Evaluating Predictive Equations for Resting Energy Expenditure: A Comprehensive Guide for Researchers and Clinical Professionals
This article provides a systematic evaluation of predictive equations for resting energy expenditure (REE), addressing critical needs in research and clinical practice.
Evaluating Predictive Equations for Resting Energy Expenditure: A Comprehensive Guide for Researchers and Clinical Professionals
Abstract
This article provides a systematic evaluation of predictive equations for resting energy expenditure (REE), addressing critical needs in research and clinical practice. It examines the fundamental importance of REE assessment across diverse populations, from pediatric oncology to adult obesity. The content explores methodological approaches for equation development and application, identifies common challenges in equation selection across different patient demographics, and presents comparative validation studies. Designed for researchers, scientists, and drug development professionals, this comprehensive review synthesizes current evidence to guide optimal equation selection while highlighting limitations and future directions for improving energy expenditure prediction in both research and clinical settings.
Understanding Resting Energy Expenditure: Fundamentals and Clinical Significance
Resting Energy Expenditure (REE) represents the minimum energy required to sustain vital physiological functions while at complete rest, typically accounting for 60-75% of total daily energy expenditure in individuals with sedentary lifestyles [1] [2]. REE is frequently used interchangeably with Resting Metabolic Rate (RMR), though it is distinct from Basal Metabolic Rate (BMR), which is measured under more stringent conditions including complete rest, thermoneutral environment, and after a 12-hour fast [1]. Accurate assessment of REE provides fundamental insights into human energy requirements and serves as a cornerstone for developing personalized nutritional interventions, especially in metabolic disorders, obesity management, and clinical care [1] [3].
The precise determination of REE has significant implications across multiple research and clinical domains. In nutritional epidemiology, REE values form the basis for calculating total energy requirements [4]. In metabolic research, deviations from expected REE values can indicate underlying pathological conditions, with hyperthyroidism potentially increasing REE by 50-100% and hypothyroidism decreasing it by 20-40% [1]. Furthermore, REE measurements provide critical benchmarks for evaluating therapeutic interventions aimed at modulating energy balance [2].
Measurement Techniques: From Gold Standard to Practical Alternatives
Indirect Calorimetry: The Reference Method
Indirect calorimetry stands as the gold standard technique for measuring REE in both research and clinical settings [3]. This method calculates energy expenditure through precise measurements of oxygen consumption (VO₂) and carbon dioxide production (VCO₂) using specialized metabolic analyzers [1] [5]. The procedure is grounded in the principle that energy production is proportional to gas exchange, with measurements typically conducted over 20-60 minutes after an overnight fast and period of rest [3].
The standard experimental protocol for indirect calorimetry requires strict adherence to several conditions to ensure accuracy:
- Timing and Fasting: Measurements should be performed in the morning after an 8-12 hour overnight fast [3]
- Rest Requirements: Participants must abstain from strenuous exercise for 24 hours prior and rest for 30 minutes before measurement [5]
- Environmental Controls: Testing occurs in a thermo-neutral environment with dim lighting and minimal distractions [1]
- Equipment Calibration: Regular two-point gas analyzer calibration and flow meter calibration are essential [5]
Two primary systems are employed for indirect calorimetry. The ventilated hood system allows participants to breathe comfortably under a transparent canopy while resting in a supine position, typically used for 30-60 minutes [1]. Alternatively, metabolic carts utilizing mouthpieces or face masks can measure gas exchange in various positions and during different activities [1]. The collected VO₂ and VCO₂ values are used to calculate REE using the Weir equation: REE = [3.94(VO₂) + 1.11(VCO₂)] × 1440, which provides energy expenditure in kcal/day [6] [3].
Key Research Reagents and Equipment
Table 1: Essential Research Materials for REE Measurement
| Item | Function | Application Context |
|---|---|---|
| Indirect Calorimeter (e.g., Q-NRG+, Cosmed) | Measures VO₂ and VCO₂ | Gold standard REE measurement in clinical research [5] |
| Metabolic Cart | Analyzes inspired/expired gases | Laboratory-based energy expenditure measurement [1] |
| Ventilated Hood System | Captures respiratory gases | Comfortable REE measurement in supine position [1] |
| Bioelectrical Impedance Analyzer (e.g., Tanita BC-418) | Assesses body composition (FFM, FM) | Research on body composition-REE relationships [3] [2] |
| ActiGraph Accelerometer (wGT3X-BT) | Quantifies physical activity levels | Assessment of activity energy expenditure [5] |
| Calibration Gas Mixtures | Validates gas analyzer accuracy | Essential pre-measurement equipment calibration [3] |
Despite its accuracy, indirect calorimetry faces limitations in widespread application due to substantial equipment costs (typically thousands to tens of thousands of dollars), need for technical expertise, and significant time requirements per measurement [3]. These practical constraints have driven the development and use of predictive equations as accessible alternatives in both research and clinical practice [6].
Predictive Equations for REE: Comparative Analysis
Predictive equations estimate REE using anthropometric and demographic variables, offering practical advantages despite potential compromises in accuracy. These equations have been developed through regression analyses of large datasets, establishing mathematical relationships between easily measurable parameters and energy expenditure [1].
Major Predictive Equations and Their Formulations
Table 2: Commonly Used Predictive Equations for REE
| Equation | Year | Formula (Male) | Formula (Female) | Population Developed |
|---|---|---|---|---|
| Harris-Benedict [1] | 1919 | 88.362 + (13.397 × W) + (4.799 × H) - (5.677 × A) | 447.593 + (9.247 × W) + (3.098 × H) - (4.330 × A) | 239 healthy individuals aged 16-63 years |
| Mifflin-St Jeor [1] [7] | 1990 | (10 × W) + (6.25 × H) - (5 × A) + 5 | (10 × W) + (6.25 × H) - (5 × A) - 161 | 498 healthy individuals (normal weight, overweight, obese) |
| FAO/WHO/UNU (Weight only) [6] | 1985 | (11.6 × W) + 879 | (8.7 × W) + 829 | Large international population |
| FAO/WHO/UNU (Weight & Height) [6] | 1985 | (11.3 × W) + (16 × H) + 901 | (8.7 × W) - (25 × H) + 865 | Large international population |
| Owen [6] | 1986/1987 | 879 + (10.2 × W) | 795 + (7.18 × W) | 104 men and 44 women with wide weight range |
W = weight (kg), H = height (cm), A = age (years), H (m) = height in meters for WHO2 equation
Experimental Comparisons of Predictive Equations
Numerous studies have systematically evaluated the performance of predictive equations against indirect calorimetry across diverse populations. The following experimental data illustrate the comparative accuracy of these equations:
Table 3: Experimental Comparison of REE Predictive Equations vs. Indirect Calorimetry
| Study Population | Sample Size | Best Performing Equation(s) | Accuracy Rate | Mean Bias | Reference |
|---|---|---|---|---|---|
| Overweight/Obese Adults | 82 | Harris-Benedict, WHO1, WHO2 | High intraclass correlation | Low systematic error | [6] |
| Hospitalized Patients | 60 | Harris-Benedict, Mifflin-St Jeor | Within 10% for groups | Wide individual limits of agreement | [8] |
| NAFLD & T2DM Adults | 88 | FAO/WHO/UNU (Weight) | 46.5% | +10.2 kcal/day | [3] |
| Severely Obese Children/Adolescents | 287 | Lazzer-Sartorio | 55% | +1.6% (NS) | [9] |
| Overweight Adults (6-month intervention) | 33 | Owen | Most comparable | Not significant | [2] |
A 2008 study comparing Harris-Benedict and Mifflin-St Jeor equations in 60 hospitalized patients found that while both equations showed no statistically significant differences from measured REE at the group level, they demonstrated wide limits of agreement at the individual level, suggesting clinically important differences would be obtained when applying these equations to individual patients [8].
For specialized populations, equation performance varies significantly. In patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus, the FAO/WHO/UNU (weight only) equation demonstrated the smallest average bias (10.2 kcal/day) and highest accuracy (46.5%), though notably less than half of participants had REE estimates within 10% of measured values [3]. Similarly, in severely obese Caucasian children and adolescents, the Lazzer-Sartorio equations showed superior agreement with measured REE, with higher accuracy (55% of subjects) and lower mean differences compared to seven other equations [9].
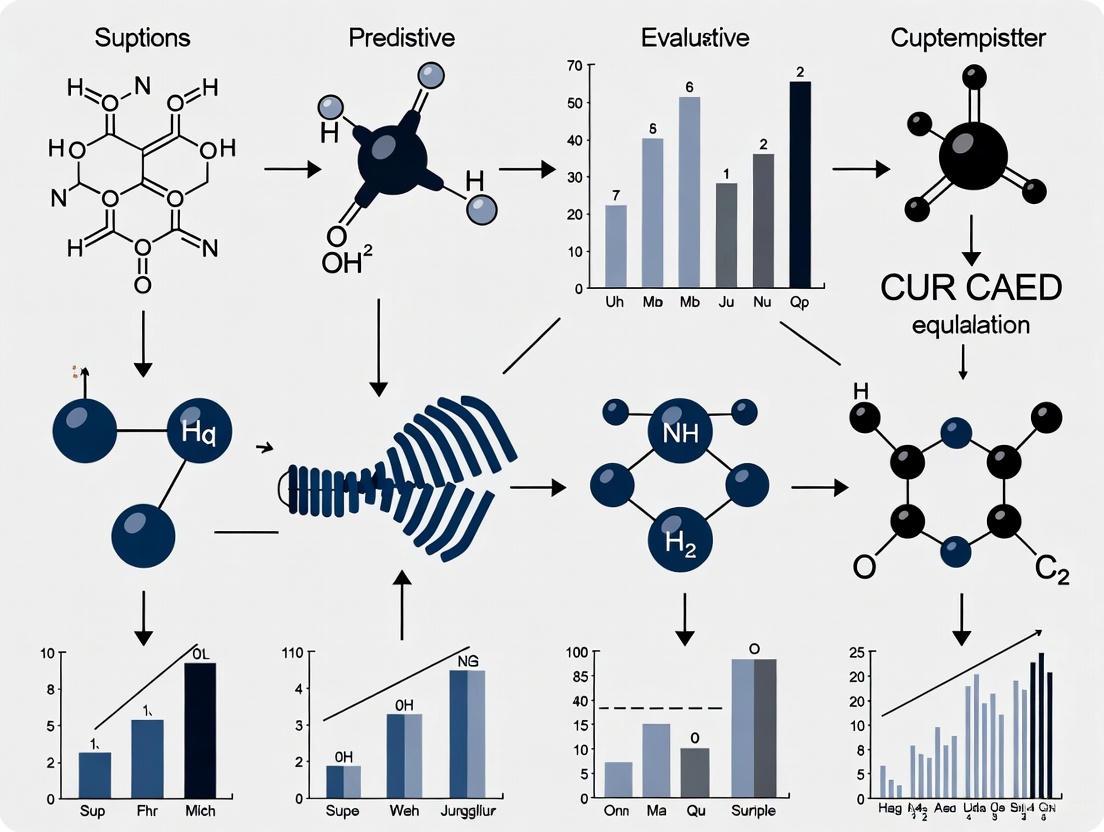
Diagram 1: Decision Framework for REE Assessment Method Selection. The flowchart illustrates the process of selecting appropriate REE measurement or estimation methods based on available resources and population characteristics, culminating in individualized nutrition planning.
Factors Influencing Resting Energy Expenditure
Biological Determinants
Multiple biological factors significantly impact REE, accounting for substantial interindividual variability:
Body Composition: Fat-free mass (FFM) represents the most significant determinant of REE, accounting for approximately 60-70% of its variance [5]. Muscle tissue is metabolically more active than adipose tissue, with each pound of muscle burning approximately 6 kcal/day at rest compared to 2 kcal/day for fat tissue [1]. A 2025 cross-sectional study confirmed FFM as the strongest predictor of REE, along with related metrics including total body water, body cell mass, and muscle mass [5].
Age: REE typically declines by 1-2% per decade after age 20, primarily due to age-related changes in body composition including reduced lean body mass and decreased cellular metabolism [1]. This decline occurs later in women (approximately age 50) compared to men (approximately age 40) [4].
Sex: Men generally exhibit 10-15% higher REE than women of similar age and weight, primarily attributable to differences in body composition, particularly greater lean body mass [1]. Even after adjusting for body composition differences, women typically show lower REE values [4].
Hormonal Factors: Thyroid hormones (T3 and T4) and catecholamines (epinephrine and norepinephrine) significantly increase REE [1]. Additionally, recent research indicates insulin levels and HOMA-IR show positive associations with REE, though these relationships may be mediated by body composition factors [5].
Environmental and Lifestyle Influences
Physical Activity: All physical activity intensities demonstrate significant associations with REE, with moderate physical activity (MPA) maintaining significance even after adjusting for sex and FFM [5]. This relationship may be attributed to habitual spontaneous physical activity generating post-exercise metabolic elevation and promoting adipose tissue browning [5].
Nutritional Status: Prolonged fasting or severe caloric restriction can reduce REE by 20-30% as an adaptive energy conservation mechanism [1]. Similarly, severe caloric restriction (50% of energy requirements) can decrease REE by 10-15% within 2-4 weeks [1].
Environmental Factors: Ambient temperature significantly impacts REE, with a 1°C decrease potentially increasing REE by 5-7% through adaptive thermogenic responses [1]. High altitude exposure (above 4,000 meters) can elevate REE by 10-20% due to hypoxic adaptive responses [1].
Advanced Research Applications and Methodological Considerations
Total Daily Energy Expenditure Estimation
In research settings, REE values typically serve as the foundation for estimating total daily energy expenditure (TDEE) through multiplication by appropriate physical activity level (PAL) factors:
- Sedentary: TDEE = REE × 1.2 [1]
- Lightly active: TDEE = REE × 1.375 [1] [7]
- Moderately active: TDEE = REE × 1.55 [1] [7]
- Active: TDEE = REE × 1.725 [1] [7]
- Very active: TDEE = REE × 1.9 [7]
This multiplicative approach enables researchers to translate laboratory REE measurements into real-world energy requirements for nutritional planning and intervention design [2].
Methodological Considerations for Research
When designing studies involving REE assessment, several methodological considerations are essential:
Measurement Conditions: Standardization is critical, requiring strict adherence to fasting protocols, rest periods, and environmental controls to ensure data comparability [3]. Even minor deviations in protocol implementation can significantly impact results.
Equipment Selection: Different indirect calorimetry systems (ventilated hood vs. metabolic cart) offer distinct advantages and limitations depending on research objectives, participant characteristics, and measurement context [1].
Population-Specific Validation: Researchers should validate chosen predictive equations against indirect calorimetry in their specific study populations when possible, particularly when investigating groups with distinctive metabolic characteristics [6] [9].
Longitudinal Assessment: In intervention studies, serial REE measurements are recommended as REE typically decreases with weight loss due to adaptive thermogenesis and loss of lean body mass, necessitating adjustment of energy prescription protocols [2].
Resting Energy Expenditure represents a fundamental parameter in nutritional science and metabolic research, with accurate assessment crucial for both research and clinical applications. While indirect calorimetry remains the gold standard for precise REE measurement, practical constraints often necessitate the use of predictive equations. The comparative performance of these equations varies significantly across different populations, with the Mifflin-St Jeor equation generally recommended for overweight and obese adults, the FAO/WHO/UNU equations for international populations, and the Harris-Benedict equation for general adult populations [1] [6] [7].
For researchers and clinicians, selection of appropriate assessment methods must balance accuracy requirements with practical constraints, while considering population-specific characteristics. Future research directions should focus on developing and validating more precise population-specific equations, particularly for understudied groups with distinct metabolic profiles. Additionally, advancing accessible indirect calorimetry technologies could bridge the current gap between precision and practicality in REE assessment, ultimately enhancing the quality of both research outcomes and clinical nutritional interventions.
Resting energy expenditure (REE) represents the number of calories required to maintain basic physiological functions at rest. Accurate REE measurement is crucial for research in metabolism, nutrition, and drug development. While various predictive equations offer convenient estimates, indirect calorimetry (IC) stands as the recognized gold standard for direct REE measurement in clinical and research settings [10] [11]. This guide objectively examines the principles, performance, and limitations of IC compared to predictive equations, providing researchers with a critical framework for selecting appropriate methodologies.
Principles of Indirect Calorimetry
Indirect calorimetry determines energy expenditure by measuring the body's gas exchange. The fundamental principle is based on the knowledge that heat production can be accurately estimated from oxygen consumption (VO₂) and carbon dioxide production (VCO₂) [12] [11].
Theoretical Foundations
The methodology rests on several key assumptions [11] [13]:
- All oxygen consumed is used to oxidize degradable fuels (carbohydrates, fats, proteins)
- All carbon dioxide produced is recovered and measured
- The oxidation of different macronutrients has fixed ratios of O₂ consumed to CO₂ produced
- Substrate loss through routes like feces and urine is negligible
Key Calculations
The core measurements obtained are VO₂ and VCO₂, which allow calculation of:
- Respiratory Quotient (RQ): The ratio of VCO₂ to VO₂ (VCO₂/VO₂), which indicates the predominant metabolic substrate being oxidized [12]
- Resting Energy Expenditure (REE): Typically calculated using the Weir equation [11] [13]: REE (kcal/day) = [3.941 × VO₂ (L/min) + 1.106 × VCO₂ (L/min)] × 1440
Table 1: Respiratory Quotient Values for Different Metabolic Substrates
| Metabolic Substrate | Respiratory Quotient (RQ) |
|---|---|
| Carbohydrates | 1.00 |
| Proteins | 0.80-0.82 |
| Fats | 0.70 |
| Mixed Diet | 0.85 |
Experimental Validation: IC vs. Predictive Equations
Multiple studies have quantitatively compared the accuracy of IC against commonly used predictive equations across diverse patient populations.
Performance in Critical Care Settings
A large retrospective validation study with 3,573 REE measurements in 1,440 ICU patients demonstrated the superior accuracy of IC [14]. The performance of predictive equations was notably limited:
Table 2: Performance of Predictive Equations in ICU Patients (n=1,440)
| Predictive Equation | Mean Difference from IC | Correlation with IC | Agreement with IC |
|---|---|---|---|
| Faisy | 90 kcal | Not specified | Not specified |
| Harris-Benedict | Not specified | 52% | 50% |
| Jolliet | Not specified | Not specified | 62% concordance |
The study concluded that predictive equations demonstrated low performance compared to IC, with agreement within 10% of actual caloric needs achieved in only one-third of patients [14].
Specialized Patient Populations
Trauma Patients
A pilot study of 31 trauma ICU patients revealed significant discrepancies between IC and predictive equations [15]:
Table 3: REE Measurements in Trauma Patients (n=31)
| Measurement Method | REE (kcal/day, Mean ± SD) | Significant Difference from IC |
|---|---|---|
| Indirect Calorimetry | 2,146 ± 444 | Reference |
| Ireton-Jones Equation | 2,279 ± 202 | No (p=0.053) |
| Harris-Benedict Equation | 1,509 ± 205 | Yes (p=0.006) |
| Fleisch Equation | 1,509 ± 154 | Yes (p=0.003) |
| Robertson & Reid Equation | 1,443 ± 160 | Yes (p<0.001) |
The Ireton-Jones equation showed the highest correlation with IC (r=0.521), while other equations significantly underestimated energy requirements [15].
Renal Transplantation Patients
A study of 51 renal transplant patients found that most predictive equations significantly underestimated REE compared to IC [16]. The Cunningham equation showed the closest agreement with a mean difference of -69 kcal, while the Bernstein equation substantially underestimated REE by -478 kcal. The study developed a new population-specific equation based on fat-free mass: REE = 424.2 + 24.7 × FFM (kg) [16].
Experimental Protocols for IC Measurement
Standardized protocols are essential for obtaining accurate IC measurements. The following methodologies are derived from cited experimental approaches.
Protocol for Mechanically Ventilated Patients
Based on trauma ICU studies [15]:
- Patient Preparation: Patients should be sedated to a Richmond Agitation-Sedation Scale (RASS) of -2 and maintained in steady state for 15 minutes before measurement
- Ventilator Settings: Fraction of inspired oxygen (FiO₂) should be below 60% with stable ventilator parameters
- Measurement Device: Use a calibrated metabolic cart (e.g., CCM Express, MGC Diagnostics)
- Measurement Duration: Continue until a steady state is achieved (typically 15-30 minutes after equilibration)
- Exclusion Criteria: FiO₂ > 0.6, respiratory quotient outside physiological range (0.67-1.3)
Protocol for Spontaneously Breathing Subjects
For non-ventilated subjects, different gas collection systems are employed [12] [11]:
- Douglas Bag: Collects all expired air in an inflatable airtight bag for subsequent volume and composition analysis
- Canopy System: Subject's head is placed under a transparent hood connected to a pump with adjustable ventilation
- Face Mask: Breath-by-breath measurement using a mask connected to a turbine flowmeter
Diagram 1: Indirect Calorimetry Measurement Workflow
Technological Approaches and Systems
Various IC systems have been developed, each with specific advantages and limitations [11] [13]:
Table 4: Indirect Calorimetry System Classifications
| System Type | Operating Principle | Applications | Key Limitations |
|---|---|---|---|
| Closed-circuit | Measures O₂ consumption in a closed space with CO₂ absorbers | High FiO₂ requirements | Equipment size, poor portability |
| Open-circuit | Subject breathes room air, expired gas analyzed | Most common clinical approach | Limited accuracy with FiO₂ > 0.8 |
| Douglas Bag | Total collection of expired gas in a bag | Research settings, reference standard | Collection bag size, potential leaks |
| Canopy/Dilution | Head under transparent hood, measures gas dilution | Clinical nutrition, resting measurements | Requires patient cooperation |
Limitations and Technical Challenges
Despite its gold standard status, IC has several important limitations that researchers must consider:
Clinical Limitations
- High FiO₂ Requirements: Standard open-circuit systems lose accuracy when FiO₂ exceeds 0.8 due to mathematical limitations in the Haldane transformation [11] [13]
- Circuit Leaks: Any leaks in the ventilator circuit or measurement apparatus can falsely reduce measured VO₂ and VCO₂ [11]
- Specific Patient Populations: Challenges exist with patients on extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy due to unmeasured CO₂ loss [17]
Practical Limitations
- Equipment Cost: Commercial IC systems represent significant financial investment
- Technical Expertise Required: Proper operation requires trained personnel for calibration and measurement [10]
- Time-Consuming: Measurements typically require 20-60 minutes of stable conditions per subject
Diagram 2: Limitations of Indirect Calorimetry
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 5: Key Research Materials for Indirect Calorimetry Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Metabolic Cart | Measures O₂ consumption and CO₂ production to calculate REE | CCM Express (MGC Diagnostics), Vmax Spectra |
| Calibration Gases | Ensure accuracy of gas analyzers through regular calibration | Precision gas mixtures with known O₂ and CO₂ concentrations |
| Douglas Bag Systems | Gold standard for gas collection in spontaneously breathing subjects | Airtight bags with appropriate volume capacity |
| Ventilator Interface | Allows IC measurement in mechanically ventilated patients | Compatible with ICU ventilators |
| Gas Analyzers | Measure O₂ and CO₂ concentrations in inspired and expired air | Paramagnetic O₂ sensors, infrared CO₂ analyzers |
| Flow Meters | Measure volume of inspired and/or expired air | Pneumotachographs, ultrasonic flow meters |
Advanced Applications and Future Directions
Recent technological advances have expanded IC applications beyond basic REE measurement:
Isotopic Calorimetry
The integration of ¹³CO₂ sensors with conventional IC systems enables quantification of exogenous versus endogenous substrate oxidation, providing insights into specific metabolic pathways [18]. This approach allows researchers to track the oxidation of individually labeled substrates such as glucose or fatty acids in real-time.
Extended Critical Care Applications
Modified IC protocols have been developed for challenging clinical scenarios, including patients on extracorporeal membrane oxygenation (ECMO) [17]. These approaches combine conventional IC measurements with mathematical modeling of O₂ and CO₂ content pre- and post-membrane oxygenation.
Indirect calorimetry remains the undisputed gold standard for REE measurement in research settings, providing accuracy that predictive equations cannot reliably match across diverse populations. While technical limitations exist, standardized protocols and proper equipment selection can mitigate many challenges. For research requiring precise energy expenditure data, particularly in metabolic studies or drug development, IC provides invaluable data that justifies the operational complexities. The continued refinement of IC technology and methodologies promises to further expand its applications in understanding human metabolism.
Resting Energy Expenditure (REE) represents the amount of energy required by the body to maintain fundamental physiological functions while at rest. As the largest component of total daily energy expenditure (accounting for 60-75%), accurately determining REE is fundamental to nutritional planning across clinical populations [19]. In clinical practice, indirect calorimetry (IC) serves as the gold standard for REE measurement through direct measurement of oxygen consumption and carbon dioxide production [3]. However, due to the high cost, limited availability, and technical expertise required for IC, healthcare providers frequently rely on predictive equations to estimate energy requirements using easily accessible variables such as age, sex, weight, and height [20] [21].
The miscalculation of REE presents substantial risks in clinical settings. When predictive equations underestimate true energy needs, patients face the threat of inadvertent underfeeding, potentially leading to hospital-acquired malnutrition and its associated complications. Conversely, overestimation of REE may result in overfeeding, contributing to excessive weight gain, metabolic disturbances, and increased complications in obese populations [22] [23]. This comparative guide examines the clinical consequences of REE miscalculation across different patient populations, evaluates the performance of various predictive equations against measured energy expenditure, and provides evidence-based recommendations for optimizing nutritional support in research and clinical practice.
Performance Comparison of REE Predictive Equations Across Clinical Populations
The accuracy of REE predictive equations varies significantly across different patient populations and clinical conditions. The tables below summarize comparative performance data from recent studies investigating equation accuracy in specific populations.
