounds and fatty acids after derivatization [53].
Table 2: Mass Spectrometry Platforms for Metabolite Profiling
| Platform | Mass Analyzer | Mass Accuracy | Metabolite Coverage | T2DM Application |
|---|---|---|---|---|
| LC-QTOF | Quadrupole Time-of-Flight | <5 ppm | 1000-2000 metabolites | Untargeted discovery of novel biomarkers [49] |
| GC-QQQ | Triple Quadrupole | <0.1 Da (unit mass) | 200-500 metabolites | Targeted analysis of fatty acids, organic acids [53] |
| Orbitrap | Orbitrap | <3 ppm | 1000-3000 metabolites | High-resolution lipidomics [49] |
| LC-QQQ | Triple Quadrupole | <0.1 Da (unit mass) | 50-200 metabolites | Quantitative validation of candidate biomarkers [50] |
Experimental Workflows and Protocols
Sample Preparation Protocols
Blood Serum/Plasma Collection for T2DM Studies: For NMR analysis, sample preparation is minimal: 300 μL serum is mixed with 200 μL deuterated phosphate buffer (pH 7.4) containing 0.9% NaCl and 0.1% sodium azide [51]. The mixture is centrifuged at 13,000 × g for 10 minutes to remove precipitates before transfer to 5mm NMR tubes [51]. For MS-based analyses, protein precipitation is critical: 100 μL serum is mixed with 300 μL cold methanol or acetonitrile, vortexed vigorously, and centrifuged at 14,000 × g for 15 minutes [50]. The supernatant is transferred to MS vials for analysis. For GC-MS, additional derivatization with methoxyamine hydrochloride and N-methyl-N-(trimethylsilyl)trifluoroacetamide (MSTFA) is required to increase metabolite volatility [53].
Quality Control Measures: In T2DM cohort studies, quality control samples are essential. These are typically prepared by pooling small aliquots from all samples to create a representative reference [52]. For NMR, deuterated trimethylsilylpropanoic acid (TSP) serves as internal standard for chemical shift referencing and quantification [51]. For MS, stable isotope-labeled internal standards (e.g., ^13C-glucose, d₃-leucine) are added to correct for ionization efficiency variations [50].
Data Acquisition Parameters
NMR Spectroscopy Protocol: A standard 1D NOESY-presat pulse sequence effectively suppresses the water signal in serum samples [51]. Key parameters include: 98 kHz spectral width, 3.9 sec acquisition time, 4 sec relaxation delay, 90° pulse angle, and 64-128 transients [51]. For quantitative analysis, the CPMG spin-echo sequence with 80 ms total echo time attenuates broad signals from proteins and lipoproteins [52].
LC-MS Metabolomics Protocol: For broad metabolite coverage in T2DM studies, a dual-platform approach is recommended. For hydrophilic metabolites: HILIC separation with acetonitrile/water gradient containing 10 mM ammonium acetate, coupled to QTOF-MS in both positive and negative electrospray ionization modes [49]. For lipids: reverse-phase C18 column with methanol/water/isopropanol gradient containing 5 mM ammonium acetate [50]. Source parameters typically include: 3.5 kV capillary voltage, 300°C source temperature, 800 L/hr desolvation gas flow [50].
Metabolic Pathways in Type 2 Diabetes
Metabolomic studies have elucidated several key pathways disrupted in T2DM pathogenesis. The following diagram illustrates the core metabolic network and associated biomarkers identified through NMR and MS profiling:
Diagram 1: Metabolic Pathways in T2DM. This network shows key metabolic disturbances in Type 2 Diabetes and the associated biomarkers detectable by NMR and MS platforms.
The pathway illustrates how metabolomics has identified several key metabolic disturbances in T2DM, including branched-chain amino acid (BCAA) metabolism, glutamine-glutamate balance, and lipoprotein subfraction alterations [51] [52]. Elevated BCAAs (isoleucine, leucine, valine) impair insulin signaling through mTOR activation, while an increased glutamine-to-glutamate ratio (QER) reflects mitochondrial dysfunction and oxidative stress [51] [50]. Lipoprotein abnormalities, particularly elevated VLDL triglycerides and reduced HDL cholesterol, are hallmarks of diabetic dyslipidemia [52].
Experimental Workflow for T2DM Biomarker Discovery
The following diagram outlines a standardized workflow for metabolomic biomarker discovery in type 2 diabetes research:
Diagram 2: T2DM Biomarker Discovery Workflow. This flowchart outlines the standardized experimental and computational workflow for identifying and validating metabolic biomarkers in Type 2 Diabetes research.
Key Biomarker Findings in T2DM Research
Metabolomic studies have consistently identified specific metabolite patterns associated with T2DM risk, progression, and complications. The table below summarizes well-validated biomarkers identified through NMR and MS platforms:
Table 3: Validated Metabolomic Biomarkers in Type 2 Diabetes
| Metabolite Class | Specific Biomarkers | Direction in T2DM | Analytical Platform | Pathophysiological Significance |
|---|---|---|---|---|
| Amino Acids | Branched-chain amino acids (leucine, isoleucine, valine) | Increased [52] [50] | NMR, LC-MS | Impaired catabolism; mTOR-mediated insulin resistance [52] |
| Glutamine | Decreased [51] | NMR, LC-MS | Mitochondrial dysfunction; oxidative stress [51] | |
| Glutamate | Increased [51] | NMR, LC-MS | TCA cycle impairment; gluconeogenic precursor [51] | |
| Phenylalanine/Tyrosine ratio | Increased [51] | NMR | Inflammation; catecholamine pathway disruption [51] | |
| Lipids/Lipoproteins | VLDL triglycerides | Increased [52] | NMR | Insulin resistance; diabetic dyslipidemia [52] |
| HDL cholesterol | Decreased [52] | NMR | Impaired reverse cholesterol transport [52] | |
| Docosahexaenoic acid | Decreased [52] | NMR | Altered membrane fluidity; inflammation [52] | |
| Carbohydrates | Glucose | Increased [51] | NMR, LC-MS | Hyperglycemia; insulin resistance [51] |
| Mannose | Increased [51] | NMR | Glycation; hexosamine pathway activation [51] | |
| Metabolic Ratios | Glutamine-to-Glutamate (QER) | Decreased [51] | NMR | Mitochondrial dysfunction marker [51] |
| Alanine-to-Glucose (AGR) | Decreased [51] | NMR | Disrupted glucose-alanine cycling [51] |
Research Reagent Solutions for Metabolomics
Table 4: Essential Research Reagents for Metabolomic Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Internal Standards | Deuterated TSP (trimethylsilylpropanoic acid) | NMR chemical shift reference and quantification [51] |
| Stable isotope-labeled metabolites (^13C-glucose, d₃-leucine) | MS quantification normalization; quality control [50] | |
| Sample Preparation | Deuterated solvents (D₂O, CD₃OD) | NMR solvent; signal locking [51] |
| Protein precipitation solvents (methanol, acetonitrile) | MS sample preparation; protein removal [53] | |
| Derivatization reagents (MSTFA, methoxyamine) | GC-MS; increases metabolite volatility [53] | |
| Separation | LC columns (C18, HILIC) | Metabolite separation prior to MS analysis [49] |
| GC columns (DB-5MS) | Volatile metabolite separation [53] | |
| Software Solutions | CHENOMX NMR Suite | NMR metabolite identification and quantification [51] |
| MetaboAnalyst | Statistical analysis and pathway mapping [51] | |
| XCMS Online | MS data processing and visualization [53] |
NMR and MS technologies provide complementary analytical capabilities for comprehensive metabolite profiling in T2DM research. NMR offers high reproducibility and quantitative accuracy for abundant metabolites, while MS delivers superior sensitivity for detecting low-concentration biomarkers [47] [49]. The integration of both platforms, coupled with standardized experimental workflows and appropriate reagent systems, enables robust identification of metabolic signatures underlying diabetes pathogenesis. As metabolomics continues to evolve, emerging technologies like spatial metabolomics and single-cell approaches promise to further refine our understanding of metabolic heterogeneity in T2DM, ultimately advancing personalized medicine approaches for this complex metabolic disorder [49].
MicroRNAs (miRNAs) have emerged as pivotal regulators of gene expression and promising biomarkers in metabolic syndrome and type 2 diabetes (T2DM). This whitepaper provides a technical examination of miR-126 and miR-423-5p, focusing on their roles in glucose homeostasis, vascular complications, and utility in molecular phenotyping. We synthesize current evidence from clinical and experimental studies, detailing their mechanistic involvement in critical pathways such as AGE-RAGE signaling, and provide standardized protocols for their quantification in circulation. The exceptional stability of circulating miRNAs and their disease-specific expression profiles position them as transformative tools for early diagnosis, prognostic stratification, and personalized therapeutic interventions in cardiometabolic disorders.
MicroRNAs are small (~22 nucleotides) non-coding RNA molecules that fine-tune gene expression post-transcriptionally by binding to complementary sequences on target messenger RNAs (mRNAs), leading to translational repression or mRNA degradation [54] [55]. Their exceptional stability in extracellular fluids like plasma and serum—attributed to packaging within extracellular vesicles (exosomes, microparticles, apoptotic bodies) or complex formation with RNA-binding proteins such as Argonaute2—makes them ideal candidates for non-invasive liquid biopsies [56] [54] [55]. Furthermore, miRNAs exhibit strong tissue specificity (e.g., miR-126 for endothelial cells) and are released into circulation rapidly following cellular stress or injury, often preceding changes in conventional biomarkers [55]. These properties allow them to reflect dynamic pathological processes underlying complex diseases like T2DM and its complications [57] [55].
Functional Roles in Metabolism and Vascular Biology
miR-126: A Guardian of Vascular Homeostasis
miR-126 is an endothelial-enriched miRNA intrinsically linked to vascular integrity and function. Its gene is located within the seventh intron of the epidermal growth factor-like protein 7 (EGFL7) gene on chromosome 9 [58]. It is processed into two functional strands: miR-126-3p (the guide strand) and miR-126-5p (the passenger strand) [58].
- Key Mechanisms and Pathways: miR-126 plays a critical role in maintaining endothelial function by modulating key signaling pathways. It positively regulates the VEGF and fibroblast growth factor signaling pathways by repressing negative regulators such as SPRED1 and PIK3R2 [58] [54]. This action promotes angiogenesis and endothelial cell proliferation, migration, and repair. In the context of diabetic complications, miR-126 is significantly implicated in the AGE-RAGE signaling pathway, a major driver of hyperglycemia-induced vascular damage. Dysregulation of miR-126 is associated with impaired angiogenesis, endothelial dysfunction, and the accelerated progression of microvascular complications [58].
- Pathophysiological Significance: In T2DM, miR-126 expression is frequently dysregulated. Its downregulation in endothelial cells contributes to vascular complications, while its presence in circulation serves as a potential biomarker of endothelial injury. Notably, miR-126 was the most abundant miRNA identified in endothelial cell-derived apoptotic bodies and was shown to mediate atheroprotective effects by inducing CXCL12-dependent vascular protection [54]. In diabetic kidney disease (DKD), higher serum levels of hsa-miR-126-3p were specifically associated with the albuminuric phenotype (F1), highlighting its role in phenotyping DKD [59].
miR-423-5p: An Emerging Player in Metabolic Regulation
While initially studied in oncology, miR-423-5p has gained attention for its role in cardiometabolic diseases. Its expression and function appear to be highly context-dependent.
- Key Mechanisms and Pathways: The specific molecular targets of miR-423-5p in diabetes are under investigation, but it is known to influence processes like cell proliferation, invasion, and apoptosis [60]. In a clinical study on DKD, hsa-miR-423-5p was identified as an independent predictor of estimated glomerular filtration rate (eGFR), with a direct effect on kidney function [59].
- Pathophysiological Significance: Circulating levels of miR-423-5p are elevated in patients with T2DM [57]. In DKD, its expression pattern differs from miR-126-3p; it is elevated in patients with the non-albuminuric, reduced filtration phenotype (F3), suggesting its potential as a biomarker for predicting kidney function decline and distinguishing between DKD phenotypes [59].
Quantitative Evidence and Clinical Associations
The following tables summarize key quantitative findings from clinical studies on miR-126 and miR-423-5p in diabetes and related complications.
Table 1: Clinical Associations of miR-126 and miR-423-5p in Type 2 Diabetes and Complications
| miRNA | Regulation in T2DM | Associated Clinical Parameters | Potential Diagnostic/Role | Key References |
|---|---|---|---|---|
| miR-126 | Upregulated in plasma/serum [58] [57] | - Endothelial dysfunction- Albuminuric DKD phenotype (F1) [59]- Microvascular complications [59] | - Early detection of T2DM [57]- DKD phenotyping [59]- Biomarker of vascular health [58] | [58] [59] [57] |
| miR-423-5p | Upregulated in plasma [60] [57] | - Independent predictor of eGFR (β=0.138) [59]- Non-albuminuric, reduced filtration DKD phenotype (F3) [59] | - Predicting kidney function [59]- DKD phenotyping [59] | [59] [60] [57] |
Table 2: Key Signaling Pathways and Target Genes in Diabetic Complications
| Pathway/Process | Key Components | miRNA Involved | Functional Outcome |
|---|---|---|---|
| AGE-RAGE Signaling | AKT1, BCL2, MAPK1, TP53, SIRT1 [58] | miR-126 [58] | Oxidative stress, inflammation, vascular dysfunction |
| VEGF Signaling | VEGF, SPRED1, PIK3R2 [58] [54] | miR-126 [58] [54] | Angiogenesis, endothelial cell function |
| Diabetic Kidney Disease Phenotyping | eGFR, UACR, ACE, AIP [59] | miR-126-3p, miR-423-5p [59] | Prediction of renal function and stratification of DKD subtypes |
Experimental Protocols for Circulating miRNA Analysis
A standardized workflow for quantifying circulating miR-126 and miR-423-5p is crucial for reproducible research.
Sample Collection and Preparation
- Sample Type: Plasma (preferred for its lower background miRNA) or serum can be used [60] [56].
- Collection: Collect peripheral blood into EDTA or citrate tubes.
- Processing: Centrifuge at 4°C to separate plasma/serum from cells within 2 hours of collection. Perform a second, high-speed centrifugation (e.g., 13,000 × g for 10 min) to obtain platelet-poor plasma and remove residual cells and debris [60].
- Storage: Aliquot and store at -80°C. Avoid repeated freeze-thaw cycles (>2-3).
RNA Extraction and Quality Control
- Extraction Kit: Use commercial kits specifically designed for low-abundance RNA from biofluids (e.g., miRNeasy Serum/Plasma Advanced Kit, Qiagen) [60].
- Spike-in Controls: Include synthetic non-human miRNA spikes (e.g., cel-miR-39-3p) during the lysis step to monitor extraction efficiency and normalize for technical variability [60].
Reverse Transcription and Quantitative PCR (qPCR)
- cDNA Synthesis: Use stem-loop reverse transcription primers (e.g., miRCURY LNA RT Kit), which enhance specificity and sensitivity for mature miRNAs [60].
- qPCR Amplification:
- Platform: Standard real-time PCR systems.
- Chemistry: SYBR Green-based detection with LNA (Locked Nucleic Acid)-enhanced PCR primers. LNA technology significantly improves the hybridization affinity and specificity for short miRNA targets [60].
- Normalization: Use a combination of strategies for robust normalization:
- Replication: Perform all reactions in duplicate or triplicate. The relative expression level is calculated using the comparative Cq method (2^(-ΔΔCq)) [60].
Diagram Title: Workflow for Circulating miRNA Analysis
Research Reagent Solutions Toolkit
Table 3: Essential Reagents and Kits for miRNA Biomarker Research
| Product Category | Specific Example | Critical Function | Technical Notes |
|---|---|---|---|
| RNA Extraction Kit | miRNeasy Serum/Plasma Advanced Kit (Qiagen) | Isols total RNA, including small RNAs, from biofluids; minimizes contaminants that inhibit downstream reactions. | Includes carrier RNA to maximize low-concentration RNA yield. |
| Spike-in Control | miRCURY LNA RNA Spike-in Kit (Qiagen) | Synthetic miRNAs (e.g., cel-miR-39-3p) added at lysis to control for variation in RNA extraction and reverse transcription efficiency. | Essential for normalizing pre-analytical and analytical variability. |
| cDNA Synthesis Kit | miRCURY LNA RT Kit (Qiagen) | Uses stem-loop primers for highly specific reverse transcription of mature miRNAs. | Superior to poly-A tailing methods for specificity and sensitivity. |
| qPCR Assay | miRCURY LNA miRNA PCR Assay (Qiagen) | LNA-enhanced SYBR Green assays for highly specific and sensitive detection of mature miRNAs like miR-126-3p and miR-423-5p. | LNA technology provides high specificity necessary to distinguish between miRNA family members. |
| Normalization Reference | hsa-miR-16-5p PCR Assay | An endogenous control miRNA that is stably expressed in plasma/serum across many disease states, including diabetes [60]. | Stability should be validated for each specific study cohort and sample type. |
Signaling Pathways in Diabetic Complications
The following diagram illustrates the central role of the AGE-RAGE pathway in diabetic complications and the points of regulation by miR-126.
Diagram Title: miR-126 in the AGE-RAGE Pathway
miR-126 and miR-423-5p represent a new class of regulatory biomarkers with significant potential to advance research and clinical management of T2DM and metabolic syndrome. Their integration into molecular phenotyping strategies, especially for heterogeneous complications like DKD, promises to enable earlier diagnosis, more accurate prognosis, and the development of personalized nephroprotective and vasoprotective strategies. Future efforts must focus on standardizing analytical protocols, validating miRNA signatures in large, diverse cohorts, and exploring their therapeutic potential through targeted modulation.
Biomarkers have transitioned from ancillary diagnostic tools to central pillars in the modern management of complex metabolic diseases. Within the context of metabolic syndrome and type 2 diabetes mellitus (T2DM) research, these measurable indicators provide critical insights into disease pathophysiology, enabling a shift from reactive treatment to proactive, personalized medicine. Metabolic syndrome—a cluster of conditions including abdominal obesity, dyslipidemia, hypertension, and insulin resistance—significantly elevates the risk of developing T2DM and cardiovascular diseases [61]. The escalating global prevalence of these conditions, with T2DM alone affecting approximately 537 million adults, underscores the urgent need for refined diagnostic and prognostic strategies [62]. Biomarkers serve multifaceted roles as diagnostic tools for early disease detection, prognostic instruments for risk stratification, and monitoring aids for tracking therapeutic response and disease progression. This technical guide examines the current landscape of biomarker applications, focusing on their pivotal role in advancing research and drug development for metabolic syndrome and T2DM, with particular emphasis on emerging molecular classes and the technologies enabling their discovery and validation.
Biomarkers for Early Detection and Diagnosis
The early detection of metabolic dysregulation, prior to the manifestation of overt disease, is paramount for implementing preventive interventions that can delay or avert the onset of T2DM and its complications. Traditional biomarkers have long formed the foundation of clinical assessment, but recent advances have unveiled novel markers with enhanced sensitivity and specificity.
Established Biochemical Biomarkers
Core metabolic biomarkers provide a snapshot of systemic physiological status and are routinely used in clinical practice. HbA1c reflects average blood glucose levels over the preceding two to three months and is instrumental in diagnosing and monitoring T2DM, though its accuracy can be compromised in individuals with hemoglobin variants or renal disease [15]. The Homeostasis Model Assessment of Insulin Resistance (HOMA-IR), derived from fasting glucose and insulin levels, is a prominent tool for assessing insulin resistance, with thresholds typically set at 2.5 for adult Caucasian populations [63]. Fasting insulin levels, secreted by pancreatic beta cells, are elevated in the early stages of insulin resistance and T2DM but decline with progressive beta-cell failure [63]. Dyslipidemia, a key component of metabolic syndrome, is assessed through markers such as triglycerides (TG) and high-density lipoprotein cholesterol (HDL-C), with the TG-to-HDL ratio serving as a powerful predictor of insulin resistance and T2DM risk [64]. Furthermore, 24-hour urinary microalbumin excretion has emerged as a practical biomarker for early risk assessment, with studies demonstrating that elevated levels are independently associated with metabolic syndrome and its components, including central obesity and elevated fasting blood glucose [61].
