Saliva and Urine ELISA Protocols for Metabolic Biomarker Analysis: A Comprehensive Guide for Research and Drug Development
This article provides a detailed, protocol-focused guide for researchers and drug development professionals on employing Enzyme-Linked Immunosorbent Assay (ELISA) to quantify metabolic biomarkers in saliva and urine.
Saliva and Urine ELISA Protocols for Metabolic Biomarker Analysis: A Comprehensive Guide for Research and Drug Development
Abstract
This article provides a detailed, protocol-focused guide for researchers and drug development professionals on employing Enzyme-Linked Immunosorbent Assay (ELISA) to quantify metabolic biomarkers in saliva and urine. It covers the scientific rationale for using these non-invasive biofluids, explores their distinct advantages and biomarker profiles. A step-by-step methodological workflow is presented, addressing critical sample-specific challenges such as viscosity, osmolarity, and interfering substances. The guide includes a robust troubleshooting and optimization section to enhance assay sensitivity and reproducibility. Finally, it discusses rigorous validation strategies and compares ELISA performance with alternative analytical platforms like LC-MS/MS, providing a comprehensive resource for integrating these assays into preclinical and clinical research pipelines.
The Power of Non-Invasive Biomarkers: Understanding Saliva and Urine in Metabolic Profiling
Metabolic biomarkers are quantifiable indicators of biological processes, pathogenic states, or pharmacological responses. Their measurement in accessible biofluids like saliva and urine provides a non-invasive window into systemic health, enabling early disease detection, personalized treatment monitoring, and accelerated drug development. This application note details protocols for the analysis of salivary and urinary metabolic biomarkers within a thesis framework focusing on ELISA-based methodologies.
Key Metabolic Biomarkers and Their Clinical Significance
Table 1: Key Metabolic Biomarkers in Saliva and Urine for Disease Monitoring
| Biomarker | Primary Biofluid | Associated Disease/Condition | Significance | Typical Concentration Range |
|---|---|---|---|---|
| Cortisol | Saliva/Urine | Stress Disorders, Cushing's Syndrome, Adrenal Insufficiency | HPA axis activity indicator | Saliva: 0.5-10 nmol/L (diurnal) |
| 8-Hydroxy-2'-deoxyguanosine (8-OHdG) | Urine/Saliva | Oxidative Stress, Cancer, Neurodegenerative Diseases | DNA oxidative damage marker | Urine: 1.0-20.0 ng/mg creatinine |
| Lactate | Saliva | Periodontal Disease, Oral Cancer, Systemic Metabolic Acidosis | Anaerobic metabolism marker | Saliva: 0.5-2.5 mmol/L |
| Urea Nitrogen | Saliva | Chronic Kidney Disease | Renal function marker | Saliva: 3-7 mg/dL (correlates with serum) |
| Alpha-Amylase | Saliva | Pancreatitis, Salivary Gland Disorders, Stress | Exocrine pancreatic & salivary function | Saliva: 50-200 U/mL |
| Creatinine | Urine | Kidney Function, Muscular Disorders | Glomerular filtration rate (GFR) normalizer | Urine: 0.6-2.5 g/24h (varies with muscle mass) |
Table 2: Metabolic Biomarkers in Drug Development Phases
| Development Phase | Biomarker Utility | Example Biomarkers (Saliva/Urine) | Impact on Decision-Making |
|---|---|---|---|
| Preclinical | Target engagement, Toxicity screening | 8-OHdG (oxidative stress), Clusterin (nephrotoxicity) | Go/No-Go for candidate selection |
| Phase I/II | Pharmacodynamics, Dose optimization | Cortisol (HPA axis modulation), Lactate (metabolic shift) | Establish therapeutic window |
| Phase III | Efficacy confirmation, Safety monitoring | Disease-specific metabolite panels | Primary endpoint support |
| Post-Marketing | Long-term safety, Personalized dosing | Creatinine (renal adjustment), Immunogenicity markers | Risk management & label updates |
Detailed ELISA Protocols for Salivary and Urinary Metabolic Biomarkers
Protocol 3.1: Salivary Cortisol ELISA
Principle: Competitive ELISA measuring unbound, biologically active cortisol. Reagent Preparation:
- Coating Buffer (Carbonate-Bicarbonate, 0.05 M, pH 9.6): Dissolve 1.59 g Na₂CO₃ and 2.93 g NaHCO₃ in 1 L dH₂O.
- Saliva Collection & Pre-treatment: Collect saliva using passive drool into a polypropylene tube. Centrifuge at 10,000 x g for 15 minutes at 4°C. Collect clear supernatant. Perform a 1:10 dilution in assay buffer (0.1 M PBS, pH 7.4, 0.1% BSA). Procedure:
- Coat microplate wells with 100 µL of cortisol-3-CMO-BSA conjugate (1 µg/mL in coating buffer). Incubate overnight at 4°C.
- Wash 3x with PBS-T (0.05% Tween-20). Block with 200 µL/well of 1% BSA in PBS for 2 hours at 25°C.
- Add 50 µL of standard (0.5-50 nmol/L) or pre-treated sample per well, followed by 50 µL of anti-cortisol-HRP antibody (1:5000 dilution). Incubate 2 hours at 25°C.
- Wash 5x. Add 100 µL TMB substrate. Incubate 20 minutes in the dark.
- Stop reaction with 50 µL 2 M H₂SO₄. Read absorbance at 450 nm, reference 620 nm. Calculations: Plot log[cortisol] vs. absorbance. Use 4-parameter logistic curve fit for quantification.
Protocol 3.2: Urinary 8-OHdG Competitive ELISA
Principle: Quantifies oxidative DNA damage marker; normalizes to urinary creatinine. Sample Pre-processing:
- Collect spot urine in sterile cup. Centrifuge at 3000 x g for 10 min.
- Creatinine Measurement (Jaffe method): Dilute urine 1:50 in dH₂O. Mix 50 µL diluted sample with 200 µL alkaline picrate. Read at 492 nm after 10 min.
- For 8-OHdG, dilute urine sample 1:5 in assay buffer (provided in kit). Use immediately or store at -80°C. ELISA Steps:
- Add 50 µL standard (0.5-200 ng/mL) or diluted sample to pre-coated (anti-8-OHdG mAb) wells.
- Add 50 µL of HRP-conjugated 8-OHdG tracer to each well. Incubate 1 hour at 37°C.
- Wash 5x with provided wash buffer. Add 100 µL TMB, incubate 15 min.
- Stop with stop solution. Read at 450 nm. Normalization: 8-OHdG concentration (ng/mL) / Creatinine concentration (mg/mL) = 8-OHdG (ng/mg creatinine).
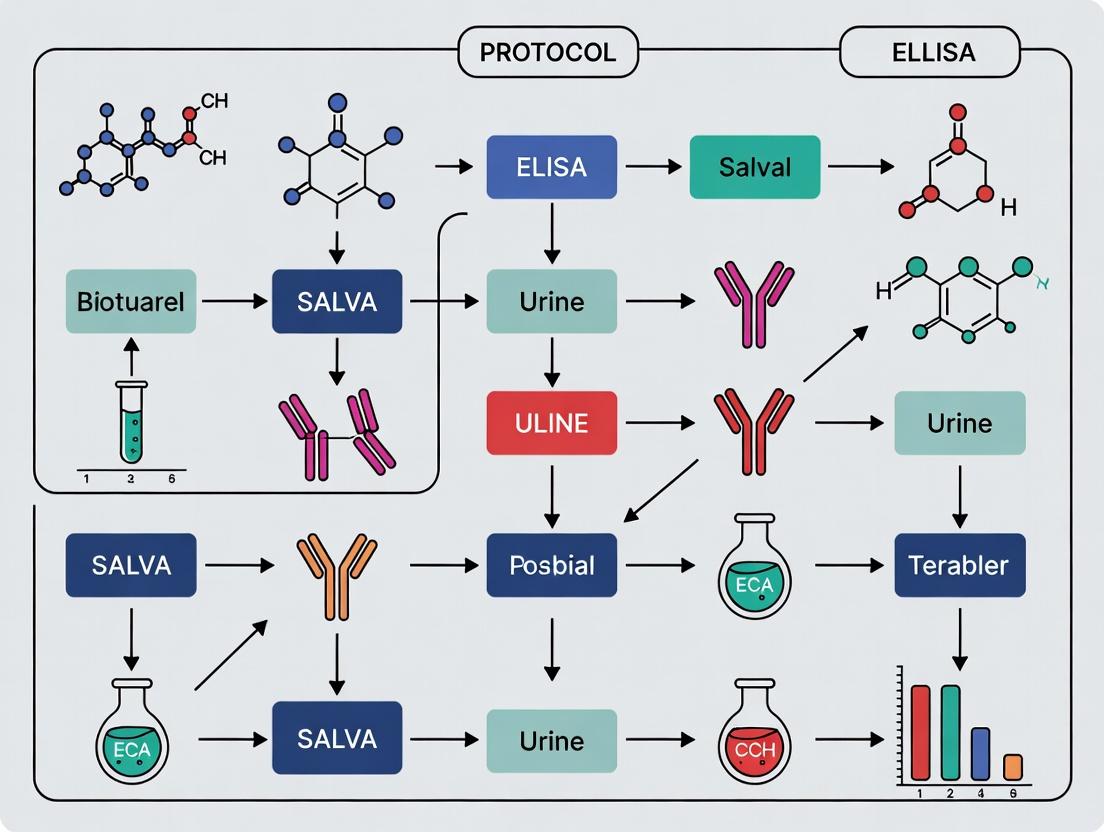
Visualizing Metabolic Pathways and Workflows
Diagram 1: Salivary Cortisol as an HPA Axis Biomarker (Workflow)
Diagram 2: Urinary 8-OHdG as an Oxidative Stress Biomarker Pathway
Diagram 3: General ELISA Protocol Workflow for Metabolic Biomarkers
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Metabolic Biomarker ELISA
| Item/Category | Function/Benefit | Example Product/Supplier Notes |
|---|---|---|
| High-Binding Polystyrene Microplates | Optimal adsorption of capture molecules (antibodies/antigens). | Corning Costar 9018; Nunc MaxiSorp. |
| Recombinant/Purified Biomarker Antigens | For standard curve generation and assay validation. | Must be identical or immunologically similar to endogenous biomarker. |
| Monoclonal/Polyclonal Antibody Pairs | Specific capture and detection for sandwich ELISA. High affinity is critical. | Validate cross-reactivity with saliva/urine matrix. |
| HRP or ALP Conjugation Kits | For labeling detection antibodies with enzymes. | Thermo Fisher Pierce kits; ensure consistent molar ratio. |
| TMB (3,3',5,5'-Tetramethylbenzidine) Substrate | HRP enzyme substrate; yields soluble blue product for colorimetric read. | Single-component, ready-to-use solutions reduce variability. |
| Stop Solution (e.g., 2M H₂SO₄) | Halts enzymatic reaction, stabilizes color for reading. | Acidic stop for TMB/HRP changes yellow. |
| Saliva Collection Aid (e.g., Salivettes) | Standardized, hygienic collection with cotton/polyester swabs. | Sarstedt Salivettes; minimizes interference. |
| Urine Preservative Tablets | Stabilize metabolites, prevent bacterial growth in spot/24h urine. | Boric acid-based tablets (e.g., Fisherbrand). |
| Matrix-Matched Calibrators & Controls | Calibrators in artificial saliva/urine account for matrix effects. | Prepare in-house or source from commercial providers. |
| Plate Washer (Automated/Manual) | Consistent removal of unbound reagents, critical for low CV%. | Use PBS with 0.05-0.1% Tween-20. |
| Microplate Reader (Absorbance/Fluorescence) | Accurate optical density measurement at specific wavelengths. | Filter-based readers (450 nm) are standard. |
Why Saliva and Urine? Advantages of Non-Invasive Sampling for Longitudinal Studies
Non-invasive sampling is pivotal for longitudinal research, where repeated measurements are required over time. Saliva and urine offer distinct logistical and ethical advantages over blood, enhancing participant compliance and enabling higher-frequency sampling.