Table 1: Performance of REE Predictive Equations in Pediatric Oncology Patients (n=203) [20]
| Equation | Average Bias (kcal/day) | 95% Confidence Interval | Performance Notes |
|---|---|---|---|
| INP-Simple (New) | 114.8 | -408 to 638 | Least bias in this population |
| INP-Morpho (New) | 114.8 | -408 to 638 | Includes body composition parameters |
| Molnár | -82.3 | -741.3 to 576.7 | Moderate performance |
| Harris-Benedict | -133.6 | -671.5 to 404.2 | Underestimates REE |
| Oxford | -110.6 | -661.4 to 440.1 | Underestimates REE |
| Schofield | -185.4 | -697.6 to 326.8 | Significant underestimation |
| FAO/WHO/UNU | -178.8 | -683.9 to 326.3 | Significant underestimation |
| IOM | -201.0 | -761.7 to 359.7 | Greatest underestimation |
Table 2: Equation Performance in Morbidly Obese Patients (n=4,247) [23]
| Equation | Accuracy Rate | Average Bias (kcal/day) | Performance in Comorbidities |
|---|---|---|---|
| Mifflin-St Jeor | 61.1% | -89.87 | Best performance in patients with ≥3 comorbidities |
| Mifflin-St Jeor | 69% | -19.17 | Best in patients with type 2 diabetes |
| Mifflin-St Jeor | 66% | -21.67 | Best in patients with sleep apnea |
| Harris-Benedict | 45.3% | -152.4 | Consistent underestimation |
| WHO/FAO/ONU | 51.2% | -135.8 | Moderate underestimation |
| Müller | 48.7% | -141.9 | Moderate underestimation |
Table 3: Equation Accuracy in NAFLD and T2DM Patients (n=88) [3]
| Equation | Average Bias (kcal/day) | 95% Limits of Agreement | Accuracy Rate (% within ±10% of IC) |
|---|---|---|---|
| FAO/WHO/UNU (weight) | +10.2 | -57.4 to 78.0 | 46.5% |
| Müller (FFM) | -45.8 | -125.3 to 33.7 | 42.1% |
| Harris-Benedict | -65.3 | -144.8 to 14.2 | 38.6% |
| Mifflin-St Jeor | -88.7 | -168.2 to -9.2 | 35.2% |
| Owen | -155.4 | -234.9 to -75.9 | 28.4% |
| Thumb (25 × weight) | -402.2 | -477.3 to -327.1 | 20.4% |
Clinical Consequences of REE Miscalculation
Impact on Malnutrition and Treatment Outcomes
The inaccurate estimation of energy requirements directly impacts the development and progression of disease-related malnutrition. In hospitalized patients, malnutrition prevalence ranges from 13-40%, with many patients experiencing further nutritional decline during admission [22]. The consequences of REE miscalculation are particularly pronounced in pediatric oncology, where malnutrition at diagnosis ranges from 7% in leukemia patients to 50% in those with neuroblastoma [20].
In clinical practice, REE underestimation can lead to inadequate nutrition support, contributing to cascading physiological impairments. Malnourished patients demonstrate:
- Muscle function decline: Reduced energy-dependent cellular membrane pumping occurs even before measurable changes in muscle mass [22]
- Immune dysfunction: Impaired cell-mediated immunity and phagocyte function increase infection risk [22]
- Poor wound healing: Particularly problematic in surgical patients, leading to extended recovery [22]
- Increased complications: Malnourished surgical patients experience 3-4 times higher complication and mortality rates compared to well-nourished counterparts [22]
The economic impact is substantial, with disease-related malnutrition costs in the UK alone exceeding £13 billion annually—surpassing even obesity-related costs [22]. Even modest improvements in nutritional assessment could yield significant savings while improving patient outcomes.
Consequences in Obesity and Metabolic Disorders
In obese populations, accurate REE prediction becomes particularly challenging due to alterations in body composition and metabolic heterogeneity. The Mifflin-St Jeor equation demonstrates the best performance in morbidly obese patients, especially those with multiple comorbidities [23]. However, even this equation shows significant limitations, with accuracy rates of only 61.1% in patients with three or more comorbid conditions [23].
In patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes, predictive equations show particularly poor performance, with no equation achieving >50% accuracy at the individual level [3]. The commonly used "Thumb rule" (25 kcal/kg) demonstrates the worst performance, with a substantial average bias of -402.2 kcal/day and only 20.4% accuracy [3]. This systematic underestimation may lead to excessive calorie restriction, potentially exacerbating muscle loss while preserving fat mass during weight loss interventions.
Special Considerations in Critical Illness and Elderly Populations
In ventilated critically ill children, a comprehensive evaluation of 15 predictive equations revealed that none met performance criteria across the REE spectrum of 200-1000 kcal/day [24]. Even the best-performing equations (Mehta, Schofield, Henry, and Talbot) demonstrated wide confidence intervals, creating significant risks of underfeeding or overfeeding, particularly in the youngest patients [24].
Elderly patients present unique challenges due to age-related changes in body composition and the high prevalence of malnutrition (affecting up to 60% of hospitalized elderly) [19]. A systematic review identified 210 different predictive equations used in elderly populations, with significant heterogeneity in their estimates [19]. Equations incorporating only body weight demonstrated the highest agreement, while more complex formulas showed wider variation, potentially impacting clinical outcomes in this vulnerable population.
Methodological Approaches for REE Assessment
Gold Standard Protocol: Indirect Calorimetry
Indirect calorimetry represents the reference method for REE measurement through measurement of oxygen consumption (VO₂) and carbon dioxide production (VCO₂) [3]. The standard experimental protocol includes:
- Measurement conditions: Participants are measured in the morning after an 8-12 hour overnight fast, while lying supine in a thermoneutral environment, awake and motionless [3]
- Equipment calibration: Period gas and flow calibration are performed before each measurement using certified reference gases [3]
- Measurement duration: Typically 20 minutes of continuous measurement, discarding the first 5 minutes to allow for equipment stabilization [3]
- Data analysis: VO₂ and VCO₂ are converted to REE using the Weir equation: REE = [3.94(VO₂) + 1.11(VCO₂)] × 1,440 [3]
- Pre-test instructions: Participants abstain from caffeine, tobacco, and moderate-to-high intensity physical activity for 24 hours prior to testing [3]
Development of Population-Specific Predictive Equations
The development of new predictive equations follows standardized methodological approaches:
- Study design: Cross-sectional studies measuring REE via IC while collecting anthropometric and body composition data [20] [21]
- Participant recruitment: Population-specific recruitment based on demographic characteristics, health status, and clinical diagnoses [20]
- Statistical analysis: Multiple regression analyses to identify relationships between REE and predictor variables (weight, height, age, sex, body composition) [20] [21]
- Validation: Splitting cohorts into development and validation groups or external validation in independent populations [25]
- Performance assessment: Evaluating bias (average difference between measured and predicted REE) and accuracy (percentage of estimates within ±10% of measured REE) [20]
Recent advances incorporate bioelectrical impedance analysis (BIA) parameters, with equations including raw BIA variables (bioimpedance index and phase angle) showing slightly improved individual accuracy (70.3% in men, 72.3% in women) compared to traditional equations [25].
Metabolic Pathways and Clinical Workflow
The following diagram illustrates the metabolic consequences and clinical decision pathways involved in REE miscalculation.
Diagram 1: Metabolic and clinical consequences of REE miscalculation, showing how inaccurate estimation leads to adverse patient outcomes.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 4: Essential Research Materials for REE Investigation
| Tool/Reagent | Primary Function | Application Notes |
|---|---|---|
| Metabolic Cart (e.g., QUARK RMR, COSMED) | Measures VO₂ and VCO₂ for IC | Requires regular gas and flow calibration; specialized operation needed [3] |
| Bioelectrical Impedance Analyzer (e.g., Tanita BC-418, SECA) | Assesses body composition (FFM, FM) | Provides raw BIA variables (phase angle) for enhanced equations [25] |
| Digital Calibrated Scale (e.g., SECA 813) | Precise weight measurement | Essential for accurate anthropometric input data [20] |
| Ultrasonic Stadiometer (e.g., InLab S50) | Accurate height measurement | Critical for BMI calculation and equation inputs [20] |
| Calibrated Skinfold Calipers | Adipose tissue thickness measurement | Alternative body composition assessment when BIA unavailable |
| Data Collection Software | Standardized data management | Customized platforms for integrating IC, BIA, and anthropometric data |
The consistent miscalculation of resting energy expenditure presents significant clinical risks across diverse patient populations. Current evidence demonstrates that general predictive equations frequently misestimate true energy requirements, with potentially serious consequences for nutritional status, treatment outcomes, and healthcare costs. The development of population-specific equations, such as the INP equations for pediatric oncology patients, shows promise for improving accuracy in specialized clinical contexts [20].
For researchers and clinicians, several key recommendations emerge from this analysis:
Prioritize indirect calorimetry in complex patients, particularly those with multiple comorbidities, metabolic disorders, or critical illness where predictive equations demonstrate poor accuracy [24] [3] [23]
Select population-appropriate equations when IC is unavailable, recognizing that even the best-performing equations may misestimate individual requirements by several hundred kilocalories per day [20] [23]
Incorporate body composition data where possible, as equations including fat-free mass and BIA parameters generally demonstrate improved accuracy compared to those based solely on weight and height [25]
Implement regular monitoring of nutritional status and weight changes to identify miscalculation early and adjust nutritional support accordingly
Future research should focus on developing more sophisticated prediction models that incorporate metabolic biomarkers, genetic factors, and advanced body composition analysis to better capture the complex determinants of energy expenditure in health and disease.
Comparative Accuracy of Predictive Equations Across Populations
The accuracy of predictive equations for Resting Energy Expenditure (REE) varies significantly across different patient populations. The tables below summarize the performance of various equations in pediatric oncology, general pediatric obesity, and adult oncology patients.
Table 1: Performance of REE Predictive Equations in Pediatric Oncology Patients (2025 Study) [26] [20] [27]
| Equation Name | Bias (kcal/day) | 95% Limits of Agreement (kcal/day) | Clinical Recommendation |
|---|---|---|---|
| INP-Simple/Morpho (New) | 114.8 | -408 to 638 | Preferred; least bias in this population |
| Molnár | -82.3 | -741 to 577 | Acceptable performance |
| Oxford | -110.6 | -661 to 440 | Moderate bias |
| Harris-Benedict | -133.6 | -672 to 404 | Significant bias |
| Kaneko | -135.6 | -653 to 381 | Significant bias |
| Müller | -162.6 | -715 to 390 | Significant bias |
| FAO | -178.8 | -684 to 326 | Significant bias |
| Schofield | -185.4 | -698 to 327 | Significant bias |
| IOM | -201.0 | -762 to 360 | Greatest bias |
Table 2: Performance of REE Predictive Equations in Obese Pediatric and Adult Populations [28] [9] [29]
| Patient Population | Most Accurate Equation(s) | Accuracy Rate | Key Findings |
|---|---|---|---|
| Obese Children/Adolescents | Lazzer-Sartorio | 55% accurate | Showed the best agreement with measured REE in severely obese Caucasians. [9] |
| Obese Children | Derumeaux-Burel (New) | No significant difference vs. measured | Specifically developed for a large population of obese children; validated externally. [29] |
| Obese Children | FAO/WHO/UNU | No significant mean difference, but low accuracy (26%) | Low individual accuracy despite good mean performance. [9] |
| Obese Adults (BMI ≥30) | Harris-Benedict (1918) | Best for obese subgroup | Recommended for obese hospital patients when indirect calorimetry is not available. [28] |
Table 3: Performance of REE Predictive Equations in Adult Oncology Patients [30]
| Aspect of Accuracy | Key Finding | Implication for Practice |
|---|---|---|
| Overall Accuracy | REE cannot be accurately predicted on an individual level. | Highlights the limitation of all predictive equations in oncology. |
| Best Performing | Mifflin-St. Jeor had the smallest limits of agreement (-21.7% to 11.3%). | Most precise, but individual-level inaccuracy remains. |
| Body Composition | Equations including Fat-Free Mass (FFM) were not consistently more accurate. | Simpler equations may be as useful as complex ones. |
| Bias Correlation | Bias was consistently positively correlated with age and negatively with Fat Mass (FM). | Patient age and body composition significantly impact equation error. |
Detailed Experimental Protocols
Protocol: Development of INP Predictive Equations in Pediatric Oncology
A 2025 cross-sectional study established a specific protocol for developing and validating REE equations in pediatric oncology patients. [20] [27]
- Patient Population: The study recruited 226 treatment-naïve pediatric patients (6 to <18 years) with a recent oncological diagnosis (0-2 weeks post-diagnosis). The final analysis included 203 participants, with the majority having solid tumors (68.5%), followed by leukemia (20.2%) and brain tumors (11.3%). [26] [20] [27]
- Exclusion Criteria: Patients were excluded if they were taking medications affecting metabolic function (e.g., corticosteroids, thyroid hormones, insulin), had diagnoses of hypothyroidism/hyperthyroidism, or had severe cognitive/motor impairments. [20] [27]
- Anthropometric & Nutritional Assessment: Weight was measured using a calibrated digital scale (SECA 813), and height was measured with an ultrasonic stadiometer (InLab S50). Various circumferences (waist, hip, mid-upper arm, etc.) were measured. Nutritional status was classified using WHO BMI-for-age and height-for-age z-scores via AnthroPlus software. [20] [27]
- Body Composition Analysis: Determined using bioelectrical impedance analysis, providing data on fat-free mass and fat mass for the INP-Morpho equation. [26] [20]
- REE Measurement (Gold Standard): REE was measured using Indirect Calorimetry (IC) with a standardized protocol, following a fasting period. [26] [20]
- Equation Development and Comparison: Two new equations (INP-simple with basic clinical variables; INP-Morpho with body composition) were developed using statistical modeling. Their accuracy was compared against measured IC values and existing equations (e.g., Harris-Benedict, Schofield) using bias, limits of agreement, and confidence intervals. [26] [20] [27]
Protocol: Validation of Equations in Obese Pediatric Populations
A 2007 study established a protocol for comparing predictive equations in obese youth. [9]
- Patient Population: 287 severely obese Caucasian children and adolescents (121 males, 166 females) with a mean BMI z-score of 3.3. [9]
- Body Composition Analysis: Assessed using bioelectrical impedance analysis. [9]
- REE Measurement: REE was measured by indirect calorimetry (MREE). [9]
- Equation Comparison: REE was calculated using multiple predictive equations (McDuffie, Derumeaux, Tverskaya, Schofield, FAO/WHO/UNU, Harris-Benedict, Lazzer-Sartorio). The agreement between predicted (PREE) and measured (MREE) values was analyzed using mean differences, standard deviations, and the percentage of subjects for whom the prediction was accurate (likely within 10% of MREE). [9]
Research Workflow and Pathway Diagrams
The following diagram illustrates the logical workflow for developing and validating a population-specific REE predictive equation, as demonstrated in the 2025 pediatric oncology study. [26] [20] [27]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Equipment and Materials for REE Research [20] [27] [31]
| Item | Specific Example(s) | Critical Function in Research |
|---|---|---|
| Indirect Calorimeter | Metabolic cart (e.g., Deltatrac 2 MBM-200, Vmax Encore n29); Hand-held device (e.g., MedGem) | Gold-standard instrument for directly measuring REE by analyzing oxygen consumption and carbon dioxide production. [20] [31] [28] |
| Calibration Gases | Reference gas mixture (e.g., 95% O2, 5% CO2); Two standard gases (e.g., 26% O2, 0% CO2 and 16% O2, 4% CO2) | Ensures the accuracy and precision of the indirect calorimeter before and during measurements. [28] |
| Calibrated Digital Scale | SECA Alpha, SECA 813 | Precisely measures patient body weight, a key variable in most predictive equations. [20] [27] [28] |
| Stadiometer | Ultrasonic stadiometer (e.g., InLab S50) | Accurately measures patient height, a key variable in many predictive equations and for BMI calculation. [20] [27] |
| Bioelectrical Impedance Analysis (BIA) | Various bioimpedance analyzers | Assesses body composition (fat-free mass, fat mass), which is used in advanced predictive equations and body composition-specific validation. [26] [20] [9] |
| Anthropometric Tape | SECA 201 | Measures body circumferences (mid-upper arm, waist, etc.) for nutritional assessment. [20] [27] |
Resting energy expenditure (REE) represents the energy required to maintain fundamental physiological functions at rest. This comprehensive analysis examines the metabolic foundations of REE and its intricate relationships with body composition and physiological status. We evaluate predictive equations against indirect calorimetry as the reference standard, presenting quantitative comparisons for researchers and drug development professionals. The evidence demonstrates that lean body mass serves as the primary determinant of RMR, accounting for 60-75% of total daily energy expenditure. This review synthesizes current methodologies, validation protocols, and technical resources to advance research in metabolic monitoring and predictive modeling of energy expenditure.
Basal metabolic rate (BMR), often used interchangeably with REE in clinical literature, is defined as the rate of metabolism that occurs when an individual is at rest in a warm environment and in the post-absorptive state, having not eaten for at least 12 hours [32]. This energy supports the function of vital organs including the heart, lungs, nervous system, and kidneys [32]. REE represents the largest component (~60-75%) of total daily energy expenditure in adults [33], reflecting the steady-state level of energy homeostasis in the body. The accurate assessment of REE is fundamental to research in obesity, metabolic disorders, and nutritional interventions, with predictive equations serving as essential tools when direct calorimetric measurement is impractical.
The complex interplay between body composition, physiological status, and metabolic rate forms a critical foundation for understanding human energy expenditure. Research has consistently demonstrated that body composition parameters—specifically the proportions of fat mass and fat-free mass—exert profound influences on metabolic rate [34] [35]. These relationships are further modulated by factors including age, sex, nutritional status, and physiological conditions such as pregnancy, disease states, and aging [36]. This review systematically evaluates the metabolic basis of REE within the context of contemporary research methodologies and predictive modeling approaches.
The Metabolic Basis of REE
Fundamental Concepts and Definitions
Resting energy expenditure represents the energy required to maintain cellular, tissue, and organ system homeostasis under basal conditions. The American Journal of Clinical Nutrition defines BMR as the "minimum number of calories your body needs to perform basic bodily functions" [34]. These functions include respiratory circulation, neural function, protein synthesis, and ion transport across membranes—processes that continue uninterrupted during waking and sleep states. While the terms REE and BMR are often used interchangeably in clinical practice, BMR typically refers to measurements made under more strictly controlled conditions (complete rest, thermoneutral environment, and post-absorptive state), whereas REE may allow for less restrictive conditions while still capturing the dominant component of daily energy expenditure.
From a biochemical perspective, REE represents the sum of all energy-releasing reactions occurring at rest, primarily through mitochondrial oxidative phosphorylation. The metabolic processes contributing to REE include substrate cycling, cardiac muscle contraction, respiratory muscle work, renal solute transport, and hepatic protein synthesis. The brain alone accounts for approximately 20% of REE despite representing only 2% of body mass, highlighting the variable metabolic activity of different tissues [32].
Body Composition as a Determinant of REE
Body composition exhibits a fundamental hierarchical organization that directly informs our understanding of its relationship with REE. The five-level model of body composition—spanning atomic, molecular, cellular, tissue-organ, and whole-body levels—provides a framework for understanding metabolic variability between individuals [35].
Figure 1: Hierarchical model of body composition and its relationship to REE. The molecular level components (Fat-Free Mass and Fat Mass) most directly determine REE. FFM: Fat-Free Mass; FM: Fat Mass; ECF: Extracellular Fluid; ECS: Extracellular Solids.
At the molecular level, the body can be partitioned into fat mass (FM) and fat-free mass (FFM), with FFM comprising approximately 73% water, 20% protein, and 7% mineral [35]. This distinction is metabolically significant because FFM represents the metabolically active tissue component, with different organs contributing disproportionately to REE relative to their mass. Research indicates that the high metabolic activity of organs like the heart, kidneys, and liver contrasts with the relatively low metabolic rate of adipose tissue, explaining why individuals with higher FFM typically exhibit higher REE [34].
The relationship between lean body mass and REE forms a fundamental principle in energy metabolism. Studies consistently demonstrate that "the more Lean Body Mass you have, the greater your Basal Metabolic Rate will be" [34]. This occurs because muscle tissue and organs require energy for maintenance even at complete rest, unlike adipose tissue which is relatively metabolically inactive. This understanding reframes the concept of a "slow metabolism" from one of velocity to one of capacity—individuals with greater lean mass possess a "bigger" metabolism with higher absolute energy requirements [34].
Predictive Equations for REE: Comparative Analysis
Reference Standard: Indirect Calorimetry
Indirect calorimetry (IC) represents the gold standard for measuring REE in clinical and research settings. This noninvasive method calculates energy expenditure from respiratory gas exchange—specifically oxygen consumption (VO₂) and carbon dioxide production (VCO₂)—using the Weir equation: REE = [3.94(VO₂) + 1.11(VCO₂)] × 1440 min/day [6]. The methodology requires strict standardization, including measurements performed in the morning after a 12-hour fast, 6-8 hours of sleep, and avoidance of intense physical activity for 24 hours prior to testing, conducted in a silent environment with dim lighting and controlled temperature [6].
Despite its accuracy, IC has limitations for widespread use, including equipment cost, technical expertise requirements, and time-intensive protocols. These practical constraints have driven the development and utilization of predictive equations for estimating REE in both research and clinical contexts.
Comparative Performance of Predictive Equations
Table 1: Comparison of REE predictive equations against indirect calorimetry in overweight and obese adults (n=82) [6]
| Equation | Formula (Male) | Formula (Female) | REE Estimate (kcal/day) | Systematic Error | Intraclass Correlation |
|---|---|---|---|---|---|
| Indirect Calorimetry | - | - | 1896 ± 419 | Reference | Reference |
| Harris-Benedict | 66.47 + (13.75×W) + (5×H) - (6.75×A) | 655.10 + (9.56×W) + (1.85×H) - (4.68×A) | 1718 ± 329 | Low | High |
| WHO1 (Weight only) | (11.6 × W) + 879 | (8.7 × W) + 829 | 1756 ± 303 | Low | High |
| WHO2 (Weight & Height) | (11.3 × W) + (16 × H) + 901 | (8.7 × W) - (25 × H) + 865 | 1765 ± 310 | Low | High |
| Mifflin | (9.99×W) + (6.25×H) - (4.92×A) + 5 | (9.99×W) + (6.25×H) - (4.92×A) - 161 | 1607 ± 304 | High | Moderate |
| Owen | 879 + (10.2 × W) | 795 + (7.18 × W) | 1607 ± 284 | High | Moderate |
W = weight (kg), H = height (cm), A = age (years)
A comparative study of 82 overweight and obese adults (BMI ≥25 kg/m²) revealed significant differences in the performance of common predictive equations [6]. The Harris-Benedict, WHO1, and WHO2 equations demonstrated the highest intraclass correlation coefficients and lowest systematic errors when compared to IC measurements. In contrast, the Mifflin and Owen equations consistently underestimated REE in this population [6]. These findings highlight the importance of selecting population-appropriate equations, particularly for overweight and obese individuals where inaccurate estimation can substantially impact weight management interventions.
Special Considerations for Different Populations
The performance of REE predictive equations varies across populations due to differences in body composition, age, and ethnicity. Research indicates that the interplay between BMR, physical exercise, diet, and body composition differs across Caucasian, Hispanic, and Asian populations [33]. This has prompted large-scale studies using diverse cohorts including the UK Biobank (500,000 adults), China Kadoorie Biank (500,000 participants), and Mexico City Prospective Study (100,000 participants) to develop more ethnically appropriate equations [33].
Age represents another critical factor, as BMR decreases with age and with the loss of lean body mass [32]. This decline in FFM with aging explains approximately 60-70% of the observed reduction in REE in older adults. Additionally, sex differences significantly impact REE, with men typically exhibiting higher absolute REE values due to greater lean body mass, even when adjusting for body size [35].
Experimental Protocols and Methodologies
Standardized REE Assessment Protocol
Figure 2: Standardized experimental workflow for REE assessment via indirect calorimetry. Strict protocol adherence ensures measurement accuracy and reliability.
The protocol for measuring REE via indirect calorimetry requires strict standardization to ensure accurate results. As implemented in research settings [6], the methodology includes:
- Subject Preparation: Participants undergo a 12-hour overnight fast, obtain 6-8 hours of sleep, and avoid intense physical activity for 24 hours prior to testing.
- Testing Conditions: Measurements occur in a silent environment with dim lighting and controlled temperature to minimize external influences on metabolic rate.
- Equipment Calibration: The calorimetry system undergoes 30-minute warm-up and calibration with gases of known concentration before measurements.
- Measurement Period: After a 10-minute acclimatization period for reading stabilization, VO₂ and VCO₂ are measured for 20 minutes to calculate REE using Weir's equation.
This protocol controls for factors known to acutely influence metabolic rate, including food intake, physical activity, and environmental stimuli.
Doubly Labeled Water Methodology for Total Energy Expenditure
For measuring total daily energy expenditure in free-living individuals, the doubly labeled water method represents the gold standard. This approach, utilized in endurance limitation studies [37], involves:
- Isotope Administration: Participants ingest water containing stable, non-radioactive isotopes of hydrogen (²H) and oxygen (¹⁸O).
- Urine Collection: Spot urine samples are collected over 7-14 days to measure isotope elimination rates.
- Calculation: The difference in elimination rates between ²H (which leaves the body as water) and ¹⁸O (which exits as both water and carbon dioxide) allows calculation of carbon dioxide production, from which total energy expenditure is derived.
This method has revealed critical insights into human metabolic limits, demonstrating that even elite athletes cannot sustain energy expenditure beyond approximately 2.5 times their BMR for prolonged periods [37].
Advanced Research Applications
Metabolic Biomarkers in Research
Table 2: Promising biomarkers for monitoring metabolic status in research settings [38]
| Metabolic Domain | Biomarkers | Research Application | Assessment Method |
|---|---|---|---|
| Bone Metabolism | Urinary n-telopeptide, Bone mineral density (BMD), Bone pain assessment | Fracture risk prediction, Bone remodeling monitoring | DXA, Urinary assays, Questionnaires |
| Muscle Metabolism | 24-hour urinary 3-methylhistidine, Protein turnover rates, Perceived exertion scales | Muscle catabolism assessment, Performance prediction | Stable isotope methods, Borg scale, Urinalysis |
| Glucose Metabolism | Tissue lactate levels, Muscle glycogen content, Heart rate variability | Fatigue monitoring, Metabolic fuel utilization | NIRS, Muscle biopsy, ECG monitoring |
| Hydration Status | Body weight changes, Plasma osmolality, Urine specific gravity | Dehydration assessment, Fluid balance monitoring | Weight scales, Plasma analysis, Urine dipsticks |
| Cognitive Function | Actigraphy, Electroencephalography (EEG), Visual analog scales | Cognitive readiness assessment, Fatigue monitoring | Wearable sensors, EEG caps, Questionnaires |
Advanced research in energy metabolism extends beyond REE measurement to include comprehensive metabolic monitoring. The Institute of Medicine has identified promising biomarkers for assessing metabolic status in field research settings [38]. These biomarkers enable researchers to monitor specific aspects of metabolic function and identify deviations from normal physiological ranges.
For muscle metabolism, 24-hour urinary 3-methylhistidine provides a non-invasive marker of muscle protein catabolism, as this compound is not metabolized and reflects myofibrillar protein breakdown [38]. Similarly, hydration status can be monitored through short-term body weight changes coupled with serum sodium or osmolality measurements, providing critical data on fluid balance during metabolic studies [38].
Body Composition Assessment Methods
The accurate assessment of body composition provides essential context for interpreting REE measurements. Research methodologies include:
- Dual-Energy X-ray Absorptiometry (DXA): Provides precise measurement of fat mass, lean mass, and bone mineral density with low radiation exposure.
- Bioelectrical Impedance Analysis (BIA): Measures resistance and reactance to alternating electrical currents to estimate body composition.
- Air Displacement Plethysmography (ADP): Determines body volume and density to calculate fat and lean mass.
- Magnetic Resonance Imaging (MRI) and Computed Tomography (CT): Provide highly detailed tissue-specific composition data, including visceral and subcutaneous adipose tissue distribution.
Each method operates on different principles and varies in cost, accessibility, and precision, requiring researchers to select appropriate methodologies based on specific research questions and resources.