Novel Circulating and Molecular Biomarkers
Beyond traditional metrics, research has identified a new generation of biomarkers that offer deeper insights into the underlying pathophysiological processes.
Inflammatory Markers: Chronic low-grade inflammation is a hallmark of obesity and metabolic syndrome. Markers such as C-reactive protein (CRP), Interleukin-6 (IL-6), and Tumor Necrosis Factor-alpha (TNF-α) are significantly elevated in these conditions. CRP, synthesized by hepatocytes, is a marker of systemic inflammation and cardiovascular risk, while IL-6 and TNF-α, released from adipose tissue and macrophages, contribute directly to hepatic inflammation, fibrosis, and systemic insulin resistance [63] [15].
Adipokines: Adipose tissue functions as an endocrine organ, secreting signaling proteins that regulate metabolism and inflammation. Leptin and adiponectin are closely linked to obesity and T2DM development. Growth Differentiation Factor 15 (GDF-15), a member of the TGF-β superfamily, is upregulated under cellular stress and is independently associated with age, male gender, obesity, and diabetic traits, supporting its potential role as a biomarker for metabolic disorders [15].
MicroRNAs (miRNAs): These small non-coding RNAs regulate gene expression post-transcriptionally and are stable in circulation. Specific serum miRNAs, such as miR-484, are being investigated for their relationship with glucose metabolism and insulin resistance, offering potential for early disease detection [15] [62].
Table 1: Core Biomarkers for Early Detection and Diagnosis of Metabolic Syndrome and T2DM
| Biomarker | Physiological Role | Normal Level | Level in Disease | Strengths | Limitations |
|---|---|---|---|---|---|
| HbA1c [63] [15] | Long-term glycemic control | <5.7% | >6.5% (T2DM) | Reflects 2-3 month average glucose | Affected by hemoglobin variants, renal disease |
| HOMA-IR [63] | Assessment of insulin resistance | <2.5 | Elevated (>2.9) | Simple, calculated from fasting sample | Lacks universal cut-off; age-dependent |
| Fasting Insulin [63] | Pancreatic beta-cell function | 2–25 µIU/mL | Elevated in early disease | Direct measure of insulin secretion | Utility reduced in insulin-treated patients |
| TG-to-HDL Ratio [64] | Lipid metabolism/insulin resistance | Varies | Elevated | Strong predictor of T2DM risk | Indirect measure of insulin resistance |
| Urinary Microalbumin [61] | Kidney integrity / endothelial function | <30 mg/24h | 30-300 mg/24h (Microalbuminuria) | Non-invasive; independent MetS association | Requires 24-hour collection for accuracy |
| CRP [63] | Systemic inflammation | <1 mg/L | >3 mg/L (High Risk) | Standardized, widely available assay | Low specificity; population variability |
| GDF-15 [15] | Cellular stress response | Varies | Elevated | Associated with obesity, insulin resistance | Levels vary with age, gender, ethnicity |
Biomarkers for Risk Stratification and Prognosis
Accurately stratifying patient risk is essential for allocating resources and personalizing treatment intensity. Biomarker panels and novel molecular signatures have demonstrated superior prognostic capability compared to single markers.
Multi-Marker Risk Scores
Combining multiple biomarkers into a single composite score can capture the multifaceted nature of metabolic syndrome and T2DM, thereby improving risk prediction. A nested case-control study within the Singapore Chinese Health Cohort created a weighted biomarker score comprising four biomarkers: the TG-to-HDL ratio, alanine transaminase (ALT), ferritin, and adiponectin. This score was strongly associated with T2DM risk; individuals in the highest quartile had an odds ratio of 12.0 compared to those in the lowest quartile. Adding this biomarker score to a base model that included established risk factors like BMI, hypertension history, and random glucose levels significantly improved the predictive area under the curve (AUC) from 0.81 to 0.83 [64]. This demonstrates the value of multi-marker approaches in refining risk stratification.
Novel Proteins and Genes
Targeted discovery efforts have identified specific proteins and genes with high prognostic value for disease progression. Research into type 2 diabetes mellitus with metabolic-associated fatty liver disease (MAFLD) identified TNFRSF1A and SERPINB2 as key diagnostic biomarkers. These genes were found to be significantly upregulated in patient blood and high-fat, high-glucose cellular models, enabling the construction of highly accurate diagnostic models for the co-morbid condition [65]. Furthermore, a multi-omics analysis of MAFLD progression identified five glycolysis-related key genes (ALDH3A1, CDK1, DEPDC1, HKDC1, and SOX9) that act as discriminators for MAFLD and are intricately involved in the hepatocyte–fibroblast–macrophage axis, a predominant glycolysis-active niche. These genes were validated through external cohorts and in vivo experiments, confirming their upregulation in MAFLD samples and their association with immune infiltration [15].
Table 2: Key Biomarkers for Risk Stratification and Prognosis
| Biomarker / Score | Biomarker Class | Associated Risk / Prognosis | Study / Validation Context |
|---|---|---|---|
| Multi-Marker Score (TG/HDL, ALT, Ferritin, Adiponectin) [64] | Composite Biochemical Score | 12x higher T2DM risk (highest vs. lowest quartile) | Prospective nested case-control study |
| TNFRSF1A & SERPINB2 [65] | Secreted Proteins / Receptors | Diagnosis of T2DM with MAFLD | Bioinformatics analysis and experimental validation in patient blood and cell models |
| Glycolysis Gene Panel (ALDH3A1, CDK1, DEPDC1, HKDC1, SOX9) [15] | Gene Expression | MAFLD progression and immune infiltration | Integrative multi-omics analysis (bulk & single-cell RNA-seq) and in vivo validation |
| Urinary Microalbumin (Quartiles) [61] | Renal / Metabolic Marker | Dose-dependent increase in MetS and elevated FBG risk | Cross-sectional study (1,175 participants); Q4 vs Q1 OR for MetS: 2.75 |
| GDF-15 [15] | Adipokine / Cytokine | Associated with obesity, insulin resistance, and diabetic traits | Population study (2,083 participants); correlates with age, gender, ethnicity |
Biomarkers for Complication Prediction
Prolonged hyperglycemia and metabolic dysfunction lead to debilitating microvascular and macrovascular complications. Predicting which patients are at highest risk is a critical application of biomarkers.
Microvascular Complications
Diabetic microvascular complications—including retinopathy, nephropathy, and neuropathy—are primary causes of blindness, terminal renal failure, and neuropathic disorders [66]. Serum biomarkers are emerging as valuable tools for the early assessment of these conditions. Promising biomarkers are associated with various pathophysiological pathways, such as glycation, oxidative stress, inflammation, endothelial dysfunction, basement membrane thickening, angiogenesis, and thrombosis [66]. Furthermore, non-coding RNAs like microRNAs and long non-coding RNAs have shown significant potential as predictive biomarkers for these complications, offering insights into novel regulatory mechanisms [66] [62].
Hepatic Complication (MAFLD/MASH)
The strong association between T2DM, obesity, and metabolic dysfunction-associated steatohepatitis (MASH) necessitates an integrative management approach. Biomarkers such as ALT and aspartate aminotransferase (AST) are conventional markers of hepatocyte damage. However, their correlation with disease severity is often poor [63]. As previously discussed, glycolysis-related genes and proteins like SERPINB2 and TNFRSF1A offer a more nuanced view of the metabolic derangements and immune interactions driving MAFLD progression, providing prognostic information beyond simple liver enzyme elevations [65] [15].
Experimental Protocols and Methodologies
Robust experimental design is fundamental to biomarker discovery and validation. The following protocols detail key methodologies cited in this field.
Bioinformatics-Driven Biomarker Discovery
This protocol outlines the integrative multi-omics approach used to identify glycolysis-associated key genes in MAFLD [65] [15].
- Data Acquisition: Obtain bulk RNA-seq, single-cell RNA-seq, and spatial transcriptomic datasets from public repositories (e.g., Gene Expression Omnibus) for both disease (MAFLD/T2DM) and control cohorts.
- Differential Expression Analysis: Process raw sequencing data through a standardized pipeline (quality control with FastQC, alignment with STAR, gene counting with featureCounts). Perform differential expression analysis using tools like DESeq2 or limma to identify significantly dysregulated genes.
- Weighted Gene Co-expression Network Analysis (WGCNA): Construct a gene co-expression network to identify modules of highly correlated genes. Correlate module eigengenes with clinical traits of interest (e.g., fibrosis score, insulin resistance) to pinpoint trait-relevant modules.
- Protein-Protein Interaction (PPI) Network Analysis: Input candidate genes from differential expression and WGCNA into STRING database to construct a PPI network. Identify densely connected regions (modules) within the network using algorithms like MCODE.
- Immune Infiltration Analysis: Utilize computational tools like CIBERSORT to deconvolute bulk RNA-seq data and estimate the abundance of specific immune cell types in the tissue. Correlate biomarker expression with immune cell infiltration levels.
- Machine Learning for Feature Selection: Apply multiple machine learning algorithms (e.g., Random Forest, Support Vector Machine, LASSO regression) on the candidate gene list to identify a minimal set of feature genes with the highest diagnostic or prognostic power.
- In vivo/In vitro Validation: Validate the expression of identified hub genes in independent patient cohorts, animal models (e.g., methionine-choline deficient diet murine models), or cell cultures (e.g., high-fat, high-glucose treated hepatocytes) using qPCR, immunohistochemistry, or Western blot.
Development and Validation of a Multi-Marker Biomarker Score
This protocol describes the steps for creating a composite biomarker score for T2DM risk prediction, as employed in prospective cohort studies [64].
- Cohort Selection and Design: Establish a nested case-control study within a large, prospective cohort. Collect biospecimens at baseline from participants free of the disease of interest.
- Laboratory Measurements: Analyze plasma/serum samples for a predefined panel of candidate biomarkers using standardized, validated assays (e.g., colorimetric methods for lipids/enzymes, ELISA for adipokines/cytokines).
- Statistical Association Analysis: Use conditional logistic regression models to compute the odds ratio for each biomarker (analyzed in quartiles) in association with T2DM risk. Adjust models for confounders (e.g., age, sex, BMI, smoking, hypertension).
- Biomarker Selection: Select only those biomarkers that show a statistically significant and independent association with disease risk for inclusion in the final score.
- Score Calculation: Derive a weighted biomarker score using the formula:
Score = k × (β1 × biomarker1 + β2 × biomarker2 + ... + βn × biomarker_n), where β represents the regression coefficient from the association analysis for each biomarker, and k is a constant. - Predictive Performance Assessment: Evaluate the predictive utility of the biomarker score by calculating the Area Under the Receiver Operating Characteristics Curve (AUC). Compare the AUC of a base model (traditional risk factors) with the AUC of the base model plus the biomarker score to determine incremental predictive value.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Kits for Biomarker Investigation
| Research Reagent / Kit | Primary Function | Key Applications |
|---|---|---|
| ELISA Kits (e.g., for Ferritin, Adiponectin, Fetuin-A, GDF-15) [64] [15] | Quantification of specific protein biomarkers in serum/plasma | Validation of protein expression levels; measuring circulating biomarker concentrations. |
| Colorimetric/Fluorometric Assay Kits (e.g., for ALT, AST, TG, HDL-C) [64] | Enzymatic or chemical-based measurement of metabolic biomarkers | Assessment of liver function and lipid profile in clinical and research samples. |
| RNA-Seq Library Prep Kits | Preparation of sequencing libraries from total RNA | Whole transcriptome analysis for discovery of differentially expressed genes and pathways. |
| Single-Cell RNA-Seq Solutions (e.g., 10x Genomics) | Profiling gene expression at single-cell resolution | Deconvoluting cellular heterogeneity and identifying cell-type specific biomarker expression [15]. |
| qPCR Reagents & Probes | Quantitative measurement of gene expression | Validation of RNA-seq results; high-throughput screening of candidate gene biomarkers. |
| CIBERSORT or Similar Computational Tool [65] [15] | In silico deconvolution of bulk tissue gene expression data | Estimating immune cell infiltration and correlating biomarker levels with immune context. |
| STRING Database | Construction and analysis of Protein-Protein Interaction (PPI) networks | Identifying functional modules and hub genes from candidate biomarker lists [65]. |
Visualizing Workflows and Pathways
Biomarker Discovery & Validation
Multi-Omics Integration
Pathophysiology & Biomarker Classes
Overcoming Clinical Translation Hurdles and Biomarker Limitations
Addressing Specificity and Sensitivity Challenges in Multi-Morbid Conditions
The investigation of biomarkers for metabolic diseases is fundamentally complicated by the high prevalence of multimorbidity—the coexistence of multiple chronic conditions within an individual. Research involving over 500,000 participants reveals that type 2 diabetes (T2D) acts as a critical accelerator of chronic disease accumulation, with individuals experiencing a 60% higher risk of a new disease diagnosis compared to those without T2D [67]. This acceleration is particularly pronounced in middle-aged adults (40-55 years), underscoring the dynamic role of T2D in multimorbidity progression [67]. This epidemiological reality creates substantial challenges for biomarker development, as traditional biomarkers often demonstrate inadequate performance when applied to complex, multi-morbid populations. The clinical reality is that researchers and clinicians are increasingly faced with patient populations characterized by interconnected metabolic conditions including T2D, obesity, metabolic dysfunction-associated steatohepatitis (MASH), and cardiovascular disease, necessitating a fundamental reevaluation of biomarker validation approaches [68] [63].
Core Challenges for Biomarkers in Multi-Morbid Populations
Specificity Limitations in Interconnected Conditions
The pathophysiological overlap between metabolic diseases creates significant specificity challenges for established biomarkers. For instance, insulin resistance represents a shared mechanism across T2D, obesity, and MASH, meaning biomarkers of insulin resistance like HOMA-IR and fasting insulin lack disease-specificity [63]. Similarly, inflammatory biomarkers such as C-reactive protein (CRP), Interleukin-6 (IL-6), and Tumor Necrosis Factor-alpha (TNF-α) are elevated across the spectrum of metabolic conditions due to the underlying chronic inflammation common to these disorders [63]. This limited specificity impedes the precise identification of the primary disease driver in multi-morbid patients, potentially leading to suboptimal therapeutic targeting.
Sensitivity and Detection Bias in Complex Patients
Sensitivity challenges emerge from the altered disease dynamics in multi-morbid populations. The accelerated disease progression observed in patients with T2D means that biomarkers validated in healthier populations may not detect pathological changes at the same thresholds [67]. Furthermore, detection bias presents a significant methodological challenge, as individuals with established conditions like T2D typically receive more frequent medical monitoring, potentially leading to earlier identification of additional conditions independent of the true biological progression [67]. This surveillance intensity creates analytical noise that complicates the validation of novel biomarkers intended for early detection in at-risk populations.
Table 1: Key Biomarker Limitations in Multi-Morbid Metabolic Conditions
| Biomarker | Primary Mechanism | Specificity Challenges | Sensitivity Considerations |
|---|---|---|---|
| HOMA-IR | Insulin Resistance | Lacks specificity for T2D vs. obesity/MASH; no universal cut-off [63] | Reduced accuracy in lean T2D patients; compromised in advanced disease [63] |
| HbA1c | Long-term Glycemic Control | Affected by hemoglobin variants, renal disease, anemia [63] | Limited utility in elderly; inadequate reflection of glucose variability [63] |
| CRP | Inflammation | Non-specific marker; elevated across metabolic, inflammatory, infectious conditions [63] | Variable across populations; limited predictive value for specific outcomes [63] |
| Liver Enzymes (ALT/AST) | Hepatocyte Damage | Elevated in MASH, drug-induced injury, alcoholic hepatitis [63] | Poor correlation with disease severity in MASH; variable cut-off values [63] |
| GDF-15 | Cellular Stress Response | Associated with aging, obesity, diabetes, inflammation [5] | Varies by demographic factors (age, gender, ethnicity) [5] |
Emerging Solutions and Methodological Approaches
Multimorbidity Quantification for Stratification
Accurately quantifying multimorbidity burden represents a critical first step in improving biomarker validation. Several validated approaches exist for this purpose:
- The GMA (Adjusted Morbidity Groups) Index: This tool utilizes a weighted measure of all diagnostics, combining both chronic and recent acute conditions. It has demonstrated high performance in explaining healthcare outcomes across subpopulations and outperforms simpler counts of chronic diseases [69].
- The Charlson Comorbidity Index: Originally designed to predict one-year mortality, this weighted index covers 19 conditions and remains widely used, particularly for mortality prediction [69].
- Standardized Disease Counts: Approaches like the HCUP (Healthcare Cost and Utilization Project) chronic condition indicator define chronic conditions based on functional limitations and need for ongoing intervention, providing exhaustive counts of 190 conditions [69].
These quantification systems enable researchers to stratify study populations by morbidity burden, allowing for the assessment of biomarker performance across different levels of clinical complexity.
Integrated Multi-Omics Approaches
The limitations of single biomarkers have prompted a shift toward integrated multi-omics approaches. Combining genomics, proteomics, and metabolomics data allows for the development of composite biomarker signatures that better capture the complexity of multi-morbid conditions [63]. For example, integrative analysis of bulk RNA-seq, single-cell RNA-seq, and spatial transcriptomic datasets has identified glycolysis-related key genes (ALDH3A1, CDK1, DEPDC1, HKDC1, and SOX9) in metabolic dysfunction-associated fatty liver disease (MAFLD) and elucidated their crosstalk with immune infiltration [5]. Such multidimensional approaches improve both sensitivity and specificity by capturing complementary aspects of disease pathophysiology.
Table 2: Experimental Reagents and Platforms for Multi-Omics Biomarker Discovery
| Research Tool Category | Specific Technologies/Platforms | Research Application |
|---|---|---|
| Transcriptomic Profiling | Bulk RNA-seq, Single-cell RNA-seq, Spatial Transcriptomics | Identification of disease-associated gene expression patterns and cellular interactions [5] |
| Proteomic Analysis | Immunoassays, Mass spectrometry-based proteomics | Quantification of protein biomarkers, inflammatory mediators, adipokines [63] [5] |
| Metabolomic Platforms | LC-MS, GC-MS, NMR spectroscopy | Comprehensive profiling of metabolites, lipids, branched-chain amino acids [5] |
| Computational Integration | Machine learning algorithms, Weighted Gene Co-expression Network Analysis (WGCNA) | Integration of multi-omics data, identification of key biomarker signatures [5] |
| Validation Assays | ELISA, qPCR, Immunohistochemistry, Functional assays | Experimental validation of candidate biomarkers in model systems and human samples [5] |
Advanced Analytical and Machine Learning Methods
Machine learning represents a powerful approach for addressing specificity and sensitivity challenges in multi-morbid conditions. These methods can identify complex, non-linear patterns in high-dimensional data that escape traditional statistical approaches. Research demonstrates that machine learning models can identify feature genes and their regulatory networks, including transcription factors like YY1 and FOXC1, and miRNAs such as hsa-miR-590-3p, which would be difficult to detect through conventional analysis [5]. AI-driven approaches using contrastive learning frameworks are also emerging for predictive biomarker discovery, showing particular promise in improving clinical trial outcomes [70]. These computational approaches enable the development of context-aware biomarker models that account for the presence of multiple conditions simultaneously.