Table 1: Comparative Analysis of Bio-Sampling Matrices
| Parameter | Blood (Serum/Plasma) | Saliva | Urine |
|---|---|---|---|
| Invasiveness | High (Venipuncture) | None | None |
| Collection Risk | Bruising, infection, pain | Minimal | Minimal |
| Participant Compliance | Low, especially for frequent draws | Very High | Very High |
| Self-Collection | Not feasible | Easy (passive drool, swab) | Easy (mid-stream catch) |
| Sampling Frequency | Limited by ethics/logistics | Very High (e.g., diurnal) | High (e.g., first morning void) |
| Pre-analytical Handling | Complex (centrifugation, aliquoting) | Simple (often just centrifugation) | Simple (often just centrifugation) |
| Primary Biomarker Class | Circulating proteins, hormones, metabolites | Steroid hormones, cytokines, immunoglobulins, drugs | Steroid hormones, metabolites, extracellular vesicles, drugs |
| Key Advantage | Gold-standard concentration | Reflects free, bioavailable fraction | Integrated concentration over time (kidney filtration) |
| Key Disadvantage | Invasiveness limits longitudinal design | Lower analyte concentration, variable viscosity | Requires normalization (e.g., to creatinine) |
Key Metabolic Biomarkers in Saliva and Urine
Table 2: Exemplar Biomarkers Amenable to ELISA in Non-Invasive Matrices
| Biomarker | Biological Role | Presence in Saliva | Presence in Urine | Research Application |
|---|---|---|---|---|
| Cortisol | Stress hormone (HPA axis) | Excellent (free fraction) | Excellent (free & metabolites) | Stress physiology, circadian rhythm |
| Alpha-Amylase | Digestive enzyme, sympathetic marker | High (secreted locally) | Low | Sympathetic nervous system activity |
| C-Reactive Protein (CRP) | Acute-phase inflammatory protein | Low but detectable | Low but detectable | Chronic low-grade inflammation |
| 8-Hydroxy-2'-Deoxyguanosine (8-OHdG) | Oxidative DNA damage product | Detectable | High (excreted) | Oxidative stress assessment |
| Interleukin-6 (IL-6) | Pro-inflammatory cytokine | Detectable | Detectable (in exosomes) | Inflammatory profiling |
| Dehydroepiandrosterone (DHEA) | Neurosteroid precursor | Good (sulfated form) | Excellent (sulfated form) | Aging, stress balance |
| Insulin-like Growth Factor 1 (IGF-1) | Growth/metabolism hormone | Low correlation with serum | Detectable | Metabolic studies |
Detailed Application Notes & Protocols
Protocol: General Pre-Analytical Processing for Saliva (Passive Drool Method)
Objective: To collect, process, and store saliva samples for downstream ELISA analysis of biomarkers such as cortisol and alpha-amylase.
Materials (Research Reagent Solutions):
- Saliva Collection Aid (e.g., Salimetrics Oral Swab or passive drool straw): Facilitates hygienic collection into a pre-chilled tube.
- Polypropylene Cryogenic Vials (e.g., Corning): Chemically inert, prevent analyte adsorption.
- Protease Inhibitor Cocktail (e.g., Sigma-Aldrich): Optional but recommended for protein/peptide biomarkers to prevent degradation.
- 0.01% Sodium Azide Solution: Optional bacteriostatic agent for long-term storage.
- Refrigerated Centrifuge (capable of 1,500-3,000 x g): For clearing mucins and debris.
- -80°C Freezer: For long-term storage.
Procedure:
- Timing & Preparation: Instruct participant to avoid eating, drinking (except water), brushing teeth, or using mouthwash for at least 30 minutes prior. Collect preferably at standardized times (e.g., upon waking, pre-lunch).
- Collection: Participant passively drools through a straw into a pre-chilled 50 mL polypropylene conical tube placed on ice until 1-2 mL is collected. Do not use stimulants (e.g., gum, citric acid) unless the biomarker is validated for stimulated saliva.
- Immediate Processing: Centrifuge samples at 2,500 x g for 15 minutes at 4°C. This step is critical to remove mucins, buccal cells, and debris.
- Aliquoting: Carefully pipette the clear supernatant (the aqueous phase) into pre-labeled cryovials. Avoid the viscous sediment and any lipid layer. Add protease inhibitors if required.
- Storage: Flash-freeze aliquots in liquid nitrogen or a -80°C freezer. Store at -80°C until analysis. Avoid repeated freeze-thaw cycles.
Protocol: General Pre-Analytical Processing for Urine (First Morning Void)
Objective: To collect, process, and normalize urine samples for ELISA analysis.
Materials (Research Reagent Solutions):
- Sterile Polypropylene Urine Collection Cups: For mid-stream catch.
- Urine Preservative Tablets (e.g., boric acid-based): Stabilize analytes if immediate processing is delayed (>2 hours).
- Creatinine Assay Kit (colorimetric or ELISA): For normalization of analyte concentration to account for hydration status.
- 0.22 µm PVDF Syringe Filter: For clarifying particulates if centrifugation is insufficient.
- Refrigerated Centrifuge.
Procedure:
- Collection: Collect first-morning void (highly concentrated) or timed collections as per study design using a mid-stream clean catch into a sterile cup.
- Preservation: If processing within 2 hours, keep on ice. If delayed, add preservative tablets as per manufacturer instructions.
- Processing: Centrifuge at 2,000 x g for 10 minutes at 4°C to remove cells and crystals.
- Aliquoting & Normalization: Aliquot supernatant. Creatinine Measurement: A separate aliquot must be used to determine creatinine concentration using a standardized assay. Final biomarker concentrations (e.g., pg/mL) are often reported as a ratio to creatinine (e.g., pg/mg creatinine).
- Storage: Store aliquots at -80°C.
Protocol: Adapted Sandwich ELISA for Salivary Cortisol
Note: This is a representative protocol. Always optimize for your specific commercial kit.
Workflow:
Diagram 1: Competitive ELISA workflow for salivary cortisol.
Key Adaptations for Saliva:
- Matrix Effects: Saliva samples and standards must be diluted in the same matrix. Use assay diluent or charcoal-stripped saliva for preparing standards.
- Sample Dilution: Cortisol in saliva typically requires no dilution or a 1:2-1:5 dilution. Validate dilution linearity.
- Interference: Centrifugation (Protocol 3.1) is mandatory to remove mucins that cause high background.
Protocol: Sandwich ELISA for Urinary 8-OHdG with Creatinine Normalization
Workflow:
Diagram 2: Dual-path workflow for urinary biomarker normalization.
Procedure Notes:
- Run the 8-OHdG ELISA according to kit instructions. Urine samples often require a 1:5 to 1:20 dilution in the provided diluent to fall within the standard curve range.
- In parallel, assay the same urine samples (neat or diluted as per assay range) for creatinine using a validated method (e.g., Jaffe reaction).
- Calculate the normalized value: (8-OHdG concentration in pg/mL) / (Creatinine concentration in mg/dL). Result is expressed as pg/mg creatinine.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for Non-Invasive Biomarker ELISA
| Item | Function & Rationale |
|---|---|
| Charcoal/Dextran-Stripped Saliva or Urine | Provides an analyte-free matrix for preparing calibration standards, critical for accurate quantification and correcting for matrix interference. |
| Cortisol ELISA Kit (Competitive) | Validated for saliva/urine; includes matched antibody pairs, conjugates, and pre-coated plates optimized for sensitivity in these matrices. |
| Human IL-6/CRP High-Sensitivity ELISA Kit | Designed to detect very low levels of inflammatory markers present in non-invasive samples. |
| Protease & Phosphatase Inhibitor Cocktail (Saliva) | Preserves protein and phosphoprotein biomarkers (e.g., cytokines) from degradation by endogenous enzymes during collection. |
| Creatinine Colorimetric Assay Kit | Essential for normalizing urinary biomarker concentrations to account for urine dilution, a major source of variability. |
| Salivary Alpha-Amylase Kinetic Assay Kit | Not an ELISA, but a key companion assay for measuring sympathetic activity via enzymatic activity in saliva. |
| Stable TMB (3,3',5,5'-Tetramethylbenzidine) Substrate | A sensitive, low-background chromogen for HRP-based ELISA detection. One-step, ready-to-use solutions ensure reproducibility. |
| Low-Binding Microcentrifuge Tubes & Pipette Tips | Minimize adsorptive loss of low-abundance proteins and steroid hormones to plastic surfaces during processing. |
Key Metabolic Biomarkers Detectable in Saliva (e.g., cortisol, cytokines, oxidative stress markers)
Application Notes Saliva is a valuable, non-invasive biofluid for monitoring metabolic status, stress response, and inflammation. Its collection is simple, cost-effective, and suitable for high-frequency sampling. Within a broader thesis on ELISA protocols for metabolic biomarkers across biofluids, salivary analysis provides a critical correlate to urinary data, offering insights into systemic physiology with different temporal dynamics.
Key Biomarker Classes and Quantitative Data
Table 1: Primary Metabolic Biomarkers in Saliva and Their Significance
| Biomarker Class | Example Analytes | Typical Salivary Concentration Range (Healthy Adults) | Physiological & Research Significance |
|---|---|---|---|
| Stress Hormones | Cortisol | 0.5 - 4.0 ng/mL (diurnal variation) | Hypothalamic-pituitary-adrenal (HPA) axis activity, chronic stress, metabolic syndrome. |
| Alpha-amylase (surrogate) | 20 - 400 U/mL | Sympathetic nervous system (SNS) activity. | |
| Inflammatory Cytokines | Interleukin-1β (IL-1β) | 5 - 100 pg/mL | Local & systemic inflammation, periodontitis, response to infection. |
| Interleukin-6 (IL-6) | 1 - 50 pg/mL | Acute phase response, metabolic inflammation. | |
| Tumor Necrosis Factor-α (TNF-α) | 0.5 - 20 pg/mL | Pro-inflammatory signaling. | |
| Oxidative Stress Markers | 8-hydroxy-2'-deoxyguanosine (8-OHdG) | 100 - 1000 pg/mL | Oxidative DNA damage. |
| Malondialdehyde (MDA) | 0.5 - 5.0 µM | Lipid peroxidation end-product. | |
| Metabolic Hormones | Insulin | 5 - 30 µIU/mL | Insulin resistance, metabolic health. |
| Leptin | 10 - 200 pg/mL | Adipose tissue signaling, satiety. |
Detailed Experimental Protocols
Protocol 1: Saliva Collection and Pre-processing for ELISA Objective: To obtain clean, stable saliva samples for reproducible biomarker quantification. Materials: Saliva collection aid (polyethylene straw, Salivette), sterile cryovials, low-speed centrifuge, -80°C freezer.
- Pre-collection: Participant should fast (water only) and abstain from brushing teeth, eating, or drinking (except water) for at least 60 minutes prior.
- Collection: Use passive drool into a pre-chilled tube over 5-10 minutes, aiming for ≥1 mL. Alternatively, use a Salivette cotton swab chewed for 1-2 minutes.
- Processing: Centrifuge raw saliva at 4°C, 1500-3000 x g for 15 minutes.
- Aliquoting: Carefully aspirate the clear supernatant (cell-free saliva) avoiding the pellet and mucous layer. Aliquot into cryovials.
- Storage: Immediately snap-freeze and store at ≤ -80°C. Avoid repeated freeze-thaw cycles (≤3 recommended).
Protocol 2: High-Sensitivity Salivary Cortisol ELISA Objective: To quantify low levels of free cortisol in saliva. Materials: Commercial high-sensitivity cortisol ELISA kit (e.g., Salimetrics, DRG International), microplate reader (450 nm), vortex mixer.
- Thaw & Centrifuge: Thaw samples on ice, vortex, and centrifuge at 4°C, 1500 x g for 10 minutes.
- Plate Setup: Reconstitute standards as per kit. Pipette 25 µL of standard, control, or sample in duplicate to appropriate wells.
- Assay Procedure: Add 100 µL of Enzyme Conjugate to each well. Incubate for 60 minutes at room temperature (RT) on a plate shaker.
- Wash: Manually or automatically wash wells 3 times with Wash Buffer.
- Substrate: Add 100 µL of TMB Substrate. Incubate for 30 minutes in the dark at RT.
- Stop & Read: Add 100 µL of Stop Solution. Read optical density at 450 nm within 15 minutes.
- Analysis: Generate a 4- or 5-parameter logistic standard curve. Apply correction for dilution factor if used.
Protocol 3: Salivary Cytokine (IL-1β) ELISA Protocol Objective: To measure pro-inflammatory cytokine IL-1β in saliva. Materials: Commercial Human IL-1β ELISA Kit (e.g., R&D Systems DuoSet), plate washer, precision pipettes.
- Sample Prep: Thaw and centrifuge as in Protocol 1. Due to potential matrix effects, a dilution series (1:2, 1:4 in Calibrator Diluent) is recommended for initial validation.
- Coating: Coat plate with 100 µL/well of capture antibody overnight at RT.
- Blocking: Aspirate, wash 3x, then block with 300 µL/well of Reagent Diluent for 1 hour at RT.
- Incubations: Add 100 µL of standard or sample per well. Incubate 2 hours at RT. Wash, then add detection antibody (2 hours), followed by Streptavidin-HRP (20 minutes, protected from light).