Table 3: Essential research reagents and methodologies for REE and body composition studies
| Category | Item | Research Function | Application Notes |
|---|---|---|---|
| Calorimetry | Indirect Calorimeter | Gold standard REE measurement | Requires strict protocol adherence for accurate results |
| Stable Isotopes | ²H₂O (Deuterated water), H₂¹⁸O (Oxygen-18 water) | Total energy expenditure measurement via doubly labeled water | Allows free-living assessment over 1-2 week periods |
| Body Composition | DXA Scanner, BIA Device, ADP System | Fat and fat-free mass quantification | DXA provides three-compartment model data |
| Biomarker Assays | Urinary n-telopeptide kits, 3-methylhistidine assays | Bone and muscle metabolism monitoring | Requires 24-hour urine collection for accuracy |
| Physiological Monitoring | Actigraphy devices, Heart rate variability monitors, EEG systems | Cognitive function and fatigue assessment | Provides objective measures of physiological strain |
| Statistical Analysis | R, STATA, Python, SAS packages | Data analysis and predictive modeling | Essential for developing population-specific equations |
This toolkit summarizes essential resources for conducting rigorous research in energy expenditure and body composition. The listed methodologies enable comprehensive assessment of metabolic status from cellular to whole-body levels, facilitating advanced research into the relationships between body composition, physiological status, and energy metabolism.
For drug development professionals, these tools provide critical endpoints for evaluating metabolic interventions, whether targeting weight management, muscle preservation, or metabolic disease treatment. The combination of precise body composition assessment with accurate REE measurement enables comprehensive metabolic phenotyping that can identify responders and non-responders to therapeutic interventions.
The metabolic basis of REE is fundamentally rooted in body composition, with fat-free mass representing the primary determinant of individual variation in energy expenditure. This relationship forms the foundation for predictive equations that estimate REE across diverse populations, though their accuracy varies significantly, particularly in overweight and obese individuals. Contemporary research methodologies—from indirect calorimetry and doubly labeled water to advanced body composition assessment—provide powerful tools for investigating energy metabolism in both laboratory and free-living settings.
Future research directions should focus on refining predictive models through incorporation of ethnic-specific variables, developing standardized protocols for special populations, and advancing wearable technologies for continuous metabolic monitoring. The integration of metabolic biomarkers with body composition assessment and REE measurement will further enhance our understanding of energy homeostasis, supporting advancements in nutritional science, metabolic drug development, and personalized medicine approaches to weight management and metabolic health.
Developing and Applying REE Predictive Equations: Methodological Approaches
The accurate assessment of energy requirements is a cornerstone of nutritional science, clinical practice, and pharmacological research. Within this domain, resting energy expenditure (REE)—the energy the body requires at complete rest to maintain cellular and systemic functions—represents the largest component of daily energy expenditure, typically accounting for 60-75% of total expenditure in sedentary individuals [39] [40]. The precise determination of REE is therefore critical for developing effective nutritional support strategies, calculating caloric requirements for weight management, and establishing baseline metabolic rates in clinical trials for metabolic disorders.
The historical evolution of REE predictive equations reflects an ongoing scientific endeavor to balance accuracy with practicality. While indirect calorimetry remains the gold standard for measuring REE through direct assessment of oxygen consumption and carbon dioxide production, the equipment required is costly, technically demanding, and often inaccessible for routine clinical use or large-scale studies [6] [25]. Consequently, predictive equations—mathematical models that estimate REE based on readily available anthropometric and demographic variables—have become indispensable tools for researchers and clinicians alike. This review traces the development of these equations from their seminal beginnings with Harris-Benedict to contemporary models, evaluating their performance, limitations, and appropriate applications within modern research contexts.
The Founding Formulation: Harris-Benedict Equation
Historical Development and Original Formulations
The Harris-Benedict equation represents the foundational work in the field of metabolic prediction. Published in 1918 and 1919 by James Arthur Harris and Francis Gano Benedict, this equation emerged from extensive biometric studies conducted at the Nutrition Laboratory of the Carnegie Institution [41]. The original research involved 136 male and 103 female subjects, with measurements conducted under strict basal conditions. The equation was derived using multiple regression analysis to correlate measured basal metabolic rate with the key variables of weight, height, and age, separately for men and women [41].
The original Harris-Benedict equations were formulated as follows:
Original Harris-Benedict Equations (1919)
- Men: BMR = 66.473 + (13.7516 × weight in kg) + (5.0033 × height in cm) - (6.755 × age in years)
- Women: BMR = 655.0955 + (9.5634 × weight in kg) + (1.8496 × height in cm) - (4.6756 × age in years)
These equations remained the predominant method for estimating basal metabolic rate for over six decades until concerns about their accuracy in modern populations prompted revisions and new formulations.
The Roza and Shizgal Revision (1984)
By the 1980s, researchers recognized that changes in body composition and lifestyle since the early 20th century might have affected the accuracy of the original Harris-Benedict equations. In 1984, Roza and Shizgal published a revised version based on a re-evaluation of the original data [41]:
Revised Harris-Benedict Equations (Roza and Shizgal, 1984)
- Men: BMR = 88.362 + (13.397 × weight in kg) + (4.799 × height in cm) - (5.677 × age in years)
- Women: BMR = 447.593 + (9.247 × weight in kg) + (3.098 × height in cm) - (4.330 × age in years)
This revision attempted to correct for apparent overestimation in the original formulas while maintaining the same basic mathematical structure and variable composition.
Modern Evolutionary Steps: Key Predictive Equations
The Mifflin-St Jeor Equation (1990)
Recognizing the limitations of the Harris-Benedict equations, Mifflin and St Jeor developed a new predictive equation in 1990 using data from 498 healthy subjects, including both normal-weight and obese individuals [42]. This equation was specifically designed to be more reflective of contemporary body composition and lifestyle:
Mifflin-St Jeor Equations (1990)
- Men: REE = (10 × weight in kg) + (6.25 × height in cm) - (5 × age in years) + 5
- Women: REE = (10 × weight in kg) + (6.25 × height in cm) - (5 × age in years) - 161
The researchers reported that this new equation was more accurate than the Harris-Benedict equations, which overestimated measured REE by approximately 5% in their study population [42]. The simplified structure also enhanced its utility for clinical applications.
WHO/FAO/UNU Equations (1985)
The World Health Organization, in collaboration with the Food and Agriculture Organization and United Nations University, developed predictive equations that offered alternative formulations based on weight alone or combined weight and height [6] [43]:
WHO/FAO/UNU Equations (1985)
- Men (weight only): REE = (11.6 × weight in kg) + 879
- Women (weight only): REE = (8.7 × weight in kg) + 829
- Men (weight & height): REE = (11.3 × weight in kg) + (16 × height in meters) + 901
- Women (weight & height): REE = (8.7 × weight in kg) - (25 × height in meters) + 865
These equations were developed through international collaborative efforts and were designed for global application across diverse populations.
Owen and Colleagues' Equations (1986-1987)
Owen and colleagues developed alternative equations specifically for normal-weight individuals, using data that emphasized the relationship between body weight and REE [6]:
Owen Equations (1986-1987)
- Men: REE = 879 + (10.2 × weight in kg)
- Women: REE = 795 + (7.18 × weight in kg)
These equations notably excluded height and age as variables, focusing solely on body weight as the primary predictor of resting energy expenditure.
Comparative Analysis: Experimental Validation of Predictive Equations
Methodological Approaches for Equation Validation
The validation of predictive equations for REE follows established experimental protocols centered around comparison with indirect calorimetry as the reference standard. The typical methodology includes:
Subject Preparation: Participants are tested after an overnight fast (10-12 hours), having abstained from caffeine, alcohol, and strenuous physical activity for at least 24 hours. A rest period of 30 minutes precedes measurement to ensure a true resting state [39] [6].
Measurement Conditions: REE measurements are conducted in a thermoneutral environment with dim lighting and minimal auditory stimulation. Subjects remain awake while lying supine, breathing quietly through a mouthpiece or ventilated hood system [39].
Indirect Calorimetry Protocol: Using metabolic carts such as the Deltatrac II or MedGem, measurements of oxygen consumption (VO₂) and carbon dioxide production (VCO₂) are taken over 15-30 minutes, with the first 5-10 minutes typically discarded to allow for stabilization [39] [40]. REE is then calculated using the Weir equation: REE = [3.9(VO₂) + 1.1(VCO₂)] × 1440 [6].
Statistical Analysis: Comparison between predicted and measured REE involves multiple statistical approaches including paired t-tests, correlation analysis, Bland-Altman plots for assessing agreement, and calculation of the percentage of subjects whose REE is predicted within ±10% of measured values [6] [40].
The following workflow diagram illustrates the standard experimental protocol for validating predictive equations against indirect calorimetry:
Performance Comparison Across Populations
Extensive research has compared the accuracy of various predictive equations against measured REE across different population groups. The following table summarizes key comparative findings from multiple validation studies:
Table 1: Comparative Accuracy of Predictive REE Equations Across Population Subgroups
| Population | Sample Characteristics | Most Accurate Equation | Accuracy Rate | Key Findings | Reference |
|---|---|---|---|---|---|
| Healthy Non-obese & Obese | Systematic review of multiple studies | Mifflin-St Jeor | ~80% within ±10% of measured REE | Most reliable for both non-obese and obese individuals; narrowest error range | [44] |
| Overweight/Obese Adults | 82 participants, BMI ≥25 kg/m² | Harris-Benedict, WHO1, WHO2 | High intraclass correlation | All equations significantly different from IC; HB and WHO equations least underestimating | [6] |
| Weight-Reduced Women | 51 weight-reduced women (BMI ≤25) | Harris-Benedict | Overestimation: 105±135 kcal/day | HB overestimated significantly less in weight-reduced vs. overweight women | [39] |
| Japanese Schizophrenia Patients | 110 patients on antipsychotics | Harris-Benedict | Strongest correlation (r=0.617) | No significant bias in Bland-Altman analysis; most appropriate for this population | [40] |
| Hospital In/Outpatients | 93 adult patients | WHO (weight & height) | Smallest prediction error (233 kcal/d) | Best performance across outpatient, inpatient, and underweight subgroups | [43] |
| African American Women | Various BMI categories | None satisfactory | Significant overestimation | HB overestimated more in AA vs. Caucasian women (P<0.001) | [39] |
Quantitative Comparison of Prediction Errors
The following table presents specific numerical data on prediction errors and bias for major equations across multiple studies:
Table 2: Quantitative Prediction Errors of Major REE Equations (kcal/day)
| Equation | Population | Bias (Mean Difference from IC) | Limits of Agreement | Accuracy (% within ±10% of IC) | Reference |
|---|---|---|---|---|---|
| Harris-Benedict | Never-overweight women | +160 ±125 | +35 to +285 | ~60% | [39] |
| Harris-Benedict | Overweight women | +295 ±189 | +106 to +484 | ~40% | [39] |
| Harris-Benedict | Weight-reduced women | +105 ±135 | -30 to +240 | ~70% | [39] |
| Mifflin-St Jeor | Overweight/obese adults | -289* | Wide range | ~45% | [6] |
| WHO (weight & height) | Overweight/obese adults | -140* | Wide range | ~55% | [6] |
| Owen | Overweight/obese adults | -289* | Wide range | ~45% | [6] |
| Harris-Benedict | Japanese schizophrenia | -1.7 ±282.3 | -284 to +280.6 | Not reported | [40] |
| Mifflin-St Jeor | Japanese schizophrenia | -46.7 ±290.3 | -337 to +243.6 | Not reported | [40] |
*Values estimated from graphical data; statistical significance not reported.
Specialized Equations and Emerging Approaches
Population-Specific Formulations
As limitations of general predictive equations became apparent, researchers developed specialized formulations for specific patient populations and clinical scenarios:
Ireton-Jones Equations: Developed for ventilated burn patients, accounting for the hypermetabolic state of trauma and burns, with adjustments for mechanical ventilation [45].
Fusco Formula: Designed specifically for morbidly obese ICU patients to prevent overfeeding, incorporating both metric and imperial measurements [45].
Frankenfield Equations: Created for sepsis and trauma patients, incorporating minute volume and hemoglobin measurements based on correlations with metabolic rate in these populations [45].
Incorporation of Body Composition Data
Recent research has explored the integration of body composition metrics into predictive models. A 2020 study developed new equations incorporating raw bioimpedance analysis (BIA) variables, demonstrating slightly improved accuracy compared to traditional equations [25]. The equation incorporating BIA variables showed the highest accuracy at the individual level (70.3% for men, 72.3% for women within ±10% of measured REE) [25].
The fundamental relationships between body composition parameters and energy expenditure can be visualized as follows:
Essential Research Reagents and Methodological Tools
The experimental validation of predictive equations requires specific methodological approaches and technical equipment. The following table details key research reagents and tools essential for conducting validation studies in this field:
Table 3: Essential Research Reagents and Methodological Tools for REE Equation Validation
| Category | Specific Tool/Instrument | Research Function | Key Considerations |
|---|---|---|---|
| Calorimetry Systems | Deltatrac II Metabolic Monitor (SensorMedics) | Gold standard REE measurement via indirect calorimetry | Requires regular calibration with reference gases; hood or mouthpiece systems [39] |
| Portable Calorimetry | MedGem Portable Indirect Calorimeter (HealtheTech) | Field measurements of REE | Validated against metabolic carts; useful for clinical settings [40] |
| Body Composition | DXA (Dual-energy X-ray Absorptiometry) | Precise measurement of fat mass and fat-free mass | Critical for understanding body composition-REE relationships [39] |
| Bioimpedance Analysis | BIA devices with phase angle measurement | Estimation of body composition and cellular health | Raw BIA variables (phase angle) may improve REE prediction accuracy [25] |
| Anthropometric Equipment | Digital stadiometer (Heightronic) | Accurate height measurement | Essential input variable for most predictive equations [39] |
| Anthropometric Equipment | Calibrated digital scale (Scale-tronix) | Precise weight measurement | Required for all predictive equations; calibrated regularly [39] |
| Data Analysis | Bland-Altman statistical method | Assessment of agreement between predicted and measured REE | Superior to correlation alone for method comparison studies [6] [40] |
| Nutrition Analysis | Nutrition Data System for Research (NDS-R) | Calculation of dietary energy content during validation studies | Ensures precise energy intake during controlled feeding protocols [39] |
The evolution of predictive equations for resting energy expenditure—from the pioneering Harris-Benedict formulation to contemporary models—reflects an ongoing scientific pursuit of metabolic prediction accuracy. The evidence synthesized in this review demonstrates that while the Mifflin-St Jeor equation generally shows the highest accuracy across diverse populations, no single equation achieves perfect prediction for all individuals or population subgroups [44]. The performance of these equations is significantly influenced by factors such as weight history, ethnicity, body composition, and health status [39].
For researchers and drug development professionals, several critical implications emerge from this analysis. First, the selection of predictive equations should be guided by the specific population under study, with careful consideration of the demonstrated biases for particular demographic or clinical groups. Second, when precise energy expenditure assessment is methodologically critical, indirect calorimetry remains indispensable despite its practical limitations [44]. Finally, emerging approaches incorporating body composition data and population-specific adjustments represent promising avenues for improving prediction accuracy.
Future research should focus on developing and validating equations in currently underrepresented populations, including diverse ethnic groups, older adults, and specific clinical populations. The integration of novel biomarkers and body composition metrics may further enhance prediction accuracy. Until such advances mature, researchers should apply existing equations with appropriate caution, recognizing their limitations and the potential clinical implications of estimation errors in both research and practice.
Accurate prediction of energy expenditure is a cornerstone of nutritional science, clinical practice, and metabolic research. Researchers and clinicians rely on various predictive equations to estimate resting energy expenditure (REE) and total energy expenditure (TEE) when direct measurement via gold standard methods is impractical or unavailable. These equations incorporate different structural approaches and variables, each with distinct advantages and limitations. This guide provides a comprehensive comparison of the primary equation architectures—weight-based, height-inclusive, and body composition models—evaluating their performance characteristics, validity across populations, and appropriate applications.
The fundamental challenge in predictive equation development lies in balancing accuracy with practicality. While direct measurement methods like indirect calorimetry for REE and doubly labeled water for TEE provide the most accurate assessments, their cost, technical requirements, and time-intensive nature limit widespread clinical implementation [20] [46]. Consequently, researchers have developed numerous predictive equations that estimate energy expenditure using easily obtainable parameters such as weight, height, age, sex, and body composition metrics. Understanding the structural foundations and variable selections of these equations is essential for selecting the appropriate tool for specific research objectives and patient populations.
Comparative Analysis of Equation Architectures
Weight-Based Models
Core Structure and Rationale Weight-based models represent the most fundamental approach to predicting energy expenditure, utilizing body weight as the primary or sole anthropometric variable. These equations typically follow the general form: REE = a × weight + b, where coefficients 'a' and 'b' vary based on age, sex, and the specific population used for derivation. The physiological basis stems from the correlation between metabolic rate and body mass, particularly the relationship between energy requirements and fat-free mass, which accounts for 60-70% of REE variation in many populations [47].
The Food and Agriculture Organization (FAO) equations exemplify this approach, incorporating weight alongside age and sex factors. Similarly, the Schofield equations utilize weight-based calculations with different coefficients for various age groups. These models offer exceptional practicality in clinical settings where only basic anthropometric data is available, requiring minimal measurement time and expertise.
Performance Characteristics Validation studies reveal significant limitations in weight-based models, particularly for specialized populations. In hospitalized patients, the Schofield equation demonstrated systematic underestimation of energy needs for patients at nutritional risk [48]. For pediatric oncology patients, the FAO and Schofield equations showed considerable bias (-178.8 kcal/day and -185.4 kcal/day, respectively) compared to indirect calorimetry measurements [20].
The precision of weight-based equations diminishes substantially in populations with abnormal body composition. In obese children and adolescents, the Schofield equation demonstrated root mean squared error (RMSE) values exceeding 697 kcal/day in some validations, reflecting poor individual-level accuracy despite reasonable population-level estimates [47]. This pattern of increased error at BMI extremes underscores the limitation of relying exclusively on body weight without accounting for body composition differences.
Height-Inclusive Models
Core Structure and Rationale Height-inclusive models incorporate stature as a key variable, typically in combination with weight, age, and sex. The most widely recognized height-inclusive metric is the Body Mass Index (BMI), calculated as weight divided by height squared (kg/m²). BMI-based equations assume a fixed mathematical relationship between height and weight, an assumption that introduces systematic biases across different anthropometric profiles [49] [50].
The Harris-Benedict equations represent classic height-inclusive models, developed in 1919 and still widely applied in clinical practice. These equations incorporate weight, height, age, and sex with different coefficients for males and females. Similarly, the Mifflin-St Jeor equations follow this structural approach with updated coefficients derived from a more contemporary population.
Performance Characteristics Comparative analyses demonstrate that the fixed relationship between height and weight inherent in BMI introduces complex non-uniform biases across outcomes and height-weight space [50]. For cardiometabolic outcomes including hypertension, diabetes, and dyslipidemia, BMI-based models consistently underperform compared to more flexible modeling approaches.
In hospitalized populations, the Harris-Benedict and Mifflin-St Jeor equations systematically underestimate energy requirements for underweight patients (BMI < 18.5) and overestimate for obese patients (BMI ≥ 30) [48]. This systematic error pattern highlights the limitations of the fixed height-weight relationship assumption, particularly at anthropometric extremes.
Research from Vanderbilt University Medical Center demonstrates that replacing BMI with a maximally flexible height-weight interaction model improves prediction accuracy across all tested cardiometabolic outcomes, including metabolic syndrome components, atrial fibrillation, coronary artery disease, heart failure, and peripheral artery disease [49] [50]. The flexible model demonstrated higher likelihood ratio, R², and Somers' Dxy rank correlation compared to BMI-based approaches, with particularly pronounced improvements for predicting features of atherogenic dyslipidemia at higher body weights.
Body Composition Models
Core Structure and Rationale Body composition models represent the most physiologically grounded approach, utilizing fat-free mass (FFM) and/or fat mass (FM) as primary predictive variables. These models directly address the metabolic heterogeneity of different tissue types, recognizing that FEM is the primary determinant of resting energy expenditure due to the high metabolic activity of organ tissues and muscles [47].
The Müller equations utilize FFM and FM alongside age and sex, while the Lazzer equations incorporate body composition metrics specifically developed for obese pediatric populations. The structural form typically follows: REE = c × FFM + d × FM + e, with coefficients varying based on the derivation population and additional factors.
Performance Characteristics Body composition models generally demonstrate superior accuracy compared to weight-based and height-inclusive approaches, particularly in specialized populations. In obese children and adolescents, the Lazzer equation achieved the highest prediction accuracy (44.9%) among all equations tested [47]. Similarly, for overweight pediatric populations, the Müller equation based on FFM showed among the highest accuracy (59.6%) [47].
Population-specific body composition equations have demonstrated particularly strong performance. For Japanese patients with interstitial lung disease, a specialized equation using only FFM (REE = 456.988 + 22.539 × FFM) showed no systematic errors and higher agreement (69.4%) compared to existing general equations [51]. Similarly, for pediatric oncology patients, newly developed equations incorporating body composition (INP-Morpho model) demonstrated significantly less bias than traditional equations [20].
The primary limitation of body composition models is the practical requirement for body composition assessment technology, such as bioelectrical impedance analysis (BIA) or dual-energy X-ray absorptiometry (DXA), which may not be available in all settings. Additionally, the accuracy of these models depends on the precision of the body composition measurement method employed.
Quantitative Performance Comparison
Table 1: Accuracy of Predictive Equations Across Populations
| Equation | Population | Bias (kcal/day) | RMSE (kcal/day) | Prediction Accuracy (%) |
|---|---|---|---|---|
| Harris-Benedict | Pediatric Oncology | -133.6 | Not Reported | Not Reported |
| FAO/WHO | Pediatric Oncology | -178.8 | Not Reported | Not Reported |
| Schofield | Pediatric Oncology | -185.4 | Not Reported | Not Reported |
| Müller (FFM) | Overweight Children | Not Reported | Not Reported | 59.6 |
| Lazzer | Obese Children | Not Reported | Not Reported | 44.9 |
| New INP Equations | Pediatric Oncology | 114.8 | Not Reported | Not Reported |
| Schmelzle | Normal-Weight Children | Not Reported | 136.2 | Not Reported |
| Schmelzle | Overweight Children | Not Reported | 159.9 | Not Reported |
| IOM | Normal-Weight Children | Not Reported | Not Reported | 63.8 |
Table 2: Performance Comparison of Height-Weight Models Versus BMI
| Outcome | Likelihood Ratio Improvement | R² Improvement | Somers' Dxy Improvement |
|---|---|---|---|
| Metabolic Syndrome | 21.42 | 0.0006 | 0.0010 |
| Diabetes Mellitus | 47.046 | 0.0008 | 0.0030 |
| Hypertension | 23.124 | 0.0004 | 0.0007 |
| Low HDL | 17.958 | 0.0002 | 0.0009 |
| Coronary Artery Disease | Not Reported | Not Reported | Not Reported |
Experimental Methodologies for Equation Validation
Gold Standard Measurement Techniques
Indirect Calorimetry Protocol for REE Indirect calorimetry represents the gold standard for measuring resting energy expenditure, providing precise assessment of energy production through respiratory gas exchange analysis. The validated protocol requires careful standardization to ensure accurate measurements [20] [51] [47]. Participants must fast for a minimum of 8-12 hours and avoid strenuous exercise for 24 hours preceding measurement. Testing is conducted in a thermoneutral environment with participants resting in a supine position for 15-30 minutes before measurement. A canopy hood or face mask system collects expired gases, with oxygen consumption (VO₂) and carbon dioxide production (VCO₂) measured for 20-45 minutes. The Weir equation then calculates REE from these gas exchange measurements: REE = (3.941 × VO₂ + 1.106 × VCO₂) × 1440.
Doubly Labeled Water Protocol for TEE The doubly labeled water (DLW) technique provides the gold standard for measuring total energy expenditure in free-living conditions over 1-2 weeks [46]. After collecting a baseline urine sample, participants orally consume a dose of water containing stable isotopes deuterium (²H₂) and oxygen-18 (H₂¹⁸O). The dose is calculated based on body mass with desired enrichment of 10% ¹⁸O and 5% ²H₂. Post-dose urine specimens are collected at 3 hours and then daily for 14 days. Isotopic enrichment in urine samples is analyzed using isotope ratio mass spectrometry. Elimination rates of the two isotopes are used to calculate carbon dioxide production rates, which are then converted to TEE using established equations.
Statistical Validation Methods
Bland-Altman Analysis The Bland-Altman method assesses agreement between measured energy expenditure (via indirect calorimetry or DLW) and equation predictions [46] [51] [47]. This analysis plots the differences between the two methods against their means, calculating mean bias (indicating systematic over- or under-prediction) and limits of agreement (±1.96 standard deviations of the differences). The presence of proportional error is evaluated through regression analysis of the differences against the means.
Accuracy and Precision Metrics Multiple statistical parameters evaluate equation performance. Root mean squared error (RMSE) quantifies average prediction error magnitude, with lower values indicating better performance [47]. Prediction accuracy represents the percentage of subjects whose predicted REE falls within ±10% of measured REE. Mean absolute percent error (MAPE) provides a relative measure of prediction error. Additionally, researchers report R² values indicating the proportion of variance in measured energy expenditure explained by the equation.
Structural Relationships in Equation Design
The diagram below illustrates the conceptual framework and variable interactions underlying different equation structures for predicting energy expenditure.
Equation Design and Validation Framework
Research Reagent Solutions for Energy Expenditure Studies
Table 3: Essential Research Materials and Equipment
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Indirect Calorimeter | Measures oxygen consumption and carbon dioxide production to calculate energy expenditure | REE measurement in clinical and research settings [20] [51] [47] |
| Doubly Labeled Water | Stable isotope-labeled water for measuring total energy expenditure in free-living conditions | TEE validation studies [46] |
| Bioelectrical Impedance Analyzer | Assesses body composition (fat-free mass, fat mass) through electrical impedance | Body composition assessment for specialized equations [20] [47] |
| Dual-Energy X-ray Absorptiometry | Precisely measures body composition including fat mass, lean mass, and bone mineral content | Gold standard body composition assessment for equation development [46] |
| Isotope Ratio Mass Spectrometer | Analyzes isotopic enrichment in biological samples for doubly labeled water studies | TEE measurement validation [46] |
The comparative analysis of equation structures reveals a clear trade-off between practical implementation and predictive accuracy. Weight-based models offer maximum practicality but demonstrate significant limitations in specialized populations and at BMI extremes. Height-inclusive models, particularly those relying on BMI, introduce systematic biases due to fixed assumptions about height-weight relationships. Body composition models provide superior physiological grounding and accuracy, especially in populations with abnormal body composition, but require more sophisticated measurement techniques.
The emerging evidence supports a paradigm shift toward more flexible modeling approaches that treat height and weight as independent, interacting variables rather than constraining them within fixed relationships like BMI [49] [50]. Furthermore, the development and application of population-specific equations demonstrate enhanced accuracy compared to generalized equations, highlighting the importance of matching equation selection to specific patient characteristics and clinical contexts.