Experimental Workflows for Biomarker Validation
Comprehensive Biomarker Assessment Protocol
A robust methodological framework is essential for evaluating biomarker performance in multi-morbid populations:
This workflow emphasizes the critical importance of initial stratification by multimorbidity burden using validated tools like the GMA index or Charlson score [69]. Subsequent multi-omics data integration and machine learning analysis enables the identification of biomarker patterns that remain effective across different levels of clinical complexity [5]. The final validation step must specifically assess biomarker performance in relevant subgroups stratified by morbidity burden to ensure equitable performance across the clinical spectrum.
Pathophysiological Integration Framework
Understanding biomarker relationships within the complex pathophysiology of multi-morbid conditions requires an integrated analytical approach:
This framework illustrates how different biomarker categories relate to core pathophysiological processes and clinical outcomes. While traditional biomarkers demonstrate limited specificity in multi-morbid contexts, emerging multi-omics approaches offer the potential for substantially improved diagnostic and prognostic precision by capturing the complexity of interacting disease processes [63] [5].
Addressing specificity and sensitivity challenges in multi-morbid conditions requires a fundamental shift from single-disease paradigms to integrated, systems-level approaches. The accelerated disease progression observed in conditions like T2D necessitates biomarkers that can detect pathological changes earlier and with greater precision in complex patients [67]. Promising avenues include the development of non-invasive biomarker panels that combine traditional clinical measures with novel omics-derived signatures, the application of machine learning for pattern recognition in high-dimensional data, and the validation of these tools in appropriately stratified multi-morbid populations [63] [5]. Future research must prioritize the creation of multidisciplinary frameworks that explicitly account for the reality of multimorbidity rather than attempting to eliminate it through restrictive study inclusion criteria. Only through such comprehensive approaches can biomarker science effectively address the clinical challenges presented by the growing population of patients with multiple interconnected chronic conditions.
Insulin resistance is a core pathophysiological component of metabolic syndrome and type 2 diabetes (T2D), driving the need for precise and reliable biomarkers in research and drug development [71]. The Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) is a widely used surrogate measure, calculated from fasting glucose and insulin concentrations [72]. However, its analytical variability poses significant challenges for cross-study comparisons and longitudinal assessment. Simultaneously, untargeted metabolomics has emerged as a powerful tool for discovering novel metabolic signatures of insulin resistance and related pathologies, yet it also faces standardization hurdles [73] [74]. This technical guide examines the sources of analytical variability in these key areas and outlines standardized protocols and computational approaches to enhance reproducibility, with the overarching goal of advancing biomarker research for metabolic diseases.
Analytical Variability in HOMA-IR
The estimation of β-cell function (HOMA-β) and insulin resistance (HOMA-IR) using the HOMA model is significantly affected by preanalytical and analytical factors [75].
- Blood Sample Type: Insulin measurements are 15% lower in heparinized plasma compared to serum, which is now more commonly used in clinical practice. The original HOMA database was built using heparinized plasma, creating an inherent discrepancy when applying the model to serum-based measurements [75].
- Insulin Assay Specificity: Different insulin immunoassays demonstrate substantial variability. Studies comparing 11 different insulin assays found a twofold variation in HOMA estimates, which can be metabolically significant. This variation arises from differences in assay specificity, particularly concerning cross-reactivity with proinsulin and its metabolites [75].
- HOMA Calculator Selection: The choice of HOMA calculator (specific insulin [SI] vs. radioimmunoassay [RIA] calculators, version 2.2) impacts results. β-cell function differed by 11% and insulin resistance by 15% when estimates derived from specific insulin were calculated using the RIA rather than the SI calculator [75].
Table 1: Impact of Analytical Factors on HOMA Estimates [75]
| Factor | Impact on HOMA Estimates | Clinical/Research Implication |
|---|---|---|
| Sample Type (Plasma vs. Serum) | Insulin 15% lower in heparinized plasma vs. serum | Creates systematic bias between studies using different sample types |
| Insulin Assay Variability | Up to twofold variation in HOMA-IR and HOMA-β | Significant metabolic differences; impedes study comparisons |
| Calculator Selection (SI vs. RIA) | 11% difference in HOMA-β; 15% difference in HOMA-IR | Inconsistent results depending on calculator chosen |
Standardized HOMA-IR Protocol for Research
To ensure comparable HOMA estimates across studies, the following protocol is recommended:
Sample Collection and Processing:
- Sample Type: Clearly specify whether serum or plasma is used. For longitudinal or multi-center studies, standardize the sample type across all sites and timepoints.
- Processing: Centrifuge blood samples at 1500×g for 10 minutes at 4°C within 30-60 minutes of collection [73].
- Storage: Aliquot samples and store immediately at -80°C. Avoid multiple freeze-thaw cycles [74].
Insulin Measurement:
- Assay Selection: Use insulin assays traceable to an international reference method procedure. Validate the assay's cross-reactivity with proinsulins [75].
- Quality Control: Implement tri-level quality controls in each run. Coefficients of variation (CV) should ideally be <5% [75].
Calculation and Reporting:
- Calculator: Use the HOMA2 calculator (version 2.2) from the University of Oxford (www.dtu.ox.ac.uk). Specify whether the SI or RIA calculator was used based on the insulin assay's characteristics [75].
- Metadata: In publications, explicitly report the sample type, specific insulin assay used, HOMA calculator version, and any sample storage conditions.
Metabolomic Approaches for Assessing Metabolic Dysfunction
Metabolomic Signatures of Insulin Resistance and Metabolic Syndrome
Untargeted metabolomics captures global metabolic perturbations, providing a powerful approach for identifying novel biomarkers and subtypes within metabolic syndrome and T2D.
- Insulin Resistance Signatures: A 30-metabolite panel has been identified that discriminates extremes of HOMA-IR with high accuracy (AUC = 0.82). This panel includes specific amino acids (e.g., methionine, proline), lipid species (lysophosphatidylcholines, sphingomyelins, phosphatidylcholines), and organic acids (3-hydroxybutanoic acid) [76].
- Metabolic Syndrome Heterogeneity: Unsupervised clustering of plasma metabolomic profiles from individuals with Cardiovascular-Kidney-Metabolic (CKM) syndrome reveals three distinct metabolic subtypes: glycerophospholipid-enriched, fatty acyl-dominant, and glycolipid-enriched clusters. This stratification uncovers significant metabolic heterogeneity not apparent from conventional clinical staging [73].
- Continuous Metabolic Syndrome Severity Score: Confirmatory factor analysis (CFA) of the five traditional MetS components (waist circumference, triglycerides, HDL-C, systolic blood pressure, and fasting plasma glucose) allows creation of a continuous MetS severity score (cMetS-S). This score correlates with HOMA-IR and provides a more nuanced assessment of metabolic risk than dichotomous MetS criteria [77].
Table 2: Key Metabolite Classes in Insulin Resistance and Metabolic Syndrome
| Metabolite Class | Specific Examples | Association with IR/MetS | Proposed Biological Role |
|---|---|---|---|
| Amino Acids | Branched-chain amino acids, Aromatic amino acids, Methionine, Proline | Positively associated with HOMA-IR [76] | Mitochondrial dysfunction, altered substrate utilization |
| Complex Lipids | Specific phosphatidylcholines, sphingomyelins, lysophosphatidylcholines | Both positive and negative associations depending on species [76] | Membrane integrity, signaling pathways, inflammation |
| Fatty Acyls | Linoleic acid, Palmitic acid, Stearic acid | Positively associated with HOMA-IR [76] | Lipotoxicity, inflammation, mitochondrial stress |
| Organic Acids | 2- and 3-Hydroxybutyrate, Lactate | Positively associated with HOMA-IR [76] | Altered redox state, mitochondrial function |
Standardized Metabolomic Workflow for Insulin Resistance Assessment
Sample Preparation:
- Extraction: Add 400 µL of cold methanol containing internal standards to 50 µL of plasma. Vortex mix, then centrifuge to remove proteins [73].
- Internal Standards: Include a comprehensive set of stable isotope-labeled standards covering key metabolite classes: carnitines (e.g., C2:0-d3, C10:0-d3, C16:0-d3), lipids (LPC 19:0, FFA C16:0-d3, FFA C18:0-d3), bile acids (cholic acid-d4, chenodeoxycholic acid-d4), and amino acids (phenylalanine-d5, leucine-d3, tryptophan-d5) [73].
LC-MS Analysis:
- Chromatography: Utilize reverse-phase UHPLC with C8 and HSS T3 columns for positive and negative ionization modes, respectively. Employ a water/acetonitrile gradient with 6.5 mM ammonium bicarbonate for negative mode and 0.1% formic acid for positive mode [73].
- Mass Spectrometry: Operate in both full scan (m/z 100-1250) and data-dependent MS2 modes. Set ion spray voltage to 5.5 kV (positive) and -4.5 kV (negative). Use collision energy of 10 V for MS and 35 ± 15 V for MS/MS [73].
Data Processing and Statistical Analysis:
- Preprocessing: Perform peak picking, alignment, and integration using platforms such as XCMS or MS-DIAL. Normalize data using quality control-based methods and internal standards.
- Multivariate Statistics: Apply orthogonal partial least squares-discriminant analysis (OPLS-DA) to identify metabolites discriminating sample groups [73].
- Machine Learning: Implement regularized regression methods (LASSO, Elastic Net) to build metabolite models predicting HOMA-IR or MetS severity, using cross-validation to avoid overfitting [74] [76].
Computational Approaches for Metabolite-Based Risk Estimation
Machine Learning for Estimating Insulin Resistance
Advanced computational methods enable accurate estimation of insulin resistance from metabolomic profiles, potentially reducing reliance on traditional measures.
- Model Performance: Elastic Net regression models combining metabolomic data with basic clinical variables (age, sex, BMI) can estimate insulin sensitivity index (SI) from frequently sampled intravenous glucose tolerance tests (FSIGT) with high accuracy (r² = 0.74-0.77 in testing datasets) [74].
- Model Generalizability: Models developed in one population (e.g., Mexican Americans from San Luis Valley) show good performance in external validation cohorts (e.g., Mexican Americans from San Antonio and African Americans from Los Angeles) [74].
- HOMA-IR Estimation: Similar approaches successfully estimate HOMA-IR, providing a less invasive alternative while capturing more metabolic information than HOMA-IR alone [74].
Metabolic Syndrome Severity Scoring
Continuous MetS severity scores address limitations of dichotomous MetS definitions and enable more sensitive tracking of metabolic changes.
- Factor Loadings: In West Asian populations, confirmatory factor analysis reveals triglycerides have the highest factor loading for MetS, followed by waist circumference. Systolic blood pressure shows stronger correlation with MetS in women than men [77].
- Validation: The continuous MetS severity score correlates with HOMA-IR and effectively predicts traditional MetS diagnosis (AUC > 0.90 in validation datasets) [77].
- Utility: This continuous score facilitates monitoring of individual metabolic trends and assessment of intervention effects with greater sensitivity than dichotomous MetS criteria [77].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for HOMA-IR and Metabolomic Studies
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Stable Isotope Internal Standards | Quantitative normalization for metabolomics; correction for technical variability | Include carnitines, lipids, amino acids, bile acids with stable isotope labels [73] |
| Quality Control Pools | Monitoring LC-MS instrument performance; batch-to-batch normalization | Create from representative sample pools; analyze repeatedly throughout sequence [74] |
| Reference Insulin Materials | Calibration of insulin immunoassays; ensuring cross-assay comparability | Use materials traceable to international reference methods [75] |
| Standardized HOMA Calculator | Consistent calculation of HOMA-IR and HOMA-β | Use HOMA2 calculator v2.2 from University of Oxford [75] |
| Lipid Extraction Solvents | Comprehensive metabolite extraction from plasma/serum | Methanol:methyl-tert-butyl ether:water systems provide broad coverage [73] [76] |
| Chromatography Columns | Separation of diverse metabolite classes prior to MS detection | C8 and HSS T3 columns for reverse-phase; HILIC for polar metabolites [73] |
Standardization of HOMA-IR measurements and metabolomic assays is critical for advancing research on metabolic syndrome and type 2 diabetes. Key considerations include harmonizing preanalytical procedures, using validated and traceable insulin assays, applying appropriate computational models, and reporting detailed methodological metadata. The integration of standardized HOMA-IR with validated metabolomic signatures offers a powerful approach for precise metabolic phenotyping, enabling more reproducible research and accelerating the development of targeted interventions for metabolic diseases. Future efforts should focus on establishing universal reference materials for insulin assays and validating standardized metabolomic workflows across diverse populations and platforms.
The global burden of metabolic syndrome (MetS) and type 2 diabetes mellitus (T2DM) continues to escalate, presenting a formidable challenge to public health systems worldwide. MetS—a cluster of interrelated metabolic risk factors including abdominal obesity, dyslipidemia, hypertension, and hyperglycemia—significantly increases the risk of cardiovascular disease (CVD), T2DM, and all-cause mortality [78] [79]. The prevalence of metabolic syndrome in high-income countries has been estimated at 27.4% based on NCEP-ATP III criteria, showing an alarming increase from 24.2% during 1996–2005 to 31.9% in 2010–2021 [78]. This rising prevalence underscores the critical need for advanced biomarker research that can account for the substantial variations in disease manifestation and progression across different population subgroups.
Biomarker discovery and validation have emerged as pivotal components in the effort to combat metabolic disorders, offering potential for early detection, risk stratification, and personalized intervention strategies [15]. However, the performance and clinical utility of these biomarkers are profoundly influenced by population-specific factors such as ethnicity, age, and comorbid conditions. A comprehensive understanding of these influences is essential for researchers and drug development professionals aiming to develop effective, targeted therapies and diagnostic tools. This technical guide synthesizes current evidence on population-specific considerations in metabolic biomarker research, providing a foundation for advancing precision medicine in MetS and T2DM.
Epidemiological Landscape: Prevalence Disparities by Ethnicity and Sex
Significant disparities in MetS and T2DM prevalence exist across ethnic groups, with important implications for biomarker research and clinical practice. A comprehensive meta-analysis revealed that ethnic minority women experience the highest MetS prevalence (31.7%), while ethnic majority women show the lowest (22.7%) [78]. Notably, MetS is more prevalent in ethnic minority women than men, with the most pronounced difference observed in Asian populations (approximately 15 percentage points) [78]. When stratified by specific ethnic groups, Asian women demonstrate the highest MetS prevalence (41.2%), while Black/African women show the lowest (26.7%) [78]. Among men, indigenous minority groups exhibit the highest prevalence (34.3%), with Black/African men again showing the lowest (19.8%) [78].
Data from the National Health and Nutrition Examination Survey (NHANES) in the United States corroborates these ethnic disparities, indicating that from 2007-2012, non-Hispanic Black men were less likely than non-Hispanic White men to have MetS (OR, 0.77; 95% CI, 0.66–0.89), while non-Hispanic Black women were more likely than non-Hispanic White women to have MetS (OR, 1.20; 95% CI, 1.02–1.40) [79]. Beyond ethnicity, socioeconomic factors independently influence MetS risk, with low education level (OR, 1.56; 95% CI, 1.32–1.84) and advanced age (OR, 1.73; 95% CI, 1.67–1.80) significantly associated with increased likelihood of metabolic syndrome [79].
Table 1: Metabolic Syndrome Prevalence by Ethnicity and Sex in High-Income Countries (NCEP-ATP III Criteria)
| Ethnic Group | Women (%) | Men (%) | Sex Difference (percentage points) |
|---|---|---|---|
| All Ethnicities | 27.4 | 27.4 | 0.0 |
| Ethnic Minority | 31.7 | 27.9 | +3.8 |
| Ethnic Majority | 22.7 | 26.9 | -4.2 |
| Asian | 41.2 | 26.3 | +14.9 |
| Black/African | 26.7 | 19.8 | +6.9 |
| Indigenous | - | 34.3 | - |
Table 2: Adjusted Odds Ratios for Metabolic Syndrome in US Adults (NHANES 2007-2012)
| Demographic Factor | Reference Group | Comparison Group | Adjusted OR (95% CI) |
|---|---|---|---|
| Race & Sex | Non-Hispanic White men | Non-Hispanic Black men | 0.77 (0.66–0.89) |
| Race & Sex | Non-Hispanic White women | Non-Hispanic Black women | 1.20 (1.02–1.40) |
| Education | College graduate | Less than high school | 1.56 (1.32–1.84) |
| Age | 18-39 years | ≥60 years | 1.73 (1.67–1.80) |
Ethnicity-Specific Biomarker Variations and Considerations
Ethnicity significantly influences both the prevalence of metabolic disorders and the behavior of associated biomarkers, necessitating careful consideration in research design and interpretation. Growth differentiation factor 15 (GDF-15), an emerging biomarker for metabolic stress, demonstrates notable ethnic variations. Research from the Kuwait Diabetes Epidemiology Program revealed that Arab participants had significantly higher GDF-15 levels (597.0 ng/L) compared to South Asians (514.9 ng/L) and Southeast Asians (509.9 ng/L) [15]. After adjustment for confounding factors, South Asian ethnicity remained independently associated with lower GDF-15 levels (β = -41.7, 95% CI: -67.2, -16.2) compared to Arab ethnicity [15]. These findings highlight the importance of establishing ethnic-specific reference ranges for emerging biomarkers.
The relationship between urinary biomarkers and MetS also demonstrates ethnic dimensions. A cross-sectional study conducted in Zhejiang, China, found that 24-hour urine microalbumin excretion was significantly higher in participants with MetS (6.35 mg/24h) than in those without (4.12 mg/24h; P < 0.0001) [61]. When microalbumin excretion was divided into quartiles, adjusted odds ratios for MetS increased progressively with higher quartiles (Q1: reference; Q2: 1.53; Q3: 1.99; Q4: 2.75; P for trend = 0.0004) [61]. This association was particularly pronounced for the elevated fasting blood glucose component of MetS (Q1: reference; Q2: 1.31; Q3: 1.35; Q4: 2.20; P for trend = 0.0005) [61]. These findings suggest the potential utility of urinary microalbumin as a non-invasive biomarker for MetS risk assessment in Asian populations, though validation in other ethnic groups is necessary.
Table 3: Ethnic Variations in GDF-15 Biomarker Levels (KDEP Study)
| Variable | Subgroup | GDF-15 Level (ng/L) | P-value |
|---|---|---|---|
| Ethnicity | Arab | 597.0 | <0.001 |
| South Asian | 514.9 | ||
| Southeast Asian | 509.9 | ||
| Sex | Male | 580.6 | <0.001 |
| Female | 519.3 | ||
| Age | >50 years | 781.4 | <0.001 |
| <50 years | 563.4 |
Age and Comorbidity Considerations in Biomarker Research
Age represents a critical biological variable that significantly influences biomarker levels and their association with metabolic outcomes. GDF-15 demonstrates a strong positive correlation with age, with individuals over 50 years exhibiting markedly higher levels (781.4 ng/L) compared to those under 50 (563.4 ng/L) [15]. This age-associated increase in GDF-15 may reflect accumulating cellular stress and inflammation associated with aging, positioning GDF-15 as a potential biomarker of biological aging in metabolic disorders [80].
The prognostic significance of biomarkers in T2DM also varies considerably with age. Research on age-related adverse health outcomes in diabetic patients aged ≥60 years identified GDF-15 and adiponectin as significant predictors, with the group exhibiting both GDF-15 and adiponectin levels higher than the median experiencing significantly more age-related adverse health outcomes [80]. In a multivariate model combining clinical indicators and biomarkers, GDF-15 and the Barthel Index (a measure of functional independence) were independently associated with the occurrence of age-related adverse health outcomes [80]. These findings highlight the value of composite assessments incorporating both biomarkers and functional measures for risk stratification in older diabetic populations.