- Detection: Add 100 µL of Substrate Solution (1:1 mixture of Color Reagents A & B). Incubate 20 minutes in the dark.
- Stop & Read: Add 50 µL of Stop Solution. Read immediately at 450 nm, with 540 nm or 570 nm wavelength correction.
- Analysis: Subtract corrected 540 nm readings. Plot standard curve and interpolate sample concentrations.
Visualizations
Title: Saliva Sample Processing Workflow
Title: Biomarker Pathways from Source to Saliva
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Salivary Biomarker ELISA
| Item | Function/Benefit |
|---|---|
| Cortisol ELISA Kit (High-Sensitivity) | Optimized for saliva matrix; measures physiologically relevant low levels. |
| Cytokine ELISA Kit (DuoSet or similar) | Allows separate antibody pair purchase; superior flexibility and optimization for saliva. |
| Saliva Collection Aid (Salivette) | Standardizes collection, contains neutral cotton/polyester swab; reduces mucins. |
| Protease & Phosphatase Inhibitor Cocktails | Added pre-collection or during processing to prevent biomarker degradation. |
| Reagent Diluent for Serum/Plasma | Often requires optimization (e.g., adding saliva diluent) to overcome saliva matrix effects. |
| Recombinant Biomarker Standards | Essential for generating accurate standard curves in the appropriate buffer matrix. |
| Low-Binding Microcentrifuge Tubes & Pipette Tips | Minimizes analyte loss due to adsorption to plastic surfaces. |
| TMB (3,3',5,5'-Tetramethylbenzidine) Substrate | Sensitive, colorimetric HRP substrate for detection. |
| Wash Buffer Concentrate (10-25X) | Provides consistent washing; contains buffered saline with Tween-20. |
Key Metabolic Biomarkers Detectable in Urine (e.g., 8-OHdG, prostaglandins, steroid metabolites)
Within the broader thesis investigating ELISA protocols for metabolic biomarkers in saliva and urine, this document details application notes and protocols for key urinary biomarkers. Urine offers a non-invasive, metabolically rich matrix reflecting systemic oxidative stress, inflammation, and endocrine function. Accurate detection of these biomarkers via ELISA is critical for research in chronic disease, toxicology, and drug development.
Table 1: Key Urinary Metabolic Biomarkers, Their Significance, and Typical Detection Ranges
| Biomarker Category | Specific Example | Primary Biological Significance | Typical Urinary Concentration Range (Reported in Literature) | Common ELISA Assay Type |
|---|---|---|---|---|
| Oxidative Stress | 8-Hydroxy-2'-deoxyguanosine (8-OHdG) | DNA oxidation damage product; biomarker of oxidative stress | 1.5 - 45 ng/mg creatinine | Competitive ELISA |
| Inflammation | Prostaglandin E2 (PGE2) | Key mediator of inflammation, pain, and fever | 100 - 800 pg/mg creatinine | Sandwich ELISA |
| Inflammation | 11β-Prostaglandin F2α (11β-PGF2α) | Stable metabolite of PGD2; marker for mast cell activation | 50 - 500 pg/mg creatinine | Competitive ELISA |
| Steroid Metabolism | Cortisol (free) | Active glucocorticoid; indicator of HPA axis activity | 10 - 60 µg/g creatinine | Competitive ELISA |
| Steroid Metabolism | Testosterone metabolites (e.g., Androsterone) | Androgen activity and metabolic pathways | Varies widely by sex & age | Competitive/Sandwich ELISA |
| Steroid Metabolism | Estradiol metabolites (e.g., Estrone-3-glucuronide) | Estrogen activity and metabolism | Varies with menstrual cycle | Competitive ELISA |
Detailed ELISA Protocols for Urinary Biomarkers
Protocol 1: Competitive ELISA for 8-OHdG in Urine
Principle: Native urinary 8-OHdG competes with a fixed amount of enzyme-conjugated 8-OHdG for binding to pre-coated anti-8-OHdG antibodies. Signal is inversely proportional to analyte concentration.
Pre-Analytical Urine Processing:
- Collection & Storage: Collect spot urine in preservative-free containers. Centrifuge at 3,000 x g for 10 min at 4°C to remove particulate matter. Aliquot supernatant and store at -80°C. Avoid multiple freeze-thaw cycles.
- Creatinine Normalization: Analyze creatinine concentration for each sample using a standard colorimetric assay (e.g., Jaffé method). All final biomarker concentrations should be normalized to mg or g of creatinine to account for urine dilution.
- Sample Dilution: Dilute urine supernatant 1:5 to 1:20 in the provided ELISA assay buffer to bring the expected 8-OHdG concentration within the standard curve range.
ELISA Procedure:
- Preparation: Bring all reagents, samples, and standards to room temperature (RT). Reconstitute standards as per kit instructions.
- Loading: Add 50 µL of standard or diluted sample to appropriate wells of the pre-coated anti-8-OHdG microplate. Immediately add 50 µL of the HRP-conjugated 8-OHdG reagent to each well.
- Incubation: Cover plate and incubate for 60 min at RT on a microplate shaker.
- Washing: Aspirate and wash each well 5 times with 300 µL of 1X Wash Buffer. Blot plate dry on absorbent paper.
- Detection: Add 100 µL of TMB Substrate Solution to each well. Incubate for 15 min at RT in the dark.
- Stop Reaction: Add 100 µL of Stop Solution. The blue color will turn yellow.
- Reading: Measure the absorbance at 450 nm (reference 620 nm) within 15 min using a microplate reader.
- Calculation: Generate a sigmoidal standard curve by plotting the log of the standard concentration (x-axis) against the %B/B0 (y-axis). Interpolate sample concentrations from the curve and multiply by the dilution factor and creatinine normalization factor.
Protocol 2: Sandwich ELISA for Prostaglandin E2 (PGE2) in Urine
Principle: A capture antibody specific for PGE2 is coated on the plate. Urinary PGE2 is "sandwiched" between this capture antibody and a second detection antibody conjugated to HRP.
Pre-Analytical Urine Processing:
- Collection & Stabilization: Add a cyclooxygenase inhibitor (e.g., indomethacin at 1 µM final concentration) to the collection tube prior to voiding to prevent ex vivo prostaglandin synthesis.
- Extraction (Optional but Recommended for Sensitivity): Acidify 1 mL of urine to pH 3.5 with HCl. Pass through a pre-activated C18 solid-phase extraction (SPE) column. Wash with water and hexane. Elute PGE2 with ethyl acetate. Evaporate eluent under nitrogen and reconstitute in ELISA buffer.
- Dilution: Dilute extracted or raw urine 1:2 to 1:10 in assay buffer.
ELISA Procedure:
- Preparation: As per Protocol 1.
- Loading: Add 100 µL of standard or diluted sample to the antibody-coated wells.
- Incubation & Capture: Cover and incubate for 2 hours at RT on a shaker.
- Washing: Wash 5 times as in Protocol 1.
- Detection Antibody Incubation: Add 100 µL of the HRP-conjugated anti-PGE2 detection antibody to each well. Incubate for 1 hour at RT on a shaker.
- Washing: Repeat wash step.
- Substrate, Stop, Read: Follow steps 5-7 from Protocol 1.
- Calculation: Generate a linear or four-parameter logistic standard curve of absorbance vs. concentration. Interpolate sample values and apply dilution, extraction efficiency, and creatinine normalization factors.
Visualization of Workflows and Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Urinary Biomarker ELISA Research
| Item | Function & Rationale |
|---|---|
| Commercial ELISA Kits (Validated for Urine) | Provide optimized, pre-coated plates, matched antibody pairs, standards, and buffers specific for the target analyte, ensuring reproducibility. |
| C18 Solid-Phase Extraction (SPE) Columns | For purifying and concentrating prostaglandins and steroids from urine, removing salts and interfering substances to improve assay sensitivity. |
| Creatinine Assay Kit (Colorimetric) | Essential for normalizing biomarker concentration to urine dilution, a standard practice in urinary biomarker research. |
| Microplate Washer | Ensures consistent and thorough washing of ELISA plates, critical for reducing background noise and improving precision. |
| Spectrophotometric Microplate Reader | For accurate measurement of absorbance at 450 nm (and reference wavelength) to quantify ELISA results. |
| Urine Stabilizer Cocktails | Inhibitor mixes (e.g., for cyclooxygenase) to prevent ex vivo synthesis or degradation of labile biomarkers like prostaglandins during collection. |
| Standard Curve Fitting Software | Software (e.g., Four-Parameter Logistic, linear regression) for accurate interpolation of sample concentrations from absorbance values. |
| pH Adjustment Reagents | Required for optimizing sample conditions prior to SPE extraction (e.g., acidification for prostaglandin extraction). |
This application note details critical pre-analytical protocols for saliva and urine biomarker research, specifically within the context of ELISA-based metabolic studies. The integrity of downstream ELISA quantification for biomarkers (e.g., cortisol, 8-OHdG, neopterin, cytokines) is entirely contingent upon stringent control of collection, stabilization, and storage. Failure to standardize these initial phases is a primary source of inter-study variability and irreproducible data, directly impacting drug development pipelines.
Collection Protocols
Saliva Collection
Primary Objective: Obtain a representative, uncontaminated sample without stimulating or altering salivary flow and composition. Key Variables: Collection method, time of day, participant state (fasting, posture), oral health status.
Detailed Protocol: Passive Drool Method (Recommended for Quantitative ELISA)
- Participant Preparation: Require a 1-hour pre-collection fast (water only). No brushing/flossing 45 minutes prior. Rinse mouth with water 10 minutes before collection.
- Timing: For diurnal biomarkers (e.g., cortisol), collect at standardized times (e.g., waking, 30 min post-waking, bedtime). Record exact collection time.
- Procedure: a. Have the participant pool saliva in the mouth for 30 seconds. b. Tilt head forward and allow saliva to passively drain via a short, wide straw into a pre-chilled, DNA/RNase-free polypropylene tube placed on ice. c. Continue until ≥ 2 mL is collected. Avoid forceful expectoration (can introduce foam and particulate matter). d. Cap tube and invert gently 3-5 times to mix with any preservative.
- Immediate Processing: Place tube on wet ice and proceed to centrifugation within 30 minutes of collection.
Urine Collection
Primary Objective: Obtain a stable, representative sample, accounting for biomarker concentration variability (e.g., via creatinine correction). Key Variables: Collection type (spot, first morning, 24-hour), preservation method, pH.
Detailed Protocol: Mid-Stream Clean Catch (Spot Urine for Metabolic Biomarkers)
- Container: Use sterile, preservative-free polypropylene containers. For 24-hour collections, use a large, dark container with pre-added stabilizer (e.g., boric acid).
- Procedure: a. Discard the initial stream of urine. b. Collect a mid-stream sample (typically 10-50 mL) without interrupting flow. c. Record collection time and, if possible, last void time. d. Aliquot immediately for stabilization.
Stabilization & Immediate Processing Protocols
Stabilization is non-negotiable to halt enzymatic degradation, bacterial growth, and oxidative degradation of target analytes.
Saliva Processing Protocol
- Centrifugation: Spin collected saliva at 2,600 x g for 15 minutes at 4°C.
- Phase Separation: Post-centrifugation, three phases are visible:
- Top layer: Lipid-rich, opaque foam (discard by gentle aspiration).
- Middle layer: Aqueous, clear supernatant (contains soluble biomarkers). This is the analysis fraction.
- Bottom layer: Mucins, debris, and cellular components (pellet).
- Aliquoting & Stabilization: Piper the clear supernatant into pre-labeled 0.5 mL cryovials. Add protease inhibitor cocktail (e.g., 1 µL per 100 µL saliva) to aliquots for cytokine analysis. For cortisol, acid-stable inhibitors may be required.
- pH Measurement (Optional but Recommended): Record pH of an aliquot. Salivary pH < 6.5 can degrade certain biomarkers.
Urine Stabilization Protocol
- Preservative Addition: For general metabolic panels, immediately add commercial urine preservative tablets (e.g., containing sodium azide, EDTA) per manufacturer's instructions. For oxidative stress markers (e.g., 8-OHdG), add 10 mM EDTA and 0.1% butylated hydroxytoluene (BHT).
- pH Adjustment: For many analytes, adjust pH to 7.0-7.5 using 1M NaOH or HCl to prevent acid hydrolysis.
- Centrifugation & Filtration: Clarify by centrifugation at 2,000 x g for 10 minutes at 4°C. Filter supernatant through a 0.8 µm syringe filter to remove residual particulates.
- Creatinine Normalization: Immediately after processing, analyze an aliquot for creatinine concentration to enable future biomarker normalization.