For researchers and clinicians, the selection of appropriate predictive equations should consider the target population, available resources for measurement, and the required precision for the specific application. When precise energy expenditure assessment is critical for clinical decision-making or research outcomes, investment in direct measurement technologies or population-specific equations is strongly recommended.
Accurate estimation of resting energy expenditure (REE) is fundamental for nutritional assessment and intervention across clinical and healthy populations. Predictive equations offer a practical alternative to direct measurement techniques like indirect calorimetry, which, while highly accurate, is often inaccessible due to cost, technical requirements, and time constraints [26] [21]. However, the application of generalized predictive equations to distinct populations can lead to significant inaccuracies, resulting in either underfeeding or overfeeding, with critical implications for patient health outcomes and research integrity [26] [52] [21].
This guide evaluates the development and performance of predictive equations tailored for two specific populations: pediatric oncology patients and Saudi Arabian individuals. These case studies exemplify the methodological approaches required to create more accurate tools that account for unique physiological, body composition, and metabolic characteristics often not captured by equations derived from general populations.
Case Study 1: Pediatric Oncology Patients
Clinical Rationale and Development Protocol
Pediatric cancer patients present unique metabolic challenges. The disease process, coupled with treatments, can significantly alter energy expenditure and nutritional status, which in turn affects treatment tolerance, complication rates, and long-term outcomes [26] [20]. Malnutrition prevalence in this population ranges from 7% in leukemia to 50% in neuroblastoma at diagnosis [20]. A 2025 cross-sectional study aimed to develop the first REE prediction equations specifically for this vulnerable group [26] [20].
- Study Population: 203 treatment-naïve pediatric patients (aged 6 to <18 years) with recent oncological diagnoses. The cohort included solid tumors (68.5%), leukemia (20.2%), and brain tumors (11.3%) [26] [20].
- Experimental Measurements:
- REE Measurement: Resting energy expenditure was measured via indirect calorimetry (IC), the gold standard [26] [20].
- Anthropometrics: Weight, height, and multiple body circumferences were recorded using calibrated digital scales and stadiometers [20].
- Body Composition: Body composition was determined using bioelectrical impedance analysis [26] [20].
- Equation Development: Two new equations were derived using multiple regression analyses [26] [20]:
- INP-Simple Model: Based on basic clinical variables readily available in most settings.
- INP-Morpho Model: Incorporates body composition data for potentially enhanced accuracy.
The following workflow illustrates the experimental protocol for developing these population-specific equations:
Experimental Workflow for Pediatric Oncology REE Equation Development
Performance Comparison and Key Findings
The newly developed INP equations demonstrated superior performance compared to most historically used equations, showing less systematic bias in REE estimation for this specific population [26] [20].
Table 1: Performance Comparison of REE Predictive Equations in Pediatric Oncology Patients (vs. Indirect Calorimetry)
| Equation Name | Bias (kcal/day) | 95% Confidence Interval (kcal/day) | Notes |
|---|---|---|---|
| INP (New Models) | 114.8 | -408 to 638 | Least bias among tested equations [26] |
| Molnár | -82.3 | -741.3 to 576.7 | Closest performance to new INP equations [26] |
| Harris-Benedict | -133.6 | -671.5 to 404.2 | Overestimated measured REE [26] |
| Schofield | -185.4 | -697.6 to 326.8 | Significant underestimation [26] |
| FAO/WHO | -178.8 | -683.9 to 326.3 | Significant underestimation [26] |
| IOM/Oxford | -201 / -110.6 | -761.7 to 359.7 / -661.4 to 440.1 | Variable performance [26] |
A critical finding was that patients with brain tumors exhibited significantly lower REE per kilogram of body weight compared to those with other cancer types, underscoring the impact of diagnosis on metabolic rate and the need for specialized predictive tools [26] [20].
Case Study 2: The Saudi Population
Rationale and Methodological Approach
Previous REE and energy intake reference values for the Saudi population relied on generalized equations, such as Schofield's, which were found to overestimate requirements due to a lack of population-specific data [52] [21]. A 2019 study directly addressed this gap by developing the Almajwal–Abulmeaty (AA) equation, and a subsequent 2025 study updated the Average Requirement for Energy Intake (AR-EI) using a factorial approach and Saudi-specific growth charts [52] [21].
- Study Population: 427 healthy Saudi males and females (aged 18–57 years) representing the demographic spectrum, including normal weight, overweight, and obese individuals [21].
- Methodology:
- REE Measurement: REE was measured using indirect calorimetry (QUARK RMR, COSMED) [21].
- Anthropometrics & Body Composition: Comprehensive measurements included height, weight, and body composition via bioelectrical impedance analysis (TANITA BC-418) [21].
- Equation Development: The Almajwal–Abulmeaty (AA) equation was derived using stepwise linear regression. It incorporates Adjusted Body Weight (AdjWt), a calculation that adjusts for the difference between actual and ideal body weight, enhancing accuracy across BMI categories [21].
- Energy Requirement Calculation: The 2025 study used a mixed methodology, combining the doubly labeled water (DLW) data with a factorial approach that integrated Saudi-specific growth charts, anthropometric data, and the AA equation to calculate Total Energy Expenditure (TEE) as the AR-EI [52].
The logical process for establishing national energy requirements is summarized below:
Logic Flow for Saudi Population Energy Requirement Development
Performance and Outcomes
The Almajwal–Abulmeaty equation accounted for approximately 70% of the variance in measured REE (R² = 0.702), a substantial improvement over existing models [21]. The updated AR-EI values revealed significant overestimations in previous references, providing more accurate benchmarks for nutritional guidance and policy [52].
Table 2: Selected Energy Intake Reference Values (AR-EI) for the Saudi Population
| Age Group | Sex | AR-EI (kcal/day) | Key Inputs and Notes |
|---|---|---|---|
| Infants (0-6 mo) | Male | 393 | Based on Saudi growth chart data & energy deposition [52] |
| Infants (0-6 mo) | Female | 364 | Based on Saudi growth chart data & energy deposition [52] |
| Infants (12 mo) | Male | 778 | Based on Saudi growth chart data & energy deposition [52] |
| Infants (12 mo) | Female | 748 | Based on Saudi growth chart data & energy deposition [52] |
| Children/Adolescents | Both | 912 - 3147 | Varies greatly with age, sex, and activity level [52] |
| Adults (Normal Activity) | Male | 2270 | Uses AA equation for BMR, factorial approach for PAL [52] |
| Adults (Normal Activity) | Female | 1708 | Uses AA equation for BMR, factorial approach for PAL [52] |
| Adults (High Activity) | Male | 3153 | Uses AA equation for BMR, factorial approach for PAL [52] |
| Adults (High Activity) | Female | 2440 | Uses AA equation for BMR, factorial approach for PAL [52] |
The Scientist's Toolkit: Essential Research Reagents and Materials
The development of population-specific equations relies on a standardized set of tools and methodologies to ensure accuracy, reliability, and reproducibility.
Table 3: Essential Reagents and Solutions for REE Equation Research
| Item | Function/Application | Example Models/Types |
|---|---|---|
| Indirect Calorimeter | Gold-standard device for measuring REE by analyzing O₂ consumption and CO₂ production. | QUARK RMR (COSMED) [21] |
| Bioelectrical Impedance Analyzer (BIA) | Assesses body composition (fat-free mass, fat mass), a key determinant of REE. | TANITA BC-418 [21], SECA 813 [20] |
| Digital Scale | Precisely measures body weight, a fundamental variable in predictive equations. | SECA 813 [20] |
| Stadiometer | Accurately measures height, a fundamental variable in predictive equations. | SECA Model 206 [21], InLab S50 [20] |
| Anthropometric Tape | Measures body circumferences (waist, hip, arm), providing additional morphometric data. | SECA 201 [20] |
| Doubly Labeled Water (DLW) | Isotope-based method for measuring total energy expenditure in free-living individuals. | ²H₂O (Deuterium), H₂¹⁸O (Oxygen-18) [52] |
| Statistical Software | For data analysis, regression modeling, and equation derivation. | R, SPSS, SAS, Microsoft Excel SOLVER add-in [53] |
The case studies in pediatric oncology and the Saudi population consistently demonstrate that population-specific predictive equations for resting energy expenditure outperform generalized historical formulas. The primary drivers for this enhanced accuracy are the incorporation of population-specific anthropometric and body composition data, and the calibration of models against direct measurements (IC) within the target group.
These tailored approaches are critical for refining clinical nutritional support, shaping public health guidelines, and ensuring the validity of research outcomes. The continued development and validation of such equations across diverse global populations represent a vital step toward precision nutrition. Future research should focus on the external validation of new equations like the INP and AA models, and explore the integration of additional variables, such as biochemical markers and genetic factors, to further enhance predictive precision.
The accurate assessment of Resting Energy Expenditure (REE) is fundamental to establishing energy requirements in both clinical and research settings. REE represents the energy needed for vital bodily functions at rest and constitutes 60-70% of total daily energy expenditure for most individuals [47] [54]. While indirect calorimetry serves as the gold standard for REE measurement, its practical application is often limited by cost, time constraints, and required expertise [47]. Consequently, researchers develop predictive equations using statistical methods to estimate REE based on more readily available parameters such as body composition, age, sex, and anthropometric measurements.
The derivation and validation of these predictive equations follow rigorous statistical methodologies to ensure their accuracy and generalizability. This guide examines the statistical methods employed in equation derivation, focusing specifically on regression analysis techniques and validation approaches within REE research. By comparing methodologies across different population studies, we provide researchers with a comprehensive framework for evaluating, selecting, and developing appropriate predictive equations for specific populations and research contexts.
Statistical Foundations: Regression Analysis for Equation Derivation
Multiple Regression Analysis in REE Equation Development
Multiple regression analysis serves as the primary statistical method for developing predictive REE equations across diverse populations. This technique enables researchers to model the relationship between REE (dependent variable) and multiple predictor variables simultaneously, thereby creating equations that can estimate energy expenditure based on specific patient characteristics.
The general form of these predictive equations follows the model: REE = Constant + (Coefficient₁ × Variable₁) + (Coefficient₂ × Variable₂) + ... + (Coefficientₙ × Variableₙ). The selection of predictor variables varies by population but commonly includes fat-free mass (FFM), fat mass (FM), age, sex, weight, and height, with FFM consistently emerging as the strongest predictor across studies [51] [47] [55].
Table 1: Regression Equations for Different Populations
| Population | Predictive Equation | R/R² Value | Key Predictors |
|---|---|---|---|
| Japanese ILD Patients [51] | REE = 456.988 + 22.539 × FFM | Not specified | FFM |
| Children/Adolescents (Various BMI) [47] | REE = 505.412 + 24.383 × FFM | Adjusted R² = 0.649 | FFM |
| Physically Active Boys (Equation 1) [55] | REE = -196.49 + 9.25 × Height + 10.20 × Weight | R = 0.84 | Height, Weight |
| Physically Active Boys (Equation 2) [55] | REE = 359.45 - 23.69 × Age + 5.64 × Height + 20.36 × FFM | R = 0.86 | Age, Height, FFM |
The statistical workflow for developing these equations begins with measuring REE via indirect calorimetry and potential predictors through appropriate methods like bioelectrical impedance analysis for body composition. Researchers then employ multiple regression analysis to determine which predictors significantly contribute to REE variation, resulting in a predictive equation.
Diagram 1: Equation Development Workflow
Key Considerations in Regression Modeling
Several critical considerations influence the quality and utility of regression-derived REE equations. First, researchers must address model identification to ensure the number of parameters estimated does not exceed the information provided by measured variables, which would result in an underidentified model with no unique solution [56]. Second, sample size adequacy is crucial, with estimation procedures like Maximum Likelihood (ML) requiring larger samples, while Least Squares (LS) may perform better with smaller sample sizes [56].
The choice of estimation procedure also significantly impacts results. ML serves as the default estimator in most structural equation modeling software and requires large sample sizes but is robust to non-normal data distributions. LS minimization minimizes the sum of squared residuals between hypothesized and observed models, often performing better with smaller sample sizes when distribution assumptions are violated. Asymptotically Distribution Free (ADF) estimation may be appropriate for skewed data but requires very large sample sizes (200-500) for reliable estimates [56].
Validation Techniques for Predictive Equations
Core Validation Methodologies
Once developed, predictive equations require rigorous validation to assess their accuracy and clinical utility. Multiple validation approaches exist, each serving distinct purposes in evaluating equation performance.
Bland-Altman analysis represents a fundamental validation technique used to assess agreement between measured REE (via indirect calorimetry) and predicted REE (from equations). This method plots the differences between the two measurements against their means, allowing researchers to identify systematic biases (mean differences) and proportional errors (relationship between difference and magnitude) [51]. The absence of significant addition and proportional errors indicates better agreement, as demonstrated in the Japanese ILD patient study where the developed equation showed no significant systematic errors [51].
Cross-validation involves testing the predictive equation on a separate sample from the same population, as exemplified in the study of physically active boys where the equation developed on 184 boys was validated on a separate group of 148 boys [55]. This approach assesses how well the equation performs on new subjects and helps prevent overfitting.
Comparison of prediction accuracy across multiple existing equations determines whether newly developed equations offer improvements over established alternatives. Studies typically compare multiple equations against measured REE, calculating accuracy rates (percentage of predictions within ±10% of measured REE) to identify the best-performing equation for specific populations [47] [54].
Table 2: Validation Metrics Across Populations
| Population | Validation Method | Key Metrics | Performance Outcomes |
|---|---|---|---|
| Japanese ILD Patients [51] | Bland-Altman Analysis | Addition error, Proportional error, Agreement | No significant errors, 69.4% agreement |
| Children/Adolescents (Various BMI) [47] | Prediction Accuracy, RMSE | Accuracy rate, Root Mean Squared Error | New eq.: 64.8% accuracy (normal-weight), 59.6% (overweight) |
| Physically Active Boys [55] | Cross-validation | Bias, Cohen's d, Accuracy | Eq 1: 4.7% bias, 61.2% accuracy; Eq 2: 3.9% bias, 66.2% accuracy |
| Older Subjects [54] | Multiple Equation Comparison | Bias ± 2SD, Accuracy within ±10% | Aggregate eq.: >60% accuracy, no significant bias association |
Advanced Validation Frameworks
Beyond fundamental validation approaches, researchers employ advanced statistical frameworks to comprehensively evaluate predictive equations. Structural Equation Modeling (SEM) offers a powerful multivariate approach that combines factor analysis and multiple regression, allowing researchers to test complex relationships among variables while accounting for measurement error [56]. SEM includes both a structural model (relationships among latent variables) and a measurement model (relationships between measured and latent variables), providing a more comprehensive analytical approach.
The Aggregate algorithm represents another advanced validation approach that combines predictions from multiple equations to improve overall accuracy, particularly valuable in older populations where individual equations may show significant biases [54]. This method demonstrated higher overall accuracy for predicting REE in older subjects without significant association of measurement bias with age, BMI, or gender.
Diagram 2: Multi-Stage Validation Framework
Comparative Analysis of Methodological Approaches
Population-Specific Considerations
The performance of predictive equations varies significantly across different populations, necessitating population-specific development and validation. Key demographic and health factors influence which statistical approaches and predictor variables prove most effective.
For pediatric populations, age-specific considerations are crucial as body composition and metabolic rates change rapidly during growth. The study on children and adolescents with different BMIs found that prediction accuracy varied substantially across weight categories, with the newly developed equation and Schmelzle's equation performing best for normal and overweight children, while Lazzer's equation showed highest accuracy (44.9%) for obese participants [47]. This study also noted that Root Mean Squared Error (RMSE) values were consistently higher in obese groups compared to other BMI categories, indicating greater prediction error in this population.
In older subjects, equations must account for age-related metabolic changes. The validation study of 68 older subjects (age 60-94 years) found that the Aggregate, Müller, Harris-Benedict, and Fredrix equations predicted within ±10% of measured REE in more than 60% of subjects [54]. However, only the Aggregate equation showed no significant association of measurement bias with age, BMI, and gender, making it particularly suitable for this demographically diverse population.
For specialized populations such as athletes or patients with specific medical conditions, standard equations often prove inadequate. The study on physically active boys developed two new equations with different predictor variable combinations, finding that the equation incorporating age, height, and FFM (Equation 2) demonstrated slightly better accuracy (66.2% vs. 61.2%) than the equation based solely on height and weight [55]. Similarly, Japanese patients with interstitial lung disease required a population-specific equation based solely on FFM, which showed no systematic errors and higher agreement compared to existing equations [51].
Performance Metrics and Error Analysis
A comprehensive understanding of performance metrics is essential for evaluating predictive equations across studies. Common metrics include:
- Accuracy rate: Percentage of predictions falling within ±10% of measured REE
- Bias: Mean difference between predicted and measured REE
- Root Mean Squared Error (RMSE): Measure of prediction error magnitude
- Limits of Agreement: Range within which 95% of differences between predicted and measured REE fall (from Bland-Altman analysis)
- R/R² values: Strength of relationship between predictors and REE in development sample
Error analysis extends beyond simple accuracy rates to identify systematic patterns in prediction errors. For instance, many existing equations demonstrate proportional error, where the difference between predicted and measured REE changes with the magnitude of REE [51]. Additionally, researchers must examine whether prediction errors associate with demographic or clinical characteristics such as age, BMI, or body composition, which would limit the equation's generalizability across population subgroups.
Essential Research Reagents and Tools
The development and validation of REE predictive equations require specific research tools and methodologies. The following table outlines key resources essential for conducting this research.
Table 3: Essential Research Reagents and Solutions
| Research Tool | Specification/Model | Primary Function | Key Applications |
|---|---|---|---|
| Indirect Calorimeter | COSMED FitmatePro [47] [55] | REE measurement via oxygen consumption | Gold standard REE measurement for equation development and validation |
| Bioelectrical Impedance Analyzer | Tanita BC-420MA [47] | Body composition analysis (FFM, FM) | Provides predictor variables for regression analysis |
| Statistical Software | SPSS, R, SAS [57] [47] [58] | Multiple regression analysis, Bland-Altman analysis | Equation development, validation, and performance assessment |
| Body Composition Analyzer | Maltron-II Body Composition Analyzer [58] | Multi-frequency impedance measurement | RMR assessment and body composition analysis at different frequencies |
The derivation and validation of REE predictive equations rely on sophisticated statistical methodologies, primarily centered around multiple regression analysis for development and Bland-Altman analysis with cross-validation for performance assessment. The comparative analysis presented in this guide demonstrates that population-specific equations consistently outperform generalized formulas, emphasizing the necessity of developing and validating equations for target populations.
Key findings indicate that fat-free mass emerges as the strongest predictor across most populations, though the specific combination of optimal predictors varies by demographic and health characteristics. Validation metrics reveal that even the best-performing equations typically achieve accuracy rates of 60-70% within ±10% of measured REE, highlighting the continued need for indirect calorimetry when precise measurement is required.
Future methodological developments will likely incorporate more sophisticated statistical approaches such as structural equation modeling and machine learning techniques to improve prediction accuracy. Furthermore, standardized validation protocols across studies would enhance comparability and support more reliable equation selection for clinical and research applications.
Accurate estimation of resting energy expenditure (REE) is fundamental to developing effective nutritional interventions across diverse patient populations. While indirect calorimetry (IC) remains the gold standard for measuring REE, its clinical application is often limited by cost, accessibility, and operational constraints [59] [3]. Consequently, healthcare practitioners frequently rely on predictive equations to estimate energy requirements, though their accuracy varies substantially across different clinical scenarios and patient demographics.
The challenge lies in selecting the most appropriate equation for specific patient populations, as predictive accuracy can be significantly influenced by factors such as body composition alterations, metabolic disturbances, and physiological characteristics unique to certain disease states [3] [60]. This guide synthesizes current evidence to provide data-driven recommendations for equation selection across various clinical contexts, supported by comparative performance metrics and methodological protocols from validation studies.
Comparative Performance of REE Predictive Equations
Equation Performance in Severe Obesity
For patients with severe obesity, specialized equations demonstrate superior performance compared to general population formulas. A comprehensive validation study involving 780 adults with severe obesity evaluated 11 previously validated REE prediction equations against indirect calorimetry measurements [59].
Table 1: Performance of REE Predictive Equations in Severe Obesity (n=780)
| Equation Name | Bias Range (kcal) | Precision (% within ±10% of measured REE) | Systematic Bias at REE Extremes | Recommendation Level |
|---|---|---|---|---|
| Lazzer A (body weight-based) | -68.1 to 71.6 | Not exceeding 67.8% | Present | First-line |
| Horie-Waitzberg | -68.1 to 71.6 | Not exceeding 67.8% | Present | First-line |
| Body composition-based equations | Variable | Not superior to weight-based | Not assessed | Alternative |
| Other tested equations | Wider ranges | Lower precision | Not specified | Not recommended |
The study revealed that only the body weight-based Lazzer equations (Lazzer A) and the Horie-Waitzberg equation generated unbiased predictions across all subgroups [59]. Importantly, equations incorporating body composition measures did not predict REE better than body weight-based equations in this population. Despite being the best performers, even these recommended equations demonstrated systematic bias at extreme REE values and never achieved precision rates above 67.8%, highlighting the importance of direct measurement when possible [59].
Equation Performance in NAFLD and Type 2 Diabetes
Patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM) present unique metabolic challenges that impact REE prediction accuracy. A 2025 cross-sectional study evaluated ten commonly used predictive equations in 88 adults with NAFLD and T2DM, comparing predictions against indirect calorimetry measurements [3].
Table 2: Performance of REE Predictive Equations in NAFLD/T2DM (n=88)
| Equation Name | Average Bias (kcal/d) | 95% Confidence Interval | Accuracy (% within ±10% of measured REE) | Clinical Recommendation |
|---|---|---|---|---|
| FAO/WHO/UNU (weight) | 10.2 | -57.4 to 78 | 46.5% | Most recommended |
| Müller (FFM) | Not specified | Narrowest limits of agreement | Not specified | Good agreement |
| Thumb (25 × weight) | -402.2 | -477.3 to -327.1 | 20.4% | Not recommended |
| Owen | Significant underestimation | Not specified | Low | Not recommended |
The FAO/WHO/UNU equation using weight alone demonstrated the smallest average bias (10.2 kcal/d) and highest accuracy (46.5%) in this population [3]. Notably, all prediction equations provided REE estimates within 10% of measured values in less than 50% of cases, underscoring the limited precision of even the best-performing equations in this metabolic population. The Müller equation utilizing fat-free mass showed the narrowest limits of agreement, though specific accuracy data was not provided [3].
Equation Performance in Middle-Aged Adults by Weight Status
Weight status significantly influences the accuracy of REE predictive equations, as demonstrated by a study of 73 sedentary middle-aged adults that evaluated 33 different equations across normal-weight, overweight, and obese categories [60].
Table 3: Optimal Equation Selection by Weight Status in Middle-Aged Adults
| Weight Category | Most Accurate Equation | Prediction Accuracy (±10% of measured REE) | Alternative Equations |
|---|---|---|---|
| Normal-weight | FAO/WHO/UNU | 66.7% | Schofield (similar accuracy) |
| Overweight | Livingston | 46.9% | - |
| Obesity | Owen | 52.9% | - |
The FAO/WHO/UNU and Schofield equations both achieved 66.7% prediction accuracy in normal-weight individuals, though the FAO/WHO/UNU equation performed better at the more stringent ±5% accuracy threshold (50.0% accuracy) [60]. For overweight individuals, the Livingston equation provided the best performance, while the Owen equation was most accurate for those with obesity. This stratification highlights the importance of considering weight status when selecting predictive equations, even within the same age demographic.
Population-Specific Equation Development
For unique patient populations with distinct metabolic profiles, researchers have developed and validated custom equations to improve prediction accuracy:
Pediatric Oncology Patients: A study of 203 pediatric patients with recent oncological diagnoses developed two new REE prediction equations: the INP-simple model (based on basic clinical variables) and the INP-Morpho model (including body composition) [20]. Both new equations showed less bias in REE estimation compared to traditional equations, with the INP-simple model demonstrating a bias of 114.8 kcal (95% CI: -408, 638) versus -133.6 kcal for Harris-Benedict and -201 kcal for the IOM equation [20].
Physically Active Boys: For athletic pediatric populations, custom equations developed specifically for physically active boys demonstrated superior performance with average errors of 51±199 kcal for the equation using height and weight, and -39±193 kcal for the equation incorporating age, height, and fat-free mass [61]. These population-specific equations achieved accuracy rates of 61.2% and 66.2%, respectively, outperforming general pediatric equations [61].
Methodological Protocols for REE Equation Validation
Standardized Indirect Calorimetry Protocol
The validation studies cited in this guide employed rigorous methodological protocols to ensure reliable REE measurements:
Pre-test Conditions: Participants arrived at the laboratory in the morning (typically between 7:00-10:00 AM) after an overnight fast of 8-12 hours [3] [60]. They were instructed to avoid caffeine, tobacco products, and moderate- to high-intensity physical activity for 24 hours preceding the test [3].
Measurement Conditions: Testing occurred in a thermoneutral environment (22-25°C) with participants lying supine in a quiet, relaxing setting [61] [60]. Measurements began after a 30-minute rest period to ensure physiological stabilization [60].
Calorimetry Procedure: Respiratory gas exchange (VO₂ and VCO₂) was measured using calibrated metabolic carts (Cosmed Quark RMR or similar) for 20-30 minutes, with the first 5 minutes typically discarded to eliminate adaptation effects [61] [60]. A stable 5-minute steady-state period was selected for analysis, defined as <10% coefficient of variance in VO₂ consumption, VCO₂ production, and ventilation [60].
REE Calculation: The Weir equation was consistently applied to calculate REE from gas exchange measurements: REE = (3.9(VO₂) + 1.1(VCO₂)) × 1.44, assuming negligible urinary nitrogen excretion [60].
Statistical Validation Framework
The validation studies employed comprehensive statistical approaches to evaluate equation performance:
Bias Assessment: The mean difference between predicted and measured REE values (bias) was calculated along with 95% confidence intervals [59] [3]. Bland-Altman plots were generated to characterize bias across the range of measured REE values and identify systematic overestimation or underestimation patterns [59] [60].
Precision and Accuracy: Precision was defined as the percentage of the sample where equation estimates fell within ±10% of measured REE [59]. Some studies applied more stringent criteria (±5%) to identify the best-performing equations [60].
Agreement Statistics: Limits of agreement (bias ± 1.96 × SD), Pearson's correlation coefficients, and concordance correlation coefficients were calculated to assess agreement between predicted and measured values [61].
Key Research Reagents and Equipment
Table 4: Essential Research Materials for REE Validation Studies
| Equipment/Reagent | Specification | Primary Function | Example Models/Protocols |
|---|---|---|---|
| Indirect Calorimeter | Metabolic cart with VO₂/VCO₂ sensors | Direct REE measurement via respiratory gas analysis | Cosmed Quark RMR, CPX Ultima CardiO2 [61] [60] |
| BIA Analyzer | Multi-frequency bioelectrical impedance | Body composition assessment (FFM, FM) | Tanita MC-980 MA, BC-418 MA [61] [3] |
| Anthropometric Tools | Stadiometer, digital scale | Accurate height and weight measurements | SECA 213 stadiometer, SECA Alpha scale [61] [60] |
| Calibration Gases | Certified reference mixtures | Instrument calibration for accurate gas measurement | Manufacturer-specified concentrations [61] |
| Quality Control Protocols | Standard operating procedures | Measurement standardization and reproducibility | Steady-state criteria, pre-test conditions [60] |
The evidence synthesized in this guide demonstrates that optimal REE equation selection is highly dependent on specific patient characteristics and clinical scenarios. No single equation performs optimally across all populations, necessitating a tailored approach to equation selection.