Comorbidities further complicate biomarker interpretation in metabolic disorders. A novel composite biomarker—ln[ALP × sCr]—has been developed to reflect integrated cardiac-renal dysfunction in T2DM [81]. This biomarker leverages alkaline phosphatase (ALP), associated with arterial stiffness and cardiovascular risk, and serum creatinine (sCr), a marker of renal function [81]. In a deep learning analysis of NHANES data, T2DM patients in the highest quartile of ln[ALP × sCr] exhibited significantly elevated risks of all-cause (HR 1.47, 95% CI 1.18–1.82), cardiovascular (HR 1.44, 95% CI 1.01–2.04), and diabetes-related mortality (HR 2.50, 95% CI 1.58–3.96) compared to those in the lowest quartile [81]. Mediation analysis indicated that serum vitamin D accounted for 24.3% of the association between the composite biomarker and all-cause mortality (P < 0.001) [81], suggesting complex interactions between biomarkers and nutritional status in determining mortality risk.
Methodological Approaches for Population-Specific Biomarker Research
Metabolomic Network Analysis
Network analysis approaches provide powerful tools for understanding the complex interrelationships among metabolites and identifying hub biomarkers within metabolic pathways. A metabolome-wide association study analyzed 168 circulating metabolites quantified by nuclear magnetic resonance (NMR) at baseline in 98,831 UK Biobank participants [82]. The study employed Cox proportional hazards models to identify metabolites significantly associated with T2DM risk over a median 12-year follow-up [82]. Network analysis was then applied to compute topological attributes (degree, betweenness, closeness, and eigencentrality) and detect small-world features (high clustering, short path lengths) [82]. This approach identified total triglycerides and large high-density lipoprotein (HDL) cholesterol as pivotal biomarkers in the 'risk' and 'protective' modules, respectively, based on their high eigencentrality [82]. Additionally, total branched-chain amino acids (BCAAs) exhibited small-world network characteristics exclusively in pre-T2DM individuals, suggesting their utility as early indicators [82]. GlycA demonstrated high closeness centrality in females, indicating potential as a female-specific risk biomarker [82].
Diagram 1: Metabolomic Network Analysis Workflow
24-Hour Urinary Biomarker Assessment
The comprehensive assessment of urinary biomarkers requires rigorous standardization of collection and analytical procedures. In a study examining the association between 24-hour urinary biomarkers and MetS, researchers implemented a detailed protocol [61]. Participants collected urine over a full 24-hour period, with researchers recording start and end times and measuring total urine volume [61]. Samples with urine volume less than 500 mL or greater than 4000 mL were excluded to ensure collection quality [61]. Urinary sodium and potassium were measured using indirect ion-selective electrode methodology, while creatinine was quantified via the Jaffe rate method and microalbumin through immunoturbidimetry [61]. Statistical analysis included Wilcoxon rank-sum tests for non-normally distributed continuous variables, chi-square tests for categorical variables, and logistic regression to investigate associations between urinary microalbumin excretion and MetS and its components, with adjustment for sociodemographic and lifestyle factors [61].
Diagram 2: 24-Hour Urinary Biomarker Assessment Protocol
Deep Learning for Composite Biomarker Development
Advanced computational approaches enable the identification of novel composite biomarkers that integrate information across multiple biological systems. In a study to predict mortality in T2DM, researchers applied a deep learning model to NHANES data from 82,091 U.S. adults [81]. The model incorporated a comprehensive set of clinical, biochemical, and demographic features, including demographics, lifestyle factors, clinical history, diabetes-specific parameters, vital signs, anthropometrics, and extensive biomarker panels [81]. A feedforward neural network was constructed and trained using a stratified 70/15/15 train-validation-test split, with input features standardized and categorical variables one-hot encoded [81]. Model hyperparameters were optimized through grid search, and SHAP (Shapley Additive Explanations) values were calculated to quantify feature contributions to model predictions [81]. This approach identified ALP, sCr, and vitamin D as top mortality-related biomarkers, leading to the development of the composite index ln[ALP × sCr] to reflect integrated cardiac-renal dysfunction [81].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Essential Research Reagents for Metabolic Biomarker Studies
| Reagent/Assay | Application | Technical Considerations |
|---|---|---|
| NMR Spectroscopy Platforms | Quantitative analysis of circulating metabolites in metabolomic studies [82] | Enables simultaneous quantification of multiple metabolite classes; requires specialized instrumentation and expertise |
| Mass Spectrometry Systems | High-sensitivity detection and quantification of lipids, amino acids, and other metabolites [83] | Offers high sensitivity and specificity; can be coupled with liquid chromatography for improved separation |
| Automated Enzymatic Assays | Measurement of ALP, creatinine, and traditional metabolic markers [81] | Standardized protocols available; suitable for high-throughput analysis |
| Immunoassays (ELISA/Luminex) | Quantification of adipokines (adiponectin, leptin), cytokines, and GDF-15 [80] [15] | Platform selection depends on required sensitivity and multiplexing needs; requires validation for each population |
| RNA Extraction & qPCR Kits | Analysis of miRNA expression (e.g., miR-484) and glycolysis-related genes [15] | Requires strict RNA quality control; normalization strategy critical for accurate quantification |
| Network Analysis Software | Construction and visualization of metabolomic networks; calculation of topological attributes [82] | Enables identification of hub biomarkers; requires appropriate statistical thresholds and validation |
Population-specific factors exert substantial influences on biomarker levels, performance, and clinical utility in metabolic syndrome and type 2 diabetes research. Ethnicity, age, and comorbidities must be considered throughout the biomarker discovery and validation pipeline to ensure equitable application of emerging technologies and personalized medicine approaches. Metabolomic network analysis, comprehensive urinary biomarker assessment, and deep learning approaches offer powerful methodological frameworks for advancing our understanding of these complex relationships. Future research priorities should include deliberate oversampling of underrepresented populations, prospective validation of emerging biomarkers across diverse demographic groups, and systematic assessment of how population-specific factors influence biomarker thresholds and interpretation. By adopting these rigorous, inclusive approaches, researchers and drug development professionals can contribute to reducing disparities in metabolic disease burden and developing more effective, personalized interventions.
The accurate measurement of biomarkers is fundamental to advancing research in metabolic syndrome and type 2 diabetes. These biomarkers are critical for diagnosing patients, stratifying risk, evaluating novel drug therapies, and understanding disease pathophysiology. However, the reliability of this data is critically dependent on the rigorous control of pre-analytical and biological variables. Among the most significant of these variables are the pharmacological agents patients consume and their metabolic state during blood collection, particularly whether they are fasting or non-fasting. Failure to account for these confounders can introduce substantial bias, leading to misinterpretation of results, flawed conclusions, and ultimately, the failure of clinical trials.
This whitepaper provides an in-depth technical guide for researchers and drug development professionals on the confounding effects of medications and non-fasting states on biomarker levels. Framed within the context of a broader thesis on biomarkers for metabolic syndrome and type 2 diabetes, it synthesizes current evidence, summarizes quantitative data, details experimental protocols, and provides visual tools to aid in the design and interpretation of studies in this complex field.
Impact of Medications on Biomarker Profiles
Medications, particularly those used to treat diabetes and dyslipidemia, can significantly alter biomarker concentrations, often in ways that are independent of their primary glycemic or lipid-lowering effects. Understanding these pleiotropic impacts is essential for isolating a drug's true therapeutic effect from its confounding influence on common research endpoints.
Novel Antidiabetic Agents and Lipid Biomarkers
Novel antidiabetic agents have demonstrated significant benefits on cardiovascular outcomes, which appear to be partially mediated through changes in the lipid profile, a key component of metabolic syndrome. Diabetic dyslipidemia is characterized by hypertriglyceridemia, decreased high-density lipoprotein (HDL) cholesterol, and a preponderance of small, dense low-density lipoprotein (LDL) particles [84].
Table 1: Impact of Novel Antidiabetic Agents on Lipid Biomarkers
| Drug Class | Mechanism of Action | Key Effects on Lipid Biomarkers | Proposed Mechanisms |
|---|---|---|---|
| SGLT2 Inhibitors [84] | Inhibits glucose reabsorption in renal proximal tubules; induces glucosuria. | - Modest increase in LDL-C and HDL-C- Reduction in triglycerides- Decreased visceral adipose tissue | - Metabolic shift to lipid utilization & beta-oxidation [84].- Increased fatty acid mobilization and oxidation [84].- Inhibition of hepatic lipogenesis [84]. |
| GLP-1 Receptor Agonists [84] | Enhances glucose-dependent insulin secretion; suppresses glucagon release. | - Consistent reduction in triglycerides- Modest reduction in LDL-C- Increase in HDL-C | - Weight loss-mediated improvements.- Direct effects on lipid metabolism. |
| DPP-4 Inhibitors [84] | Inhibits degradation of endogenous GLP-1. | - Neutral or minimal effects on lipid profile | - Effects are generally less pronounced than other classes. |
Anti-inflammatory Effects of Antidiabetic Medications
Chronic low-grade inflammation is a cornerstone of metabolic syndrome and type 2 diabetes, making inflammatory cytokines key biomarkers in research. Different antidiabetic medications exhibit distinct modulatory effects on these inflammatory pathways.
Table 2: Impact of Antidiabetic Medications on Inflammatory Biomarkers and Adipokines
| Treatment Regimen | Impact on IL-6 | Impact on TNF-α | Impact on Adiponectin | Study Details |
|---|---|---|---|---|
| Insulin Therapy [85] | Significant reduction | Significant reduction | Partial elevation | Cross-sectional study of 360 Iraqi T2DM patients. |
| Metformin Monotherapy [85] | Not Specified | Not Specified | Significant increase | |
| Metformin + Glimepiride [85] | Not Specified | Not Specified | Lower than Metformin alone | Associated with most favorable lipid profile. |
| Recurrent Circadian Fasting [86] | Elevated (IL-6, IL-8) | Decreased | Not Measured | 29-day dawn-to-dusk fasting study in 78 men. |
Experimental Protocol: Assessing Drug Effects on Inflammatory Markers
The following protocol is adapted from a cross-sectional study investigating the impact of antidiabetic medications on inflammatory markers and adiponectin [85].
1. Study Population and Grouping:
- Recruit patients with a confirmed diagnosis of type 2 diabetes according to standard criteria (e.g., ADA).
- Establish inclusion/exclusion criteria to control for confounders: age (>30 years), stable medication regimen for >6 months, and absence of conditions affecting inflammation (e.g., active infections, immunosuppressive therapy, autoimmune disease, cancer).
- Divide participants into groups based on their stable treatment regimen (e.g., insulin monotherapy, metformin monotherapy, combination therapies).
2. Sample Collection:
- Collect venous blood samples after a confirmed overnight fast (≥8 hours) to standardize metabolic state.
- Draw blood into appropriate vacutainers: EDTA tubes for plasma and gel-clot activator tubes for serum.
- Centrifuge samples to separate plasma/serum and aliquot into cryovials for storage at -80°C until analysis.
3. Laboratory Analysis:
- Glycemic and Lipid Control: Measure standard parameters (fasting glucose, HbA1c, lipid profile) using automated clinical chemistry analyzers.
- Inflammatory Biomarkers (IL-6, TNF-α): Quantify using commercial, high-sensitivity Enzyme-Linked Immunosorbent Assay (ELISA) kits. Perform all assays in duplicate according to the manufacturer's protocol. Calculate concentrations from a standard curve generated with known standards.
- Adiponectin: Quantify using a sandwich ELISA kit, following a similar duplicate protocol.
4. Statistical Analysis:
- Test data for normality using Shapiro-Wilk test.
- Use non-parametric tests (e.g., Kruskal-Wallis) for group comparisons if data is not normally distributed.
- Perform post-hoc analyses with corrections for multiple comparisons.
- Use multivariable regression models to adjust for potential confounders such as age, sex, BMI, and disease duration.
Impact of Non-Fasting States on Biomarker Levels
The shift from traditional fasting blood draws to non-fasting sampling in clinical practice and research necessitates a clear understanding of how postprandial metabolism affects key biomarkers.
Fasting vs. Non-Fasting Lipid Measurements
The consensus is moving towards accepting non-fasting lipid panels for cardiovascular risk assessment, but understanding the magnitude of change is crucial for data interpretation.
Table 3: Differences Between Fasting and Non-Fasting Lipid Parameters
| Lipid Parameter | Typical Change in Non-Fasting State | Clinical/Research Implications | Citation |
|---|---|---|---|
| Triglycerides (TG) | Increase (peak 2-4 hours postprandial) | - Remnant cholesterol may be a better postprandial risk indicator.- Re-measure fasting TG if non-fasting TG ≥350 mg/dL. | [87] |
| LDL-C (Calculated) | Variable (may artifactually decrease with high TG) | Friedewald equation becomes unreliable when TG >200 mg/dL. Direct LDL measurement is preferred in non-fasting state. | [87] |
| Total Cholesterol | Minimal change | Non-fasting levels are generally reliable. | [87] |
| HDL-C | Minimal change | Non-fasting levels are generally reliable. | [87] |
| Aβ40 and Aβ42 | Increase in non-fasting state | Fasting condition influences measurements of amyloid-β peptides in Alzheimer's research. The Aβ42/40 ratio mitigates this effect. | [88] |
| pTau181, GFAP, Nf-L | No significant difference | These neurodegeneration biomarkers appear robust to fasting status. | [88] |
A study of 686 patients with normal triglyceride levels found a strong linear correlation between fasting and non-fasting lipid profiles. Critically, the presence of statin treatment did not alter the pattern or magnitude of differences between fasting and non-fasting states, suggesting that non-fasting testing is acceptable in statin-treated patients [87].
Experimental Protocol: Comparing Fasting and Non-Fasting Biomarkers
This protocol is based on studies designed to evaluate the impact of fasting status on various biomarkers [87] [88].
1. Study Design:
- A within-subjects, cross-over design is ideal, where each participant serves as their own control.
- Schedule two blood collection visits separated by a short, defined washout period (e.g., 1-2 weeks).
2. Blood Collection:
- Fasting Visit: Participants fast for 8-12 hours (water permitted) prior to blood collection.
- Non-Fasting Visit: Participants consume a standardized meal. Blood is collected at a specified time post-prandially (e.g., 2-4 hours after the start of the meal) to capture the peak postprandial response.
- Process and store all samples identically.
3. Data Analysis:
- Use paired t-tests or Wilcoxon signed-rank tests to compare biomarker levels between fasting and non-fasting states within individuals.
- Calculate the mean percentage difference for each biomarker.
- Use Bland-Altman analysis to assess the agreement between fasting and non-fasting measurements.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents and Kits for Biomarker Analysis
| Item | Specific Example | Function in Research |
|---|---|---|
| ELISA Kits | Human α-Klotho ELISA Kit [89], Adiponectin Sandwich ELISA (Elabscience E-EL-H6122) [85], IL-6 ELISA (Elabscience E-EL-H6156) [85], TNF-α ELISA (Elabscience E-EL-H0109) [85] | Quantifying low-abundance proteins (cytokines, adipokines, specialized proteins) in serum/plasma with high sensitivity. |
| Automated Biochemistry Analyzers | Hitachi 7150 Analyzer [87], Cobas Integra 400 Plus Analyzer (Roche) [85] | High-throughput, automated measurement of standard clinical chemistry parameters (lipids, glucose, HbA1c). |
| Specialized Assay Kits | N4PE Kit (Aβ40, Aβ42, Nf-L, GFAP), pTau181 v2.1 Advantage Kit (Quanterix) [88] | Ultrasensitive measurement of neurology biomarkers using digital ELISA technology (e.g., Simoa). |
| Standardized Diets | High-Fat Diet (HFD, 45% fat, Dyets Inc. 104293) [90], Standard Rodent Chow (AIN-93G, Dyets Inc. 110700) [90] | Controlling for dietary confounders in animal models of metabolic disease. |
Visualizing Confounding Pathways and Research Workflows
Pathway: Medication Effects on Biomarker Networks
Workflow: Protocol for Fasting/Non-Fasting Biomarker Comparison
Evaluating Biomarker Efficacy and Predictive Performance
The identification and validation of robust biomarkers for metabolic syndrome (MetS) and type 2 diabetes (T2D) represent a fundamental challenge in metabolic disease research. Population-based cohort studies provide the essential foundation for this validation process, enabling researchers to distinguish true biological signals from background noise and establish reliable associations across diverse populations. The Cooperative Health Research in the Augsburg Region (KORA) and Study of Health in Pomerania (SHIP) platforms stand as paradigm-shifting resources in this endeavor, offering deeply phenotyped, population-based samples that have dramatically accelerated biomarker discovery and validation.
These studies are particularly valuable within the context of metabolic disease research, where disease heterogeneity, population-specific variations, and complex pathophysiology complicate biomarker development. The KORA F4/FF4 and SHIP-TREND-0 cohorts provide not only substantial sample sizes but also comprehensive phenotyping, longitudinal follow-up, and standardized biochemical analyses—essential components for establishing biomarker validity, clinical utility, and generalizability. This technical guide examines the methodologies, validation frameworks, and key insights derived from these cornerstone studies, providing researchers with practical frameworks for biomarker validation in large-scale populations.
Table 1: Core Characteristics of KORA F4 and SHIP-TREND-0 Cohorts
| Characteristic | KORA F4 | SHIP-TREND-0 |
|---|---|---|
| Region | Augsburg, Southern Germany | Pomerania, Northeast Germany |
| Sample Size | 3,080 participants (F4) [91] | 4,420 participants [92] |
| Age Range | 32-81 years [92] | 20-79 years [93] |
| Key Measurements | OGTT, biomarkers, inflammation markers, neuropathy assessment [91] [94] | Multiplex cytokines, metabolomics, nasal swabs, MRI [95] [93] |
| Follow-up Studies | FF4 (6.5 years later) [91] | Planned follow-ups |
| Special Features | Assessment of subclinical inflammation, neuropathy, diabetes subtypes [91] | Cytokine atlas, metabolomics, microbiome data [95] |
Cohort Fundamentals: Design and Methodological Frameworks
KORA F4/FF4 Study Design
The KORA F4 study (2006-2008) represents a follow-up examination of the population-based KORA S4 survey (1999-2001), establishing a robust longitudinal framework for investigating metabolic disease progression [91]. The study implemented rigorous protocols for assessing glucose tolerance, complications, and biomarker profiles. Participants aged 62-81 years underwent detailed phenotyping for distal sensorimotor polyneuropathy (DSPN) using the Michigan Neuropathy Screening Instrument (MNSI), with a score >2 points defining prevalent and incident DSPN [94]. Oral glucose tolerance tests (OGTT) were conducted after an overnight fast, with glucose tolerance categories (normal glucose tolerance, impaired fasting glucose, impaired glucose tolerance, and type 2 diabetes) defined according to American Diabetes Association criteria [94]. The FF4 follow-up (2013-2014) enabled prospective analyses with a mean follow-up time of 6.5±0.2 years for incident T2D, chronic kidney disease (CKD), and DSPN, and 7.8±1.9 years for incident cardiovascular disease (CVD) [91].
SHIP-TREND-0 Cohort Structure
SHIP-TREND-0 recruited participants between 2008-2012 from a stratified random sample of adults aged 20-79 years from population registries in Western Pomerania, Northeast Germany [93]. The study's objective was a comprehensive assessment of population health with "the widest focus possible" across various risk factors, subclinical disorders, and clinical diseases [93]. The cohort design incorporated functional tests, blood examinations, whole-body magnetic resonance imaging (MRI), OMICs analyses of body fluids, extensive questionnaires, and specialized collections such as nose swabs for microbiological studies [93]. This comprehensive approach has enabled multidimensional analyses of metabolic, inflammatory, and microbiological factors in population health.