Table 1: Stabilization Agents & Their Applications
| Stabilizer | Target Class | Mechanism | Example Biomarker | Final Concentration in Sample |
|---|---|---|---|---|
| Protease Inhibitor Cocktail | Peptides/Proteins | Inhibits serine, cysteine, metalloproteases | Cytokines (IL-6), Enzymes | 1% v/v |
| Sodium Azide | Microbial Growth | Bacteriostatic | General | 0.1% w/v |
| EDTA | Metalloenzymes, Oxidative Stress | Chelates divalent cations (Ca2+, Mg2+) | 8-OHdG, MMPs | 1-10 mM |
| BHT | Lipid Oxidation | Antioxidant | Isoprostanes | 0.01-0.1% |
| Acid (HCl) | Catecholamines | Prevents degradation | Cortisol (specific assays) | pH ~3 |
Storage & Logistics Protocols
Table 2: Storage Conditions for Saliva & Urine Biomarkers
| Biomarker Category | Sample Type | Short-term (≤1 week) | Long-term (>1 week) | Freeze-Thaw Cycles (Max) | Key Degradation Risk |
|---|---|---|---|---|---|
| Steroid Hormones | Saliva | -20°C | -80°C | 3 | Adsorption to tube walls |
| Cytokines/Chemokines | Saliva | -80°C | -80°C (in vapor phase LN2 preferred) | 1 | Proteolytic cleavage |
| Oxidative Stress Markers | Urine | -80°C, with antioxidant | -80°C under argon | 2 | Oxidation |
| Metabolic Panels (LC-MS) | Both | -80°C | -80°C | 2 | Enzymatic activity |
Protocol for Aliquot Storage:
- Aliquot processed samples into single-use volumes to avoid repeated freeze-thaw cycles.
- Use low-protein-binding, internally-threaded cryovials.
- For long-term storage at -80°C, place vials in sealed plastic bags or boxes to prevent desiccation (freezer burn).
- Maintain a detailed sample inventory with location, freeze date, and freeze-thaw history.
Experimental Protocol: Validation of Pre-Analytical Conditions
Aim: To empirically determine the impact of varying pre-analytical conditions on the recovery of a target metabolic biomarker (e.g., salivary cortisol) via ELISA.
Materials: See The Scientist's Toolkit below.
Method:
- Sample Collection: Collect a large-volume saliva pool from a single donor under controlled conditions.
- Baseline Processing: Immediately process a reference aliquot (T=0) per the optimal protocol (centrifugation, inhibitor addition, snap-freeze).
- Variable Introduction: Process remaining pool with deliberate variables:
- Variable A (Time Delay): Hold samples at room temperature for 0, 30, 60, 120 min before processing.
- Variable B (Temperature): Hold samples for 60 min on ice, at RT (22°C), or at 37°C before processing.
- Variable C (Freeze-Thaw): Subject aliquots to 0, 1, 3, or 5 freeze-thaw cycles.
- ELISA Analysis: Analyze all samples in the same ELISA batch, in duplicate, following manufacturer protocol.
- Data Analysis: Express biomarker concentration as a percentage of the T=0 reference control. Perform ANOVA to determine significant degradation thresholds.
Visualizations
The Scientist's Toolkit
| Research Reagent / Material | Function in Pre-Analytical Phase | Critical Specification / Example |
|---|---|---|
| DNA/RNase-Free Polypropylene Tubes (Saliva) | Minimizes biomarker adsorption; prevents nucleic acid contamination | Low protein-binding, sterile, with secure cap (e.g., Sarstedt Salivette alternatives) |
| Sterile Urine Collection Cup | Aseptic collection to limit bacterial load at source | Polypropylene, wide mouth, graduated volume markings |
| Protease Inhibitor Cocktail (Broad-Spectrum) | Halts endogenous proteolysis of protein biomarkers | Must be compatible with saliva/urine pH; EDTA-free if needed for downstream assays |
| Urine Preservative Tablets | Stabilizes metabolic profile for up to 72h at RT | Typically contain bacteriostatic agents (sodium azide) and buffers |
| Low-Protein-Binding Cryovials (0.5-2.0 mL) | Prevents analyte loss during long-term storage | Internally threaded, silicone O-ring, sterile (e.g., Nunc) |
| pH Test Strips (Range 4.0-9.0) | Rapid pH verification for stabilization optimization | Non-bleeding, high resolution (0.5 pH unit increments) |
| Benchtop Refrigerated Centrifuge | Rapid sample clarification at controlled temperature | Fixed-angle rotor capable of 2,600 x g at 4°C for 15 mL tubes |
| Portable Wet Ice or Cold Packs | Maintains sample integrity from collection to lab | Consistent temperature (~0°C) for transport |
| Sample Inventory Software (LIMS) | Tracks storage location, freeze-thaw cycles, and chain of custody | Barcode compatible, cloud-based for multi-user access |
Introduction (Within Thesis Context) This document provides Application Notes and Protocols to support a thesis investigating ELISA for metabolic biomarkers in saliva and urine. Accurate quantification is fundamentally challenged by matrix-specific interfering substances. These protocols outline systematic approaches to characterize and mitigate these effects, which is critical for developing robust, translatable assays in clinical research and drug development.
1. Comparative Matrix Composition & Challenges Saliva and urine present distinct matrices that introduce specific interferences in immunoassays like ELISA. Key challenges are summarized below.
Table 1: Primary Matrix Effects and Interfering Substances
| Matrix | Key Interfering Substances | Primary Effects on ELISA | Typical Concentration Ranges |
|---|---|---|---|
| Saliva | Mucins (e.g., MUC5B), α-amylase, food debris, bacterial enzymes, variable pH (6.2-7.6) | High viscosity, non-specific binding, analyte degradation/proteolysis, altered antibody-antigen kinetics. | Mucins: 0.5-2.5 mg/mL; α-amylase: 50-200 U/mL. |
| Urine | Urea, creatinine, salts (high ionic strength), urinary pigments (urobilinogen), pH variability (4.6-8.0) | High osmolarity, chemical denaturation of antibodies, spectral interference in colorimetric detection, hook effect. | Urea: 200-400 mM; Creatinine: 3-20 mM. |
| Common to Both | Human Anti-Animal Antibodies (HAAA), heterophilic antibodies, lipids, dissolved drugs/metabolites. | False positives/negatives via cross-linking or blocking. | HAAA prevalence: 1-15% of population. |
2. Experimental Protocols for Characterizing Matrix Effects
Protocol 2.1: Spike-and-Recovery and Linear Dilution Test Objective: To assess the impact of matrix components on analyte detection accuracy and parallelism. Materials: Purified target analyte standard, pooled saliva (stimulated), pooled urine (first morning void), assay buffer, candidate ELISA kit. Procedure:
- Prepare a high-concentration stock of the purified analyte in assay buffer.
- Generate two sets of serial dilutions: one in assay buffer (Buffer Standard) and one in the biological matrix (Matrix Standard). Use a minimum of 5 dilution points spanning the assay's dynamic range.
- For spike-and-recovery, prepare matrix samples spiked with a known mid-range concentration of analyte. Include unspiked matrix controls.
- Run all samples in duplicate on the ELISA according to the manufacturer's protocol, with appropriate buffer-only blanks.
- Calculation: % Recovery = [(Measured concentration in spiked matrix – Measured concentration in unspiked matrix) / Theoretical spike concentration] x 100. Parallelism is assessed by comparing the slopes of the Buffer vs. Matrix standard curves after log-log transformation. Acceptance Criterion: Recovery of 80-120% and parallelism (matrix slope / buffer slope) of 0.90-1.10 suggest minimal interference.
Protocol 2.2: Protocol for Mitigating Interferences via Sample Pre-Treatment Objective: To evaluate pre-treatment methods for reducing matrix effects. Materials: Saliva/urine samples, centrifugation filters (e.g., 10kDa MWCO), solid-phase extraction (SPE) columns for analyte purification, lipid-removing agents (e.g., LipidURE), heterophilic antibody blocking reagents. Procedure: A. For Viscosity/Protein Removal (Saliva Focus):
- Centrifuge raw saliva at 10,000 x g for 10 minutes at 4°C to remove debris.
- Aliquot supernatant for: a) No further treatment (control), b) Additional filtration through a 0.22μm syringe filter, c) Centrifugal ultrafiltration (10kDa MWCO) to exclude high-MW mucins. B. For Heterophilic Antibody Blocking:
- Add a proprietary heterophilic blocking reagent (HBR) or increased non-specific IgG (e.g., 1% w/v) to the assay buffer or sample diluent.
- Pre-incubate samples with this modified buffer for 30-60 minutes prior to ELISA. C. For Analyte Extraction/Concentration (Urine Focus):
- Acidify urine sample to pH ~3.0 (if analyte is stable).
- Pass through a conditioned reversed-phase SPE column.
- Wash with 5% methanol/water, elute with 70% methanol/water.
- Dry eluent under nitrogen and reconstitute in assay buffer. Validation: Perform spike-and-recovery (Protocol 2.1) on pre-treated vs. raw samples to quantify improvement.
3. The Scientist's Toolkit: Essential Reagent Solutions
Table 2: Key Research Reagent Solutions
| Reagent/Material | Primary Function | Application Note |
|---|---|---|
| Heterophilic Blocking Reagent (HBR) | Blocks human anti-mouse antibodies (HAMA) and other heterophilic interferents, reducing false signals. | Essential for both saliva and urine. Add to diluent or pre-incubate with sample. |
| Protease Inhibitor Cocktail (EDTA-free) | Inhibits salivary proteases (e.g., amylase) and bacterial enzymes that degrade analyte or assay components. | Critical for saliva. Add immediately upon collection. |
| Lipid Removal Agent (e.g., LipidURE) | Precipitates and removes lipids that cause non-specific binding or turbidity. | Useful for lipemic saliva samples. |
| Stabilized Analyte Standards | Pure analyte in a defined buffer for generating standard curves. | Must be matrix-matched or validated via recovery studies. |
| Matrix-Matched Calibrators | Analyte standards prepared in a characterized, artificial or stripped matrix. | Gold standard for accurate quantification; difficult to source for saliva. |
| High-Binding, Low-Protein Binding Plates | Optimized microplates for ELISA. | Low-protein binding plates can reduce non-specific adsorption of interfering proteins. |
4. Visualization of Workflows and Pathways
Title: ELISA Matrix Validation & Mitigation Workflow
Title: Common Interferents and Their Effects on ELISA
Step-by-Step ELISA Protocols: From Sample Prep to Data Acquisition for Saliva and Urine
Within the context of developing robust ELISA protocols for metabolic biomarkers in saliva and urine, the selection of the appropriate assay format is a foundational decision. This choice, primarily between competitive and sandwich ELISA, is dictated by the molecular size and structural characteristics of the target analyte. This application note provides a detailed comparison, protocols, and key considerations to guide researchers and drug development professionals in assay design for biomarker validation.
Core Principles and Format Selection
The fundamental difference between the two formats lies in the number of antibody epitopes required.
Sandwich ELISA: Requires two distinct, non-overlapping epitopes. A capture antibody is immobilized on the plate, binding the target analyte, which is then detected by a second, enzyme-conjugated detection antibody. This format is ideal for large proteins (>10 kDa).
Competitive ELISA: Employed when the analyte is too small to be bound by two antibodies simultaneously (e.g., haptens, peptides, small molecules <5 kDa). The analyte in the sample competes with a labeled analyte (conjugate) for a limited number of immobilized antibody binding sites. The signal is inversely proportional to the analyte concentration.
The logical selection process is summarized in the following diagram:
Diagram Title: ELISA Format Selection Logic Based on Analyte Properties
Quantitative Comparison of ELISA Formats
Table 1: Characteristics of Competitive vs. Sandwich ELISA Formats
| Parameter | Competitive ELISA | Sandwich ELISA |
|---|---|---|
| Optimal Analyte Size | < 5 kDa (haptens, steroids, drugs) | > 10 kDa (cytokines, hormones, antibodies) |
| Antibody Requirement | One high-affinity, epitope-specific antibody. | Two antibodies targeting different epitopes. |
| Assay Time | Typically shorter (2-3 hrs). | Typically longer (3-5 hrs) due to extra step. |
| Sensitivity Range | Varies; often in ng/mL to µg/mL range. | Generally higher; often in pg/mL to ng/mL range. |
| Dynamic Range | Narrower (1.5-2 log). | Broader (2-3 log). |
| Signal Relationship | Signal inversely proportional to analyte concentration. | Signal directly proportional to analyte concentration. |
| Interference Risk | Lower risk from heterophilic antibodies. | Higher risk from heterophilic antibody interference. |
| Best for Biomarkers in | Small molecule metabolites (e.g., cortisol, estradiol), drugs. | Protein biomarkers (e.g., IL-6, CRP, amylase). |
Detailed Protocols
Protocol 1: Competitive ELISA for Cortisol in Saliva
Application: Measurement of low-molecular-weight metabolic stress biomarkers.