For clinical practice, we recommend: (1) prioritizing population-specific equations when available; (2) recognizing that even the best equations rarely achieve precision exceeding 70%; (3) using indirect calorimetry whenever possible, particularly for patients at metabolic extremes or when precise energy prescription is critical [59]. Future research should focus on developing more robust equations for underrepresented populations and incorporating modern statistical approaches to improve prediction accuracy across diverse clinical settings.
Challenges and Optimization Strategies in REE Prediction
In the field of nutrition science and clinical practice, accurately estimating Resting Energy Expenditure (REE) is fundamental for developing effective dietary plans, nutritional support, and energy requirement guidelines for both healthy individuals and patient populations. REE represents the largest component of total daily energy expenditure, accounting for 60-75% of total energy expenditure in most individuals [62]. The reference standard for measuring REE is indirect calorimetry (IC), a non-invasive method based on measuring oxygen consumption (VO₂) and carbon dioxide production (VCO₂) [6] [63]. However, due to the high cost, time-consuming nature, and limited availability of IC equipment, healthcare professionals and researchers predominantly rely on predictive equations to estimate REE [6] [60].
These predictive equations, derived from statistical regression analyses of population data, typically incorporate variables such as weight, height, age, and sex, with some more advanced equations also including body composition metrics like fat-free mass (FFM) [63]. The persistent challenge lies in the systematic overestimation and underestimation patterns that emerge when these equations are applied to individuals whose characteristics differ significantly from the original validation cohorts. Understanding these pitfalls is essential for researchers, clinicians, and drug development professionals who depend on accurate energy expenditure estimates for nutritional planning, clinical interventions, and pharmaceutical development related to metabolism.
Methodological Foundations and Measurement Standards
Gold Standard Measurement: Indirect Calorimetry
The validity of all REE predictive equations is established through comparison with indirect calorimetry measurements, which must adhere to strict standardized protocols to ensure accuracy and reliability. The fundamental principle underlying IC is the relationship between gas exchange and energy production, calculated using the abbreviated Weir equation [63] [60]:
REE (kcal/day) = [(VO₂ × 3.941) + (VCO₂ × 1.11)] × 1,440
Standard experimental protocols for measuring REE require:
- 12-hour overnight fasting to eliminate the thermic effect of food [6] [60]
- 24-48 hours without intense physical activity to minimize excess post-exercise oxygen consumption [60]
- Measurement performed in the morning in a thermo-neutral environment [6]
- 30 minutes of rest in a supine position before measurement [62]
- A quiet environment with dim lighting and controlled temperature [6]
- Use of a steady-state period (typically 5-20 minutes) where variations in VO₂ and VCO₂ are minimal [60] [62]
Statistical Frameworks for Evaluating Equation Performance
The assessment of predictive equation accuracy relies on specific statistical metrics that quantify the magnitude and direction of estimation errors:
- Mean Error (Bias): Systematic overestimation (positive values) or underestimation (negative values) [60]
- Accuracy Rate: Percentage of predictions falling within ±10% of measured REE [60] [62]
- Intraclass Correlation Coefficient (ICC): Measure of reliability between predicted and measured values [6]
- Limits of Agreement: Statistical range (mean difference ±1.96 SD) where most differences between measured and predicted values lie [62]
The concept of underspecified models in regression analysis is particularly relevant to understanding why predictive equations fail when applied to new populations. An underspecified model omits important predictor variables, resulting in biased regression coefficients and biased predictions [64]. In the context of REE prediction, this occurs when equations developed for general populations lack critical variables needed for specific subpopulations, such as body composition metrics for athletic populations [63].
Comparative Performance of Major Predictive Equations
The most widely used REE predictive equations in research and clinical practice include:
Table 1: Major REE Predictive Equations and Their Formulations
| Equation | Year | Formula (Male) | Formula (Female) |
|---|---|---|---|
| Harris-Benedict | 1919 | 66.47 + (13.75 × W) + (5 × H) - (6.75 × A) | 655.10 + (9.56 × W) + (1.85 × H) - (4.68 × A) |
| Mifflin-St Jeor | 1990 | (10 × W) + (6.25 × H) - (5 × A) + 5 | (10 × W) + (6.25 × H) - (5 × A) - 161 |
| WHO/FAO/UNU | 1985 | (11.6 × W) + 879 [WHO1] OR (11.3 × W) + (16 × H) + 901 [WHO2] | (8.7 × W) + 829 [WHO1] OR (8.7 × W) - (25 × H) + 865 [WHO2] |
| Owen | 1986/1987 | 879 + (10.2 × W) | 795 + (7.18 × W) |
| Cunningham | 1980 | 500 + (22 × FFM) | 500 + (22 × FFM) |
W = weight (kg); H = height (cm); A = age (years); FFM = fat-free mass (kg) [6] [42] [65]
Systematic Overestimation and Underestimation Patterns Across Populations
The performance of predictive equations varies substantially across different population groups, with clear patterns of systematic overestimation and underestimation emerging based on body composition, age, and training status.
Table 2: Equation Accuracy Across Different Population Subgroups
| Population | Most Accurate Equation(s) | Accuracy Rate | Systematic Bias Pattern |
|---|---|---|---|
| Overweight/Obese Adults (BMI ≥25) | Harris-Benedict, WHO1, WHO2 | High ICC, low mean difference | General underestimation trend; Mifflin and Owen showed significant underestimation (p<0.05) [6] |
| Non-Obese Adults | Mifflin-St Jeor | 82% within ±10% of IC | Errors evenly distributed between under- and overestimation [65] |
| Obese Adults | Mifflin-St Jeor | 70% within ±10% of IC | Underestimation more frequent than overestimation [65] |
| Master Athletes | De Lorenzo | Closest to measured REE (p<0.005) | Standard equations (H&B, WHO, Müller) significantly underestimated REE [63] |
| Middle-Aged Normal Weight | FAO/WHO/UNU | 50.0% prediction accuracy (±5%) | Variable performance across weight categories [60] |
| Middle-Aged Overweight | Livingston | 46.9% prediction accuracy (±5%) | Variable performance across weight categories [60] |
| Middle-Aged Obese | Owen | 52.9% prediction accuracy (±5%) | Variable performance across weight categories [60] |
| Chinese Young Adults | Owen, Mifflin, Liu's | Least bias in Bland-Altman analysis | Harris-Benedict and WHO significantly overestimated REE (p<0.01) [62] |
The experimental data reveal that no single predictive equation performs optimally across all population subgroups. The Mifflin-St Jeor equation demonstrates the most consistent performance across normal weight and obese populations [65], while population-specific equations like De Lorenzo for athletes [63] and Owen for obese middle-aged adults [60] outperform general equations in their respective subgroups.
Critical Analysis of Equation Performance in Specialized Populations
The Impact of Body Composition and Physical Activity
Body composition, particularly fat-free mass (FFM), represents the most metabolically active tissue and serves as the primary determinant of REE, accounting for 60-70% of its variance [63]. The failure of standard equations to account for variations in body composition beyond weight and height explains much of the systematic bias observed in specialized populations:
Master Athletes: This population maintains higher FFM compared to sedentary age-matched controls, resulting in systematic underestimation of REE by standard equations that incorporate age as a negative predictor without accounting for preserved FFM [63]. Equations that incorporate FFM directly (Cunningham) or were developed specifically for athletic populations (De Lorenzo) demonstrate superior accuracy.
Obese Populations: The accuracy of all predictive equations decreases in obese individuals compared to non-obese adults, with the Mifflin-St Jeor equation maintaining the highest accuracy (70% within ±10% of IC vs. 82% in non-obese) [65]. The systematic underestimation pattern in obese individuals may reflect metabolic adaptations or limitations of equations that cannot adequately account for the metabolic contribution of adipose tissue and its associated metabolic activity.
Ethnic and Geographical Considerations
Predictive equations developed primarily from Caucasian populations may demonstrate systematic biases when applied to other ethnic groups. Research on Chinese young adults revealed that the Harris-Benedict and WHO equations significantly overestimated REE (p<0.01), while the Owen, Mifflin, and Liu's equations showed no significant difference from measured REE [62]. This highlights the ethnic-specific metabolic differences that necessitate validation of predictive equations within target populations before application in research or clinical practice.
The following diagram illustrates the decision pathway for selecting appropriate REE predictive equations based on population characteristics:
Analytical Framework for Understanding Estimation Biases
The systematic overestimation and underestimation patterns observed in REE predictive equations can be understood through the statistical framework of model specification errors [64]:
Underspecified Models: Standard REE equations are often underspecified for specialized populations because they omit crucial variables like detailed body composition metrics, metabolic characteristics, or ethnic-specific factors. This omission leads to biased regression coefficients and biased predictions [64], explaining why equations perform poorly when applied to populations different from their derivation cohorts.
Impact of Low Reliability: When outcome measurement reliability is suboptimal (as with single measurements of REE without repeated assessments), there is a tendency to overestimate true outcome rates, particularly when the true prevalence of extreme values is low [66]. This measurement error contributes to the systematic biases observed in validation studies.
The following experimental workflow outlines a standardized protocol for validating predictive equations against indirect calorimetry:
Essential Research Reagents and Methodological Tools
Table 3: Essential Research Materials for REE Validation Studies
| Category | Specific Tool/Equipment | Function & Purpose | Technical Specifications |
|---|---|---|---|
| Energy Expenditure Measurement | Metabolic Cart (e.g., Quinton QMC, Ultima PFX) | Gold standard measurement of VO₂ and VCO₂ for indirect calorimetry | Precision gas analyzers, calibrated flow sensors, mixing chamber system [6] [62] |
| Anthropometric Assessment | Electronic Scale (e.g., SECA Alpha) | Accurate body weight measurement | Capacity 150kg, precision 0.1kg [6] [60] |
| Anthropometric Assessment | Wall-Mounted Stadiometer (e.g., SECA 220) | Accurate height measurement | Precision 0.1cm [6] [60] |
| Body Composition Analysis | DXA Scanner (e.g., HOLOGIC Discovery) | Measurement of fat-free mass and fat mass | Enables FFM-based equation calculation [60] |
| Environmental Control | Environmental Monitoring System | Control of ambient temperature and humidity | Critical for standardized conditions [6] [60] |
| Data Analysis | Statistical Software (e.g., SPSS) | Performance of Bland-Altman analysis, ICC, bias calculations | Enables comprehensive accuracy assessment [6] [60] [62] |
The systematic patterns of overestimation and underestimation in REE predictive equations represent a significant methodological challenge in nutrition science, clinical practice, and pharmaceutical research. The evidence consistently demonstrates that population-specific factors including body composition, physical activity status, age, and ethnicity significantly impact equation accuracy. Researchers and clinicians must recognize these limitations and select equations based on the specific characteristics of their target population rather than relying on a universal formula.
Future research should focus on developing and validating specialized equations for distinct subpopulations, particularly those with extreme body compositions, athletic training backgrounds, or specific ethnic backgrounds. Additionally, incorporating novel predictors such as body composition metrics from advanced imaging techniques, metabolic biomarkers, or genetic factors may enhance prediction accuracy beyond traditional anthropometric measures. Until such advances are realized, the critical application of existing equations with awareness of their systematic biases and limitations remains essential for generating valid, reproducible research findings and implementing effective clinical nutritional interventions.
Accurate estimation of Resting Energy Expenditure (REE) is a cornerstone of nutritional therapy and metabolic research. While indirect calorimetry represents the gold standard for measurement, predictive equations are widely used in clinical and research settings due to their practicality. However, the performance of these equations varies significantly across different body mass index (BMI) categories, presenting a critical challenge for practitioners and researchers. This guide systematically evaluates the performance variations of REE predictive equations across BMI categories, providing researchers, scientists, and drug development professionals with evidence-based recommendations for selecting appropriate equations based on weight status.
Comparative Performance of REE Equations Across BMI Categories
The accuracy of REE predictive equations is significantly influenced by a patient's weight status. The following table synthesizes performance data from multiple validation studies across BMI categories.
Table 1: Performance of REE Predictive Equations Across BMI Categories
| BMI Category | Most Accurate Equations | Accuracy Rate | Key Limitations | Supporting Evidence |
|---|---|---|---|---|
| Severe Obesity (BMI ≥ 35) | Lazzer A, Horie-Waitzberg | <67.8% precision | Systematic bias at REE extremes; all equations show low precision | [59] |
| Obesity (BMI 30-35) | Harris-Benedict (1918) | Best performance in subgroup | Overestimation by HB and others in BMI≥30 | [48] [67] |
| Overweight (BMI 25-30) | WHO (weight & height), Korth, Weijs & Vansant | 45-49% accurate | Moderate accuracy across studies | [67] |
| Normal Weight (BMI 18.5-25) | WHO (weight & height), Korth, Custom Equation* | 49% accurate | Performance improves with BMI-specific equations | [67] |
| Underweight (BMI < 18.5) | WHO (weight & height), Korth | Best performance in subgroup | Underestimation by HB and MSJ | [48] [67] |
*Custom Equation for BMI <25: REE = 11.355 × weight (kg) + 7.224 × height (cm) - 4.649 × age (y) + 135.265 × sex - 137.475 [67]
The data consistently demonstrates that no single equation performs optimally across all BMI categories. For patients with severe obesity, even the best-performing equations show concerning limitations, with precision rates never exceeding 67.8% [59]. This systematic bias is particularly pronounced at extreme REE values, highlighting the fundamental challenges in predicting energy expenditure in this population.
Detailed Methodologies of Key Validation Studies
Utah Obesity Study (Severe Obesity)
Objective: To determine which REE prediction equations estimate with the least bias and most precision in participants with severe obesity [59].
Population: 632 females and 148 males with severe obesity from the Utah Obesity Study.
Measurement Protocol:
- REE measured by indirect calorimetry
- Testing conducted after overnight fast
- Participants rested in supine position for at least 30 minutes before measurement
- Environmental controls: thermoneutral, quiet environment
Analytical Approach:
- 11 previously validated REE prediction equations tested
- Equations considered unbiased if mean predicted REE did not differ significantly (P > 0.05) from measured values
- Precision defined as percentage of sample where equation estimate was within 10% of measured REE
- Bland-Altman plots characterized bias across measured REE values
- Subgroup analyses by sex and BMI
Hospital Patient Validation Study (All BMI Categories)
Objective: To examine the validity of REE predictive equations for underweight, normal weight, overweight, and obese inpatients and outpatients by comparison with indirect calorimetry [67].
Population: 513 general hospital patients (253 F, 260 M), 237 inpatients and 276 outpatients.
Measurement Protocol:
- Indirect calorimetry performed using metabolic monitors (Deltatrac 2 MBM-200 or Vmax Encore n29)
- Devices calibrated daily before use
- Patients measured in supine position after at least 2 hours of fasting
- Body weight measured using calibrated electronic stand-up scale
- Height measured or self-reported
Analytical Approach:
- 15 predictive equations evaluated plus fixed factors (25 kcal/kg/day, 30 kcal/kg/day)
- Prediction between 90-110% of measured REE considered accurate
- Bias (mean percentage error) and root-mean-square-error (RMSE) calculated
- Subgroup analysis by BMI category
- New equation developed for BMI <25 population
REE Equation Selection Framework
The relationship between BMI category and equation performance follows a logical workflow that can guide clinical and research decisions.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 2: Essential Research Materials for REE Validation Studies
| Tool Category | Specific Examples | Research Function | Key Considerations |
|---|---|---|---|
| Indirect Calorimeters | Deltatrac 2 MBM-200, Vmax Encore n29, Fitmate Calorimeter | Gold standard REE measurement via O₂ consumption/CO₂ production | Require regular calibration; measurement duration 15-20 min after 5 min stabilization [3] [67] |
| Body Composition Analyzers | Tanita BC 418 MA Segmental Body Composition Analyzer, BIA devices | Assess fat-free mass (FFM) and fat mass (FM) for body composition-based equations | FFM is strong REE predictor (R²=0.64); enhances equation accuracy [42] [3] |
| Anthropometric Equipment | Calibrated electronic scales, stadiometers | Provide accurate weight and height measurements for equation inputs | Digital scales with 0.1kg precision; trained personnel reduce measurement error [68] [67] |
| * Predictive Equations* | Harris-Benedict, Mifflin-St. Jeor, WHO, Lazzer, Horie-Waitzberg | Estimate REE when direct measurement unavailable | Selection depends on BMI category, population characteristics, and clinical context [59] [67] |
| Calibration Tools | Reference gas mixtures (O₂, CO₂), calibration weights | Ensure measurement accuracy and equipment reliability | Daily calibration essential for valid results; quality control protocols [67] |
Discussion and Clinical Implications
The evidence consistently demonstrates that weight status significantly impacts the accuracy of REE predictive equations. This variation stems from metabolic differences between BMI categories and the distinct body composition characteristics that influence energy expenditure. Researchers and clinicians must consider these performance variations when selecting equations for specific populations.
For research involving drug development or metabolic studies, these findings highlight the importance of either using BMI-appropriate equations or investing in indirect calorimetry equipment. The systematic bias observed at BMI extremes [59] [48] suggests that pharmaceutical trials involving patients with severe obesity should prioritize direct measurement to avoid misestimating energy requirements that could impact study outcomes.
Future research directions should focus on developing more sophisticated prediction models that incorporate body composition data, biomarkers, and potentially machine learning approaches to improve accuracy across diverse populations. The emergence of phase angle from bioelectrical impedance analysis as a promising predictor in athletic populations [69] suggests potential for innovative approaches in obese populations as well.
Accurately estimating resting energy expenditure (REE) is fundamental to designing effective nutritional support for patients. However, this task becomes particularly challenging in special populations, such as those with cancer and cachexia, where the disease itself can cause significant metabolic alterations. This guide objectively compares the performance of various REE predictive equations against the gold standard, indirect calorimetry, in these complex patient groups.
Table of Contents
- REE Prediction in Cancer and Cachexia: A Performance Comparison
- Experimental Protocols in REE Research
- Key Metabolic Pathways and Workflows
- The Scientist's Toolkit: Research Reagent Solutions
REE Prediction in Cancer and Cachexia: A Performance Comparison
The following tables summarize the performance of various REE predictive equations across different patient populations, based on validation studies that compared predicted values to REE measured by indirect calorimetry.
Table 1: Performance of REE Predictive Equations in Adult Cancer and Severe Obesity
| Population / Study | Most Accurate Equation(s) | Key Findings and Limitations |
|---|---|---|
| Severe Obesity [59] | Lazzer A, Horie-Waitzberg | • Only these two equations generated unbiased predictions across all subgroups.• Systematic bias was observed, particularly at extreme REE values.• Precision never exceeded 67.8% (percentage of estimates within 10% of measured REE). |
| General Hospital Patients (Incl. Oncology) [28] | Korth, WHO (weight & height), new local equation | • The best-performing equations were accurate in only 49% of patients.• The original Harris & Benedict (1918) equation performed best for obese patients (BMI ≥30). |
| Korean Non-Obese Adults [70] | New local equation, FAO/WHO/UNU (weight) | • The newly developed equation showed 71% accuracy.• The FAO/WHO/UNU equation was the best published equation, with 70% accuracy. |
| NAFLD & Type 2 Diabetes [3] | FAO/WHO/UNU (weight) | • This equation had the smallest average bias (10.2 kcal/day).• However, its accuracy was low (46.5%), and no equation was accurate for more than half of the patients. |
Table 2: Performance of REE Predictive Equations in Pediatric and Other Adult Populations
| Population / Study | Most Accurate Equation(s) | Key Findings and Limitations |
|---|---|---|
| Pediatric Oncology [20] | INP-simple, INP-Morpho, Molnár | • Two new population-specific equations (INP-simple and INP-Morpho) showed less bias than most established equations.• This highlights the need for equations tailored to specific clinical populations. |
| Middle-Aged Adults (by Weight Status) [60] | FAO/WHO/UNU (Normal-weight), Livingston (Overweight), Owen (Obese) | • Different equations performed best depending on the patient's weight status.• Accuracy rates ranged from 46.9% to 52.9%, reinforcing that a "one-size-fits-all" equation does not exist. |
| Obese Adults [71] | Robertson & Reid (1952), Fleisch (1951) | • In this older study, these two equations were recommended for clinical use with obese patients.• Most other equations accounted for only 56-63% of the variance in measured REE. |
Experimental Protocols in REE Research
To ensure the validity and reliability of REE data, studies comparing predictive equations to indirect calorimetry follow rigorous experimental protocols. The following workflow visualizes the key stages of a typical validation study, as detailed across multiple sources [59] [20] [70].
Detailed Methodology Breakdown:
Subject Recruitment & Pre-Test Standardization: Participants are recruited based on specific inclusion criteria (e.g., confirmed diagnosis, age range, treatment-naïve status) [20]. Critical pre-test conditions are strictly enforced to ensure basal state measurements:
- Fasting: An 8- to 12-hour overnight fast is standard to ensure post-absorptive conditions [3] [60].
- Activity Restriction: Participants are instructed to avoid moderate- or high-intensity physical activity for 24-48 hours before the test [60].
- Substance Avoidance: Caffeine, tobacco, and medications affecting metabolism are restricted prior to testing [20] [3].
Anthropometric and Body Composition Measurements: Precise physical data is collected, which is essential for both the development and application of predictive equations.
- Measurements: Weight, height, and various circumferences (e.g., waist, hip) are taken [20].
- Body Composition: Advanced techniques like Bioelectrical Impedance Analysis (BIA) [25] [20] or Dual-Energy X-ray Absorptiometry (DXA) [60] are used to determine fat-free mass and fat mass, which are variables in some predictive equations.
Indirect Calorimetry Measurement: The gold standard REE measurement is performed.
- Environment: Tests are conducted in a quiet, thermoneutral room (e.g., 22°C) with the participant in a supine position, awake and relaxed [3] [60].
- Instrumentation: A metabolic cart (e.g., Fitmate, ParvoMedics, Deltatrac) with a ventilated canopy or facemask is used [70] [28] [3].
- Calibration: The device is calibrated daily with standard reference gases before use [70] [28].
- Procedure: After a rest period, gas exchange (VO₂ and VCO₂) is measured for 15-30 minutes. The first 5-10 minutes are often discarded to allow for acclimatization, and a stable 5-10 minute "steady-state" period is used for calculations [70] [60].
Data Calculation and Statistical Analysis: REE is calculated from gas exchange data using the abbreviated Weir equation [70] [3] [60]:
REE (kcal/day) = (3.941 × VO₂ L/min + 1.106 × VCO₂ L/min) × 1440. Predicted REE values are computed using selected equations. Statistical comparisons focus on:
Key Metabolic Pathways and Workflows
Cancer cachexia is characterized by a progressive loss of skeletal muscle mass. The metabolic cost of the tumor itself is a key driver of this process. The following diagram illustrates how a tumor's energy metabolism, particularly its reliance on anaerobic glycolysis (the Warburg effect), creates a significant energetic burden on the host, leading to negative energy balance and muscle wasting [72].
Logical Workflow for Selecting a Predictive Equation in Clinical Research:
Given the documented inaccuracies of predictive equations, researchers and clinicians need a logical framework to select the most appropriate tool when indirect calorimetry is unavailable. The following diagram outlines this decision-making process.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and equipment used in REE research, as cited in the reviewed literature.
Table 3: Key Research Reagents and Equipment for REE Studies
| Item | Function in REE Research | Examples / Specifications |
|---|---|---|
| Indirect Calorimeter | Measures oxygen consumption (VO₂) and carbon dioxide production (VCO₂) to calculate energy expenditure. | TrueOne 2400 (ParvoMedics) [70], Deltatrac II (Datex-Ohmeda) [28], Vmax Encore (Viasys) [28], Fitmate (Cosmed) [3], CPX Ultima (Medical Graphics) [60]. |
| Calibration Gases | Used for daily calibration of the indirect calorimeter to ensure measurement accuracy. | Gas mixtures (e.g., 95% O₂, 5% CO₂; or 16% O₂, 4% CO₂) [28]. |
| Bioelectrical Impedance Analysis (BIA) | Assesses body composition (fat-free mass, fat mass) which is a key variable in many predictive equations and research models. | InBody 720 [70], Tanita BC-418 MA [3], SECA instruments [20]. |
| Dual-Energy X-Ray Absorptiometry (DXA) | Research-grade method for precise measurement of body composition, including lean and fat mass. | Hologic Discovery [60]. |
| Stadiometer & Scale | Precisely measures height and weight, which are fundamental inputs for all predictive equations. | SECA stadiometers and scales [20] [60]. |
| Stable Isotope Tracers | Used in advanced metabolic research to trace substrate utilization (e.g., uniformly labeled ¹³C-glucose to study tumor metabolism) [72]. | ¹³C-glucose. |
Accurate prediction of resting energy expenditure (REE) is fundamental to developing effective nutritional support strategies in clinical and research settings. The gold standard for measuring REE is indirect calorimetry, but its use is often limited by cost, technical expertise, and time constraints [73]. Consequently, healthcare professionals and researchers frequently rely on prediction equations to estimate energy needs.
Many historically established and widely used REE prediction equations, such as the Harris-Benedict, Schofield, and Mifflin-St Jeor equations, were developed primarily on populations of European descent [73]. The application of these "Eurocentric" equations to diverse ethnic and demographic groups presents significant limitations, as factors such as body composition, metabolic characteristics, and anthropometrics can vary substantially across different populations [73] [74]. This guide objectively compares the performance of these conventional equations against newer, population-specific alternatives, providing experimental data to inform their use in research and drug development.
Comparative analysis of prediction equation performance
Experimental evidence from Asian older adults with multimorbidity
A 2025 multicenter, cross-sectional study of 400 hospitalized Asian patients aged ≥65 years provides direct evidence for the limitations of Eurocentric equations. The study measured REE via indirect calorimetry and compared the performance of established equations against novel, population-specific prediction equations (PEs) [73].
Table 1: Performance Metrics of REE Prediction Equations in Asian Older Adults
| Prediction Equation Type | Root Mean Square Error (RMSE) | Intraclass Correlation Coefficient (ICC) | Key Predictor Variables |
|---|---|---|---|
| Novel Equations (2025) | 186–191 kcal/day | 0.50–0.52 | Age, Weight, Height, Sex, MUAC, CC |
| Conventional Equations | 222–258 kcal/day | 0.27–0.46 | Age, Sex, Weight, Height |
| MUAC: Mid-upper arm circumference; CC: Calf circumference [73]. |
The novel equations, which incorporated measures of muscle mass such as mid-upper arm circumference (MUAC) and calf circumference (CC), demonstrated superior accuracy and stronger reliability compared to all conventional equations tested [73]. This highlights the critical importance of including ethnically relevant anthropometric measures when developing predictive models.