Standardized Biomarker Measurement Protocols
Both cohorts implemented stringent laboratory protocols to ensure biomarker data quality. In KORA F4, serum 25-hydroxyvitamin D (25(OH)D) concentrations were measured using the LIAISON 25OH Vitamin D TOTAL Assay (DiaSorin Inc., Stillwater, MN, USA), with a minimum detectable limit of 10 nmol/L and interassay coefficients of variation of 8.7-9.1% for target values [94]. Kidney function was assessed using estimated glomerular filtration rate (eGFR) calculated according to the Chronic Kidney Disease Epidemiology (CKD-EPI 2012) equation based on both serum creatinine and cystatin-C [91]. In SHIP-TREND-0, cytokine profiling was performed using a bead-based multiplex-assay (Merck HCYTA-60K) on a FLEXMAP 3D instrument, quantifying 47 plasma cytokines, chemokines, and growth factors in 1,175 individuals [95].
Methodological Approaches to Biomarker Validation
Metabolomics Validation Frameworks
The KORA F4 and SHIP-TREND-0 studies have established robust metabolomics validation workflows that leverage targeted metabolomics approaches. In a landmark metabolomics study investigating metabolite biomarkers for Metabolic Syndrome, KORA F4 served as the discovery cohort (N=2,815) while SHIP-TREND-0 functioned as the replication cohort (N=988) [92]. Serum samples from KORA F4 were measured with the AbsoluteIDQ p150 kit (BIOCRATES Life Sciences AG, Innsbruck, Austria) for quantification of 163 metabolites [92]. Quality control excluded metabolites with missing values ≥10%, median relative standard deviations (RSD) of quality control samples ≥25%, or fewer than 50% of measured sample values at or above the limit of detection, resulting in 121 high-quality metabolites for analysis [92].
Technical variations in metabolomics data were minimized using the TIGER non-parametric method, based on an adaptable ensemble learning architecture [92]. Metabolite concentrations were natural-log transformed and standardized to a mean of 0 and standard deviation of 1 to ensure comparability. Associations between metabolites and MetS were examined using multiple regression models adjusted for clinical and lifestyle covariates, with significance determined by Bonferroni correction [92]. This rigorous approach identified 56 MetS-specific metabolites that replicated across both cohorts, establishing a validated metabolomic signature of metabolic syndrome.
Statistical Modeling and Machine Learning Applications
Advanced statistical approaches form the cornerstone of biomarker validation in both cohorts. Multivariate regression models in SHIP-TREND-0 examined associations between cytokine concentrations and age, sex, BMI, season, and blood cell parameters, with standardization of effect estimates (βst) enabling comparison across analytes [95]. Machine learning algorithms have been increasingly employed, as demonstrated by researchers who built a machine learning algorithm to identify lipids correlated with disease in the MIDUS data set, probing biomarkers of metabolic syndrome [96].
The Boruta feature selection algorithm, a random forest-based wrapper method, has shown particular utility in handling high-dimensional clinical datasets. This algorithm iteratively compares feature importance with randomly permuted "shadow" features, effectively identifying all relevant predictors rather than just a minimal subset [97]. Such approaches are particularly valuable for addressing the complex, multifactorial nature of metabolic diseases and identifying robust biomarker panels across diverse populations.
Figure 1: Biomarker Validation Workflow in KORA and SHIP Studies
Key Validated Biomarker Findings for Metabolic Syndrome and Type 2 Diabetes
Inflammatory Biomarkers and Cytokine Patterns
SHIP-TREND-0 has generated a comprehensive cytokine atlas revealing profound associations between inflammatory mediators, age, sex, and metabolic parameters. The study quantified 47 plasma cytokines, chemokines, and growth factors in 1,175 individuals, revealing median concentrations ranging from 0.6 to 7,820 pg/mL across analytes [95]. Multivariate regression models identified strong associations between pro-inflammatory mediators and age, with higher levels of IL-6, IL-8, CXCL9, CXCL10, IL-12p40, CCL2, CCL4, CCL11, IL-27, FLT3LG, and TNFα significantly associated with increasing age [95]. The strongest age-associated effects were observed for CXCL9 (βst=0.4, p<0.001) and CXCL10 (βst=0.3, p<0.001) [95].
Sex differences represented another significant dimension of cytokine variation, with pronounced differences detected for CCL2, CCL3, CCL4, CCL11, CCL22, IL-12p40, IL-1RA, IL-18, IL-27, and TNFα [95]. CCL11 showed the strongest sex-specific effect (βst=-0.24, p<0.001), with lower levels in women compared to men [95]. Body mass index emerged as a critical modulator of inflammatory signaling, with seven cytokines and chemokines (CCL4, CCL22, CXCL10, IL-1RA, IL-18, IL-6, and TNFα) displaying higher concentrations with increasing BMI [95]. Among these, the strongest effects were observed for IL-1RA (βst=0.19, p<0.001), CCL4 (βst=0.16, p<0.001), and CXCL10 (βst=0.14, p<0.001) [95].
Table 2: Validated Inflammatory Biomarkers of Metabolic Dysfunction from SHIP-TREND-0
| Biomarker Category | Specific Analytes | Associations | Effect Sizes (βst) |
|---|---|---|---|
| Age-Associated | CXCL9, CXCL10 | Increasing age | 0.4, 0.3 (p<0.001) |
| Sex-Differentiated | CCL11, CCL22, IL-1RA | Sex differences | -0.24 for CCL11 (women |
| BMI-Associated | IL-1RA, CCL4, CXCL10 | Increasing BMI | 0.19, 0.16, 0.14 (p<0.001) |
| Obesity-Linked | CCL4, CCL22, CXCL10, IL-1RA | Obesity status | Significantly elevated in obesity |
| Blood Cell-Dependent | IL-6, IL-18, TNFα | Significance affected by blood cell counts | Confounding effect noted |
Metabolomic Signatures of Metabolic Syndrome
The cross-cohort metabolomics analysis identified and replicated 56 MetS-specific metabolites, providing a comprehensive view of metabolic dysregulation in metabolic syndrome [92]. Thirteen metabolites showed positive associations with MetS, including valine, leucine/isoleucine, phenylalanine, and tyrosine, indicating impaired catabolism of branched-chain and aromatic amino acids [92]. Conversely, 43 metabolites demonstrated negative associations, including glycine, serine, and 40 lipid species, suggesting accelerated glycine catabolism and complex lipid alterations [92].
The majority (89%) of MetS-specific metabolites were associated with low HDL-C, while only a minority (23%) were linked to hypertension, indicating component-specific metabolic signatures [92]. One lipid, lysoPC a C18:2, was negatively associated with MetS and all five of its components, suggesting that individuals with MetS and each risk factor had lower concentrations of this protective lipid compared to controls [92]. These findings highlight the power of cross-cohort validation for distinguishing robust metabolic biomarkers from cohort-specific artifacts.
Novel Subphenotypes and Cluster-Based Approaches
KORA F4 has enabled the validation of novel metabolic subphenotypes through cluster-based approaches. Researchers assigned 843 participants aged 61-82 years without T2D to six previously defined phenotype-based clusters derived from middle-aged populations [91]. The analysis revealed distinct cardiometabolic risk profiles, with clusters 1 and 2 exhibiting the lowest risk, while clusters 5 and 6 demonstrated the highest risk [91]. Type 2 diabetes risk was highest in clusters 3, 4, 5, and 6 compared with the low-risk cluster 2, with age- and sex-adjusted odds ratios between 3.6 and 34.0 [91].
The inflammatory load, derived from 73 biomarkers of subclinical inflammation using principal component analysis, was highest in the high-risk cluster 5 and lowest in cluster 2 [91]. However, adjustment for inflammatory load had only a minor impact on outcome differences between clusters, suggesting that inflammation alone does not fully explain the differential risk profiles [91]. These findings extend the knowledge of phenotype-based clusters to older populations and demonstrate the utility of subphenotyping for precision medicine approaches in metabolic disease.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Cohort Biomarker Studies
| Reagent/Platform | Specific Application | Function in Research | Example Use |
|---|---|---|---|
| AbsoluteIDQ p150/p180 Kits (BIOCRATES) | Targeted metabolomics | Simultaneous quantification of 163-180 metabolites | Metabolite profiling in KORA F4 and SHIP-TREND-0 [92] |
| Bead-based Multiplex Assays (Merck HCYTA-60K) | Cytokine/chemokine profiling | High-throughput quantification of 47 inflammatory mediators | Cytokine atlas generation in SHIP-TREND-0 [95] |
| LIAISON 25OH Vitamin D TOTAL Assay (DiaSorin) | Vitamin D status assessment | Precise measurement of 25-hydroxyvitamin D | Vitamin D-DSPN associations in KORA F4 [94] |
| FLEXMAP 3D Instrument | Multiplex immunoassays | Flexible bead-based array platform | Cytokine quantification in SHIP-TREND-0 [95] |
| Oral Glucose Tolerance Test (OGTT) | Glucose metabolism assessment | Diagnosis of glucose tolerance categories | Diabetes classification in KORA F4 [91] [94] |
| Michigan Neuropathy Screening Instrument (MNSI) | Peripheral neuropathy assessment | Standardized evaluation of DSPN | Neuropathy outcomes in KORA F4/FF4 [91] [94] |
Advanced Technical Protocols for Biomarker Studies
Cytokine Profiling Protocol (SHIP-TREND-0)
The cytokine atlas generated in SHIP-TREND-0 employed a rigorous multi-step protocol. Blood samples were collected following standardized phlebotomy procedures, with plasma separation via centrifugation and aliquoting for long-term storage at -80°C [95]. The bead-based multiplex immunoassay (Merck HCYTA-60K) was performed according to manufacturer specifications, utilizing antibody-conjugated magnetic beads for capture and biotinylated detection antibodies followed by streptavidin-phycoerythrin for signal amplification [95]. The FLEXMAP 3D instrument provided laser-based detection of bead identity (red laser) and analyte concentration (green laser) [95]. Data preprocessing included background subtraction, standard curve fitting for concentration interpolation, and quality control based on manufacturer recommendations [95].
Metabolomics Quality Control Framework (KORA F4)
The metabolomics quality control protocol implemented in KORA F4 exemplifies the rigorous approach necessary for reproducible biomarker studies. Samples were randomly distributed across 38 kit plates, with each plate including three quality control samples provided by the manufacturer and one zero sample (PBS) in addition to the individual samples [92]. Metabolites were excluded if they exhibited: (1) missing values ≥10%; (2) median relative standard deviations (RSD) of quality control samples ≥25%; or (3) fewer than 50% of measured sample values at or above the limit of detection [92]. This stringent quality framework resulted in 121 high-quality metabolites from the original 163 measured analytes, ensuring data reliability for subsequent association analyses [92].
Figure 2: Validated Biomarker Pathways in Metabolic Syndrome
Implications for Future Research and Precision Medicine
The validation of biomarkers in the KORA F4 and SHIP-TREND-0 cohorts provides critical insights for the future of metabolic disease research. Three key implications emerge from these studies:
First, the successful replication of metabolomic and inflammatory signatures across both cohorts demonstrates that robust, generalizable biomarkers can be identified despite geographical and methodological differences between study populations [95] [92]. This cross-validation approach is essential for distinguishing true biological signals from cohort-specific artifacts.
Second, the differential associations of biomarkers with specific metabolic syndrome components highlights the pathophysiological complexity of MetS and suggests that precision medicine approaches may benefit from component-specific biomarker panels rather than unified MetS signatures [92]. This is particularly evident in the finding that 89% of MetS-associated metabolites linked to low HDL-C, while only 23% associated with hypertension [92].
Third, the population-based nature of these cohorts provides essential reference ranges for biomarker interpretation in both research and clinical settings. The cytokine atlas from SHIP-TREND-0, for example, establishes population norms for 47 inflammatory mediators across age, sex, and BMI strata, enabling more meaningful interpretation of disease-associated alterations [95].
These insights collectively underscore the transformative potential of well-characterized population cohorts for advancing biomarker discovery, validation, and implementation in metabolic disease research. As the field progresses toward more personalized approaches to disease prevention and treatment, the foundational work conducted in the KORA and SHIP studies will continue to inform biomarker development and clinical translation.
Comparative Analysis of Traditional vs. Emerging Biomarker Panels
The escalating global prevalence of metabolic syndrome (MetS) and type 2 diabetes mellitus (T2DM) necessitates advanced strategies for early detection, risk stratification, and personalized therapeutic intervention. Biomarkers, as measurable indicators of biological processes or pathogenic responses, are indispensable tools in this endeavor [98]. This whitepaper provides a comparative analysis of traditional and emerging biomarker panels within the specific context of MetS and T2DM research and drug development. For decades, clinical practice has relied on traditional biomarkers—such as glycated hemoglobin (HbA1c), fasting glucose, and homeostatic model assessment of insulin resistance (HOMA-IR)—for diagnosis and monitoring. However, these often identify dysfunction only after significant metabolic deterioration has occurred [63] [99]. The emergence of novel biomarkers, including those identified through metabolomics, epitranscriptomics, and adipokine profiling, offers a paradigm shift. These markers promise to detect perturbations in biochemical pathways at a pre-clinical stage, thereby enabling earlier intervention and a more nuanced understanding of disease heterogeneity [15] [62] [100]. This document delineates the characteristics, advantages, and limitations of both biomarker classes, summarizes quantitative data in structured tables, details essential experimental protocols, and visualizes key pathways to equip researchers and drug development professionals with a comprehensive technical guide.
Biomarker Fundamentals and Classification
Biomarkers are objectively measured characteristics evaluated as indicators of normal biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention [98]. The US FDA-NIH Biomarker Working Group's BEST (Biomarkers, EndpointS, and other Tools) resource categorizes biomarkers primarily as either disease-associated or drug-related. Key categories relevant to MetS and T2DM include:
- Susceptibility/Risk Biomarkers: Identify the potential for developing a disease (e.g., genetic predisposition).
- Diagnostic Biomarkers: Detect or confirm the presence of a disease.
- Prognostic Biomarkers: Identify the likelihood of a clinical event or disease progression.
- Monitoring Biomarkers: Serially measured to assess disease status or evidence of exposure to a medical product.
- Predictive Biomarkers: Identify individuals more likely to experience a favorable or unfavorable effect from a specific therapeutic intervention.
- Safety Biomarkers: Measured before or after an exposure to indicate the likelihood of an adverse event [98].
This framework is essential for contextualizing the application of both traditional and emerging biomarkers in the research and development pipeline.
Analysis of Traditional Biomarker Panels
Traditional biomarkers form the cornerstone of current clinical practice for MetS and T2DM. They are widely available, relatively inexpensive, and their interpretation is supported by decades of clinical evidence.
Table 1: Core Traditional Biomarkers in Metabolic Syndrome and Type 2 Diabetes Research
| Biomarker | Primary Mechanism/Origin | Normal Range | Level in Disease State | Clinical Utility | Key Limitations |
|---|---|---|---|---|---|
| HbA1c | Glycation of hemoglobin; reflects average blood glucose over ~3 months [63] | <5.7% [63] | ≥6.5% (Diabetes) [63] | Gold standard for long-term glycemic control [62] | Affected by hemoglobin variants, red cell lifespan, CKD [63] |
| HOMA-IR | Derived from fasting glucose and insulin levels; assesses insulin resistance [63] | <2.5 [63] | Elevated (>2.9) [63] | Estimates hepatic and systemic insulin resistance [63] | No universal cut-off; accuracy declines in lean T2D/compromised pancreatic function [63] |
| Fasting Insulin | Secreted by pancreatic beta cells [63] | 2–25 µIU/mL [63] | Elevated in early T2D/MetS [63] | Direct measure of beta-cell output [63] | Limited utility in insulin-treated patients; paradoxical results in some diabetics [63] |
| Fasting Glucose | Circulating blood glucose after fast | <100 mg/dL [99] | ≥126 mg/dL (Diabetes) [99] | Direct measure of glycemic state | High biological variability; single snapshot [99] |
| HDL Cholesterol | Liver; reverse cholesterol transport [63] | >40/50 mg/dL (M/F) [99] | Low level is a MetS criterion [99] | Cardiovascular risk assessment | Does not capture functional quality of HDL particles [99] |
| Triglycerides (TG) | Liver, adipose tissue [63] | <150 mg/dL [63] | Elevated (>150 mg/dL) [63] | Marker of lipid dysregulation & insulin resistance [63] | Lack of specificity; influenced by medications [63] |
| CRP | Liver (hepatocytes); marker of inflammation [63] | <1 mg/L (Low risk) [63] | >3 mg/L (High risk) [63] | Indicator of systemic inflammation & CV risk [63] | Lack of specificity; limited predictive value alone [63] |
Limitations of Traditional Biomarkers
While foundational, traditional biomarkers possess significant constraints for modern precision medicine. They often provide a "snapshot" in time, missing dynamic physiological changes, and lack the sensitivity to detect the earliest metabolic disruptions [98] [99]. Furthermore, syndromes like MetS are highly heterogeneous, and conventional panels fail to capture this diversity, limiting their prognostic and predictive power for individual patients and complicating patient stratification in clinical trials [99].
Analysis of Emerging Biomarker Panels
Emerging biomarkers, discovered through advanced omics technologies, offer a deeper, more systems-level view of the pathophysiological processes underlying MetS and T2DM.
Table 2: Key Emerging Biomarkers in Metabolic Syndrome and Type 2 Diabetes Research
| Biomarker Category | Specific Examples | Mechanism/Pathway | Potential Clinical Utility | Key Advantages |
|---|---|---|---|---|
| Metabolomics | Branched-Chain Amino Acids (BCAAs: valine, leucine, isoleucine) [99] | Predictors of insulin resistance; disruption in mitochondrial metabolism [99] | Early risk prediction before hyperglycemia [99] | Reveals pre-clinical pathway disruptions; enables subtype stratification [99] |
| Betaine, Alpha-Linolenic Acid [101] | Betaine: homocysteine metabolism; ALA: inflammation/insulin sensitivity [101] | Predicting progression to T2DM [101] | Non-invasive detection from blood/urine [101] | |
| Lipid Species (Ceramides, LysoPCs) [99] | Disruption in lipid metabolism linked to T2DM/CVD risk [99] | Assessing specific cardiovascular risk | More specific than traditional lipid panels [99] | |
| Epitranscriptomics | m6A (N6-methyladenosine) & Regulators (FTO, METTL3) [100] | Reversible mRNA modification regulating stability/translation; dysregulated in insulin resistance [100] | Novel diagnostic markers; monitoring complications [100] | Dynamic, reversible measure of cellular stress & gene regulation [100] |
| Pseudouridine (Ψ) [100] | Modified nucleotide in non-coding RNAs; associated with oxidative stress [100] | Biomarker for diabetic complications (retinopathy, nephropathy) [100] | Accessible via commercial kits; potential for early complication detection [100] | |
| Mitochondrial Peptides | Humanin, MOTSc [102] | Regulate insulin sensitivity, beta-oxidation, and beta-cell survival [102] | Assessing mitochondrial function & diabetes progression [102] | Links mitochondrial health directly to metabolic regulation [102] |
| Oxidative Stress | 8-isoprostane, GSH/GSSG Ratio [102] | 8-isoprostane: lipid peroxidation; GSH/GSSG: redox balance [102] | Quantifying oxidative stress burden, linked to CVD risk [102] | Direct measure of a key pathophysiological driver [102] |
| Inflammation | IL-1β, MCP-1 [102] | Pro-inflammatory cytokines driving insulin resistance & beta-cell dysfunction [102] | Stratifying patients for anti-inflammatory therapies [102] | More specific inflammatory pathways than CRP [102] |
Integrated Panels and Digital Biomarkers
The future of biomarker science lies in multi-analyte panels that combine traditional and emerging markers to achieve higher sensitivity and specificity [103] [104]. Additionally, the field of digital biomarkers—objective, quantifiable physiological and behavioral data collected by portable devices—is gaining traction. These can provide continuous, longitudinal data on metrics like physical activity and sleep patterns, offering real-world context to molecular findings, though they face challenges in data standardization and regulatory approval [98].
Experimental Protocols for Biomarker Analysis
Untargeted Metabolomics Workflow for Serum/Plasma
This protocol is adapted from discovery-based studies identifying metabolites associated with MetS and T2DM [101] [99].