Key Research Reagent Solutions:
- 96-Well Microplate: Pre-coated with goat anti-rabbit IgG. Function: Solid phase for immobilization of capture antibody.
- Cortisol Standards: Prepared in steroid-free saliva matrix. Function: Calibration curve for quantification.
- Cortisol-HRP Conjugate: Cortisol linked to Horseradish Peroxidase. Function: Competes with sample cortisol for antibody binding.
- Anti-Cortisol Polyclonal Antibody (Rabbit): Primary specific antibody. Function: Binds both free cortisol and cortisol-HRP.
- TMB Substrate Solution: 3,3',5,5'-Tetramethylbenzidine. Function: Chromogenic enzyme substrate for color development.
- Stop Solution (1M H₂SO₄): Function: Terminates enzymatic reaction, stabilizes final color.
Methodology:
- Coating: Add diluted anti-cortisol antibody to goat anti-rabbit IgG coated plate. Incubate 1 hour at room temperature (RT). Wash 3x.
- Competition: Add 50 µL of cortisol standard or sample + 50 µL of cortisol-HRP conjugate to each well. Incubate 1 hour at RT on a shaker.
- Wash: Wash plate 5x with wash buffer.
- Detection: Add 100 µL TMB substrate. Incubate 15 minutes in the dark.
- Stop & Read: Add 100 µL stop solution. Measure absorbance at 450 nm immediately.
The competitive assay workflow is detailed below:
Diagram Title: Competitive ELISA Workflow for Small Molecules
Protocol 2: Sandwich ELISA for Amylase in Urine
Application: Measurement of protein biomarkers of metabolic or inflammatory status.
Key Research Reagent Solutions:
- Capture Antibody (Mouse Monoclonal): Coated on plate. Function: Specifically binds target protein from sample.
- Detection Antibody (Rabbit Polyclonal): Biotin-conjugated. Function: Binds a different epitope on the captured target.
- Streptavidin-HRP Conjugate: Function: Binds biotin on detection antibody, provides enzymatic signal amplification.
- Recombinant Protein Standard: Function: Provides precise calibration curve.
- Sample Diluent (with blockers): Contains protein (BSA) and detergent. Function: Reduces non-specific binding.
Methodology:
- Capture: Add 100 µL of sample or standard to coated plate. Incubate 2 hours at RT. Wash 4x.
- Detection: Add 100 µL biotinylated detection antibody. Incubate 1 hour at RT. Wash 4x.
- Signal Amplification: Add 100 µL Streptavidin-HRP. Incubate 30 minutes at RT. Wash 5x.
- Development: Add 100 µL TMB. Incubate 10-20 minutes in the dark.
- Stop & Read: Add 100 µL stop solution. Read absorbance at 450 nm.
The sandwich assay workflow is visualized as follows:
Diagram Title: Sandwich ELISA Workflow for Protein Biomarkers
Critical Considerations for Saliva and Urine Biomarkers
- Matrix Effects: Saliva contains mucins; urine varies in salt and pH. Both require dilution or use of matrix-matched standards.
- Analyte Stability: Some small molecule metabolites may be light- or temperature-sensitive. Protein degradation by proteases in urine must be inhibited.
- Sensitivity Requirements: Biomarker concentrations in saliva/urine can be low. The superior sensitivity of sandwich ELISA is preferred for proteins when feasible.
For a thesis focused on metabolic biomarkers in saliva and urine, the selection is clear: competitive ELISA is the default for small molecule metabolites (e.g., cortisol, steroid hormones), while sandwich ELISA is optimal for larger protein biomarkers (e.g., amylase, cytokines). This strategic choice ensures assay robustness, sensitivity, and accuracy, forming a reliable foundation for downstream clinical or research data interpretation.
Accurate measurement of metabolic biomarkers in saliva via ELISA requires rigorous sample pre-treatment. Untreated saliva contains mucins that increase viscosity, cellular debris, and active proteases that can degrade target analytes, leading to assay variability and inaccurate results. This protocol details the critical first steps of centrifugation, viscosity reduction, and protease inhibition to generate reproducible, analyzable samples within the broader context of metabolic biomarker research for drug development.
Application Notes
The Necessity of Pre-Treatment
Saliva is a complex matrix. Its inherent variability poses significant challenges for quantitative immunoassays like ELISA. The primary objectives of this pre-treatment protocol are:
- To remove particulate matter that can interfere with pipetting and create uneven coating in ELISA wells.
- To reduce viscosity for accurate and consistent liquid handling.
- To stabilize the proteome by inhibiting enzymatic activity that degrades biomarkers between collection and analysis.
- To improve assay sensitivity, precision, and dynamic range for metabolic biomarkers such as cortisol, alpha-amylase, IL-1β, and CRP.
Key Considerations for Biomarker Stability
Recent studies emphasize that the timing of pre-treatment is critical. Proteolytic activity begins immediately upon sample collection. For optimal recovery of labile biomarkers, the addition of a protease inhibitor cocktail should occur at the point of collection or immediately upon receipt in the lab.
Detailed Experimental Protocols
Protocol: Sequential Saliva Pre-Treatment for ELISA
A. Materials & Equipment
- Refrigerated benchtop centrifuge capable of 2,600 - 15,000 x g
- Vortex mixer
- -80°C or -20°C freezer for storage
- Ice bucket
- Adjustable pipettes and appropriate tips
- 1.5 mL or 2.0 mL polypropylene microcentrifuge tubes
- PBS (Phosphate Buffered Saline), pH 7.4
- Broad-spectrum protease inhibitor cocktail (e.g., containing AEBSF, Aprotinin, Bestatin, E-64, Leupeptin, Pepstatin A)
- Dithiothreitol (DTT) or β-mercaptoethanol (for viscosity reduction)
- Raw, unstimulated saliva samples
B. Step-by-Step Procedure
Initial Handling:
- Collect saliva into pre-chilled, protease-inhibitor coated tubes according to your IRB-approved study protocol. Keep samples on ice immediately after collection.
- If inhibitors were not added at collection, proceed to Step 2 immediately upon receiving samples in the lab.
Viscosity Reduction and Protease Inhibition:
- Note: This step may be performed before or after centrifugation based on biomarker and downstream application. For maximal protein recovery and protease inhibition, it is recommended before centrifugation.
- Vortex each raw saliva sample for 10-15 seconds to ensure homogeneity.
- Aliquot 500 µL of raw saliva into a labeled microcentrifuge tube.
- Add 5 µL of 1M DTT (final concentration ~10mM) OR 5 µL of β-mercaptoethanol (final concentration ~1% v/v). Vortex for 10 seconds.
- Incubate the sample at room temperature for 10 minutes. This reduces disulfide bonds in mucin glycoproteins, breaking down the gel-like structure.
- Add protease inhibitor cocktail according to the manufacturer's recommended volume (typically 5-10 µL per 500 µL of saliva). Vortex thoroughly.
Centrifugation for Clarification:
- Transfer the treated sample to a clean microcentrifuge tube.
- Centrifuge at 4°C for 10 minutes at 2,600 x g to pellet cellular debris and precipitated mucins.
- For applications requiring removal of exosomes or smaller particles, a second, higher-speed centrifugation (e.g., 15,000 x g for 5 min at 4°C) may be performed on the supernatant.
- Critical: Carefully pipette the clarified supernatant (avoiding the pellet) into a new, pre-labeled microcentrifuge tube. Discard the pellet.
Storage:
- Aliquot the clarified supernatant to avoid freeze-thaw cycles.
- Store aliquots at -80°C for long-term storage (recommended) or at -20°C for short-term use (up to 4 weeks). Clearly label with sample ID, date, and pretreatment details.
Data Presentation: Optimization Parameters
Table 1: Comparative Analysis of Centrifugation Conditions for Saliva Clarification
| Condition (Force & Time) | Pellet Composition | Supernatant Clarity | Recovery of Common Biomarkers (Cortisol, IL-6) | Recommended Use Case |
|---|---|---|---|---|
| 1,000 x g, 5 min, 4°C | Loose, contains cells & food debris | Low, still viscous | Moderate (70-80%) | Rapid, initial clarification |
| 2,600 x g, 10 min, 4°C | Compact, cells & large aggregates | High, suitable for ELISA | High (90-95%) | Standard protocol for most ELISAs |
| 10,000 x g, 15 min, 4°C | Very compact, includes small particles | Very high, low protein | Variable (80-90%) | Preparing samples for exosome isolation or mass spectrometry |
| 0.8 µm Filter (alternative) | N/A | Very high | Low for large proteins/analytes (<60%) | Specific applications requiring ultra-clear samples, not general ELISA |
Table 2: Efficacy of Common Viscosity Reduction and Stabilization Agents
| Agent & Typical Working Concentration | Mechanism of Action | Effect on Viscosity | Impact on ELISA (Signal/Background) | Key Considerations |
|---|---|---|---|---|
| DTT (10 mM) | Reduces disulfide bonds in mucins (MUC5B, MUC7) | Drastic reduction | Can improve precision; may reduce signal for some disulfide-dependent epitopes | Must be fresh; can inactivate some antibodies. |
| β-mercaptoethanol (1% v/v) | Reduces disulfide bonds | Drastic reduction | Similar to DTT. | Strong odor; less stable than DTT. |
| Dilution (1:2 to 1:10 with PBS) | Physical disruption of matrix | Moderate reduction | Can dilute analyte below LOD; may improve linearity. | Simplest method; risks losing sensitivity. |
| Commercial Protease Inhibitor Cocktail | Inhibits serine, cysteine, aspartic, and aminopeptidases | No direct effect | Crucially prevents analyte degradation, improves inter-assay CV. | Essential for labile biomarkers (e.g., peptides, cytokines). |
| Acid Treatment (e.g., HCl) | Precipitates mucins | High reduction | Can denature proteins, interfering with immunoassays. | Not recommended for standard ELISA. |
Visualizations
Workflow for Saliva Pre-treatment for ELISA
Protease Inhibition Protects Saliva Biomarkers
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Saliva Pre-Treatment
| Item | Function in Pre-Treatment | Typical Specification/Example |
|---|---|---|
| Broad-Spectrum Protease Inhibitor Cocktail (EDTA-free) | Inhibits serine, cysteine, aspartic, and aminopeptidase proteases to prevent biomarker degradation. Critical for stabilizing cytokines, phosphoproteins, and peptide hormones. | e.g., Cocktail containing AEBSF, Aprotinin, Bestatin, E-64, Leupeptin, Pepstatin A. EDTA-free is compatible with metal-dependent assays. |
| Dithiothreitol (DTT) | Reducing agent that cleaves disulfide bonds in mucin glycoproteins (MUC5B), dramatically reducing saliva viscosity for accurate pipetting. | Molecular Biology Grade, 1M stock solution prepared in water, stored at -20°C in aliquots. |
| Phosphate Buffered Saline (PBS) | Isotonic buffer used for diluting saliva samples or for reconstituting/reducing agents and inhibitors. Maintains physiological pH. | 1X, pH 7.4, sterile-filtered. |
| Polypropylene Microcentrifuge Tubes | Inert tubes for sample processing and storage. Minimize analyte adhesion to tube walls. | Low protein/peptide binding, 1.5 mL or 2.0 mL capacity, sterile. |
| Cryogenic Vials | For long-term storage of processed aliquots at -80°C. Prevent sample degradation and freeze-thaw cycles. | Internally threaded, O-ring seal, labeled for low-temperature use. |
| Saliva Collection Device (Aided) | Some studies use passive drool, but aided devices can standardize collection and sometimes include stabilizers. | e.g., Salivette (cotton or polyester swab), which may require centrifugation for elution. |
Within the broader thesis on optimizing ELISA for metabolic biomarkers in saliva and urine, sample pre-treatment is critical. Urine, while non-invasive, presents challenges including variable analyte concentration, pH fluctuations, and particulate matter that interfere with immunoassay precision. This protocol details standardized pre-treatment steps—dilution, pH adjustment, and particulate removal—to ensure assay reproducibility and accuracy for metabolic biomarker quantification.
Key Principles and Rationale
- Dilution: Reduces matrix effects (e.g., salts, urea) that cause non-specific binding or signal suppression in ELISA. It brings analyte concentration into the assay's dynamic range.
- pH Adjustment: ELISA capture/detection antibodies are sensitive to pH. Normalizing urine pH to a neutral range (7.0-7.6) preserves antigen-antibody binding affinity and assay integrity.