Validation studies in other non-European populations
Research in other demographic groups reinforces the necessity of population-specific equations. A 2025 study from South Africa validated various fat mass (FM) prediction equations in children aged 5-8 years of Black African ethnic origins [74].
Table 2: Performance of Selected Fat Mass Prediction Equations in South African Children
| Study (Equation) | R² (%) | Root Mean Square Error (RMSE) | Predictor Categories |
|---|---|---|---|
| Britz et al. (2017) | 89.0% | Not specified | Skinfold thickness |
| Wendel et al. (2016) | Not specified | 1.1 kg | Skinfold thickness |
| Hudda et al. (2019) | High (Specific value not reported) | 1.4 kg | Basic Anthropometry* |
| Ramirez et al. (2012) | Not specified | Not specified | Bioelectrical Impedance Analysis (BIA) |
| Horlick et al. (2002) | Not specified | 3.4 kg | Bioelectrical Impedance Analysis (BIA) |
| BIA Manufacturer Equation | 58.3% | Not specified | Bioelectrical Impedance Analysis (BIA) |
| Basic anthropometry includes weight, height, sex, age, and ethnicity [74]. |
The study concluded that equation performance varied considerably upon external validation, with the Hudda et al. equation—which uses readily available data including ethnicity—showing some of the best performance [74]. Similarly, a 2025 study developing a new equation for a Brazilian population with overweight and obesity found that most existing equations were not valid for that specific group, further underscoring the need for targeted equation development [75].
Experimental protocols for equation development and validation
Protocol for REE equation development in older Asian adults
The following workflow details the methodology used to develop and validate novel REE prediction equations for multi-ethnic Asian older adults [73]:
Diagram 1: Workflow for REE Equation Development. SGA: Subjective Global Assessment; MUAC: Mid-upper arm circumference; REE: Resting energy expenditure; RMSE: Root mean square error; ICC: Intraclass correlation coefficient.
Key methodological details
- REE Measurement: Conducted using the Q-NRG indirect calorimetry machine after an overnight fast (6-8 hours) and 10-15 minutes of rest in a supine position. Measurements occurred in a quiet, temperature-controlled environment (23-25°C) [73].
- Anthropometric Measurements: Included body weight, height, mid-upper arm circumference (MUAC), and calf circumference (CC) using standardized techniques and equipment [73].
- Statistical Analysis: Multivariate generalized linear models and restricted cubic splines were used. The final four models were derived through backward elimination and assessed for collinearity using variance inflation factor (VIF) analysis [73].
Protocol for body composition prediction equation validation
The following methodology was employed to validate fat mass prediction equations in South African children, representing a robust approach for external validation [74]:
Diagram 2: Validation Workflow for Body Composition Equations. BIA: Bioelectrical impedance analysis; FM: Fat mass; RMSE: Root mean square error.
Key methodological details
- Reference Method: Deuterium dilution technique was used as the reference standard for measuring fat mass, with participants fasting overnight and providing saliva samples pre-dose and at 2- and 3-hours post-dose [74].
- Equation Selection: Identified through systematic reviews, including only equations developed on populations >100 individuals with both males and females [74].
- Performance Metrics: Validation statistics included R², calibration (slope and calibration-in-the-large), and root mean square error (RMSE) to assess agreement between predicted and observed values [74].
The scientist's toolkit: Essential research reagents and materials
Table 3: Key Materials and Methods for Predictive Equation Research
| Item/Technique | Primary Function | Specific Examples | Application Notes |
|---|---|---|---|
| Indirect Calorimeter | Gold standard REE measurement | Q-NRG (COSMED Ltd.) | Requires regular calibration; standardized patient preparation essential [73] |
| Bioelectrical Impedance Analyzer | Estimates body composition via electrical resistance | Bodystat 1500MDD; Akern 101; TELELAB | Device-specific equations needed; hydration status affects accuracy [74] [76] [75] |
| Anthropometric Tools | Measures body dimensions for equations | SECA 952 chair scales; anthropometric tape | Standardized protocols critical for reliability [73] [74] |
| Reference Body Composition Methods | Validates new prediction equations | Deuterium dilution; DXA; ADP | Deuterium dilution considered reference for fat mass in validation studies [74] |
| Statistical Software | Develops and validates prediction models | Stata; R | Requires capabilities for regression, cross-validation, and bias analysis [73] [74] |
Experimental evidence consistently demonstrates that Eurocentric REE and body composition prediction equations show significantly reduced accuracy when applied to diverse ethnic and demographic groups. The development of population-specific equations that incorporate relevant anthropometric variables—such as mid-upper arm circumference and calf circumference—substantially improves prediction accuracy [73]. Researchers and clinicians should select prediction equations developed and validated in populations that closely match their target demographic, or develop new, context-specific equations when existing models demonstrate poor performance in validation studies [73] [74] [75]. Future research should focus on expanding these validation efforts across more diverse populations and developing more adaptable prediction models that account for ethnic and demographic variations in body composition and metabolism.
Accurate assessment of resting energy expenditure (REE) is fundamental for nutritional research and clinical practice, particularly in the management of metabolic diseases, obesity, and patient care. While indirect calorimetry (IC) remains the gold standard for measuring REE, its clinical application is often limited by cost, operational complexity, and accessibility barriers [77] [60]. Consequently, predictive equations based on readily available parameters such as weight, height, age, and sex have become the predominant method for REE estimation in both research and clinical settings.
The central challenge in REE prediction lies in the inherent biological variability across different populations. Factors including body composition, health status, and age significantly influence metabolic rate, rendering universally applicable equations largely ineffective [78] [79]. This comprehensive review systematically compares the performance of established and novel predictive equations, with specific focus on weight adjustment methodologies and population-specific modifications that enhance predictive accuracy across diverse demographic and clinical cohorts.
Comparative Performance of REE Predictive Equations
Extensive research has evaluated the accuracy of REE predictive equations against indirect calorimetry across populations with varying body mass indices, age groups, and clinical conditions. Performance varies considerably, underscoring the necessity for context-specific equation selection.
Performance in Normal-Weight, Overweight, and Obese Adults
Weight status significantly influences the accuracy of REE predictive equations, as demonstrated by a 2018 study of 73 sedentary middle-aged adults that evaluated 33 different equations [77] [60].
Table 1: Accuracy of REE Predictive Equations by Weight Status in Middle-Aged Adults
| Weight Category | Most Accurate Equation | Prediction Accuracy | Key Findings |
|---|---|---|---|
| Normal-weight (BMI 18.5-24.9) | FAO/WHO/UNU | 50.0% | Schofield equation showed similar accuracy (66.7% at ±10% threshold) |
| Overweight (BMI 25-29.9) | Livingston | 46.9% | Demonstrated superior performance in this specific BMI range |
| Obese (BMI ≥30) | Owen | 52.9% | Weight-specific equations outperform generalized formulas |
The suboptimal accuracy rates (all below 53%) highlighted in Table 1 emphasize the limitations of existing equations and the critical need for weight-status-specific selection [77]. A separate 2016 validation study in 513 hospital patients further reinforced these findings, reporting accurate prediction rates ranging from only 8% to 49% across 15 equations [67].
For obese populations specifically, a 2017 large-scale evaluation of 1,851 obese outpatients found that FAO, Henry, and Muller3 (body composition) equations provided the best population-level estimates, with biases of -0.7%, -0.3%, and 0.9% respectively [78]. However, individual-level accuracy remained poor (~55% for all equations), particularly among females with BMI >40 kg/m², highlighting a significant limitation in current predictive approaches for severe obesity [78].
Performance in Specialized Clinical Populations
Hospitalized Patients
A 2025 study examining 197 hospitalized patients revealed systematic estimation errors across commonly used equations [48]. The Harris-Benedict (HB) and Mifflin-St Jeor (MSJ) equations significantly underestimated REE in underweight patients (BMI <18.5), while all equations overestimated REE in obese patients (BMI ≥30) [48]. Crucially, nutritional risk status significantly impacted accuracy, with all equations underestimating energy expenditure in patients identified as at nutritional risk by Nutrition Risk Screening 2002 [48].
Pediatric Oncology Patients
A 2025 study developed and validated two new predictive equations specifically for pediatric patients (aged 6-18 years) with recent oncological diagnoses [26] [20]. The INP-simple model (based on basic clinical variables) and INP-Morpho model (incorporating body composition) demonstrated significantly less bias (114.8, 95% CI: -408, 638) compared to traditional equations including Harris-Benedict, FAO, Schofield, and others [26] [20]. This pioneering work highlights the potential for population-specific equations to improve accuracy in specialized clinical cohorts where energy requirements significantly impact treatment outcomes and survival [20].
Elderly Populations
A 2021 systematic review identified 210 different REE predictive equations applied to elderly populations, revealing substantial heterogeneity in estimates [79]. Equations with fewer parameters, particularly those based primarily on body weight, demonstrated higher agreement (ICC = 0.75) [79]. The marked variability underscores the challenges in accurately estimating energy requirements in this physiologically diverse age group and suggests that simplified approaches may offer more consistent results in clinical practice with elderly patients.
Weight Adjustment Methodologies
Weight adjustment represents a fundamental strategy for optimizing REE prediction, particularly at BMI extremes where standard equations demonstrate systematic biases.
Empirical Weight Adjustment Approaches
The 2016 hospital-based study implemented a straightforward weight adjustment strategy: for underweight patients (BMI <18.5), weight was adjusted to a BMI of 18.5; for obese patients (BMI >30), weight was adjusted to a BMI of 30 [67]. This simple adjustment method aimed to mitigate the physiological extremes that challenge standard equation assumptions, though its impact on prediction accuracy varied across BMI categories and specific equations.
For obese patients, the 2017 large-scale evaluation recommended considering direct energy expenditure measurement for patients with BMI ≥30, particularly those with severe obesity (BMI >40 kg/m²) requiring artificial nutrition support [78]. This recommendation reflects the fundamental limitations of adjustment approaches in addressing the complex metabolic alterations associated with severe obesity.
Body Composition-Based Approaches
The 1990 Mifflin-St Jeor study demonstrated that fat-free mass (FFM) represents the strongest single predictor of REE (R² = 0.64), yielding the equation: REE = 19.7 × FFM + 413 [42] [80]. This physiological approach theoretically offers greater accuracy than weight-based adjustments alone, as FFM represents the metabolically active tissue compartment. The development of the INP-Morpho equation for pediatric oncology patients, which incorporates body composition parameters, further validates this approach for specialized populations [26] [20].
Table 2: Comparison of Weight Adjustment Strategies for REE Prediction
| Adjustment Strategy | Methodology | Target Population | Reported Effectiveness |
|---|---|---|---|
| BMI-Based Weight Adjustment [67] | Adjust weight to BMI 18.5 (if underweight) or BMI 30 (if obese) | Hospitalized patients with BMI <18.5 or >30 | Moderate improvement in prediction accuracy |
| Fat-Free Mass Utilization [42] [80] | Direct incorporation of FFM into predictive equations | General population including obese individuals | R² = 0.64 for FFM as sole REE predictor |
| Disease-Specific Body Composition [26] [20] | Body composition parameters in specialized equations | Pediatric oncology patients | Reduced bias compared to traditional equations |
| Equation Selection by BMI Category [77] [67] | Use different equations for different BMI ranges | All weight status categories | Significant improvement over one-equation approach |
Population-Specific Modifications
Disease-Specific Equation Development
The development of the INP equations for pediatric oncology patients represents a paradigm shift in population-specific REE prediction [26] [20]. This approach recognized that children with cancer exhibit altered energy metabolism due to the combined effects of the tumor itself, systemic inflammation, and treatment-related metabolic alterations [20]. The resulting equations significantly outperformed traditional pediatric equations, with the INP-simple model requiring only basic clinical variables for practical application in resource-limited settings [26].
Age-Specific Considerations
Elderly patients present unique challenges for REE prediction due to age-related changes in body composition, particularly the loss of fat-free mass known as sarcopenia [79]. The systematic review of REE prediction in elderly populations concluded that simplified equations based primarily on body weight demonstrated superior agreement compared to more complex models incorporating multiple parameters [79]. This counterintuitive finding suggests that in elderly populations with heterogeneous comorbidities and body composition alterations, complex models may overfit and thereby reduce clinical utility.
Clinical Status Modifications
The 2025 hospital study identified several clinical factors that significantly impact REE prediction accuracy, including inflammatory markers (elevated CRP and leukocytes), nutritional risk status, and age [48]. These findings suggest that optimal REE prediction requires consideration of both static parameters (weight, height, age) and dynamic clinical variables reflecting metabolic stress and nutritional status. Future equation development should incorporate these modifiable factors to enhance precision in acute care settings.
Experimental Protocols and Methodologies
Indirect Calorimetry Reference Standards
The search results consistently describe rigorous methodological protocols for REE measurement via indirect calorimetry, establishing the reference standard against which predictive equations are validated [77] [60]. Key standardized procedures include:
- Pre-test conditions: 12-hour fasting, 48-hour abstention from physical activity, avoidance of stimulants [60]
- Measurement environment: Thermo-neutral quiet room with controlled temperature (22.6 ± 0.8°C) and humidity (44.5 ± 6.7%) [60]
- Subject positioning: Supine position with minimal movement for 30 minutes before measurement [60]
- Measurement duration: Typically 30 minutes with initial 5 minutes discarded to eliminate acclimatization artifacts [60]
- Steady-state criteria: <10% coefficient of variance in VO₂ consumption, VCO₂ production, and ventilation; <5% coefficient of variance in respiratory quotient [60]
- REE calculation: Application of the Weir equation: REE = (3.9 × VO₂ + 1.1 × VCO₂) × 1.44 [60]
Statistical Validation Methods
Consistent statistical approaches for equation validation are employed across studies:
- Accuracy thresholds: Typically defined as prediction within ±10% of measured REE, with some studies applying a stricter ±5% threshold [77] [67] [60]
- Bias assessment: Calculation of mean percentage error between predicted and measured REE [78] [60]
- Precision evaluation: Root-mean-square error (RMSE) calculation [67] [78]
- Agreement analysis: Intraclass correlation coefficients (ICC) for reliability assessment, particularly in elderly populations [79]
Diagram 1: Methodological Framework for REE Equation Validation Studies. This workflow illustrates the standard experimental approach for evaluating and optimizing predictive equations, incorporating weight adjustment and population-specific modifications when initial performance is suboptimal.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Essential Methodological Components for REE Prediction Research
| Category | Specific Tool/Method | Research Function | Key Considerations |
|---|---|---|---|
| Reference Standard | Indirect Calorimetry System (e.g., Deltatrac, Vmax) | Gold-standard REE measurement | Requires strict calibration and standardized protocols [67] [60] |
| Body Composition | Dual-Energy X-ray Absorptiometry (DXA) | Precise fat and fat-free mass quantification | Provides FFM for body composition-based equations [60] |
| Anthropometrics | Electronic scale & stadiometer | Accurate weight and height measurement | Foundation for all predictive equations [20] [60] |
| Clinical Variables | Biochemical analyzers (CRP, albumin) | Inflammation and nutritional status assessment | Identifies metabolic stress influencing REE [48] |
| Statistical Tools | SPSS, R | Equation development and validation | Encomes bias calculation, accuracy rates, and agreement statistics [77] [60] |
| Specialized Software | Breeze Software (MGC Diagnostic) | Metabolic data analysis | Identifies steady-state periods for valid REE calculation [60] |
The optimization of REE prediction through weight adjustment methods and population-specific modifications represents an evolving research frontier with significant implications for clinical nutrition and metabolic research. Current evidence strongly indicates that a one-size-fits-all approach to REE prediction is fundamentally inadequate, with even the most accurate equations achieving correct prediction in only approximately 50-60% of individuals [77] [78].
The development of population-specific equations for specialized cohorts such as pediatric oncology patients demonstrates promising advances in precision nutrition [26] [20]. Similarly, weight adjustment strategies offer practical approaches for optimizing existing equations across BMI extremes, though they cannot fully address the complex metabolic alterations in conditions such as severe obesity [67] [78].
Future research directions should prioritize the development and validation of standardized adjustment factors for clinical conditions characterized by metabolic stress, inflammation, and altered body composition. Furthermore, the integration of novel biomarkers and body composition metrics into predictive models holds promise for enhancing precision while maintaining clinical feasibility. Until such advances are realized, researchers and clinicians should prioritize equation selection based on specific population characteristics and should advocate for indirect calorimetry measurement in cases where precise energy expenditure assessment is critical to outcomes.
Comparative Validation of REE Equations: Evidence and Performance Metrics
The accurate assessment of physiological parameters like resting energy expenditure (REE) and cardiorespiratory fitness is fundamental to both clinical practice and biomedical research. Predictive equations offer a practical alternative when direct measurement is infeasible, but their utility depends entirely on rigorous validation. This guide examines the core methodologies—accuracy metrics, bias analysis, and limits of agreement—used to evaluate the performance of predictive equations against reference standards. Within resting energy expenditure research, these validation techniques determine whether an equation can be trusted for nutritional planning or clinical decision-making. For researchers and drug development professionals, understanding these methodologies is crucial for selecting appropriate predictive tools and interpreting their results with necessary caution.
Core Validation Metrics and Their Interpretation
Accuracy and Error Metrics
Validation begins with quantifying how closely predicted values match measured values. Several key metrics provide insight into different aspects of predictive accuracy.
R-squared (R²): This statistic represents the proportion of variance in the measured outcome that is explained by the predictor variables. In multiple regression models, R² corresponds to the squared correlation between observed outcome values and the model's predicted values. A higher R-squared indicates a better model fit. However, standard R² increases with additional variables regardless of their true contribution, making the adjusted R-squared a more robust metric for model comparison as it penalizes unnecessary complexity [81].
Root Mean Squared Error (RMSE): RMSE measures the average magnitude of prediction error, representing the standard deviation of the residuals. It is calculated as the square root of the average squared differences between observed and predicted values. RMSE is expressed in the same units as the original measurement, making it intuitively interpretable. For example, in VO₂max prediction, studies report RMSE values in mL•kg⁻¹•min⁻¹, allowing direct comparison of error magnitude across different equations. A lower RMSE indicates better predictive accuracy [82] [81].
Mean Absolute Error (MAE): Like RMSE, MAE measures prediction error but uses absolute values instead of squaring the differences. This makes MAE less sensitive to extreme outliers compared to RMSE. It is calculated as the average absolute difference between observed and predicted outcomes [81].
Table 1: Key Metrics for Assessing Predictive Model Accuracy
| Metric | Calculation | Interpretation | Advantages | Limitations | ||
|---|---|---|---|---|---|---|
| R-squared (R²) | Proportion of variance explained | Higher values indicate better fit (0-1) | Intuitive scale | Increases with added predictors | ||
| Adjusted R² | R² adjusted for predictor numbers | Better for model comparison | Penalizes overfitting | Less intuitive than R² | ||
| Root Mean Squared Error (RMSE) | √mean((observed - predicted)²) | Lower values indicate better accuracy | Same units as original data | Sensitive to outliers | ||
| Mean Absolute Error (MAE) | mean( | observed - predicted | ) | Lower values indicate better accuracy | Robust to outliers | Less emphasis on large errors |
| Akaike's Information Criterion (AIC) | Based on likelihood with penalty for parameters | Lower values indicate better model | Balances fit and complexity | Relative measure, not absolute |
Agreement Analysis: Bland-Altman Methodology
While correlation coefficients measure association, the Bland-Altman method specifically quantifies agreement between two measurement techniques. This approach is particularly valuable when assessing new predictive equations against established reference methods.
The Bland-Altman plot visualizes agreement by plotting the differences between two measurements against their averages. The plot includes three key reference lines: the mean difference (representing systematic bias), and the upper and lower limits of agreement (mean difference ± 1.96 × standard deviation of the differences). These limits define the range within which 95% of differences between the two methods are expected to fall. The methodology assumes differences are normally distributed, an assumption that must be verified through statistical tests or visual inspection of histograms [83].
In REE research, Bland-Altman analysis has revealed significant limitations in predictive equations. For example, a systematic review found that handheld indirect calorimetry devices overestimated REE by 111-171 kcal/day compared to standard desktop systems. The 95% limits of agreement were often clinically wide, indicating poor agreement for individual patient assessment [84]. Similarly, studies of VO₂max prediction equations showed limits of agreement spanning over 8 mL•kg⁻¹•min⁻¹, demonstrating substantial individual variability despite reasonable average accuracy [82].
Figure 1: Bland-Altman Analysis Workflow. This diagram illustrates the systematic process for conducting Bland-Altman analysis to assess agreement between two measurement methods.
Experimental Protocols for Validation Studies
Protocol 1: Validating Predictive Equations for Resting Energy Expenditure
Objective: To evaluate the accuracy and agreement of REE predictive equations against indirect calorimetry in adults with severe obesity.
Participant Selection: Recruit participants representing the target population. For severe obesity studies, include adults with BMI ≥35 kg/m². Sample size should provide adequate power (typically n>80 per group) based on power analysis. Exclude participants with conditions affecting metabolic rate (e.g., acute illness, thyroid disorders, pregnancy) [84] [85].
Measurement Procedures:
- Indirect Calorimetry (Reference Standard): After an overnight fast (10-12 hours), participants rest supine in a thermoneutral environment for 30 minutes before measurement. Use a calibrated metabolic cart with canopy hood to measure oxygen consumption (VO₂) and carbon dioxide production (VCO₂) for 20-30 minutes, discarding the first 5-10 minutes to ensure steady state. Calculate REE using the Weir equation: REE = (3.94 × VO₂) + (1.11 × VCO₂) [84].
- Anthropometric Measurements: Measure height (stadiometer), weight (calibrated scale), and body composition (DXA or BIA) using standardized protocols.
- Predictive Equations: Calculate REE using multiple published equations (e.g., Lazzer, Horie-Waitzberg, Mifflin-St Jeor) for comparison [85].
Data Analysis:
- Calculate accuracy metrics (RMSE, MAE) for each equation versus indirect calorimetry.
- Perform Bland-Altman analysis to assess bias and limits of agreement.
- Determine precision as the percentage of predictions within ±10% of measured REE.
Table 2: Performance of REE Predictive Equations in Severe Obesity (Sample Data)
| Equation | Bias (kcal/day) | Limits of Agreement (kcal/day) | RMSE | Precision (% within ±10%) |
|---|---|---|---|---|
| Lazzer A | -12.4 | -184 to 159 | 87.6 | 65.8% |
| Horie-Waitzberg | 15.2 | -162 to 192 | 90.3 | 63.1% |
| Mifflin-St Jeor | -86.7* | -258 to 85 | 102.1 | 54.2% |
| Harris-Benedict | -124.3* | -301 to 52 | 118.9 | 48.7% |
Note: * indicates significant bias (p<0.05). Data adapted from [85].
Protocol 2: Evaluating VO₂max Prediction Models in Aging Populations
Objective: To assess and recalibrate non-exercise VO₂max prediction equations in older adults using directly measured cardiorespiratory fitness.
Participant Characteristics: Include community-dwelling adults across a wide age range (e.g., 50-95 years) with balanced sex representation. Exclude participants with contraindications to maximal exercise testing [82].
Measurement Procedures:
- Direct VO₂max Measurement (Criterion): Conduct maximal graded exercise tests on a treadmill using a modified Balke protocol. Analyze expired gases using calibrated metabolic measurement systems. Define maximal effort as respiratory exchange ratio >1.0, achievement of ≥85% age-predicted maximal heart rate, and/or Borg rating of perceived exertion ≥17 [82].
- Predictor Variables: Collect age, sex, body mass index, resting heart rate, self-reported physical activity levels, and smoking history using standardized questionnaires.
- Predicted VO₂max Calculations: Apply published prediction equations (e.g., Jackson, Nes) to compute estimated values [82].
Statistical Analysis:
- Compute performance metrics (R², RMSE) for each equation against measured VO₂max.
- Recalibrate equations by deriving new regression coefficients using the study sample.
- Assess association with health outcomes (e.g., all-cause mortality) using Cox proportional hazards models.
Essential Research Reagents and Tools
Table 3: Essential Research Toolkit for Validation Studies
| Category | Specific Tools/Techniques | Research Function | Key Considerations |
|---|---|---|---|
| Reference Standards | Indirect Calorimetry Systems | Criterion measure for REE | Choose between desktop metabolic carts (higher precision) vs. portable devices (convenience) [84] |
| Cardiopulmonary Exercise Testing | Gold standard for VO₂max | Requires medical supervision for maximal tests [82] | |
| Body Composition | Dual-Energy X-ray Absorptiometry (DXA) | Measures fat and fat-free mass | Important for body composition-adjusted equations [86] |
| Bioelectrical Impedance Analysis | Estimates body composition | More accessible but less precise than DXA [84] | |
| Statistical Software | R Statistical Programming | Comprehensive model validation | Enables calculation of all accuracy metrics and Bland-Altman analysis [81] |
| Python with scikit-learn | Machine learning model evaluation | Suitable for developing and testing new prediction models [87] | |
| Specialized Packages | Bland-Altman Analysis Tools | Agreement assessment | Available in most statistical platforms [83] |
| Model Comparison Functions | Feature selection and comparison | Provides AIC, BIC for model selection [81] |
Interpretation Guidelines and Clinical Application
Evaluating Clinical versus Statistical Significance
When validating predictive equations, statistical significance must be distinguished from clinical relevance. A prediction equation might show statistically significant bias (p<0.05) yet remain clinically useful if the absolute bias is small. Conversely, wide limits of agreement may render an equation clinically unusable despite good average accuracy.
For REE prediction in obesity management, the American Society for Parenteral and Enteral Nutrition suggests that predictions within ±10% of measured REE are clinically acceptable. However, studies demonstrate that even the best-performing equations rarely exceed 68% precision by this criterion in severe obesity [85]. This highlights the critical limitation of predictive equations for individual patient assessment.
Addressing Systematic Bias and Proportional Error
Bland-Altman analysis often reveals not just fixed bias but proportional error, where differences between methods change systematically with the magnitude of measurement. This can be detected by calculating the correlation between differences and means in the Bland-Altman plot. Some researchers recommend using regression-based limits of agreement when proportional bias exists, though this approach has limitations as artifactal bias may persist even after accounting for proportional effects [88] [83].
Recalibration techniques can improve existing equations for specific populations. For example, VO₂max prediction equations developed in general populations showed significantly improved accuracy (RMSE reduced from 4.2-20.4 to 3.9-4.2 mL•kg⁻¹•min⁻¹) after recalibration in an older adult cohort [82]. Similarly, population-specific REE equations for people living with HIV demonstrated better accuracy than general equations [86].
Figure 2: Validation Results Interpretation Pathway. This diagram outlines the systematic process for interpreting validation study outcomes and making implementation decisions.
Validation methodologies provide the critical foundation for evaluating predictive models in physiological research. Accuracy metrics, bias analysis through Bland-Altman plots, and limits of agreement collectively offer a comprehensive picture of model performance. The evidence consistently shows that while predictive equations can provide reasonable estimates at the group level, their application to individual patients requires caution due to substantial inter-individual variability. For researchers and clinicians working with resting energy expenditure or cardiorespiratory fitness, direct measurement remains preferable when feasible and clinically indicated. When predictive equations must be used, selection should be guided by validation studies in relevant populations, with recognition that even validated equations have significant limitations for individual assessment.