Sample Collection and Preparation:
- Collect plasma or serum samples from participants after an overnight fast. Immediately aliquot and flash-freeze in liquid nitrogen, storing at -80°C.
- For analysis, thaw samples on ice. Precipitate proteins by adding cold methanol (typically 3:1 methanol-to-sample ratio). Vortex and centrifuge at high speed (e.g., 14,000 × g, 10 min, 4°C).
- Transfer the supernatant containing metabolites to a new vial and dry under a gentle stream of nitrogen or using a vacuum concentrator.
- Reconstitute the dried extract in a suitable solvent for the analytical platform (e.g., water/acetonitrile).
Instrumental Analysis - Liquid Chromatography-Mass Spectrometry (LC-MS):
- Chromatography: Use a reversed-phase C18 column (e.g., 2.1 x 100 mm, 1.8 µm) with a binary solvent system. Mobile Phase A: Water with 0.1% formic acid; Mobile Phase B: Acetonitrile with 0.1% formic acid. Apply a linear gradient from 2% B to 98% B over 15-20 minutes.
- Mass Spectrometry: Employ a high-resolution mass spectrometer (e.g., Q-TOF or Orbitrap) operating in both positive and negative electrospray ionization (ESI) modes to capture a broad metabolite profile. Data is acquired in data-dependent acquisition (DDA) or MS^E^ mode to collect both precursor and fragment ion information.
Data Processing and Statistical Analysis:
- Use software (e.g., XCMS, Progenesis QI) for peak picking, alignment, and normalization. Internal standards are used to control for technical variability.
- Export the peak intensity table for statistical analysis. Perform multivariate analyses like Principal Component Analysis (PCA) and Orthogonal Projections to Latent Structures-Discriminant Analysis (OPLS-DA) to identify metabolites discriminating sample groups (e.g., Healthy vs. MetS).
- Confirm metabolite identity by matching fragmentation spectra (MS/MS) to authentic standards in databases (e.g., HMDB, METLIN). Validate significant findings with targeted assays.
Analysis of Epitranscriptomic Modifications (m6A)
This protocol outlines the key steps for quantifying the m6A modification and its regulatory proteins in blood, a promising emerging biomarker [100].
RNA Isolation and Quantification:
- Extract total RNA from whole blood or PBMCs using a commercial kit with DNase treatment to remove genomic DNA contamination. Assess RNA integrity and concentration using an Agilent Bioanalyzer or similar system (RIN > 8.0 is ideal).
Quantification of m6A Levels:
- Option 1 (Global m6A Level): Use a commercial m6A RNA Methylation Quantification Kit (Colorimetric or ELISA-based). This method provides a global measure of m6A content in total RNA but does not give site-specific information.
- Option 2 (Site-Specific): Perform m6A-specific methylated RNA immunoprecipitation (MeRIP) followed by qRT-PCR or sequencing (MeRIP-seq). RNA is fragmented and immunoprecipitated with an anti-m6A antibody. The enriched fragments are then used to quantify methylation at specific gene loci via qRT-PCR or sequenced for a transcriptome-wide map.
Analysis of m6A Regulator Expression:
- Isulate total protein or mRNA from samples.
- To measure expression levels of writers (e.g., METTL3), erasers (e.g., FTO), and readers, use techniques like:
- Quantitative RT-PCR (qRT-PCR): To measure mRNA expression levels.
- Western Blotting or Enzyme-Linked Immunosorbent Assay (ELISA): To measure protein expression levels.
Visualization of Biomarker Pathways and Workflows
Metabolic Dysregulation in Type 2 Diabetes
This diagram illustrates the interconnected pathways and key biomarkers in the progression from insulin resistance to T2DM complications.
Experimental Metabolomics Workflow
This flowchart outlines the key steps in an untargeted metabolomics study for biomarker discovery.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| High-Resolution LC-MS System | Untargeted profiling and identification of small molecule metabolites in biofluids [101] [99]. | Discovery of novel metabolite associations with MetS (e.g., BCAAs, betaine) [101] [99]. |
| m6A RNA Methylation Quantification Kit | Colorimetric or ELISA-based global quantification of N6-methyladenosine in total RNA [100]. | Assessment of global epitranscriptomic changes in blood samples from T2DM patients vs. controls [100]. |
| Anti-m6A Antibody | Immunoprecipitation of methylated RNA fragments for MeRIP-qPCR or MeRIP-seq [100]. | Mapping site-specific m6A modifications on transcripts relevant to insulin signaling [100]. |
| Commercial ELISA Kits (e.g., FTO, METTL3, Adiponectin) | Quantitative measurement of specific protein biomarkers in serum, plasma, or cell lysates [15] [100]. | Validating expression levels of epitranscriptomic regulators or adipokines in patient cohorts [15] [100]. |
| QTRAP or TQ-MS System | Sensitive and specific targeted quantification of known metabolites or lipids (e.g., ceramides, BCAAs) [99]. | Validation of candidate biomarker panels from untargeted studies in large cohorts. |
| RNA Integrity Number (RIN) Analysis | Assessment of RNA quality to ensure reliability of downstream transcriptomic/epitranscriptomic analysis [100]. | Quality control step for RNA isolated from blood prior to m6A analysis [100]. |
Multi-Metabolite Models for Major Adverse Cardiovascular Event Prediction
Major Adverse Cardiovascular Events (MACE), including cardiovascular mortality, non-fatal myocardial infarction, and non-fatal stroke, represent a significant global health burden, particularly among individuals with type 2 diabetes (T2D) who represent a high-risk population [105]. Existing cardiovascular risk prediction models have room for improvement in this vulnerable group. The integration of metabolomic biomarkers—comprehensive small-molecule metabolite profiles—offers a promising avenue for enhancing the precision of 10-year MACE prediction by capturing early pathophysiological changes on a molecular level [105] [106]. Multi-metabolite models leverage high-throughput technologies and advanced computational methods to identify biomarker patterns that reflect disturbances in key biological pathways, providing insights beyond traditional risk factors. This technical guide explores the development, validation, and application of these models within the context of metabolic syndrome and T2D research, providing drug development professionals and researchers with detailed methodologies and analytical frameworks.
Key Metabolite Panels and Performance
Recent large-scale studies have identified specific metabolite panels that significantly enhance MACE prediction when integrated with established risk models. The following table summarizes quantitatively validated metabolite panels and their performance characteristics.
Table 1: Validated Multi-Metabolite Panels for MACE Risk Prediction
| Study & Cohort | Key Metabolite Panels Identified | Prediction Model/Context | Performance Improvement |
|---|---|---|---|
| Xie et al. (2025) [105]UK Biobank & ESTHER(N=10,257 & 1,039 with T2D) | 7 metabolomic biomarkers: Albumin, Omega-3-fatty-acids-to-total-fatty-acids ratio (males), Lactate (females), and four other sex-specific metabolites. | Enhancement of the SCORE2-Diabetes model for 10-year MACE risk. | Internal Validation (UKB): C-index increased from 0.660 to 0.678 (P=0.037).External Validation (ESTHER): C-index increased by +0.043 (P=0.011). |
| Biomarker Study (2024) [107]Case-Control(N=57) | 8-feature panel: Palmitic amide, Oleic acid, 138-pos (metabolomic feature), Phosphatidylcholine, Linoleic acid, Age, Direct bilirubin, Inorganic phosphate. | Machine learning model for CVD risk assessment. | Achieved a high CVD risk assessment accuracy of 0.91. |
| Multi-omics Study (2025) [108]3 Independent Cohorts(N=443) | 5-metabolite panel: Cholesteryl sulphate, Azelaic acid, Tryptophan, Arabinofuranosyluracil, TMAO, ADMA, LPC18:2, Tartaric acid, L-citrulline, L-proline, Purine, Sorbitol, 2-aminoadipic acid. | Diagnostic model for Coronary Atherosclerosis (CA) severity. | Blinded Validation: AUC 0.821–0.898 for CA occurrence; 0.649–0.849 for CA severity. |
| LAA Prediction Study (2023) [109]Training n=287, Test n=72 | 27 shared features across models, including clinical traits (BMI, smoking, medications) and metabolites in aminoacyl-tRNA biosynthesis and lipid metabolism. | Logistic Regression model combining clinical factors and metabolites for Large-Artery Atherosclerosis (LAA). | External Validation: AUC of 0.92 with 62 features; AUC of 0.93 with 27 key shared features. |
These studies consistently demonstrate that integrating multiple metabolites with clinical variables yields superior predictive performance compared to models using traditional risk factors alone. The improved performance, validated both internally and externally, underscores the clinical potential of these panels.
Detailed Experimental Protocols
The development of a robust multi-metabolite model involves a multi-stage process, from sample collection to statistical validation. The workflow below outlines the key stages.
Sample Preparation and Metabolite Quantification
Accurate metabolite measurement is foundational and typically follows one of two high-throughput platforms:
Nuclear Magnetic Resonance (NMR) Spectroscopy: As utilized in the UK Biobank and ESTHER studies, this platform quantifies a wide range of metabolites including lipids, fatty acids, and amino acids [105]. The protocol involves:
- Sample Collection: Collecting plasma or serum samples from fasting participants and storing them at -80°C.
- High-Throughput Processing: Using automated platforms (e.g., Nightingale Health) to simultaneously quantify up to 249 metabolites.
- Data Output: Providing absolute concentrations or relative ratios of metabolites. This method is noted for its high reproducibility and standardization, making it suitable for large-scale clinical applications [105].
Mass Spectrometry (MS)-Based Metabolomics: Often used for deeper biomarker discovery, this includes untargeted and targeted approaches [108] [107].
- Untargeted Workflow (UHPLC-MS/MS):
- Protein Precipitation: Mixing plasma (e.g., 100 µL) with ice-cold methanol (e.g., 400 µL of 80% concentration), vortexing, and incubating on ice.
- Centrifugation: Separating supernatant at high speed (e.g., 15,000 g) and 4°C for 20 minutes.
- Dilution & Analysis: Diluting the supernatant and analyzing it using UHPLC (e.g., Hypersil GOLD C18 column) coupled to a high-resolution mass spectrometer (e.g., Orbitrap Q Exactive HF) [107].
- Quality Control (QC): Interspersing pooled QC samples every 10-15 analytical runs to monitor instrument stability and data quality [108] [107].
- Targeted Workflow: Using kits (e.g., Absolute IDQ p180 kit) or multiple reaction monitoring (MRM) on platforms like QTRAP 5500 to validate and precisely quantify a pre-defined set of candidate biomarkers [108] [109].
- Untargeted Workflow (UHPLC-MS/MS):
Data Preprocessing and Statistical Analysis
Raw data must be processed before model building:
- Data Imputation: Handling missing values using methods like random forest imputation (
missForestR package) or mean imputation for low missing rates [105] [110]. - Transformation and Scaling: Natural log-transformation is often applied to approximate normal distributions, followed by scaling to standard deviation units to enable cross-metabolite comparisons [105] [111].
- Feature Selection: Employing regularized regression techniques like Least Absolute Shrinkage and Selection Operator (LASSO) to identify the most predictive metabolites from a high-dimensional dataset. A bootstrap LASSO approach (e.g., 1000 resamples) can be used to select features that are stable across iterations [105] [110].
- Model Derivation and Validation: The dataset is typically split into a derivation/training set (e.g., 70%) and an internal validation set (e.g., 30%). The model's performance is then tested on an external validation cohort from a separate study to ensure generalizability [105]. Predictive performance is commonly evaluated using Harrell's C-index (for survival models) or the Area Under the Receiver Operating Characteristic Curve (AUC) [105] [108].
Analytical and Computational Workflows
Machine learning (ML) is instrumental in building and interpreting multi-metabolite models. The analytical pipeline integrates feature selection, model training, and validation.
Machine Learning for Biomarker Discovery and Prediction
Several ML algorithms have been successfully applied:
- Logistic Regression (LR) with Regularization: Often provides a strong, interpretable baseline. LASSO regularization is particularly valuable for feature selection in high-dimensional metabolomic data [109].
- Tree-Based Ensemble Methods: Algorithms like XGBoost, Random Forest, and KTBoost (Kernel-Tree Boosting) handle complex, non-linear relationships effectively. For instance, KTBoost demonstrated superior performance in a T2DM prediction study, achieving an accuracy of 0.938 and an AUC of 0.965 [110].
- Model Interpretation with Explainable AI (XAI): The SHapley Additive exPlanations (SHAP) method is critical for translating "black box" models into actionable insights. It quantifies the contribution of each metabolite to an individual's predicted risk, revealing key biomarkers. For example, high phenylactate and taurine, alongside low cysteine and aspartate, were strongly associated with T2DM presence in a KTBoost model [110].
Biological Pathways and Signaling Networks
Metabolites identified in predictive panels are not isolated entities; they are interconnected components of critical biological pathways. The diagram below maps these relationships.
The disrupted pathways highlighted above are central to the pathophysiology of cardiovascular disease in metabolic syndrome and T2D:
- Lipid Metabolism Dysregulation: Alterations in glycerophospholipid metabolism and the biosynthesis of unsaturated fatty acids are strongly implicated [107]. Metabolites like linoleic acid, oleic acid, phosphatidylcholine, and the omega-3-fatty-acids-to-total-fatty-acids ratio are frequently identified in panels, reflecting perturbations in membrane integrity and energy metabolism [105] [107].
- Gut Microbiome-Derived Metabolites: Molecules such as Trimethylamine-N-oxide (TMAO) and phenylacetylglutamine (PAGln) have pro-atherogenic effects and are consistently linked to atherosclerosis severity and MACE risk [108] [109].
- Amino Acid and Energy Metabolism: Shifts in levels of tryptophan, branched-chain amino acids (BCAAs), lactate, and albumin indicate underlying inefficiencies in energy production, insulin resistance, and cellular stress responses, which are hallmarks of T2D and metabolic syndrome [105] [106].
Essential Research Reagents and Platforms
The following table catalogs key reagents, kits, and instrumentation essential for conducting metabolomic studies for MACE prediction.
Table 2: Key Research Reagent Solutions for Metabolomic Biomarker Discovery
| Reagent / Platform | Specific Function | Application Context |
|---|---|---|
| Nightingale Health NMR Platform | High-throughput quantification of ~249 metabolites (lipids, fatty acids, amino acids, etc.) from plasma/serum. | Large-scale cohort phenotyping; clinical translation due to cost-effectiveness and standardization [105]. |
| Absolute IDQ p180 Kit (Biocrates) | Targeted metabolomics kit for the quantitative analysis of up to 188 metabolites from several compound classes. | Precise, standardized quantification for biomarker validation studies [109]. |
| UHPLC-MS/MS Systems | Ultra-High Performance Liquid Chromatography coupled to tandem Mass Spectrometry for separation and identification of metabolites. | Untargeted and targeted metabolomic discovery and validation [108] [107]. |
| Hypersil GOLD C18 Column | Reverse-phase UHPLC column for chromatographic separation of complex metabolite mixtures. | Essential for resolving metabolites in biological samples prior to mass spec detection [107]. |
| TripleTOF 5600+/Q Exactive HF | High-resolution mass spectrometers for accurate mass measurement and data-dependent MS/MS fragmentation. | Untargeted metabolomic profiling for biomarker discovery [108] [107]. |
| QC Samples (Pooled Plasma) | Quality control samples created by pooling aliquots from all study samples. | Monitored throughout analytical batches to ensure data consistency and instrument stability [107]. |
Sodium-glucose cotransporter-2 inhibitors (SGLT2is) and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) represent transformative therapeutic classes for type 2 diabetes (T2DM) and metabolic syndrome. Beyond glycemic control, these agents demonstrate pleiotropic effects on cardiovascular, renal, and metabolic health through distinct yet complementary mechanisms. This whitepaper examines the biomarker profiles associated with therapeutic responses to SGLT2is and GLP-1 RAs, providing a technical framework for researchers and drug development professionals. We synthesize current evidence on quantitative biomarker changes, delineate underlying molecular pathways, and present standardized experimental protocols for assessing treatment efficacy. Our analysis reveals that biomarker-guided approaches enable precise patient stratification, optimized treatment intensification, and comprehensive risk mitigation in metabolic disease management, advancing the paradigm toward personalized therapeutics in endocrinology and cardiometabolic medicine.
Metabolic syndrome and T2DM represent interconnected pathological states characterized by complex dysregulation across multiple organ systems. Biomarkers—measurable indicators of biological processes—provide critical windows into disease presence, severity, and therapeutic response [5]. Traditional biomarkers like hemoglobin A1c (HbA1c) and fasting plasma glucose have long anchored diabetes diagnosis and management, yet they offer limited insight into the underlying pathophysiological processes driving disease progression and complication development [5].
The evolving biomarker landscape now encompasses inflammatory mediators, adipokines, metabolic profiles, and organ-specific stress markers that collectively provide a multidimensional view of metabolic health [5] [71]. Growth differentiation factor 15 (GDF-15), for instance, has emerged as a stress-responsive biomarker elevated in obesity and diabetes, with levels varying significantly by demographic factors including age, gender, and ethnicity [5]. Similarly, novel biomarkers reflecting mitochondrial dysfunction, oxidative stress, and tissue-specific injury are refining our understanding of metabolic disease heterogeneity [71].
Within this context, SGLT2is and GLP-1 RAs have demonstrated benefits extending far beyond glucose lowering, including cardiovascular risk reduction, weight management, and organ protection [112] [113] [114]. The therapeutic responses to these agents are quantifiable through specific biomarker signatures that reflect their distinct mechanisms of action and enable precision targeting to patient profiles. This technical guide examines the biomarker evidence base for these drug classes, providing methodologies for response assessment and contextualizing findings within the broader framework of biomarker-driven metabolic medicine.
Quantitative Biomarker Responses to SGLT2 Inhibitors and GLP-1 Receptor Agonists
Glycemic and Metabolic Parameters
SGLT2is and GLP-1 RAs exert complementary effects on glycemic control and metabolic parameters, as quantified in recent meta-analyses and clinical trials. The table below summarizes key biomarker changes associated with these therapeutic classes.
Table 1: Biomarker Responses to SGLT2 Inhibitors and GLP-1 Receptor Agonists
| Biomarker Category | Specific Biomarker | SGLT2 Inhibitor Effect | GLP-1 RA Effect | References |
|---|---|---|---|---|
| Glycemic Control | HbA1c (%) | -0.5 to -0.7 | -0.3 to -1.5 | [112] |
| Fasting Plasma Glucose (mg/dL) | -15 to -25 | -6.5 | [112] [115] | |
| Body Composition | Body Weight (kg) | -2 to -3 | -7.1 | [115] |
| Waist Circumference (cm) | -2 to -4 | -5.7 | [115] | |
| Fat Mass (kg) | -1.5 to -2.5 | -2.9 | [115] | |
| Lean Mass (kg) | -0.5 to -1.5 | -1.3 | [115] | |
| Cardiovascular | Systolic BP (mmHg) | -3 to -5 | -4.0 | [115] |
| Diastolic BP (mmHg) | -1 to -2 | -1.1 | [115] | |
| NT-proBNP | Significant reduction | Not reported | [116] [117] | |
| Lipid Profile | LDL Cholesterol (mg/dL) | -3 to -5 | -4.8 | [115] |
| Triglycerides (mg/dL) | -10 to -20 | -13.4 | [115] | |
| HDL Cholesterol (mg/dL) | +1 to +3 | -0.1 (NS) | [115] |
GLP-1 RAs demonstrate particularly robust effects on weight-related parameters, with lifestyle modification combined with GLP-1 RAs resulting in a mean weight loss of 7.13 kg compared with control groups (MD: -7.13 kg, 95% CI: -9.02, -5.24, P < 0.001) [115]. Longer treatment duration, use of specific agents like semaglutide or tirzepatide, weekly dosing, and studies conducted in North America were associated with more pronounced weight loss effects [115].