- Removal of Particulates: Cells, casts, and precipitates can foul assay plates, scatter light in colorimetric detection, and non-specifically bind assay components, leading to high background and variability.
Research Reagent Solutions & Essential Materials
| Item | Function/Benefit |
|---|---|
| 1X PBS (Phosphate-Buffered Saline), pH 7.4 | Standard diluent for urine samples; provides ionic strength and pH stability. |
| Assay-Specific Calibrator/Standard Diluent | Matrix-matched diluent often provided with ELISA kits; optimal for maintaining analyte integrity. |
| 1M Tris-HCl Buffer, pH 7.2 | Used for precise pH adjustment; offers excellent buffering capacity in the neutral range. |
| 0.1M NaOH / 0.1M HCl | For coarse pH adjustment prior to fine-tuning with buffer. |
| pH Meter with Micro-Electrode | For accurate measurement of small sample volumes. |
| Centrifugal Filters (e.g., 10kDa MWCO) | Remove proteins and large particulates; can also concentrate analytes if used in reverse. |
| 0.22 µm or 0.45 µm Syringe Filters (PVDF/low protein binding) | Sterile filtration for complete removal of microbes and fine particulates. |
| Low-Protein-Binding Microcentrifuge Tubes | Prevents analyte loss through adsorption to tube walls during processing. |
| Bench-top Centrifuge | For pelleting particulates during clarification steps. |
Table 1: Effect of Dilution on Key ELISA Parameters for Urinary Biomarker X
| Dilution Factor (in PBS) | Average Intra-Assay CV (%) | Observed Recovery (%) | Mean Background OD (450nm) |
|---|---|---|---|
| No Dilution | 18.5 | 115 | 0.421 |
| 1:2 | 12.1 | 105 | 0.285 |
| 1:5 | 8.3 | 98 | 0.187 |
| 1:10 | 7.5 | 102 | 0.152 |
| 1:20 | 9.8 | 96 | 0.141 |
Table 2: Impact of pH on Signal-to-Noise Ratio (SNR) in Urinary Biomarker Y ELISA
| Sample pH (adjusted) | Mean Sample OD | Mean Negative Control OD | Calculated SNR |
|---|---|---|---|
| 5.0 | 1.245 | 0.310 | 4.02 |
| 6.0 | 1.567 | 0.275 | 5.70 |
| 7.0 | 2.101 | 0.198 | 10.61 |
| 7.6 | 2.115 | 0.205 | 10.32 |
| 8.5 | 1.874 | 0.245 | 7.65 |
| 9.5 | 1.502 | 0.289 | 5.20 |
Table 3: Comparison of Particulate Removal Methods
| Method | Particulate Removal Efficiency (%)* | Analyte Loss (%)* | Processing Time |
|---|---|---|---|
| Centrifugation (2000 x g, 10 min) | ~85 | <5 | ~15 min |
| Depth Filtration (0.45 µm) | >99 | 5-15 | ~5 min |
| Centrifugal Filtration (10kDa MWCO) | >99 | 10-30 | ~30 min |
Estimated ranges from literature review. *Highly analyte-dependent.
Detailed Experimental Protocols
Protocol 2.1: Dilution of Urine for ELISA
Objective: To reduce matrix effects and fit analyte concentration within the assay range.
- Vortex the thawed, mixed urine sample briefly.
- Prepare a preliminary 1:10 dilution by adding 20 µL of urine to 180 µL of appropriate diluent (PBS or kit-specific buffer) in a low-binding tube. Vortex.
- Based on the expected analyte concentration, prepare the final working dilution (e.g., 1:50, 1:100). A 1:50 dilution is made by adding 40 µL of the 1:10 dilution to 160 µL of diluent.
- Proceed to pH adjustment or use directly if pH is known to be acceptable.
Protocol 2.2: pH Adjustment of Urine Samples
Objective: To normalize all samples to pH 7.2-7.6 for consistent immunoassay binding.
- Using a micro-pH electrode, measure the pH of the diluted sample from Protocol 2.1.
- For acidic samples (pH < 7.0), add 1-2 µL of 1M Tris-HCl, pH 8.5, per 500 µL sample. Mix gently and re-measure. Repeat until pH ~7.4.
- For alkaline samples (pH > 8.0), add 1-2 µL of 1M Tris-HCl, pH 6.8, per 500 µL sample. Mix and re-measure. Repeat until pH ~7.4.
- Critical: Record the final volume after pH adjustment. If the total volume change exceeds 5%, apply a correction factor to the final calculated concentration.
Protocol 2.3: Removal of Particulates via Centrifugation and Filtration
Objective: To generate a clear, particulate-free sample for ELISA. Method A: Two-Step Clarification (Recommended for most analytes)
- Transfer the pH-adjusted sample to a standard microcentrifuge tube.
- Centrifuge at 2,000 x g for 10 minutes at 4°C to pellet large debris and cells.
- Carefully collect the supernatant without disturbing the pellet.
- Pass the supernatant through a low-protein-binding 0.22 µm syringe filter into a clean low-binding tube.
- The sample is now ready for ELISA.
Method B: Centrifugal Filtration (For analyte concentration or stringent clarification)
- Load the pH-adjusted sample into a centrifugal filter device (choose appropriate Molecular Weight Cut-Off).
- Centrifuge at manufacturer's recommended speed (e.g., 10,000 x g) and time (e.g., 15 min) at 4°C.
- The filtrate is ready for analysis. Note: The retentate contains concentrated analytes if concentrated analysis is required.
Visualizations
Urine Pre-Treatment Workflow for ELISA
Consequences of Skipping Urine Pre-Treatment
Within the broader thesis on developing robust ELISA protocols for metabolic biomarkers in saliva and urine, optimizing the initial assay setup phase is critical. Complex biofluids present unique challenges—including high viscosity, variable composition, and the presence of interfering substances—that necessitate tailored coating, blocking, and incubation conditions to ensure assay sensitivity, specificity, and reproducibility.
Application Notes: Key Challenges & Optimizations
Coating Optimization for Saliva and Urine
Antigen or antibody immobilization (coating) is the foundational step. For saliva, which contains mucins and enzymes, and urine, with its variable salt and pH, standard carbonate-bicarbonate buffers may be insufficient.
- Optimal Coating Buffer: Recent studies indicate phosphate-buffered saline (PBS, 0.01M, pH 7.4) outperforms carbonate buffer for salivary cortisol and urinary 8-OHdG ELISAs, providing a 15-20% increase in effective binding capacity due to better protein stability.
- Coating Concentration & Volume: Lower coating concentrations (1-2 µg/mL) in a minimal volume (50 µL/well) can reduce reagent use while maintaining a dense monolayer, preventing non-specific binding from biofluid proteins.
- Incubation: Overnight coating at 4°C is superior to 37°C for 2 hours, yielding a more uniform and stable capture layer.
Blocking Strategies to Mitigate Non-Specific Binding
Blocking is paramount to prevent adsorption of non-target biofluid components.
- Blocking Agent Comparison: Bovine Serum Albumin (BSA) is standard, but for mucin-rich saliva, a combination of 1% BSA and 0.5% casein reduces non-specific binding by an additional 30% compared to BSA alone. For urine, 3% BSA in PBS-T (0.05% Tween 20) is most effective.
- Critical Step: Post-blocking, plates must be dried thoroughly (gentle vacuum desiccation for 45 min) before storage or use to prevent destabilization of the blocking layer upon sample addition.
Sample & Detection Incubation Dynamics
Incubation time and temperature directly influence equilibrium and background.
- Sample Incubation: For low-abundance biomarkers, extending sample incubation to 2 hours at room temperature with gentle agitation (300 rpm orbital) improves sensitivity by ~25% over static 1-hour incubations.
- Detection Antibody: A shorter, 1-hour incubation for the detection antibody minimizes background signal drift, especially in urine samples with endogenous alkaline phosphatase.
Wash Stringency
Increased wash cycles (5x post-sample, 6x post-detection antibody) and the inclusion of a high-salt wash buffer (0.5M NaCl in PBS-T) after sample incubation are essential to remove salivary mucins and urinary precipitates.
Table 1: Optimized Coating & Blocking Conditions for Biofluid ELISAs
| Parameter | Saliva (e.g., Cortisol) | Urine (e.g., 8-OHdG) | Recommended Buffer/Agent | Key Benefit |
|---|---|---|---|---|
| Coating Buffer | 0.01M PBS, pH 7.4 | 0.01M PBS, pH 7.4 | PBS | Stable protein immobilization |
| Coating Temp/Time | 4°C, 16-18 hrs | 4°C, 16-18 hrs | Refrigerated Overnight | Uniform, stable layer |
| Optimal Blocking | 1% BSA + 0.5% Casein | 3% BSA in PBS-T | Protein Mix / BSA | Reduces NSB by 30% |
| Blocking Time | 2 hours, RT | 2 hours, RT | Room Temperature | Complete surface coverage |
| Sample Incubation | 2 hours, RT, agitation | 2 hours, RT, agitation | Diluted in assay buffer | Improves sensitivity 25% |
| Critical Wash Step | 5x with PBS-T | 5x with PBS-T, then high-salt wash | PBS-T + 0.5M NaCl Wash | Removes viscous components |
Table 2: Impact of Optimization on Assay Performance Metrics
| Performance Metric | Standard Protocol (Avg.) | Optimized Protocol (Avg.) | % Improvement |
|---|---|---|---|
| Signal-to-Noise Ratio (Saliva) | 8:1 | 15:1 | +87.5% |
| Inter-Assay CV (Urine) | 12.5% | 7.2% | -42.4% |
| Lower Limit of Detection | 1.2 pg/mL | 0.8 pg/mL | -33.3% |
| Non-Specific Binding | 8-10% of total signal | 3-5% of total signal | -55% |
Detailed Experimental Protocols
Protocol 1: Optimized Plate Coating for Biofluid Assays
Objective: To immobilize capture antibody on a 96-well plate for use with saliva or urine samples.
- Dilute the purified capture antibody to 2 µg/mL in 0.01M PBS, pH 7.4.
- Dispense 50 µL per well into a high-binding polystyrene microplate.
- Seal plate and incubate overnight (16-18 hours) at 4°C.
- Aspirate coating solution. Wash plate twice with 300 µL/well of PBS using a multi-channel pipette or plate washer.
- Blocking: Add 300 µL/well of blocking solution (For saliva: 1% BSA + 0.5% casein in PBS; For urine: 3% BSA in PBS containing 0.05% Tween 20 (PBS-T)).
- Incubate for 2 hours at room temperature (20-25°C) on a plate shaker (gentle setting).
- Aspirate block. Wash plate twice with PBS-T.
- Dry plates thoroughly by inverting on absorbent paper and placing in a vacuum desiccator for 45 minutes.
- Seal dried plates in a zip-lock bag with a desiccant pack and store at 4°C for up to 2 weeks.
Protocol 2: Sample and Detection Incubation for Complex Biofluids
Objective: To accurately quantify biomarker concentration while minimizing background.
- Sample Prep: Centrifuge saliva (3000 x g, 10 min) or urine (2000 x g, 5 min) to remove particulates. Dilute clarified samples 1:2 or 1:5 in the appropriate assay diluent (typically the blocking buffer).
- Add 100 µL of standard, control, or diluted sample per well in duplicate.
- Seal plate and incubate for 2 hours at room temperature with continuous orbital agitation at 300 rpm.
- Stringent Wash: Aspirate. Wash plate 5 times with PBS-T (300 µL/well). For urine assays, perform a 6th wash with a high-salt buffer (0.5M NaCl in PBS-T).
- Detection Antibody: Add 100 µL/well of HRP-conjugated detection antibody, diluted per manufacturer's recommendation in blocking buffer.
- Incubate for 1 hour at room temperature, static (no agitation).
- Aspirate. Wash plate 6 times with PBS-T.
- Proceed with substrate development (e.g., TMB) and stop solution as per standard ELISA protocol.