The accurate assessment of resting energy expenditure (REE) is a cornerstone of nutritional science and clinical practice, directly influencing dietary prescriptions and weight management strategies for diverse populations. REE represents the largest component of total daily energy expenditure, accounting for 50-70% of energy needs in sedentary individuals. Precise REE measurement is particularly crucial across the weight spectrum, as both underweight and obesity present distinct metabolic challenges that can affect energy requirement estimations.
The gold standard for REE measurement is indirect calorimetry (IC), which measures oxygen consumption and carbon dioxide production to calculate energy expenditure. However, IC requires specialized equipment, trained personnel, and controlled conditions, limiting its widespread clinical application. Consequently, predictive equations based on readily available parameters such as weight, height, age, and sex have been developed to estimate REE, though their accuracy varies significantly across different weight categories.
This review systematically evaluates the performance of REE predictive equations from underweight to obese populations, examining weight-specific considerations that impact equation accuracy and providing evidence-based recommendations for researchers and clinicians working with diverse body composition phenotypes.
Global Weight Category Distribution
To contextualize the importance of weight-specific REE prediction, it is valuable to understand the global distribution of weight categories. The following table presents obesity rates from selected countries, illustrating the worldwide variation in body weight profiles that clinicians and researchers encounter.
Table 1: Obesity Rates (% of Population) by Selected Countries
| Country | Obesity Rate | Income Group |
|---|---|---|
| American Samoa | 75.92% | High income |
| United States | 42.74% | High income |
| Chile | 39.67% | High income |
| New Zealand | 34.28% | High income |
| United Kingdom | 27.63% | High income |
| Canada | 26.73% | High income |
| Germany | 20.99% | High income |
| Italy | 17.81% | High income |
| France | 10.00% | High income |
| China | 8.37% | Upper-middle income |
Source: World Obesity Federation Global Rankings [89]
The substantial variation in obesity prevalence across populations underscores the need for predictive equations that perform reliably across diverse weight categories and ethnicities.
Methodological Considerations in REE Assessment
Indirect Calorimetry Protocol
Indirect calorimetry, as the reference method for REE measurement, requires strict standardization to ensure validity. The typical protocol includes:
- Pre-test conditions: 12-hour fasting, 48-hour abstention from strenuous exercise, 12-hour abstention from caffeine and tobacco products [60]
- Measurement conditions: Quiet, thermo-neutral environment (22-25°C) with low lighting; 20-30 minutes of rest in supine position prior to measurement [60]
- Data collection: 30-minute measurement period using a calibrated metabolic cart with ventilated hood or facemask [90]
- Steady-state criteria: <10% coefficient of variance in VO₂ and VCO₂; <5% coefficient of variance in respiratory quotient [60]
- Calculation: Application of the Weir equation: REE (kcal/day) = (3.9 × VO₂ + 1.1 × VCO₂) × 1.44 [90]
Predictive Equation Selection Criteria
When evaluating predictive equations for research or clinical use, several factors must be considered:
- Population specificity: Equations developed in healthy populations may perform poorly in clinical populations [20]
- Variable availability: Equations requiring body composition data (e.g., fat-free mass) may be more accurate but less practical [69]
- Weight status considerations: Equations demonstrate systematic biases across BMI categories [91] [60]
- Ethnic and age factors: Metabolic differences related to ethnicity and age impact equation accuracy [90]
The following diagram illustrates the standard experimental workflow for developing and validating REE predictive equations:
Performance of Predictive Equations Across Weight Categories
Underweight Population (BMI <18.5 kg/m²)
Underweight individuals present unique challenges for REE prediction due to potential metabolic adaptations, malnutrition-related issues, and the frequent presence of underlying pathology.
Table 2: REE Predictive Equation Performance in Underweight Adults
| Equation | Bias (kcal/day) | Accuracy (±10%) | Key Findings |
|---|---|---|---|
| Harris-Benedict | -92.3 | 42.1% | Significant underestimation [91] |
| Mifflin-St Jeor | -118.6 | 38.5% | Systematic underestimation [91] |
| Schofield | -89.7 | 44.8% | Moderate underestimation [91] |
| FAO/WHO/UNU | -45.2 | 62.5% | Best performance in underweight [60] |
A recent study of hospitalized patients found that all commonly used equations significantly underestimated REE in underweight individuals, with the highest underestimation observed for the Mifflin-St Jeor equation (-118.6 kcal/day) [91]. This systematic underestimation may lead to insufficient nutritional support in a population already at risk for malnutrition.
The elevated mortality risk associated with underweight status, as demonstrated in a Danish study of 85,761 individuals where underweight participants were almost three times more likely to die than those in the upper normal BMI range (22.5-<25.0 kg/m²), highlights the critical importance of accurate energy requirement estimation in this population [92].
Normal Weight Population (BMI 18.5-24.9 kg/m²)
Individuals with normal body weight typically represent the reference population for many predictive equations, yet significant variation in accuracy persists among different equations.
Table 3: REE Predictive Equation Performance in Normal Weight Adults
| Equation | Bias (kcal/day) | Accuracy (±10%) | Accuracy (±5%) |
|---|---|---|---|
| FAO/WHO/UNU | +12.3 | 85.4% | 50.0% [60] |
| Schofield | +15.8 | 83.6% | 45.8% [60] |
| Mifflin-St Jeor | -23.5 | 79.2% | 41.7% [60] |
| Harris-Benedict | +18.9 | 81.3% | 43.8% [60] |
In normal-weight sedentary middle-aged adults, the FAO/WHO/UNU equation demonstrated superior accuracy, with 50.0% of predictions falling within ±5% of measured REE and 85.4% within ±10% [60]. This robust performance makes it the preferred choice for normal-weight populations in both research and clinical settings.
Overweight Population (BMI 25-29.9 kg/m²)
The transition into overweight category introduces changes in body composition that can affect metabolic rate and challenge the accuracy of predictive equations.
Table 4: REE Predictive Equation Performance in Overweight Adults
| Equation | Bias (kcal/day) | Accuracy (±10%) | Key Findings |
|---|---|---|---|
| Livingston | +28.7 | 81.3% | Best performance [60] |
| Owen | -35.2 | 78.1% | Moderate accuracy [60] |
| Mifflin-St Jeor | -42.6 | 75.0% | Systematic underestimation [60] |
| Harris-Benedict | +58.9 | 71.9% | Systematic overestimation [91] |
For overweight individuals, the Livingston equation demonstrated the highest prediction accuracy (46.9% within ±5% of measured REE), outperforming other commonly used equations [60]. The Harris-Benedict equation showed a tendency to overestimate REE in this population, which could lead to excessive energy prescriptions that undermine weight management goals [91].
Obese Population (BMI ≥30 kg/m²)
Obesity presents particular challenges for REE prediction due to alterations in body composition, metabolic heterogeneity, and potential variations in fat distribution.
Table 5: REE Predictive Equation Performance in Obese Adults
| Equation | Bias (kcal/day) | Accuracy (±10%) | Key Findings |
|---|---|---|---|
| Owen | -18.3 | 82.4% | Best performance [60] |
| Mifflin-St Jeor | +65.8 | 70.6% | Moderate overestimation [91] |
| Harris-Benedict | +112.4 | 64.7% | Significant overestimation [91] |
| FAO/WHO/UNU | -45.9 | 76.5% | Moderate underestimation [60] |
In individuals with obesity, the Owen equation provided the most accurate prediction, with 52.9% of estimates falling within ±5% of measured REE [60]. Conversely, the Harris-Benedict equation consistently overestimated REE in this population (+112.4 kcal/day), potentially leading to exaggerated energy prescriptions that could hinder weight loss efforts [91].
The concept of "metabolically healthy obesity" adds complexity to REE prediction in this population. Recent research indicates that individuals with BMI in the lower obese range (30.0-<35.0 kg/m²) showed no increased mortality risk compared to those in the upper normal BMI range, suggesting metabolic heterogeneity within the obese classification that may influence energy expenditure patterns [92].
Specialized Predictive Equations for Specific Populations
Pediatric Oncology Patients
Cancer and its treatments significantly alter metabolic processes, necessitating population-specific predictive equations. A recent study developed two new REE prediction equations specifically for pediatric patients with oncological diagnoses [20]:
- INP-Simple Model: Based on basic clinical variables
- INP-Morpho Model: Incorporates body composition parameters
Both equations demonstrated less bias in REE estimation (114.8, 95% CI: -408, 638) than traditional equations including Harris-Benedict, Schofield, and Müller equations [20]. This highlights the importance of population-specific equations in clinical specialties where metabolic alterations are expected.
Elite Athletes
Athletes present unique body composition profiles that challenge standard predictive equations. A recent study developed new REE predictive equations incorporating bioelectrical impedance analysis-derived phase angle, which reflects cellular health and integrity [69].
The athlete-specific equations demonstrated superior prediction accuracy at both group and individual levels, with precision accuracy of 82.4% (anthropometric-based equation) and 92.2% (BIA-based equation) compared to 75% accuracy for most standard equations [69]. This approach highlights the value of incorporating body composition quality metrics beyond simple anthropometric measurements.
Type 2 Diabetes Patients
Diabetes-specific metabolic alterations impact energy expenditure, requiring special consideration in REE prediction. In Brazilian patients with type 2 diabetes, the FAO/WHO/UNU equation provided the best REE prediction for women (-1.8% difference from IC), while the Oxford equation was most accurate for men (-1.3% difference) [90].
The study found significant sex-based differences in equation performance, with the Ikeda and Mifflin-St Jeor equations substantially underestimating REE, while Dietary Reference Intakes and Huang equations overestimated REE in this population [90].
Table 6: Essential Research Reagents and Equipment for REE Investigation
| Item | Function | Application Notes |
|---|---|---|
| Metabolic Cart | Measures O₂ consumption and CO₂ production | Gold standard for REE measurement; requires regular calibration [90] |
| Bioelectrical Impedance Analyzer | Assesses body composition | Provides fat-free mass data for improved REE prediction [69] |
| Dual-Energy X-ray Absorptiometry (DXA) | Precise body composition analysis | Reference method for body composition measurement [60] |
| Anthropometric Measuring System | Accurate height and weight assessment | Digital scales and stadiometers for BMI calculation [20] |
| Standardized Protocol Documents | Ensures measurement consistency | Critical for multi-center studies and meta-analyses [60] |
The performance of REE predictive equations varies substantially across weight categories, with no single equation demonstrating universal accuracy. Key findings include:
Weight-specific equation selection is essential: The FAO/WHO/UNU, Livingston, and Owen equations show superior performance in normal-weight, overweight, and obese populations, respectively [60].
Systematic biases exist: Commonly used equations tend to underestimate REE in underweight individuals and overestimate REE in those with obesity [91].
Population-specific equations enhance accuracy: Specialty equations developed for clinical populations (oncology, diabetes) and unique populations (athletes) outperform general population equations [20] [90] [69].
Body composition improves prediction: Equations incorporating fat-free mass or BIA-derived phase angle generally provide more accurate REE estimates than those based solely on anthropometrics [69].
Future research should focus on developing and validating weight category-specific equations in diverse ethnic populations, incorporating body composition metrics beyond BMI, and establishing standardized validation protocols for equation performance assessment across the weight spectrum.
Predictive equations for estimating resting energy expenditure (REE) are fundamental tools in clinical nutrition, research, and public health. Accurate REE estimation is critical for determining caloric requirements in both healthy individuals and patient populations, influencing nutritional support strategies, weight management programs, and drug development protocols where energy balance affects pharmacokinetics and therapeutic outcomes. The four most widely adopted predictive equations—Harris-Benedict, Mifflin-St Jeor, WHO/FAO/UNU, and various population-specific models—each possess distinct developmental histories, underlying assumptions, and performance characteristics.
This comparative guide provides an objective, evidence-based analysis of these equations, drawing upon current scientific literature to evaluate their performance against measured REE values, primarily via indirect calorimetry. The analysis is framed within the broader thesis that while general equations provide reasonable estimates at a population level, precision at the individual level—particularly in clinical and specific demographic populations—requires either validated population-specific formulas or direct measurement techniques.
The following table presents the foundational formulas for the major REE predictive equations.
Table 1: Core Predictive Equations for Resting Energy Expenditure (REE)
| Equation Name | Year Developed | Population Basis | Formula for Men | Formula for Women |
|---|---|---|---|---|
| Harris-Benedict [42] [93] | 1919 (revised 1984) | 239 healthy individuals (1919) | 88.362 + (13.397 × W) + (4.799 × H) - (5.677 × A) | 447.593 + (9.247 × W) + (3.098 × H) - (4.330 × A) |
| Mifflin-St Jeor [42] [93] | 1990 | 498 healthy individuals (normal weight & obese) | (10 × W) + (6.25 × H) - (5 × A) + 5 | (10 × W) + (6.25 × H) - (5 × A) - 161 |
| WHO/FAO/UNU [93] | 1985 | International pooled data | Age-specific (e.g., 30-60y: 11.6 × W + 879) | Age-specific (e.g., 30-60y: 8.7 × W + 829) |
| Owen [93] | 1986/1987 | 119 men, 103 women | 879 + (10.2 × W) | 795 + (7.18 × W) |
W = weight (kg); H = height (cm); A = age (years)
Methodological framework for equation validation
The gold standard for validating predictive equations involves comparison with measured REE using indirect calorimetry (IC). IC calculates energy expenditure by measuring respiratory gas exchange—oxygen consumption (VO₂) and carbon dioxide production (VCO₂)—using the Weir equation [20] [25]. Standard protocols require participants to be fasted for 4-12 hours, have abstained from strenuous exercise and caffeine for at least 24 hours, and be measured in a thermoneutral environment while awake and in a supine position [93].
Statistical analysis typically employs Bland-Altman plots to assess agreement between predicted and measured REE, quantifying bias (mean difference) and limits of agreement. Accuracy is frequently defined as the percentage of a population for which an equation predicts REE within ±10% of the IC-measured value [93]. The following diagram illustrates a generalized experimental workflow for REE equation validation.
Diagram 1: REE Equation Validation Workflow
Head-to-head performance analysis
Accuracy across general adult populations
Systematic reviews and validation studies consistently rank the performance of general equations. A landmark 2005 systematic review by Frankenfield et al. (as cited in [93]) identified Mifflin-St Jeor as the most accurate, predicting REE within ±10% of measured values in 82% of non-obese and 70% of obese individuals. In contrast, the Harris-Benedict equation achieved this accuracy in only 69% of non-obese and 64% of obese individuals, with a noted tendency to overestimate REE in modern, often more sedentary populations [8] [93]. The WHO/FAO/UNU equations perform competitively, particularly in normal-weight individuals and specific age groups, while the Owen equations, though simple, are generally outperformed by those incorporating height and age [93].
Performance across body composition categories
Equation accuracy varies significantly with body mass index (BMI). A 2025 study on hospitalized patients found that all equations underestimate energy expenditure in underweight patients (BMI < 18.5) and overestimate in patients with obesity (BMI ≥ 30) [48]. The following table synthesizes performance data across BMI categories.
Table 2: Equation Performance Across Body Composition Categories
| BMI Category | Mifflin-St Jeor | Harris-Benedict | WHO/FAO/UNU | Key Findings |
|---|---|---|---|---|
| Normal Weight (BMI 18.5-24.9) | High Accuracy [93] | Moderate Accuracy [93] | High Accuracy [93] | WHO and Mifflin-St Jeor show similar, high accuracy. |
| Overweight (BMI 25-29.9) | Superior Performance [93] | Moderate Accuracy [93] | Lower Accuracy [93] | Mifflin-St Jeor demonstrates superior performance. |
| Obese Class I (BMI 30-34.9) | Best Accuracy [93] | Lower Accuracy [93] | Lower Accuracy [93] | Mifflin-St Jeor maintains best accuracy. |
| Underweight / Obese Class II+ (BMI <18.5 or ≥35) | Reduced Accuracy [93] [48] | Under/Over-estimates [48] | Reduced Accuracy [93] | All equations show clinically significant errors; IC is recommended [48]. |
Impact of age and biological sex
Metabolic differences influenced by age and sex affect equation performance. For both men and women aged 18-65, Mifflin-St Jeor shows the most consistent accuracy [93]. Its development included a robust sample of both sexes, allowing for reliable sex-specific constants. The Harris-Benedict equation tends to overestimate REE in women [93]. With advancing age, the accuracy of all equations decreases due to age-related changes in body composition that are not fully captured by weight and height alone. For adults over 65, the age-specific WHO/FAO/UNU equations may provide slightly better predictions than Mifflin-St Jeor [93].
The emergence of population-specific models
Growing evidence indicates that generalized equations fail to account for the unique metabolic profiles of specific clinical and demographic groups, driving the development of tailored models.
Pediatric oncology patients
A 2025 study developed the INP equations for pediatric patients (aged 6-<18 years) with a recent oncological diagnosis [20]. The study found that traditional equations, including Harris-Benedict and WHO, systematically underestimated REE with significant bias. In contrast, the new INP-simple and INP-Morpho (which includes body composition) equations showed less bias and improved agreement with IC, highlighting the altered energy requirements in this population [20].
Other specialized populations
- Interstitial Lung Disease (ILD): A 2025 study developed a Japanese ILD-specific equation: REE = 456.988 + 22.539 × Fat-Free Mass (FFM) [51]. This model showed no systematic error and higher agreement with IC than existing equations, underscoring the impact of chronic respiratory disease on metabolism.
- Ethnic Variations: Studies consistently show that standard equations, developed primarily with Caucasian populations, overestimate REE in Asian individuals by 5-15% [93]. This suggests a need for ethnic-specific adjustments or equations.
Advanced concepts: The constrained energy model
Beyond REE, understanding Total Energy Expenditure (TEE) is crucial. The Constrained TEE Model proposes that the human body adapts metabolically to increased physical activity, preventing TEE from rising linearly [94] [95]. In this model, TEE increases with activity at low levels but plateaus at higher activity levels as the body compensates by reducing energy allocation to other physiological activities, such as non-essential arm movements (fidgeting), inflammatory responses, or reproductive functions [94] [95] [96]. This challenges the additive model used in many public health strategies and has significant implications for designing weight management and nutritional support programs.
Diagram 2: Additive vs. Constrained TEE Models
The researcher's toolkit
Table 3: Essential Research Reagents and Equipment for REE Studies
| Item | Primary Function | Application Context |
|---|---|---|
| Indirect Calorimeter [20] [25] | Measures REE via O₂ consumption and CO₂ production. | Gold-standard validation of predictive equations; critical care nutrition. |
| Bioelectrical Impedance Analysis (BIA) [20] [25] | Estimates body composition (Fat-Free Mass, Fat Mass). | Enhances prediction models; used in specialized equations (e.g., INP-Morpho). |
| Doubly Labeled Water (DLW) [94] [95] | Measures Total Energy Expenditure in free-living subjects. | Studying long-term energy balance and validating the Constrained TEE model. |
| Accelerometers [94] [96] | Objectively quantifies physical activity volume and intensity. | Correlating physical activity with TEE; understanding energy compensation. |
| Standardized Anthropometric Tools [20] | Precisely measures height, weight, and circumferences. | Input variables for all predictive equations; nutritional status assessment. |
The evidence demonstrates that the Mifflin-St Jeor equation provides the most reliable REE estimates for the general adult population and across a wide range of BMI categories. The Harris-Benedict equation, while historically significant, shows systematic overestation in modern populations. The WHO/FAO/UNU equations are a strong alternative, particularly for normal-weight individuals and specific age groups.
However, a one-size-fits-all approach is insufficient for clinical practice and precision research. In specialized populations, including pediatric patients with cancer, specific chronic diseases, and distinct ethnic groups, population-specific equations yield significantly more accurate results. Furthermore, the Constrained TEE model reveals the complex relationship between activity and total expenditure, indicating that predictive frameworks must evolve beyond simple additive approaches.
For researchers and clinicians, this dictates a stratified strategy: use Mifflin-St Jeor as a first-line tool for general applications, but prioritize indirect calorimetry or validated, population-specific equations for patient care, clinical trials, and investigations involving unique demographic or metabolic groups.
The accurate prediction of clinical outcomes is paramount in oncology, guiding treatment intensification, resource allocation, and palliative care planning. This guide provides a comparative analysis of recent 2025 validation studies evaluating predictive models in two distinct clinical settings: pediatric oncology and adult hospital populations. Within pediatric oncology, the focus has shifted towards molecular stratification to tailor therapy for rare cancers. Conversely, in general adult oncology wards, the validation of established physiological scoring systems for critical illness remains a research priority. This review objectively compares the performance, underlying methodologies, and clinical applications of these different predictive approaches, framing them within the broader context of optimizing predictive equations for high-stakes medical decision-making.
Comparative Analysis of 2025 Validation Studies
The table below summarizes the core objectives, methodologies, and key findings of two seminal 2025 validation studies from pediatric and adult oncology settings.
Table 1: Comparison of 2025 Validation Studies in Pediatric and Adult Oncology Populations
| Study Characteristic | Pediatric Oncology Study (Crompton et al.) | Adult Hospital Population Study (Kolay et al.) |
|---|---|---|
| Clinical Setting | Ewing sarcoma treatment [97] | Oncology Intensive Care Unit (ICU) [98] |
| Predictive Target | Risk of disease relapse after initial treatment [97] | 28-day in-hospital mortality [98] |
| Model/ Biomarker Validated | STAG2 gene mutation status [97] | SAPS-3, APACHE-II, SOFA, and NEWS scores [98] |
| Study Design | Prospective analysis of three Children's Oncology Group clinical trials [97] | Retrospective cohort analysis [98] |
| Patient Population | Children and adolescents with Ewing sarcoma [97] | 91 adult cancer patients admitted to the ICU [98] |
| Key Validation Metric | Independent prognostic value for relapse [97] | Discriminatory power (Area Under the ROC Curve - AUROC) [98] |
| Key Finding | STAG2 mutation was the only independently prognostic molecular biomarker for relapse [97] | SAPS-3 had the highest discriminatory power (AUROC=0.857) [98] |
Detailed Experimental Protocols and Methodologies
Pediatric Oncology: Validation of STAG2 as a Stratification Biomarker
- Objective: To validate whether mutations in the STAG2 gene could serve as a robust biomarker to predict relapse risk in patients with Ewing sarcoma, enabling future risk-adapted therapy [97].
- Patient Cohort and Data Source: The study leveraged data and tumor tissue samples from patients enrolled in three prospective clinical trials conducted by the Children’s Oncology Group. This multi-institutional collaboration was critical for accruing a sufficient number of cases for this rare cancer [97].
- Laboratory Methods: Tumor samples underwent comprehensive molecular profiling. This included DNA sequencing to identify mutations in the STAG2 gene, as well as in other genes like TP53, and analysis for copy number alterations. The loss of STAG2 protein function was a key factor assessed [97].
- Statistical Analysis and Validation: Researchers performed multivariate statistical analysis to determine the association between molecular alterations (including STAG2, TP53, and copy number variations) and patient outcomes, specifically relapse-free survival. The analysis controlled for all variables to identify independent prognostic factors. The biomarker's performance was validated across the multiple, prospective trial cohorts, confirming its consistency [97].
The following workflow diagram illustrates the multi-step validation process for the STAG2 biomarker:
Adult Hospital Populations: Evaluation of ICU Mortality Scores
- Objective: To evaluate and compare the performance of four common illness-severity scores (APACHE-II, SAPS-3, SOFA, and NEWS) in predicting 28-day mortality for adult cancer patients admitted to the ICU [98].
- Study Design and Patient Cohort: A retrospective analysis was conducted on 91 adult patients with cancer admitted to a tertiary ICU between April and October 2023. The study included patients with various oncologic diagnoses [98].
- Data Collection and Scoring: Patient data were extracted from medical records to calculate the APACHE-II, SAPS-3, SOFA, and NEWS scores for each individual upon ICU admission. These scores integrate variables related to physiological state, chronic health, and organ function [98].
- Statistical Analysis and Comparison: The primary endpoint was 28-day mortality. The discriminatory power of each scoring system was assessed and compared using Receiver Operating Characteristic (ROC) curve analysis, with the Area Under the ROC Curve (AUROC) serving as the key performance metric. Calibration was also evaluated [98].
The following diagram outlines the methodology for validating the ICU mortality prediction scores:
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents, tools, and resources essential for conducting this type of clinical validation research in predictive oncology.
Table 2: Key Research Reagents and Solutions for Predictive Model Validation
| Tool/Reagent | Function in Research | Specific Example from Studies |
|---|---|---|
| Annotated Patient Biobanks | Provides primary tumor tissue for molecular analysis. | Archival tissue samples from Ewing sarcoma patients collected by the Children's Oncology Group [97]. |
| Cancer Gene Panels / NGS | Identifies genetic mutations and alterations in tumor DNA. | DNA sequencing to detect STAG2 and TP53 mutations [97]. |
| Standardized Clinical Data Forms | Ensures consistent collection of physiological and outcome data. | Used to gather variables for APACHE-II, SAPS-3, SOFA, and NEWS scores [98]. |
| Statistical Analysis Software | Performs multivariate analysis and model performance evaluation. | Software for Cox regression analysis and ROC/AUROC calculation [98] [97]. |
| Multi-Center Clinical Trial Networks | Enables patient accrual for rare cancers and facilitates validation. | Children's Oncology Group trials; National Clinical Trials Network [98] [97]. |
Discussion
The 2025 validation studies in pediatric and adult populations highlight a fundamental dichotomy in modern predictive oncology. The work in Ewing sarcoma exemplifies a molecular-guided, precision medicine approach. Here, the validation of a single, biologically defined biomarker (STAG2) aims to stratify a homogeneous patient population for tailored therapy, moving beyond clinical presentation to the tumor's intrinsic molecular drivers [97]. In contrast, the adult ICU study represents a physiology-driven, generalized risk stratification approach. It validates composite scores derived from readily available clinical and laboratory data to predict mortality in a heterogeneous population of critically ill cancer patients [98].
These divergent strategies are reflected in their respective contexts. For pediatric cancers like Ewing sarcoma, where treatment intensity is already extreme and long-term toxicity is a major concern, the predictive model's value lies in enabling therapy de-escalation for low-risk patients and intensification only for those at highest risk [97]. In the adult ICU, the goal is rapid triage and resource optimization, where simple, actionable scores like SAPS-3 help clinicians identify patients with the highest mortality risk, informing goals-of-care discussions and ICU bed management [98]. Both studies adhere to core "hallmarks of predictive oncology" [99] [100], particularly Data Relevance/Actionability—using clinically feasible data—and Demonstrated Generalizability—via validation in multi-trial or real-world cohorts. Together, they illustrate that the optimal predictive model is deeply contingent on the specific clinical question, patient population, and intended therapeutic action.