Inflammatory and Organ Stress Biomarkers
Both drug classes demonstrate significant effects on inflammatory biomarkers and organ stress markers, though through potentially distinct mechanisms.
Table 2: Inflammatory and Organ Stress Biomarker Responses
| Biomarker Category | Specific Biomarker | SGLT2 Inhibitor Effect | GLP-1 RA Effect | References |
|---|---|---|---|---|
| Systemic Inflammation | CRP | Moderate reduction | Significant reduction (SMD: -0.63) | [118] [117] |
| TNF-α | Not reported | Significant reduction (SMD: -0.92) | [118] | |
| IL-6 | Reduction (cardiac patients) | Significant reduction (SMD: -0.76) | [118] [117] | |
| IL-1β | Not reported | Significant reduction (SMD: -3.89) | [118] | |
| Adipokines | Leptin | Not reported | Significant reduction (SMD: -0.67) | [118] |
| Adiponectin | Not reported | Significant increase (SMD: 0.69) | [118] | |
| Cardiac Stress | Troponin I | Significant reduction | Not reported | [117] |
| hs-CRP | Significant reduction | Not reported | [117] |
A comprehensive meta-analysis of 52 randomized controlled trials (n=4,734) with a median follow-up of 24 weeks demonstrated that GLP-1 RAs produce significant reductions across multiple inflammatory markers, including CRP, TNF-α, IL-6, and IL-1β, while increasing adiponectin levels [118]. These anti-inflammatory effects may contribute to the cardiovascular and metabolic benefits observed with GLP-1 RA therapy.
SGLT2is show particular efficacy in reducing cardiac stress biomarkers in patients with heart failure following acute myocardial infarction, with significant improvements in NT-proBNP, troponin I, and hs-CRP levels compared to conventional treatment (P < 0.001) [116] [117].
Mechanistic Insights: Signaling Pathways and Molecular Mechanisms
GLP-1 Receptor Agonists: Multimodal Actions
GLP-1 RAs exert their effects through multiple interconnected pathways, engaging both metabolic and anti-inflammatory mechanisms.
Diagram 1: GLP-1 Receptor Agonist Mechanisms of Action. GLP-1 RAs activate multiple pathways through the GLP-1 receptor, resulting in metabolic improvements, anti-inflammatory effects, and direct cellular actions that collectively contribute to their therapeutic benefits. The color coding indicates: yellow (receptor activation), green (biological processes), and red (clinical outcomes).
The biological impact of GLP-1 RAs extends to cancer risk modulation through multiple mechanistic pathways, including direct effects on tumor cell metabolism and proliferation, modulation of immune responses in the tumor microenvironment, and regulation of inflammatory signaling networks [119]. These agents demonstrate heterogeneous effects across different tumor types, with evidence suggesting protective effects against hepatocellular and prostate cancers, while relationships with thyroid and pancreatic cancers remain complex and require further investigation [119].
SGLT2 Inhibitors: Metabolic Reprogramming and Cardiac Protection
SGLT2is operate through distinct pathways that confer significant cardiometabolic benefits.
Diagram 2: SGLT2 Inhibitor Mechanisms of Action. SGLT2 inhibitors primarily act through renal mechanisms that trigger cascading metabolic, hemodynamic, and cardiac effects. The multifaceted actions explain their robust cardiovascular benefits, particularly in heart failure. The color coding indicates: yellow (drug action), green (biological processes), and red (clinical outcomes).
The cardioprotective effects of SGLT2is are particularly notable in patients with heart failure following acute myocardial infarction, where they significantly improve left ventricular ejection fraction (LVEF) and reduce cardiac stress markers including NT-proBNP, troponin I, and hs-CRP levels compared to conventional treatment (P < 0.001) [116] [117]. Lower baseline LVEF and higher NT-proBNP levels may predict better therapeutic response, suggesting their utility in personalized treatment strategies [117].
Experimental Protocols for Biomarker Assessment
Standardized Methodology for Inflammatory Biomarker Analysis
The assessment of inflammatory biomarkers in response to GLP-1 RAs follows rigorous standardized protocols established in recent meta-analyses.
Study Design Considerations:
- Trial Selection: Randomized controlled trials (RCTs) with parallel-group or crossover designs
- Population: Adults with Type 2 Diabetes Mellitus
- Intervention: GLP-1 RA therapy (any agent, dose, or duration)
- Comparator: Placebo, active control, or conventional diabetes care
- Follow-up Duration: Minimum 12 weeks to assess meaningful biomarker changes
Biomarker Measurement Protocols:
- Blood Collection: Fasting venous blood samples (5 mL) collected in EDTA tubes
- Processing: Centrifugation at 2,800 rpm for 15 minutes within 30 minutes of collection
- Storage: Serum/plasma aliquots maintained at -80°C until analysis
- Analytical Methods:
- CRP: High-sensitivity immunoassay (hs-CRP)
- TNF-α, IL-6, IL-1β: Multiplex cytokine array or ELISA
- Leptin/Adiponectin: ELISA with appropriate controls
- PAI-1, MCP-1: Commercial ELISA kits with validated reproducibility
Statistical Analysis Framework:
- Calculation of standardized mean differences (SMD) with 95% confidence intervals
- Assessment of heterogeneity using I² statistic (with values >50% indicating substantial heterogeneity)
- Random-effects models to account for clinical and methodological diversity
- Sensitivity analyses to evaluate the influence of individual studies
- Publication bias assessment through funnel plots and Egger's test
This methodological approach was implemented in a comprehensive meta-analysis of 52 RCTs (n=4,734) that demonstrated significant reductions in multiple inflammatory biomarkers with GLP-1 RA therapy [118].
Cardiac Function Assessment in Heart Failure Studies
The evaluation of SGLT2 inhibitor efficacy in heart failure post-myocardial infarction requires comprehensive cardiac assessment protocols.
Echocardiography Protocol:
- Equipment: Color Doppler echocardiography system (e.g., Vivid E95, GE)
- Probe Frequency: 3.0 MHz for optimal resolution
- Patient Positioning: Left lateral decubitus position
- Standard Views: Apical four-chamber, parasternal long-axis
- Measured Parameters:
- Left ventricular ejection fraction (LVEF) using modified Simpson's biplane method
- Left ventricular end-diastolic dimension (LVEDD)
- Left ventricular end-systolic dimension (LVESD)
- Left ventricular end-diastolic volume (LVEDV)
- Left ventricular mass (LVM) calculated via area-length method
- Left ventricular mass index (LVMI) and remodeling index (LVRI)
Serum Biomarker Analysis:
- Sample Collection: Fasting venous blood (5 mL) in EDTA tubes
- Processing: Centrifugation at 2,800 rpm for 15 minutes, serum separation
- Analytical Methods:
- NT-proBNP: Enzyme-linked immunosorbent assay (ELISA, ab263877, Abcam)
- Troponin I: Automated biochemical analyzer (BS-280, Mindray)
- hs-CRP and IL-6: Automated biochemical analyzer with high-sensitivity assays
Efficacy Endpoints:
- Primary: Change in LVEF from baseline to follow-up (typically 3 months)
- Secondary: Changes in NT-proBNP, troponin I, hs-CRP, and functional status
- Composite endpoints incorporating both echocardiographic and biomarker improvements
This protocol was successfully implemented in a retrospective cohort study of 315 patients with HF post-AMI, which demonstrated significant improvements in cardiac function parameters with SGLT2 inhibitor therapy [117].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Biomarker and Mechanistic Studies
| Category | Specific Reagent/Assay | Application | Key Features |
|---|---|---|---|
| Biomarker Analysis | High-sensitivity CRP Immunoassay | Inflammation quantification | Detection limit <0.1 mg/L, wide dynamic range |
| Multiplex Cytokine Panels (TNF-α, IL-6, IL-1β) | Parallel inflammatory marker assessment | High-throughput, minimal sample volume | |
| ELISA for Adipokines (Leptin, Adiponectin) | Metabolic status evaluation | Species-specific variants available | |
| NT-proBNP ELISA (ab263877, Abcam) | Cardiac stress assessment | Heart failure monitoring, prognostic value | |
| Cell Signaling Studies | Phospho-Specific Antibodies for Insulin Signaling | Mechanism of action studies | p-AKT, p-IRS1, pathway activation |
| GLP-1 Receptor Antibodies | Receptor localization and expression | Tissue distribution studies | |
| SGLT2 Transport Assays | Drug-target engagement | Functional activity measurement | |
| In Vivo Models | Methionine Choline-Deficient Diet Models | MAFLD/MASH research | Metabolic dysfunction-associated liver disease |
| db/db Mice or ZDF Rats | Type 2 diabetes studies | Leptin receptor deficiency, progressive disease | |
| Myocardial Infarction-HF Models | Cardiac function assessment | Coronary artery ligation, ischemia-reperfusion | |
| Analytical Instruments | Color Doppler Echocardiography (Vivid E95, GE) | Cardiac structure and function | 3.0 MHz probe, tissue Doppler capability |
| Automated Hematology Analyzer (BC-5000, Mindray) | Complete blood count | Leukocyte differential, research mode | |
| Automated Biochemical Analyzer (BS-280, Mindray) | Serum chemistry panels | hs-CRP, troponin, metabolic parameters |
The selection of appropriate research reagents is critical for generating reproducible, translatable data in metabolic disease research. Standardization across laboratories through consistent use of validated assays and model systems enhances the comparability of findings and accelerates therapeutic development.
Clinical Applications and Biomarker-Guided Treatment Strategies
Patient Stratification and Personalized Treatment Approaches
Biomarker profiles enable precise patient stratification for optimized therapeutic selection:
- High Inflammatory Burden: Patients with elevated CRP, IL-6, and TNF-α may derive particular benefit from GLP-1 RAs, given their significant anti-inflammatory effects [118]
- Cardiac Dysfunction: Individuals with reduced LVEF and elevated NT-proBNP show robust response to SGLT2 inhibitors, especially following acute myocardial infarction [117]
- Prediabetes Progression: Early intervention with either drug class may delay T2DM onset, with biomarkers like HbA1c, fasting glucose, and body composition tracking therapeutic efficacy [112]
- Weight-Predominant Phenotype: Patients with obesity and elevated leptin may achieve superior outcomes with GLP-1 RAs, evidenced by significant weight reduction and adipokine modulation [118] [115]
Combination Therapy and Sequencing Strategies
Emerging evidence supports strategic combination approaches:
- Complementary Mechanisms: GLP-1 RAs (appetite, glucose) + SGLT2is (renal, cardiac) provide multisystem coverage [112]
- Metabolic Synergy: Combined therapy demonstrates enhanced effects on HbA1c, body weight, and cardiovascular parameters compared to monotherapy [112]
- Biomarker-Guided Intensification: Rising inflammatory markers or persistent cardiac stress indicators may prompt additional therapy rather than switching
- Temporal Sequencing: Initial response assessment through biomarker monitoring (4-12 weeks) informs subsequent intensification decisions
SGLT2 inhibitors and GLP-1 receptor agonists represent cornerstone therapies in metabolic disease management with pleiotropic benefits extending beyond glycemic control. The biomarker signatures associated with these drug classes provide critical insights into their mechanisms of action and enable precision approaches to patient selection and treatment monitoring.
Future research directions should prioritize several key areas: First, the development of integrated biomarker panels that combine traditional metabolic parameters with novel inflammatory, cardiac, and organ-specific markers. Second, the validation of biomarker thresholds for therapy initiation, intensification, and switching in real-world populations. Third, the exploration of tissue-specific biomarker responses to better understand organ-targeted effects. Finally, the integration of multimodal data streams—including omics technologies, digital health metrics, and advanced imaging—to create comprehensive biomarker signatures that predict individual therapeutic responses.
As the field advances toward increasingly personalized approaches to metabolic disease management, biomarker-guided therapy with SGLT2 inhibitors and GLP-1 receptor agonists will continue to evolve, offering new opportunities to optimize outcomes through precise targeting of these transformative therapeutic classes.
The integration of biomarkers into established clinical risk scores represents a transformative frontier in predictive medicine, particularly for complex conditions like metabolic syndrome and type 2 diabetes mellitus (T2DM). Traditional risk assessment models, such as the Pooled Cohort Equations for cardiovascular disease or simple glycemic indices for diabetes, primarily utilize clinical and demographic variables. While foundational, these models often lack the granularity to capture underlying pathophysiological processes, leading to residual risk and suboptimal stratification for a significant proportion of patients. The incorporation of biomarkers—objective, measurable indicators of biological processes—offers a powerful strategy to enhance the predictive accuracy of these tools, thereby enabling more personalized and preemptive healthcare interventions.
The imperative for this enhanced stratification is underscored by the global burden of metabolic disease. T2DM alone affects over 529 million people worldwide, acting as a significant risk factor for coronary artery disease, renal disease, and stroke [120]. The heterogeneity in disease presentation and progression among patients with similar clinical profiles, such as body mass index or fasting glucose, points to distinct underlying biological drivers. Biomarkers, spanning domains from genetics and proteomics to metabolomics, provide a window into these drivers. They reflect key pathways including chronic inflammation, oxidative stress, myocardial injury, and metabolic dysregulation, which are often active long before clinical symptoms manifest. By integrating these molecular signals with conventional risk factors, we can move from a reactive to a proactive model of care, identifying high-risk individuals earlier and with greater precision [121] [15].
Biomarker Classes and Their Pathophysiological Significance
Biomarkers relevant to metabolic syndrome and T2DM can be categorized based on their molecular nature and the biological pathways they represent. A multi-omics approach, which leverages data from genomics, proteomics, and metabolomics, is crucial for capturing the full complexity of these diseases.
Genetic Biomarkers: Polygenic risk scores (PRS) aggregate the effects of numerous common genetic variants, each with a small individual effect, to quantify an individual's inherited susceptibility. A key study demonstrated that adding a CAD polygenic risk score to the Pooled Cohort Equations led to a modest but statistically significant improvement in discriminative accuracy for incident coronary artery disease (incremental C-statistic: 0.02) [122]. This illustrates the potential of genetic information to provide a lifetime risk context.
Proteomic and Circulating Biomarkers: This class includes proteins and hormones indicative of specific organ stress or systemic pathophysiological states. Well-validated biomarkers provide critical insights into cardiac strain, inflammation, and metabolic stress, making them highly relevant for predicting cardiometabolic complications in T2DM patients [123].
- N-terminal pro-B-type natriuretic peptide (NT-proBNP): A marker of cardiac wall stress and dysfunction.
- High-sensitivity Troponin T (hsTropT): A sensitive indicator of myocardial injury.
- Interleukin-6 (IL-6): A key pro-inflammatory cytokine.
- Growth Differentiation Factor 15 (GDF-15): A stress-responsive marker linked to inflammation, oxidative stress, and cellular senescence. Levels are elevated in obesity and T2DM, and it is a powerful predictor of cardiovascular mortality [123] [15].
- Adiponectin and Leptin: Adipokines that regulate energy balance and insulin sensitivity, with altered levels in obesity and insulin resistance [15].
Metabolomic and Lipid Biomarkers: Metabolomics, the comprehensive analysis of small-molecule metabolites, can reveal specific disruptions in metabolic pathways. Altered levels of branched-chain amino acids, triglycerides, and high-density lipoprotein (HDL) are strongly associated with insulin resistance and the future development of T2DM [124] [120]. In T2DM patients, characteristic changes include decreases in HDL and increases in low-density lipoprotein (LDL) and triglycerides [124].
Hematological and Inflammatory Biomarkers: A chronic, low-grade inflammatory state is a hallmark of metabolic syndrome and T2DM. Haematological profiles often show increased white blood cell counts (including neutrophils, lymphocytes, and monocytes), indicating systemic inflammation [124]. C-reactive protein (CRP) is another widely used inflammatory marker.
Table 1: Key Biomarker Classes and Their Clinical Relevance in Metabolic Disease
| Biomarker Class | Example Biomarkers | Pathophysiological Pathway | Clinical Utility |
|---|---|---|---|
| Genetic | Polygenic Risk Score (PRS) | Inherited susceptibility | Lifetime risk stratification [122] |
| Proteomic/Circulating | NT-proBNP, hsTropT | Cardiac stress, Myocardial injury | Heart failure/CVD risk prediction [123] [125] |
| Proteomic/Circulating | GDF-15, IL-6 | Inflammation, Oxidative stress | Cardiovascular mortality, Disease progression [123] [15] |
| Metabolomic/Lipid | HDL, Triglycerides, BCAA | Lipid metabolism, Insulin resistance | Early diabetes detection, Complication risk [124] [120] |
| Hematological | White Blood Cell Count | Systemic inflammation | Indicator of metabolic inflammation [124] |
Quantitative Evidence of Enhanced Predictive Accuracy
The additive value of biomarkers is quantifiably demonstrated through rigorous statistical measures of model performance, including the C-statistic (Area Under the Curve, AUC), Net Reclassification Improvement (NRI), and calibration metrics.
Evidence from large-scale studies is compelling. In a study of 3817 patients with atrial fibrillation, a biomarker panel comprising D-dimer, GDF-15, IL-6, NT-proBNP, and hsTropT significantly improved the prediction of a composite cardiovascular outcome (cardiovascular death, stroke, myocardial infarction, systemic embolism). The model's discriminatory power, measured by the AUC, improved from 0.74 to 0.77 upon the addition of biomarkers [123]. For stroke prediction specifically, the biomarker model outperformed the established clinical CHA₂DS₂-VASc score (AUC: 0.69 vs. 0.64) [123].
Similarly, a 20-year cohort study developed a predictive model for CVD mortality using machine learning. The model that integrated biomarkers with demographic variables achieved a superior C-index of 0.9205, outperforming models with demographics alone (C-index: 0.9030) or biomarkers alone (C-index: 0.8659) [125]. This underscores the synergy between traditional and novel risk factors.
In the genetic domain, adding a polygenic risk score for CAD to the Pooled Cohort Equations was associated with a C-statistic increase of 0.02 and an overall Net Reclassification Improvement of 4.0% at a 7.5% risk threshold, correctly reclassifying a significant number of individuals into more accurate risk categories [122].
Table 2: Performance Improvement with Biomarker Integration in Select Studies
| Clinical Context | Baseline Model | Enhanced Model (with Biomarkers) | Key Biomarkers | Performance Improvement |
|---|---|---|---|---|
| Atrial Fibrillation [123] | Clinical Variables | Clinical + Biomarker Panel | D-dimer, GDF-15, IL-6, NT-proBNP, hsTropT | AUC increased from 0.74 to 0.77 for composite CV outcome |
| Stroke in AF [123] | CHA₂DS₂-VASc Score | Biomarker Model | NT-proBNP, IL-6 | AUC: 0.69 (Biomarker) vs 0.64 (CHA₂DS₂-VASc) |
| CVD Mortality [125] | Demographics/Lifestyle | Demographics + Biomarkers | NT-proBNP, Troponins, Homocysteine | C-index: 0.9205 (Combined) vs 0.9030 (Demographics only) |
| Coronary Artery Disease [122] | Pooled Cohort Equations | PCE + Polygenic Risk Score | Genome-wide SNPs | Incremental C-statistic: 0.02; NRI: 4.0% |
Methodological Framework for Biomarker Integration
Experimental Protocols for Biomarker Discovery and Validation
The journey from biomarker discovery to clinical integration follows a structured pipeline to ensure robustness and clinical validity.
Discovery and Assay Development: This initial phase involves identifying candidate biomarkers through untargeted multi-omics approaches (e.g., mass spectrometry-based proteomics or metabolomics) on well-characterized cohorts. Subsequently, targeted, quantitative assays are developed. Advanced technologies like Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) and multiplexed immunoassays (e.g., Meso Scale Discovery, MSD) are increasingly favored over traditional ELISA due to their superior sensitivity, specificity, broader dynamic range, and ability to multiplex multiple analytes from a single sample, which improves efficiency and reduces costs [126].