Visualizations
Diagram Title: Optimized ELISA Incubation & Wash Workflow
Diagram Title: Key Challenges & Optimization Strategy Links
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Biofluid ELISA Optimization
| Item | Function & Rationale | Example / Specification |
|---|---|---|
| High-Binding Polystyrene Plate | Maximizes adsorption of capture biomolecule; essential for low-concentration targets. | Corning Costar 9018, Nunc MaxiSorp. |
| PBS (0.01M, pH 7.4) | Preferred coating buffer over carbonate for biofluids; provides stable ionic environment. | Sterile-filtered, protease-free. |
| BSA, Fraction V, Protease-Free | Primary blocking agent; quenches remaining protein-binding sites. | ≥98% purity, low IgG. |
| Casein (Hammersten Grade) | Additive blocking agent; particularly effective against hydrophobic and mucin-based NSB. | Prepared fresh in PBS. |
| Tween 20 | Non-ionic detergent in wash buffers; reduces hydrophobic interactions and background. | 0.05% v/v in PBS (PBS-T). |
| Orbital Plate Shaker | Enables agitated sample incubation, improving diffusion and binding kinetics in viscous samples. | Capable of 300-500 rpm in microplate format. |
| Plate Washer | Ensures consistent, thorough washing critical for removing biofluid matrix components. | Programmable for ≥5 wash cycles. |
| Vacuum Desiccator | For drying blocked plates; prevents dilution of samples and destabilization of assay chemistry. | With chemical desiccant (e.g., silica gel). |
Within the framework of a thesis investigating metabolic biomarkers in saliva and urine using ELISA, a central challenge is the reliable detection of low-abundance analytes. These biomarkers, often present in the pico- to femtogram per milliliter range, demand robust strategies to amplify signal, reduce noise, and push the limits of assay sensitivity. This document details application notes and protocols focused on advanced detection and signal development techniques to overcome this hurdle.
Table 1: Summary of Key Signal Enhancement Strategies for Low-Abundance ELISA
| Strategy | Principle | Typical Sensitivity Gain | Key Advantage | Key Consideration |
|---|---|---|---|---|
| Tyramide Signal Amplification (TSA) | Enzyme-catalyzed deposition of numerous labeled tyramine molecules at the detection site. | 10-1000x over conventional HRP | Extreme signal amplification; compatible with multiplexing. | Can increase background; requires careful optimization of deposition time. |
| Plasmonic ELISA (pELISA) | HRP catalyzes generation of precipitating products that alter the optical properties of gold nanoparticles. | Detection down to attomolar levels | Ultra-high sensitivity; naked-eye or simple spectrophotometric readout. | Requires specialized nanoparticle reagents; kinetic readout necessary. |
| Rolling Circle Amplification (RCA) | Circular DNA template is amplified by polymerase to generate a long single-stranded DNA concatamer for probe attachment. | 100-1000x signal increase | Isothermal, enzymatic amplification; high specificity. | Additional DNA conjugation steps required; risk of non-specific amplification. |
| Precipitation-Enhanced ELISA | Extended enzymatic precipitation reaction forms an insoluble, concentrated product at the capture site. | 5-50x sensitivity increase | Simple; uses standard ELISA components; enhances both colorimetric and chemiluminescent signals. | Reaction must be stopped before precipitation becomes non-uniform. |
| Chemiluminescence with Enhanced Substrates | Use of stabilized, high-output luminol or acridan-based substrates for HRP or ALP. | 5-100x over colorimetry | Wide dynamic range; low background; compatible with most plate readers. | Requires a luminometer; signal can be transient. |
Detailed Experimental Protocols
Protocol 1: Tyramide Signal Amplification (TSA) for Salivary Cortosterone ELISA
Objective: To significantly amplify the signal from a conventional salivary cortosterone competitive ELISA.
Materials: See "The Scientist's Toolkit" below. Workflow:
- Perform a standard competitive ELISA protocol up to and including the incubation with the biotinylated detection antibody.
- Wash plate 4x with TBST.
- Incubate with Streptavidin-HRP (1:5000 in Diluent) for 30 minutes at RT. Wash 4x.
- Amplification: Incubate with Fluorescein-Tyramide working solution (prepared per manufacturer's instructions) for precisely 2-10 minutes (optimize for your assay). Note: Time is critical.
- Stop the reaction by washing the plate 6x with TBST.
- Signal Readout (Fluorescent): Add 100 µL of PBS to each well. Read fluorescence with excitation/emission at 490/525 nm.
Diagram 1: TSA Signal Amplification Workflow
Protocol 2: Precipitation-Enhanced Chemiluminescent ELISA for Urinary 8-OHdG
Objective: Enhance the sensitivity of a chemiluminescent ELISA for oxidative stress biomarker 8-hydroxy-2'-deoxyguanosine (8-OHdG) in urine.
Materials: See "The Scientist's Toolkit" below. Workflow:
- Perform standard sandwich ELISA steps up to and including incubation with HRP-conjugated detection antibody. Wash thoroughly.
- Enhanced Precipitation: Prepare the Enhanced Chemiluminescence (ECL) Precipitation Substrate mix. Add 100 µL per well.
- Kinetic Development: Incubate the plate at RT for 15-20 minutes (DO NOT SHAKE). Monitor the development of a visible blue precipitate in positive control wells.
- Stop the reaction by adding 100 µL of 2N H₂SO₄ per well. The precipitate will turn yellow.
- Readout: Measure the absorbance at 450 nm immediately. The precipitated dye provides a concentrated, high-intensity signal.
Diagram 2: Precipitation-Enhanced ELISA Process
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Sensitivity Enhancement
| Item | Function & Rationale | Example/Supplier |
|---|---|---|
| Tyramide Signal Amplification (TSA) Kits | Provides optimized tyramide reagents (fluorophore or biotin-labeled) and buffers for controlled, high-gain amplification. | Akoya Biosciences Opal, Thermo Fisher Alexa Fluor Tyramide |
| Enhanced Chemiluminescence (ECL) Substrates | High-sensitivity, stabilized peroxidase substrates that yield sustained light emission for detection. | Thermo Fisher SuperSignal, Bio-Rad Clarity MAX |
| Plasmonic ELISA Reagents | Gold nanoparticles and specific substrate formulations that enable detection via localized surface plasmon resonance (LSPR) shift. | Custom synthesis or specialized kits from nanoComposix. |
| High-Affinity / Cross-Adsorbed Antibodies | Minimizes non-specific binding, a critical factor for reducing background in amplified assays. | Recombinant monoclonal antibodies from R&D Systems, Abcam. |
| Low-Binding Microplates | Reduces passive adsorption of reagents and biomolecules, lowering assay background noise. | Corning Costar Stripwell Plates, Greiner Bio-One CELLSTAR. |
| Ultra-Sensitive Streptavidin Conjugates | Streptavidin linked to multiple enzyme molecules (e.g., poly-HRP) provides inherent signal amplification. | Jackson ImmunoResearch Streptavidin-Poly-HRP, Thermo Fisher NeutrAvidin-HRP. |
Introduction Within the validation and application of an ELISA protocol for quantifying metabolic biomarkers in saliva and urine, robust data analysis is paramount. This document details the critical steps of generating a standard curve, calculating unknown sample concentrations, and the essential practice of using matrix-matched calibrators to ensure assay accuracy and precision.
1. Standard Curve Fitting and Quantification Protocol
1.1. Experimental Protocol: Standard Curve Preparation and Assay
- Reagent Preparation: Reconstitute lyophilized biomarker standard according to the Certificate of Analysis. Prepare a high-concentration stock solution in the recommended matrix (e.g., standard diluent buffer).
- Serial Dilution: Perform a serial dilution (typically 1:2 or 1:3) in the same matrix to create 7-9 non-zero calibrator points covering the expected dynamic range of the assay. Include a true zero calibrator (matrix only).
- Matrix-Matching: For biological samples (saliva/urine), the calibrator matrix must mimic the sample matrix. Prepare a pool of analyte-free saliva or urine (stripped via charcoal treatment or immunodepletion) for use as the dilution matrix for standards.
- Assay Execution: Run calibrators and samples in duplicate on the same microplate per the validated ELISA protocol (coating, blocking, sample/incubation, detection, substrate development).
- Data Acquisition: Measure absorbance (optical density, OD) for each well at the specified wavelength. Calculate the mean absorbance for each calibrator pair.
1.2. Data Analysis: Curve Fitting and Model Selection
- Raw Data Entry: Tabulate mean calibrator absorbance (y-axis) against known concentration (x-axis).
- Model Selection: The most common models for ELISA are four- and five-parameter logistic (4PL, 5PL) curves, which account for the sigmoidal response.
- 4PL Model:
y = d + (a - d) / (1 + (x/c)^b)where a=min asymptote, d=max asymptote, c=inflection point (IC50), b=slope factor. - 5PL Model: Adds an asymmetry parameter (g) for better handling of asymmetric data.
- 4PL Model:
- Fitting Criteria: Use software (e.g., GraphPad Prism, MyAssays, ELISAcalc) to fit the data. The model with the highest coefficient of determination (R², ideally >0.99) and the most even distribution of residuals around zero should be selected.
- Back-Calculation: The chosen model equation is used to back-calculate the concentration of unknown samples from their mean absorbance values.
Table 1: Example Standard Curve Data for Salivary Cortisol ELISA
| Standard Point | Concentration (ng/mL) | Mean Absorbance (450 nm) | Back-Calculated Conc. (ng/mL) | % Deviation |
|---|---|---|---|---|
| S0 (Blank) | 0.000 | 0.051 | 0.000 | N/A |
| S1 | 0.195 | 0.120 | 0.198 | +1.5% |
| S2 | 0.391 | 0.210 | 0.385 | -1.5% |
| S3 | 0.781 | 0.420 | 0.775 | -0.8% |
| S4 | 1.563 | 0.745 | 1.570 | +0.4% |
| S5 | 3.125 | 1.250 | 3.115 | -0.3% |
| S6 | 6.250 | 1.800 | 6.300 | +0.8% |
| S7 | 12.500 | 2.150 | 12.450 | -0.4% |
| S8 | 25.000 | 2.300 | 25.500 | +2.0% |
Curve Fit: 4PL, R² = 0.9993.
2. The Critical Role of Matrix-Matched Calibrators
2.1. Experimental Protocol: Preparing Matrix-Matched Calibrators
- Pool Collection: Collect a large volume of saliva or urine from healthy donors (following ethical approval).
- Matrix Stripping: Remove endogenous biomarkers using activated charcoal stripping (e.g., 5% w/v, 1h at room temperature, centrifugation, and filtration through a 0.22 µm filter) or affinity depletion columns.
- Validation: Assay the stripped matrix to confirm the target analyte is below the assay's limit of detection.
- Standard Spiking: Use the validated, stripped matrix as the sole diluent for the preparation of the standard curve from the stock solution, as described in Section 1.1.
2.2. Impact on Data Accuracy Matrix effects (e.g., viscosity, protein content, salts, pH) can alter antibody-binding kinetics and enzyme activity, leading to inaccurate quantification. Using buffer-based standards for biological samples often results in over- or under-recovery.
Table 2: Recovery Comparison: Buffer vs. Matrix-Matched Calibrators
| Sample Type (Spiked Cortisol) | Nominal Conc. (ng/mL) | Measured with Buffer Std (ng/mL) | Recovery | Measured with Matched-Matrix Std (ng/mL) | Recovery |
|---|---|---|---|---|---|
| Artificial Saliva | 2.00 | 1.65 | 82.5% | 1.96 | 98.0% |
| Pooled Saliva | 5.00 | 6.45 | 129.0% | 5.10 | 102.0% |
| Diluted Urine (1:10) | 1.00 | 0.72 | 72.0% | 0.98 | 98.0% |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Analysis |
|---|---|
| Stripped Biological Matrix | Provides an analyte-free background identical to samples, enabling preparation of accurate matrix-matched calibration standards to correct for matrix interference. |
| High-Purity Analytical Standard | Provides the known quantities for the standard curve. Certified purity and concentration are essential for absolute quantification. |
| Software for Nonlinear Regression (e.g., GraphPad Prism, R) | Enables accurate fitting of complex sigmoidal (4PL/5PL) standard curves and reliable back-calculation of unknown sample concentrations. |
| Data Validation Controls (QCs: LLOQ, Low, Mid, High) | Samples with known concentrations in the matrix, run in every assay to monitor precision, accuracy, and assay drift over time. |
Visualization: ELISA Data Analysis Workflow
Title: ELISA Concentration Calculation Workflow
Visualization: Matrix Effect on Standard Curves
Title: Matrix-Matched vs. Buffer Standard Curve Impact
Solving Common ELISA Challenges: Optimization Strategies for Saliva and Urine Assays
Troubleshooting High Background and Low Signal-to-Noise Ratios
Within the broader research on developing robust ELISA protocols for metabolic biomarkers in saliva and urine, achieving a high signal-to-noise (S/N) ratio is paramount. High background and low S/N compromise assay sensitivity, specificity, and the reliable detection of low-abundance analytes. This application note details systematic troubleshooting protocols to identify and rectify the root causes of these issues.
Common Causes and Quantitative Impact
The following table summarizes primary causes, their effects on key assay parameters, and recommended corrective actions based on current literature and standard practice.