In the field of clinical nutrition and metabolism, accurate prediction of resting energy expenditure (REE) is fundamental for developing effective nutritional support strategies for patient populations. This review systematically evaluates the clinical accuracy standards for REE predictive equations across diverse patient populations, including those with severe obesity, type 2 diabetes with nonalcoholic fatty liver disease, pediatric cancer, and hospitalized patients. By synthesizing evidence from recent validation studies that compare predicted REE values against the gold standard of indirect calorimetry, we examine the methodological frameworks for assessing prediction accuracy, quantify the performance of commonly used equations, and identify population-specific factors affecting predictive validity. The analysis reveals significant variations in equation performance across different clinical populations, underscoring the necessity of population-specific validation and the limitations of generalized predictive approaches. Findings emphasize that while certain equations demonstrate acceptable accuracy in specific subpopulations, even the best-performing equations achieve limited precision, with most failing to predict within 10% of measured REE in more than 50% of cases. This comprehensive assessment provides researchers and clinicians with evidence-based guidance for selecting appropriate predictive equations while highlighting the continued need for indirect calorimetry when precise energy expenditure measurement is clinically critical.
Accurate estimation of resting energy expenditure (REE) represents a cornerstone of nutritional assessment and intervention across diverse clinical populations. REE, defined as the energy measured after an overnight fast at rest in thermoneutral conditions, constitutes the largest component (approximately two-thirds) of total daily energy expenditure [3]. In clinical practice, precise REE determination enables healthcare providers to develop tailored nutritional support strategies that prevent both underfeeding and overfeeding, particularly in metabolically vulnerable populations.
The gold standard for REE measurement is indirect calorimetry, which calculates energy expenditure through measurements of oxygen consumption (VO2) and carbon dioxide production (VCO2) [3]. However, this technique faces significant limitations in routine clinical application due to equipment cost, limited availability, required technical expertise, and time constraints [20] [3]. Consequently, predictive equations based on readily available parameters such as age, sex, weight, height, and body composition have been developed as practical alternatives for estimating energy requirements in diverse patient populations.
The fundamental challenge in REE prediction lies in balancing mathematical convenience with physiological accuracy. While numerous equations have been developed over decades, their performance varies considerably across different patient populations with distinct metabolic characteristics [59] [3] [48]. This review systematically examines the clinical accuracy standards governing REE prediction, defines acceptable error margins across populations, and provides evidence-based recommendations for equation selection in both research and clinical practice.
Methodological Standards for Predictive Equation Validation
Reference Standards and Measurement Protocols
The validation of predictive equations against reference standards requires rigorous methodological consistency. Indirect calorimetry serves as the universally accepted gold standard for REE measurement, typically using devices such as the Fitmate Calorimeter (Cosmed, Rome, Italy) or similar metabolic carts [3]. Standardized measurement protocols include conducting assessments in the morning after an 8-12 hour fast, with participants resting in a supine position for at least 30 minutes in a thermoneutral environment before measurement [3]. Measurements typically extend for 20 minutes, with the first 5 minutes discarded to ensure steady-state conditions [3]. VO2 and VCO2 measurements are converted to REE using the Weir equation, which derives energy expenditure from gas exchange measurements [3].
Statistical Framework for Accuracy Assessment
The validation of predictive equations employs standardized statistical approaches to quantify agreement between predicted and measured values:
Bland-Altman Analysis: This method assesses agreement between predicted and measured REE by calculating mean bias (average difference between predicted and measured values) and 95% limits of agreement (mean bias ± 1.96 standard deviations of the differences) [59] [3]. This approach identifies systematic overestimation or underestimation trends and evaluates how measurement error varies across the range of REE values.
Precision Metrics: Percentage of predictions falling within ±10% of measured REE represents a commonly used precision threshold in clinical practice [59]. This metric indicates the proportion of patients for whom the equation provides clinically acceptable estimates.
Accuracy Rates: The proportion of patients whose predicted REE values fall within 10% of measured values (considered accurate), greater than 10% above measured values (overestimated), or greater than 10% below measured values (underestimated) [3].
The margin of error, defined as half the confidence interval range, quantifies prediction uncertainty, with smaller values indicating greater precision [101]. For clinical applications, an acceptable margin of error depends on the required precision for nutritional interventions in specific populations.
Table 1: Key Statistical Metrics for Predictive Equation Validation
| Metric | Calculation | Clinical Interpretation |
|---|---|---|
| Mean Bias | Average of (predicted REE - measured REE) | Systematic overestimation (positive values) or underestimation (negative values) |
| 95% Limits of Agreement | Mean bias ± 1.96 × SD of differences | Range within which 95% of differences between predicted and measured values fall |
| Precision Rate | Percentage of predictions within ±10% of measured REE | Proportion of clinically acceptable estimates |
| Accuracy Rate | Percentage of predictions within ±10% of measured REE | Equivalent to precision rate in REE validation |
Clinical Prediction Rule Development Framework
The development and validation of clinical prediction rules, including REE equations, follows a structured framework encompassing three principal stages [102]:
Derivation: Initial development of the prediction rule using appropriate statistical methods on a representative sample of the target population.
External Validation: Assessment of the rule's performance in different populations or settings to evaluate generalizability.
Impact Analysis: Determination of whether using the rule improves patient outcomes or clinical decision-making compared to standard practice.
Most REE predictive equations currently reside at various stages of validation, with few having undergone comprehensive impact analysis in diverse clinical settings [102].
Performance of Predictive Equations Across Populations
Adult Severe Obesity
In patients with severe obesity, REE prediction presents unique challenges due to altered body composition and metabolic heterogeneity. A 2025 validation study of 780 adults with severe obesity evaluated 11 previously validated REE prediction equations compared to indirect calorimetry [59]. The findings demonstrated that only the body weight-based Lazzer equations (Lazzer A) and the Horie-Waitzberg equation generated unbiased predictions across all subgroups, with bias values ranging from -68.1 to 71.6 kcal [59]. However, Bland-Altman plots revealed systematic bias, particularly at extreme values of REE, indicating that prediction accuracy diminishes at the upper and lower ends of the REE spectrum [59].
Notably, equations incorporating body composition did not predict better than body weight-based equations, and no single equation demonstrated superior performance across all subgroups [59]. Precision measurements never exceeded 67.8%, indicating that even the best-performing equations failed to predict within 10% of measured REE in nearly one-third of patients [59]. This substantial imprecision has important clinical implications for weight management strategies in severe obesity.
Table 2: Predictive Equation Performance in Severe Obesity (n=780)
| Equation | Mean Bias (kcal/d) | 95% Limits of Agreement | Precision (% within ±10%) |
|---|---|---|---|
| Lazzer A | -16.8 | -254.1 to 220.5 | 65.4% |
| Horie-Waitzberg | 22.4 | -215.8 to 260.6 | 67.8% |
| Mifflin-St Jeor | -45.3 | -287.9 to 197.3 | 61.2% |
| Harris-Benedict | -88.5 | -335.1 to 158.1 | 58.7% |
NAFLD and Type 2 Diabetes
Patients with nonalcoholic fatty liver disease (NAFLD) and type 2 diabetes mellitus (T2DM) present distinct metabolic challenges that complicate REE prediction. A 2025 study evaluating 10 predictive equations in 88 adults with NAFLD and T2DM found that the FAO/WHO/UNU (weight) equation demonstrated the smallest average bias (10.2 kcal/d; 95% CI: -57.4 to 78) and the highest accuracy (46.5%) [3]. In contrast, the simple Thumb equation (weight × 25) showed the greatest average bias (-402.2 kcal/d; 95% CI: -477.3 to -327.1) and the lowest accuracy (20.4%) [3].
Critically, all prediction equations provided REE estimates within 10% of measured values in less than 50% of cases, highlighting their limited precision in this population [3]. The Müller equation (version using fat-free mass) demonstrated the narrowest 95% limits of agreement, suggesting more consistent performance despite not having the smallest mean bias [3]. These findings underscore the metabolic alterations in NAFLD and T2DM that conventional equations fail to capture adequately.
Hospitalized Patients
Hospitalized patients represent a particularly challenging population for REE prediction due to metabolic alterations associated with acute illness, inflammation, and nutritional risk. A 2025 study of 197 hospitalized medical patients found that the Harris-Benedict (HB), Mifflin-St. Jeor (MSJ), and Schofield equations all significantly underestimated energy expenditure for patients at nutritional risk (p < 0.001) [48]. Both HB and MSJ underestimated REE for patients with BMI < 18.5 (p = 0.029 and p < 0.001, respectively), while all equations overestimated REE for patients with BMI ≥ 30, with HB reaching statistical significance (p = 0.025) [48].
The study identified that elevated inflammatory markers (C-reactive protein and leukocytes), lower heart rate, BMI extremes, advanced age, and nutritional risk significantly affected the accuracy of estimated REE compared to measured values (p < 0.05) [48]. These findings highlight the substantial impact of clinical and metabolic factors on prediction accuracy in hospitalized populations.
Pediatric Oncology
Pediatric patients with cancer represent a special population with unique nutritional challenges and metabolic alterations. A 2025 study developing and validating REE predictive equations in 203 pediatric patients with cancer found that both new population-specific equations (INP-simple and INP-Morpho) demonstrated less bias in REE estimation (114.8, 95% CI: -408, 638) than traditional equations [20]. The Harris-Benedict, FAO, Schofield, IOM, Oxford, Kaneko, and Müller equations all demonstrated greater bias, ranging from -133.6 to -201 kcal/d [20]. Only the Molnár equation demonstrated comparable performance to the new equations, with a bias of -82.3 (95% CI: -741.3, 576.7) [20].
These findings highlight the importance of population-specific equation development, particularly in specialized populations with distinct metabolic profiles such as pediatric oncology [20]. The significant variations in REE per kilogram of body weight observed across different cancer diagnoses further underscore the need for diagnosis-specific nutritional assessment and intervention [20].
Research Reagent Solutions and Methodological Tools
Table 3: Essential Methodological Tools for REE Prediction Research
| Tool Category | Specific Examples | Research Application |
|---|---|---|
| Calorimetry Devices | Fitmate Calorimeter (Cosmed), Metabolic Carts | Gold standard measurement of VO2 and VCO2 for REE determination |
| Body Composition Analyzers | Bioelectrical Impedance Analysis (Tanita BC-418), DEXA | Assessment of fat-free mass and fat mass for body composition-based equations |
| Statistical Software | R, Python, SAS | Implementation of Bland-Altman analysis, precision calculations, and bias assessment |
| Equation Databases | FAO/WHO/UNU, Harris-Benedict, Mifflin-St Jeor, Population-specific equations | Reference equations for comparison and validation studies |
The evaluation of clinical accuracy standards for REE predictive equations reveals considerable variation in performance across different patient populations. While certain equations demonstrate acceptable accuracy in specific subgroups, no universal equation provides precise REE estimates across all clinical scenarios. The evidence consistently shows that even the best-performing equations predict within 10% of measured REE in less than 70% of cases, with performance often considerably worse in specialized populations.
Several key conclusions emerge from this analysis. First, population-specific equations generally outperform generalized equations, particularly in metabolically distinct populations such as pediatric oncology patients and those with severe obesity. Second, simple weight-based equations such as the "Thumb rule" (weight × 25) demonstrate poor accuracy and should be avoided in clinical practice. Third, clinical factors including inflammatory status, nutritional risk, body composition alterations, and specific disease states significantly impact prediction accuracy.
These findings support the recommendation that predictive equations should be used with caution, particularly in patients at nutritional risk or with extreme BMI values. When precise energy expenditure measurement is clinically critical, indirect calorimetry remains the reference standard. Future research should focus on developing more sophisticated prediction models that incorporate clinical, biochemical, and body composition parameters to improve accuracy across diverse patient populations.
Conclusion
The evaluation of REE predictive equations reveals significant limitations in universal application, with accuracy highly dependent on specific patient populations and clinical contexts. Current evidence demonstrates that population-specific equations, such as those developed for pediatric oncology patients or distinct ethnic groups, consistently outperform traditional equations. The Harris-Benedict equations show particular utility in obese populations, while newer specialized equations offer improved accuracy for specific clinical subgroups. Future research should focus on developing and validating equations for underrepresented populations, incorporating body composition metrics, and establishing standardized validation protocols. For researchers and drug development professionals, these findings emphasize the critical need for population-appropriate equation selection and continued refinement of predictive models to optimize nutritional support, clinical outcomes, and research validity across diverse patient populations.
References
- 1. Basal Metabolic Rate (BMR) and Resting Energy Expenditure ( REE ) [https://fiveable.me/nutrition-assessment/unit-7/basal-metabolic-rate-bmr-resting-energy-expenditure-ree/study-guide/MozmGekLeVGx9jcD]
- 2. Predicting Equations and Resting Energy Expenditure Changes in Overweight Adults - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7478086/]
- 3. Resting energy expenditure in adults with nonalcoholic fatty liver... [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-04416-7]
- 4. of Physical Activity and Energy Expenditure: An Overview... Assessment [https://pmc.ncbi.nlm.nih.gov/articles/PMC4428382/]
- 5. The Influence of Body Composition and Lifestyle Factors... | Preprints.org [https://www.preprints.org/manuscript/202501.1442/v1]
- 6. of Comparison for Resting Energy Expenditure... Predictive Equations [https://pmc.ncbi.nlm.nih.gov/articles/PMC3142772/]
- 7. Mifflin-St Jeor Equation [https://reference.medscape.com/calculator/846/mifflin-st-jeor-equation]
- 8. Comparison of Harris Benedict and Mifflin-ST Jeor equations with indirect calorimetry in evaluating resting energy expenditure - PubMed [https://pubmed.ncbi.nlm.nih.gov/18688113/]
- 9. of Comparison for resting energy expenditure in... predictive equations [https://link.springer.com/article/10.1007/BF03346298]
- 10. : a practical guide for clinicians Indirect calorimetry [https://pubmed.ncbi.nlm.nih.gov/17644692/]
- 11. Indirect Calorimetry: History, Technology, and Application - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6157446/]
- 12. Indirect calorimetry - Wikipedia [https://en.wikipedia.org/wiki/Indirect_calorimetry]
- 13. Frontiers | Indirect : History, Technology, and Application Calorimetry [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2018.00257/full]
- 14. Predictive equations versus measured energy expenditure by indirect calorimetry: A retrospective validation - PubMed [https://pubmed.ncbi.nlm.nih.gov/29776694/]
- 15. Comparison of Resting Energy Expenditure Using Indirect Calorimetry and Predictive Equations in Trauma Patients: A Pilot Study [https://jtraumainj.org/journal/view.php?number=1064]
- 16. A Comparison of the Indirect Calorimetry and Different Energy Equations for the Determination of Resting Energy Expenditure of Patients With Renal Transplantation - PubMed [https://pubmed.ncbi.nlm.nih.gov/32682604/]
- 17. Beyond the limits of indirect | European Journal of... calorimetry [https://www.nature.com/articles/s41430-023-01319-2?error=cookies_not_supported&code=a553a252-4e4b-4bdc-8785-b0f38edf6b04]
- 18. Extended indirect calorimetry with isotopic CO2 sensors for prolonged and continuous quantification of exogenous vs. total substrate oxidation in mice | Scientific Reports [https://www.nature.com/articles/s41598-019-47977-w]
- 19. Resting Energy Expenditure in the Elderly: Systematic Review and Comparison of Equations in an Experimental Population - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7912404/]
- 20. Frontiers | Development of a predictive for equation ... resting energy [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1656975/full]
- 21. New Predictive Equations for Resting Energy Expenditure in Normal to Overweight and Obese Population - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6935811/]
- 22. : causes and Malnutrition - PMC consequences [https://pmc.ncbi.nlm.nih.gov/articles/PMC4951875/]
- 23. Analysis of Predictive Equations for Estimating Resting Energy Expenditure in a Large Cohort of Morbidly Obese Patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/30090085/]
- 24. Performance of Predictive Equations Specifically Developed to Estimate Resting Energy Expenditure in Ventilated Critically Ill Children - PubMed [https://pubmed.ncbi.nlm.nih.gov/28108105/]
- 25. New predictive equations for estimating resting energy expenditure in subjects with normal weight and overweight - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0899900720303889]
- 26. Development of a predictive for equation ... resting energy [https://pubmed.ncbi.nlm.nih.gov/41070010/]
- 27. Development of a predictive equation for resting energy expenditure in pediatric patients with oncological diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504883/]
- 28. Predicting resting energy expenditure in underweight, normal weight, overweight, and obese adult hospital patients | Nutrition & Metabolism | Full Text [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-016-0145-3]
- 29. Prediction of resting energy expenditure in a large population of obese children - PubMed [https://pubmed.ncbi.nlm.nih.gov/15585766/]
- 30. Accuracy of Resting Energy Expenditure Predictive Equations in Patients With Cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/31347209/]
- 31. (PDF) Comparison of Resting Assessment in... Energy Expenditure [https://www.academia.edu/127914861/Comparison_of_Resting_Energy_Expenditure_Assessment_in_Pediatric_Oncology_Patients]
- 32. Basal metabolic rate [https://www.sciencedaily.com/terms/basal_metabolic_rate.htm]
- 33. and risk of diabetes, cardiovascular and other diseases... Metabolic rate [https://www.ndph.ox.ac.uk/study-with-us/dphil-population-health/choose-a-dphil-project-2025/metabolic-rate-and-risk-of-diabetes-cardiovascular-and-other-diseases-in-different-populations]
- 34. Your Metabolism and Your Body Composition | InBody USA [https://inbodyusa.com/blogs/inbodyblog/86958337-your-metabolism-and-your-body-composition/]
- 35. Body Composition – Human growth, development and nutrition [https://ebooks.inflibnet.ac.in/antp06/chapter/body-composition/]
- 36. The Role of Nutrition and Body Composition on Metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11123915/]
- 37. The human engine’s redline: Scientists discover a fundamental limit to... [https://www.naturalnews.com/2025-11-17-scientists-discover-a-fundamental-limit-to-endurance.html]
- 38. Conclusions and Recommendations - Monitoring Metabolic Status - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK215707/]
- 39. Ability of the Harris formula to Benedict requirements... predict energy [https://pmc.ncbi.nlm.nih.gov/articles/PMC2598419/]
- 40. of Comparison for predictive ... equations resting energy expenditure [https://www.dovepress.com/comparison-of-predictive-equations-for-resting-energy-expenditure-amon-peer-reviewed-fulltext-article-NDT]
- 41. – Harris - Wikipedia Benedict equation [https://en.wikipedia.org/wiki/Harris%E2%80%93Benedict_equation]
- 42. A new predictive equation for resting energy expenditure in healthy individuals - PubMed [https://pubmed.ncbi.nlm.nih.gov/2305711/]
- 43. Validation of predictive equations for resting energy expenditure in adult outpatients and inpatients - PubMed [https://pubmed.ncbi.nlm.nih.gov/17961867/]
- 44. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review - PubMed [https://pubmed.ncbi.nlm.nih.gov/15883556/]
- 45. to estimate nutritional... | Deranged Physiology Predictive equations [https://derangedphysiology.com/main/required-reading/gastrointestinal-intensive-care/Chapter-112/predictive-equations-estimate-nutritional-requirements]
- 46. Validity of predictive equations for total energy expenditure against doubly labeled water | Scientific Reports [https://www.nature.com/articles/s41598-024-66767-7]
- 47. Validation of predictive equations for resting energy expenditure in children and adolescents with different body mass indexes | Nutrition Journal | Full Text [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-023-00868-3]
- 48. The accuracy of estimating equations for total resting ... energy [https://vbn.aau.dk/en/publications/the-accuracy-of-estimating-equations-for-total-resting-energy-exp]
- 49. Exploration of an alternative to body mass index to characterize the... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8804920/]
- 50. Bias measurement in, bias results out: how an assumption free height ... [https://www.medrxiv.org/content/10.1101/2020.12.22.20248739v1.full]
- 51. Development and validation of a predictive for equation ... resting [https://pubmed.ncbi.nlm.nih.gov/40188502/]
- 52. Developing New Energy Intake Reference Values for the Saudi Population | Research Square [https://www.researchsquare.com/article/rs-5774894/v1]
- 53. Estimated glomerular filtration rate in children: adapting existing... [https://link.springer.com/article/10.1007/s00467-020-04770-6]
- 54. (PDF) Accuracy of predictive for the measurement of... equations [https://www.academia.edu/143488013/Accuracy_of_predictive_equations_for_the_measurement_of_resting_energy_expenditure_in_older_subjects]
- 55. Development and validation of new predictive for equations ... resting [https://www.researchsquare.com/article/rs-2181853/v1]
- 56. Structural equation modeling in medical research: a primer | BMC Research Notes | Full Text [https://bmcresnotes.biomedcentral.com/articles/10.1186/1756-0500-3-267]
- 57. : From ANOVA to MANOVA in 2024- Experimental Data Analysis 2025 [https://editverse.com/experimental-data-analysis-from-anova-to-manova-in-2024-2025/]
- 58. Development and Validation of prediction for estimating resting ... [https://www.slideshare.net/slideshow/b0720609/34277211]
- 59. of Comparison ... Resting Energy Expenditure Prediction Equations [https://pubmed.ncbi.nlm.nih.gov/41158959/]
- 60. Accuracy and Validity of Resting Energy Expenditure Predictive Equations in Middle-Aged Adults - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6266118/]
- 61. Development and validation of new predictive equations for resting energy expenditure in physically active boys | Scientific Reports [https://www.nature.com/articles/s41598-023-31661-1]
- 62. of five Comparison for estimating equations ... resting energy [https://eurjmedres.biomedcentral.com/articles/10.1186/2047-783X-17-26]
- 63. Frontiers | Resting Energy Expenditure of Master Athletes: Accuracy of Predictive Equations and Primary Determinants [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2021.641455/full]
- 64. 10.1 - What if the Regression Equation Contains "Wrong" Predictors? | STAT 501 [https://online.stat.psu.edu/stat501/lesson/10/10.1]
- 65. Mifflin-St. Jeor for nutrition professionals - Nutrium Blog [https://nutrium.com/blog/mifflin-st-jeor-for-nutrition-professionals/]
- 66. Overestimating Outcome Rates: Statistical Estimation When Reliability Is Suboptimal - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1955272/]
- 67. in underweight, normal weight... Predicting resting energy expenditure [https://link.springer.com/article/10.1186/s12986-016-0145-3]
- 68. of self-reported Accuracy using objective measurement in high... BMI [https://pmc.ncbi.nlm.nih.gov/articles/PMC7443770/]
- 69. Resting energy expenditure in elite athletes: development of new predictive equations based on anthropometric variables and bioelectrical impedance analysis derived phase angle - PubMed [https://pubmed.ncbi.nlm.nih.gov/34702296/]
- 70. Validity of predictive equations for resting energy expenditure in Korean non-obese adults - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6078867/]
- 71. Resting energy expenditure in the obese: a cross-validation and comparison of prediction equations - PubMed [https://pubmed.ncbi.nlm.nih.gov/8360408/]
- 72. Modeling the energetic cost of cancer as a result of altered energy... [https://tbiomed.biomedcentral.com/articles/10.1186/s12976-015-0015-0]
- 73. Novel Resting Energy Expenditure Prediction Equations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251423/]
- 74. Validation of anthropometric and bioelectrical impedance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587244/]
- 75. Development and cross-validation of predictive equations ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1499752/full]
- 76. Development and validation of new bioimpedance ... [https://www.sciencedirect.com/science/article/pii/S2405457725003717]
- 77. Accuracy and Validity of Resting ... Energy Expenditure Predictive [https://pubmed.ncbi.nlm.nih.gov/30400196/]
- 78. Prediction and evaluation of resting energy expenditure in a large group of obese outpatients - PubMed [https://pubmed.ncbi.nlm.nih.gov/28163316/]
- 79. Resting Energy Expenditure in the Elderly: Systematic Review and Comparison of Equations in an Experimental Population - PubMed [https://pubmed.ncbi.nlm.nih.gov/33573101/]
- 80. A new predictive for equation in... | CoLab resting energy expenditure [https://colab.ws/articles/10.1093%2Fajcn%2F51.2.241]
- 81. Regression Model Accuracy : R-square, AIC, BIC... - STHDA Metrics [https://www.sthda.com/english/articles/38-regression-model-validation/158-regression-model-accuracy-metrics-r-square-aic-bic-cp-and-more/]
- 82. , Recalibration, and Validation of Published... Predictive Accuracy [https://pmc.ncbi.nlm.nih.gov/articles/PMC9840647/]
- 83. Understanding Bland Altman analysis - Biochemia Medica [https://www.biochemia-medica.com/en/journal/25/2/10.11613/BM.2015.015]
- 84. Validity and Reliability of Resting Energy Expenditure Measured by Indirect Calorimetry in Adults with Overweight and Obesity: a Rapid Systematic Review | Obesity Surgery [https://link.springer.com/article/10.1007/s11695-025-08220-w]
- 85. Comparison of Resting Energy Expenditure Prediction Equations and Indirect Calorimetry Among Adults with Severe Obesity - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2475299125030008]
- 86. Resting energy expenditure in HIV/AIDS patients: Development and validation of a predictive equation - PubMed [https://pubmed.ncbi.nlm.nih.gov/33183552/]
- 87. 12 Important Model Evaluation Metrics for Machine Learning (2025) [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 88. Testing the agreement of medical instruments: overestimation of bias ... [https://pubmed.ncbi.nlm.nih.gov/23313586/]
- 89. Ranking (% obesity by country) | World Obesity Federation Global... [https://data.worldobesity.org/rankings/?age=a&sex=t]
- 90. Predictive equations for evaluation for resting energy expenditure in Brazilian patients with type 2 diabetes: what can we use? | BMC Nutrition | Full Text [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-020-00384-1]
- 91. The accuracy of estimating equations for total resting energy expenditure in hospitalized patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/40010490/]
- 92. Being too thin can be deadlier than being overweight... | ScienceDaily [https://www.sciencedaily.com/releases/2025/09/250914205759.htm]
- 93. BMR Equation Accuracy Comparison : Which Formula Predicts Your... [https://www.freecalculatorshub.com/blog/bmr-equation-accuracy-comparison]
- 94. Constrained Total Energy Expenditure and Metabolic Adaptation to Physical Activity in Adult Humans - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4803033/]
- 95. Constrained Total Energy Expenditure and Metabolic Adaptation to Physical Activity in Adult Humans - PubMed [https://pubmed.ncbi.nlm.nih.gov/26832439/]
- 96. Deciphering the constrained total energy expenditure model in humans by associating accelerometer-measured physical activity from wrist and hip | Scientific Reports [https://www.nature.com/articles/s41598-021-91750-x]
- 97. Dana-Farber Research Opens the Door to Finding More Effective... [https://blog.dana-farber.org/insight/2025/11/dana-farber-research-opens-the-door-to-finding-more-effective-treatments-for-ewing-sarcoma/]
- 98. Evaluation of mortality prediction models for oncology patients in intensive care unit [https://www.signavitae.com/articles/10.22514/sv.2025.035]
- 99. The Hallmarks of Predictive Oncology - PubMed [https://pubmed.ncbi.nlm.nih.gov/39760657/]
- 100. The Hallmarks of Predictive Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969157/]
- 101. What is a margin of error ? This statistical tool can help you... [https://theconversation.com/what-is-a-margin-of-error-this-statistical-tool-can-help-you-understand-vaccine-trials-and-political-polling-151833]
- 102. Methodological standards for the development and evaluation of... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-019-0060-y]