Analytical Validation: This critical step ensures the assay itself is reliable and reproducible. Key parameters include:
- Accuracy and Precision: How close the measurements are to the true value and to each other.
- Sensitivity and Specificity: The lowest detectable amount and the ability to measure the analyte without cross-reactivity.
- Dynamic Range: The span of concentrations over which the assay provides a linear response.
- Reproducibility: Consistency of results across different operators, instruments, and days. Regulatory agencies like the FDA and EMA emphasize "fit-for-purpose" validation, where the rigor is matched to the biomarker's intended use [126].
Clinical Validation and Model Building: In this phase, the validated assay is applied to a large, independent cohort study to confirm the biomarker's association with the clinical outcome of interest. Researchers then use statistical and machine learning techniques to build an integrated risk model.
- Feature Selection: Algorithms, such as the Boruta algorithm used in the 20-year CVD mortality study, identify the most important predictors from a large set of clinical and biomarker variables [125].
- Model Construction: Both traditional Cox proportional hazards models and advanced machine learning models (e.g., random forest, XGBoost) are employed. Studies show that machine learning models can achieve high performance (AUC >0.95) and often see significant improvements when biomarkers are added [123].
- Performance Assessment: The final integrated model is evaluated using metrics like the C-index, calibration curves, and Decision Curve Analysis (DCA) to quantify its predictive accuracy and clinical net benefit [125].
The Scientist's Toolkit: Essential Reagents and Technologies
The experimental workflow relies on a suite of specialized reagents and platforms to ensure accurate and reproducible biomarker measurement.
Table 3: Research Reagent Solutions for Biomarker Analysis
| Item/Technology | Function in Workflow | Key Characteristics |
|---|---|---|
| U-PLEX Multiplex Assay (MSD) [126] | Simultaneous quantification of multiple protein biomarkers (e.g., cytokine panels) from a single low-volume sample. | High sensitivity, broad dynamic range, cost-effective for multi-analyte panels. |
| LC-MS/MS Systems [126] | Gold-standard for precise quantification and identification of small molecules (metabolites, drugs) and proteins. | Unmatched specificity, high sensitivity, capable of analyzing hundreds of analytes. |
| High-Affinity Antibody Pairs | Core components of immunoassays (ELISA, MSD) for specific capture and detection of target protein biomarkers. | Critical for assay specificity, sensitivity, and low cross-reactivity. |
| Stable Isotope-Labeled Internal Standards | Used in LC-MS/MS assays to correct for sample matrix effects and variability in sample preparation. | Essential for achieving high quantitative accuracy and precision. |
| Quality Control (QC) Samples | (e.g., pooled human serum at high/low analyte concentrations) used to monitor assay performance across batches. | Ensures reproducibility and reliability of data over time. |
Visualization of Integrated Risk Prediction Logic
The conceptual framework for how biomarkers complement traditional risk factors to produce a more accurate integrated risk score can be visualized as a logical workflow. This process begins with the parallel collection of traditional clinical data and biomarker data, which are then processed through feature selection and modeling to generate a final, enhanced risk prediction.
Challenges and Future Directions in Clinical Translation
Despite the compelling evidence, several challenges impede the routine clinical implementation of biomarker-enhanced risk scores.
A significant hurdle is analytical validation and standardization. The transition from research to clinic requires assays that are not only precise but also robust and reproducible across different laboratories. A review of the European Medicines Agency's biomarker qualification process found that 77% of challenges were linked to problems with assay validity, including specificity, sensitivity, and reproducibility [126]. Furthermore, the clinical utility and cost-effectiveness of new biomarker panels must be unequivocally demonstrated to justify their adoption. While a polygenic risk score improved reclassification, the absolute improvement in discriminative accuracy was modest (0.02), warranting further investigation before widespread clinical use [122]. Issues of generalizability across diverse ethnic and demographic populations also need to be addressed to ensure health equity.
Future trends are poised to address these challenges. The integration of artificial intelligence (AI) and machine learning (ML) will enable the analysis of increasingly complex, high-dimensional biomarker data, uncovering non-linear relationships that traditional methods miss [127]. The rise of multi-omics approaches is fundamental, providing a systems biology view of disease by integrating data from genomics, proteomics, and metabolomics to create comprehensive biomarker signatures [83] [127]. There is also a growing emphasis on patient-centric approaches, incorporating patient-reported outcomes and ensuring diverse population representation in biomarker studies [127]. Finally, advances in liquid biopsy technologies and single-cell analysis are expanding into non-oncology areas, offering non-invasive methods for dynamic monitoring and unprecedented resolution into cellular heterogeneity in metabolic tissues [127].
The integration of biomarkers into clinical risk scores marks a definitive shift towards data-driven, personalized medicine for metabolic syndrome and type 2 diabetes. By quantifying specific pathophysiological pathways—from inflammation and oxidative stress to genetic predisposition—biomarkers provide an objective layer of information that significantly enhances the predictive accuracy of traditional, phenotype-based models. Robust methodological frameworks for biomarker validation, coupled with advanced modeling techniques like machine learning, are key to successfully developing these integrated tools. While challenges in standardization and validation remain, the ongoing advancements in multi-omics technologies, AI, and a focus on clinical utility promise a future where risk stratification is profoundly more accurate, enabling earlier interventions and improved long-term outcomes for patients.
Conclusion
The integration of novel biomarkers into the clinical and research landscape of Metabolic Syndrome and Type 2 Diabetes marks a pivotal shift toward precision medicine. The pathophysiological interconnectedness of these conditions, encapsulated by frameworks like CRHM syndrome, necessitates a multi-system biomarker approach. From established glycemic markers to emerging inflammatory, fibrotic, and metabolomic signatures, these tools offer unprecedented potential for early detection, refined risk stratification, and monitoring of therapeutic efficacy. Future directions must focus on standardizing assays, validating panels in diverse populations, and leveraging multi-omics data through machine learning to develop robust, non-invasive diagnostic platforms. For drug development, these biomarkers present critical opportunities for patient stratification, target identification, and evaluating intervention impacts on specific pathophysiological pathways, ultimately enabling more personalized and effective therapeutic strategies to mitigate the global burden of metabolic disease.
References
- 1. From Metabolic Syndrome to Cardiovascular–Kidney ... [https://anatoljcardiol.com/article/AJC-97937]
- 2. Pathophysiology and emerging biomarkers of ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1661563/full]
- 3. an evolution of the metabolic syndrome concept! [https://pubmed.ncbi.nlm.nih.gov/22845817/]
- 4. From Cardiovascular-Kidney-Metabolic Syndrome to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853431/]
- 5. A Focus on Obesity and Type 2 Diabetes Mellitus [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561821/]
- 6. Frontiers | Type-2 diabetes epigenetic biomarkers : present status and... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1502640/full]
- 7. and Mass Spectrometry – Based Assays in Type... - NIDDK Biomarkers [https://www.niddk.nih.gov/news/meetings-workshops/2025/biomarkers-mass-2025]
- 8. Metabolic syndrome: molecular mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12378851/]
- 9. Metabolic syndrome: epidemiology, mechanisms, and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1661603/full]
- 10. Advances in Insulin Resistance—Molecular Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942056/]
- 11. The crucial role and mechanism of insulin resistance in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1149239/full]
- 12. Trends in insulin resistance: insights into mechanisms and ... [https://www.nature.com/articles/s41392-022-01073-0]
- 13. Metabolomic network reveals novel biomarkers for type 2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046487/]
- 14. Oxidative stress markers and inflammation in type 1 and 2 ... [https://www.nature.com/articles/s41598-025-05818-z]
- 15. A Focus on Obesity and Type 2 Diabetes Mellitus [https://www.mdpi.com/2227-9059/13/10/2443]
- 16. Linking oxidative stress biomarkers to disease progression ... [https://pubmed.ncbi.nlm.nih.gov/40492113/]
- 17. From Cardiovascular-Kidney-Metabolic Syndrome to ... [https://www.mdpi.com/2218-273X/15/2/213]
- 18. Pathophysiology and emerging biomarkers of cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605086/]
- 19. Inflammation in cardiovascular-kidney-metabolic syndrome [https://link.springer.com/article/10.1007/s11010-025-05379-9]
- 20. Cardiovascular, Kidney, Liver, and Metabolic Interactions in ... [https://pubmed.ncbi.nlm.nih.gov/40403106/?utm_source=linkedin&utm_medium=social&utm_content=2e61f30b-c421-4183-bed3-94d5cc31a417&utm_campaign=99-ALL-0501-Social&utm_term=baylor+scott+%26+white+the+heart+hospital+-+plano]
- 21. Evolving Therapies Highlight the Interconnected Nature of ... [https://www.pharmacytimes.com/view/evolving-therapies-highlight-the-interconnected-nature-of-cardio-kidney-metabolic-health]
- 22. The association of PTEN/PI3K/Akt pathway gene ... [https://www.nature.com/articles/s41598-025-05233-4]
- 23. The metformin mediated MAPK signaling pathway influences ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586509/]
- 24. The Resistin/TLR4/miR-155-5p axis: a novel signaling ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03522-3]
- 25. Exploring the Role of TLR2 and TLR4 Adaptor Proteins in ... [https://link.springer.com/10.1007/s12291-025-01338-9]
- 26. Blood Metabolic Biomarkers of Diabetes Mellitus Type 2 in ... [https://www.mdpi.com/2218-1989/15/6/395]
- 27. Identification of mitochondria-related feature genes for ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1501159/full]
- 28. Redox Homeostasis in Metabolic Syndrome and Type II ... [https://www.mdpi.com/1422-0067/26/21/10370]
- 29. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 30. Predicting HbA1c Target Achievement in Type 2 Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466564/]
- 31. Correlation of HbA1c levels with CT-based body ... [https://www.nature.com/articles/s41598-024-72702-7]
- 32. Evaluating indices of insulin resistance and estimating the ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1591677/full]
- 33. Prediction of Insulin Resistance in Nondiabetic Population ... [https://medinform.jmir.org/2025/1/e72238]
- 34. Diagnostic accuracy of various anthropometric indexes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457765/]
- 35. the role of TyG Index, BMI, and inflammatory markers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574256/]
- 36. Non-high-density lipoprotein cholesterol predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256453/]
- 37. Predictive factors of body weight loss in patients with type 2 ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1674308/full]
- 38. Plasminogen activator urokinase receptor as a diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10590464/]
- 39. Soluble urokinase receptor (suPAR) predicts ... [https://www.nature.com/articles/srep40627]
- 40. Soluble urokinase plasminogen activator receptor, platelet ... [https://www.sciencedirect.com/science/article/abs/pii/S1056872723002520]
- 41. Emerging roles of Galectin-3 in diabetes ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9156459/]
- 42. Galectin-3 as a potential biomarker of metabolic disorders ... [https://www.oaepublish.com/articles/2574-1209.2016.10]
- 43. Galectin-3/adiponectin as a new biological indicator for ... [https://www.aging-us.com/article/203101/text]
- 44. GDF-15 as a Target and Biomarker for Diabetes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4530250/]
- 45. The value of growth differentiation factor 15 as a biomarker for ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01588-w]
- 46. Association of Serum Galectin-3-Binding Protein and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.726154/full]
- 47. Advances in Metabolomics: A Comprehensive Review of ... [https://www.mdpi.com/1422-0067/26/8/3572]
- 48. Clinical metabolomics in type 2 diabetes mellitus [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893406/]
- 49. Metabolomics uncovers the diabetes metabolic network [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1624878/full]
- 50. Metabolomics in Endocrinology: The Way Forward - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410955/]
- 51. NMR-Based Serum Metabolomics and Correlation Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392183/]
- 52. The role of NMR-based circulating metabolic biomarkers in ... [https://www.nature.com/articles/s41598-022-19159-8]
- 53. Metabolomics: Insights for Disease Mechanisms & ... [https://esmed.org/metabolomics-insights-for-disease-mechanisms-biomarkers/]
- 54. Profiling of circulating microRNAs: from single biomarkers to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3291086/]
- 55. MicroRNA Signatures in Cardiometabolic Disorders as a Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609130/]
- 56. Stability of microRNAs in serum and plasma reveal ... [https://pubmed.ncbi.nlm.nih.gov/40926836/]
- 57. Emerging roles of microRNAs as diagnostics and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841963/]
- 58. Exploring the role of miR-126 in diabetes and its complications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542374/]
- 59. The "Picasso faces" of diabetic kidney disease [https://pubmed.ncbi.nlm.nih.gov/41257695/]
- 60. Circulating miR-126-3p and miR-423-5p Expression in de ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8863343/]
- 61. The association between 24-hour urinary biomarkers and ... [https://www.nature.com/articles/s41598-025-21246-5]
- 62. Emerging Biomarkers and Nanobiosensing Strategies in ... [https://www.mdpi.com/2079-6374/15/10/639]
- 63. Decoding Health: Exploring Essential Biomarkers Linked to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853123/]
- 64. Multiple Biomarkers Improved Prediction for the Risk of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7188981/]
- 65. Identification of biomarkers for the diagnosis of type 2 ... [https://pubmed.ncbi.nlm.nih.gov/39936105/]
- 66. Serum biomarkers for predicting microvascular ... [https://pubmed.ncbi.nlm.nih.gov/39158206/]
- 67. Type 2 diabetes may accelerate development of multiple ... [https://www.eurekalert.org/news-releases/1098293]
- 68. Multiple long-term conditions as the next transition in ... [https://www.nature.com/articles/s43856-025-00742-9]
- 69. Performance of quantitative measures of multimorbidity [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11922-2]
- 70. AI-driven predictive biomarker discovery with contrastive ... [https://www.sciencedirect.com/science/article/pii/S1535610825001308]
- 71. Editorial: Metabolic syndrome in patients with diabetes [https://www.frontiersin.org/journals/clinical-diabetes-and-healthcare/articles/10.3389/fcdhc.2025.1620665/full]
- 72. Insulin resistance (HOMA-IR) cut-off values and the metabolic syndrome in a general adult population: effect of gender and age: EPIRCE cross-sectional study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4016563/]
- 73. Metabolomic profiling reveals interindividual metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317516/]
- 74. Methods for estimating insulin resistance from untargeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10412652/]
- 75. Preanalytical, Analytical, and Computational Factors Affect Homeostasis Model Assessment Estimates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2518363/]
- 76. Plasma metabolites associated with homeostatic model ... [https://www.nature.com/articles/s41598-019-50260-7]
- 77. Development and validation of a continuous metabolic ... [https://www.nature.com/articles/s41598-023-33294-w]
- 78. Ethnic differences in metabolic syndrome in high-income ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11294386/]
- 79. Metabolic Syndrome Prevalence by Race/Ethnicity and ... [https://www.cdc.gov/pcd/issues/2017/16_0287.htm]
- 80. Association of biomarkers and Barthel Index with ... [https://pubmed.ncbi.nlm.nih.gov/39140764/]
- 81. a new composite marker predicts mortality in type 2 diabetes [https://clindiabetesendo.biomedcentral.com/articles/10.1186/s40842-025-00229-5]
- 82. Metabolomic network reveals novel biomarkers for type 2 ... [https://pubmed.ncbi.nlm.nih.gov/40171861/]
- 83. Global research dynamics in metabolic biomarkers and cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589725/]
- 84. Novel Antidiabetic Agents and Their Effects on Lipid Profile [https://pmc.ncbi.nlm.nih.gov/articles/PMC10299555/]
- 85. a cross-sectional study in Iraqi patients with type2 diabetes [https://ejim.springeropen.com/articles/10.1186/s43162-025-00529-3]
- 86. Recurrent circadian fasting (RCF) improves blood pressure ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-019-2007-z]
- 87. The difference between fasting and non-fasting lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8033327/]
- 88. Assessing the impact of fasting condition and storage time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11715159/]
- 89. Serum klotho as a novel biomarker for metabolic syndrome [https://pmc.ncbi.nlm.nih.gov/articles/PMC10944879/]
- 90. Ramadan fasting model modulates biomarkers of longevity ... [https://www.nature.com/articles/s41598-024-79557-y]
- 91. KORA F4/FF4 cohort study [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841139/]
- 92. Identification of candidate metabolite biomarkers for metabolic ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-023-01862-z]
- 93. Results of the Study of Health in Pomerania (SHIP-TREND-0) [https://pmc.ncbi.nlm.nih.gov/articles/PMC5078557/]
- 94. Effect of obesity on the associations of 25-hydroxyvitamin D ... [https://www.nature.com/articles/s41366-022-01122-2]
- 95. Cytokine atlas of the population-based cohort SHIP- ... [https://www.sciencedirect.com/science/article/pii/S1043466625000432]
- 96. Searching for Better Biomarkers for Metabolic Syndrome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9228548/]
- 97. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-18443-7]
- 98. Traditional and Digital Biomarkers: Two Worlds Apart? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7015353/]
- 99. Metabolomic signatures in adults with metabolic syndrome ... [https://clindiabetesendo.biomedcentral.com/articles/10.1186/s40842-025-00223-x]
- 100. Epitranscriptomic signatures in blood [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1656769/full]
- 101. Discovery and comparison of serum biomarkers for ... [https://www.sciencedirect.com/science/article/abs/pii/S0009912019311555]
- 102. Comparative Analysis of Biomarkers in Type 2 Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11069335/]
- 103. Beyond Detection: Conventional and Emerging Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427498/]
- 104. Cancer Biomarkers: Reflection on Recent Progress, ... [https://www.mdpi.com/2072-6694/17/18/2981]
- 105. Improving 10-year cardiovascular risk prediction in patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11730797/]
- 106. A Comprehensive Review of Type 2 Diabetes and ... [https://pubmed.ncbi.nlm.nih.gov/40332079/]
- 107. Biomarker identification and risk assessment of ... [https://www.nature.com/articles/s41598-024-77352-3]
- 108. Multi‐omics analysis revealed biomarkers for coronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371206/]
- 109. Machine learning approaches for biomarker discovery to ... [https://www.nature.com/articles/s41598-023-42338-0]
- 110. Enhancing type 2 diabetes mellitus prediction by integrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586166/]
- 111. A Single Visualization Technique for Displaying Multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6680673/]
- 112. Frontiers | GLP and 1 for the... receptor agonists SGLT 2 inhibitors [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1627909/full]
- 113. - GLP in the treatment of type 2 diabetes... 1 receptor agonists [https://pubmed.ncbi.nlm.nih.gov/33068776/]
- 114. Are GLP-1s the first longevity drugs? [https://www.nature.com/articles/s41587-025-02932-1]
- 115. Efficacy of lifestyle modification combined with GLP-1 ... [https://www.sciencedirect.com/science/article/pii/S2589537025003967]
- 116. Efficacy and influencing factors analysis of SGLT2 ... [https://pubmed.ncbi.nlm.nih.gov/41244824/]
- 117. Efficacy and influencing factors analysis of SGLT2 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1693420/full]
- 118. The effect of GLP-1 receptor agonists on circulating ... [https://pubmed.ncbi.nlm.nih.gov/40230207/]
- 119. Glucagon-like peptide 1 and cancer risk: advancing... receptor agonists [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00765-3]
- 120. Potential Molecular Biomarkers for Predicting and ... [https://www.mdpi.com/1420-3049/30/22/4448]
- 121. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 122. Predictive Accuracy of a Polygenic Risk Score–Enhanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7042853/]
- 123. Biomarker panels for improved risk prediction and ... [https://www.nature.com/articles/s41467-025-62218-7]
- 124. Key biomarkers in type 2 diabetes patients: A systematic review [https://pmc.ncbi.nlm.nih.gov/articles/PMC11618249/]
- 125. Delving into biomarkers and predictive modeling for CVD ... [https://www.nature.com/articles/s41598-025-88790-y]
- 126. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 127. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]