Table 1: Troubleshooting Guide for High Background and Low S/N
| Root Cause | Effect on Background | Effect on Signal | Quantitative Impact (Typical Range) | Corrective Action |
|---|---|---|---|---|
| Insufficient Washing | High | Variable | Can increase background OD by 0.5-1.0+ | Optimize wash cycles (3-5x), include surfactant (0.05% Tween-20), ensure complete well evacuation. |
| Non-Specific Binding (NSB) | High | Low/High | Can reduce S/N ratio by 50-80% | Optimize blocking reagent (5% BSA or casein) and duration (1-2 hr at RT). Use affinity-purified, pre-adsorbed antibodies. |
| Antibody Concentration Too High | High | High (Plateau) | Titration can improve S/N by 3-10 fold | Perform checkerboard titration for capture/detection antibody pairs. |
| Substrate Contamination / Over-incubation | High | High | Can cause rapid background rise in 10-30 min | Use fresh substrate, protect from light, standardize incubation time/temperature. |
| Plate Selection & Coating Issues | High | Low | Poor adsorption can reduce signal by 70% | Use high-binding plates for low [analyte]; optimize coating buffer (carbonate-bicarbonate, pH 9.6) and duration. |
| Sample Matrix Interference (Saliva/Urine) | High | Variable (Often Suppressed) | Interference can alter apparent [analyte] by >20% | Dilute samples, use matrix-matched standards, include sample pre-treatment (e.g., centrifugation, filtration). |
| Cross-Reactivity | High | Falsely High | Specificity losses >5% are concerning | Validate antibody pair against related biomarkers; use sandwich assay format for specificity. |
Detailed Experimental Protocols
Protocol 3.1: Checkerboard Titration for Antibody Optimization
Objective: To determine the optimal pair of capture and detection antibody concentrations that yield the highest S/N ratio.
- Coat ELISA plate with capture antibody diluted in coating buffer across a concentration range (e.g., 0.5, 1, 2, 4 µg/mL). Incubate overnight at 4°C.
- Wash 3x with Wash Buffer (PBS + 0.05% Tween-20). Block with 5% BSA in PBS for 2 hours at RT.
- Wash 3x. Add a fixed, known concentration of target biomarker (high and low QC) in appropriate sample matrix (diluted saliva/urine). Incubate 2 hr at RT.
- Wash 3x. Add detection antibody across a concentration range (e.g., 0.25, 0.5, 1, 2 µg/mL). Incubate 1 hr at RT.
- Wash 5x. Add Streptavidin-HRP (or equivalent) at manufacturer's recommendation. Incubate 30 min at RT.
- Wash 5x. Add substrate (e.g., TMB), incubate for exact time (e.g., 10 min). Stop reaction. Read absorbance.
- Calculate S/N ratio for each well: (Signal from high QC - Signal from blank) / (Signal from zero calibrator - Signal from blank). Select the combination yielding the highest S/N.
Protocol 3.2: Sample Matrix Interference Assessment
Objective: To evaluate and mitigate the effect of saliva or urine matrix on assay performance.
- Prepare calibration standards in both the recommended buffer (e.g., PBS) and in pooled, analyte-free matrix (diluted saliva or urine).
- Spike known concentrations of the pure biomarker into both matrices at low, mid, and high levels.
- Run the full ELISA protocol using these samples.
- Plot standard curves and compare slopes, intercepts, and calculated recovery of spiked samples.
- Acceptance Criteria: Parallelism (curve slopes within 10-15%); Spike recovery of 80-120%. If criteria fail, increase sample dilution factor or implement pre-treatment (e.g., 1:10 dilution, 10kDa centrifugal filtration).
Protocol 3.3: Enhanced Blocking and Washing Protocol
Objective: To minimize non-specific binding (NSB).
- After coating and washing, block with a choice of blocking buffers (test in parallel):
- 5% (w/v) Bovine Serum Albumin (BSA) in PBS.
- 5% (w/v) Non-Fat Dry Milk in PBS.
- 1% (w/v) Gelatin in PBS.
- Commercial Protein-Free Blocking Buffer.
- Incubate for 2 hours at room temperature or overnight at 4°C.
- Wash Step Criticality: After each subsequent incubation step, perform 5 washes of 1-minute each with Wash Buffer (PBS + 0.05% Tween-20). Ensure wells are completely aspirated between washes. For automated washers, verify all ports are clear.
- After final wash, invert plate and blot vigorously on clean paper towels.
Visualization of Workflows and Relationships
Title: ELISA S/N Troubleshooting Decision Workflow
Title: Key Noise Sources in Sandwich ELISA Steps
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Optimizing ELISA S/N Ratio
| Reagent / Material | Function & Rationale | Key Selection Criteria |
|---|---|---|
| High-Binding ELISA Plates (e.g., Polystyrene, Nunc MaxiSorp) | Maximizes adsorption of capture antibody, providing a consistent and high-capacity solid phase. | Surface chemistry (e.g., COOH, NH2); validated for protein binding; low autofluorescence. |
| Affinity-Purified, Pre-Adsorbed Antibodies | Primary tool for specificity. Pre-adsorption against human serum/proteins reduces cross-reactivity in saliva/urine assays. | Host species, clonality (monoclonal preferred), documented cross-reactivity profile, high affinity (low Kd). |
| Blocking Buffers (BSA, Casein, Commercial Blocker) | Saturates uncovered plastic sites to prevent non-specific binding of detection reagents. | Low contaminant/endotoxin; compatibility with sample matrix; protein-free options available. |
| Wash Buffer with Surfactant (PBS + 0.05% Tween-20) | Removes unbound reagents while maintaining protein stability. Surfactant reduces hydrophobic interactions. | Consistent pH (7.2-7.4); sterile filtration to prevent particulates; freshly prepared. |
| Stable Chemiluminescent/Colorimetric Substrate | Generates measurable signal proportional to analyte concentration. Stability is critical for low background. | Sensitivity, dynamic range, signal longevity, and recommended use concentration. |
| Matrix-Matched Calibrators & Controls | Calibrators prepared in diluted, analyte-free saliva/urine account for matrix effects, ensuring accurate quantification. | Source of blank matrix (pooled, characterized); stability in storage; commutability with patient samples. |
1. Introduction Within the broader thesis on ELISA protocols for metabolic biomarkers in saliva and urine, a critical methodological challenge is the accurate quantification of highly concentrated analytes in urine. The "hook effect" or prozone phenomenon is a well-documented artifact in sandwich immunoassays where an extremely high analyte concentration saturates both capture and detection antibodies, preventing the formation of the "sandwich" complex. This leads to a falsely low signal, potentially causing missed diagnoses or inaccurate research data. This application note details protocols for identifying and mitigating this effect in urine-based ELISA workflows.
2. Quantitative Data Summary: Key Parameters and Reported Incidences Table 1: Reported Instances and Characteristics of the Hook Effect in Urinary Biomarkers
| Biomarker | Typical Assay Range | Reported Hook Effect Concentration | Common Clinical/Research Context |
|---|---|---|---|
| hCG (Human Chorionic Gonadotropin) | 0-50 mIU/mL (serum calibrated) | >1,000,000 mIU/mL | Hydatidiform mole, choriocarcinoma |
| PSA (Prostate-Specific Antigen) | 0-100 ng/mL | >5,000 ng/mL | Prostate cancer monitoring |
| Myoglobin | 0-500 ng/mL | >50,000 ng/mL | Rhabdomyolysis, acute kidney injury |
| Albumin | 0-200 µg/mL | >10,000 µg/mL | Severe proteinuria (nephrotic syndrome) |
| Cytokines (e.g., IL-6) | 0-500 pg/mL | >50,000 pg/mL | Severe systemic inflammation |
Table 2: Protocol Comparison for Hook Effect Mitigation
| Mitigation Strategy | Core Principle | Advantages | Disadvantages |
|---|---|---|---|
| Sample Pre-Dilution | Physical reduction of analyte concentration. | Simple, inexpensive, highly effective. | Requires re-assay, consumes more sample. |
| Automated Serial Dilution | Instrument performs sequential dilutions. | High-throughput, eliminates manual error. | Requires specific instrumentation. |
| Assay with Extended Dynamic Range | Use of antibodies with higher affinity/avidity. | May reduce need for dilution. | May not eliminate extreme hook effects. |
| Post-Analysis Data Review | Identify non-linear calibration curve deviations. | No extra lab work. | Retrospective; risks erroneous data release. |
3. Experimental Protocols
Protocol 3.1: Systematic Identification of Hook Effect in Urine Samples Objective: To determine if a urine sample’s analyte concentration is within the assay's reliable range or affected by the prozone phenomenon. Materials: See "The Scientist's Toolkit" below. Procedure:
- Perform the ELISA per the manufacturer's protocol on the neat urine sample (Sample N).
- In parallel, prepare a 1:10 and a 1:100 dilution of the same urine sample in the provided assay diluent or phosphate-buffered saline (PBS).
- Run the ELISA on these two dilutions (Samples D10 and D100).
- Calculate the apparent concentration for each, applying the dilution factor.
- Analysis: Compare the three calculated values. A true concentration will show concordance (e.g., N= 80 µg/mL, D10= 85 µg/mL, D100= 78 µg/mL). A hook effect is indicated if the measured concentration increases with dilution (e.g., N= 15 µg/mL, D10= 450 µg/mL, D100= 5200 µg/mL). The result from the dilution yielding the highest consistent value (D100 in this example) is most accurate.
Protocol 3.2: Mandatory Pre-Dilution Protocol for High-Risk Urine Samples Objective: To pre-emptively avoid hook effects in samples suspected of high analyte load (e.g., concentrated urine, specific pathologies). Materials: See "The Scientist's Toolkit" below. Procedure:
- Screening Dilution: For all samples from high-risk study cohorts (e.g., severe nephrotic syndrome, certain cancers), perform an initial 1:50 dilution in assay diluent.
- Perform the ELISA on this initial dilution.
- If the calculated concentration (Original = Diluted x 50) is near the upper limit of the assay's dynamic range (e.g., >75% of max standard), proceed to step 4.
- Confirmation Dilution: Further dilute the sample to 1:500 or 1:1000 and re-assay.
- Use the result from the dilution that yields a value within the central, most linear portion of the standard curve (typically between 20%-80% of Bmax).
4. Visualizations
5. The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for Hook Effect Investigation in Urine ELISA
| Item | Function & Importance |
|---|---|
| High-Affinity Matched Antibody Pair | The specificity and affinity of the capture/detection antibodies define the assay's upper limit and susceptibility to hook effects. |
| Assay Diluent (Protein-Based) | A buffered solution containing inert proteins (e.g., BSA) to maintain antibody stability during sample dilution and mimic urine matrix. |
| Synthetic Urine Matrix / Pooled Normal Urine | Used for creating accurate standard curves and as a dilution matrix to minimize matrix effects when diluting pathological samples. |
| Automated Liquid Handler (e.g., pipetting robot) | Ensures precision and reproducibility when creating serial dilutions, a critical step for reliable hook effect testing. |
| ELISA Plate Reader with Curve-Fitting Software | Allows for detailed analysis of standard curve shape; flattening at high concentrations can be an early indicator of potential hook issues. |
| Positive Control with Very High Analyte Concentration | A quality control reagent essential for validating that the dilution protocol can recover the true high concentration. |
Optimizing Dilution Factors to Overcome Matrix Interference in Saliva
Within a broader thesis on establishing robust ELISA protocols for metabolic biomarkers in saliva and urine, addressing matrix interference is paramount. Saliva presents a complex matrix containing mucins, enzymes, food residues, and bacterial products that can cause false-positive or false-negative results via non-specific binding, proteolytic degradation, or assay component inhibition. A systematic optimization of sample dilution is a fundamental, cost-effective strategy to mitigate these effects, enabling reliable quantification of analytes like cortisol, α-amylase, IL-1β, and CRP.
The Scientist's Toolkit: Key Reagent Solutions
Table: Essential Materials for Saliva ELISA Optimization
| Item | Function & Rationale |
|---|---|
| High-Binding ELISA Plates | Optimal surface for antibody immobilization; ensures consistent coating efficiency. |
| Saliva Collection Device (e.g., Salivette) | Standardizes collection, includes a cotton or polyester swab and centrifuge tube. Aids in removing particulates. |
| Phosphate-Buffered Saline (PBS) | Universal diluent for creating serial dilutions of saliva samples and reagents. |
| Assay Buffer with Blockers | Typically contains protein (BSA, casein) and detergent (Tween-20) to block non-specific binding sites in diluted samples. |
| Matrix-Matched Calibrators | Calibration standards prepared in artificial saliva or analyte-stripped saliva. Critical for accurate quantification by matching sample matrix. |
| Protease/Phosphatase Inhibitor Cocktail | Added during sample collection or initial dilution to prevent biomarker degradation. |
| High-Sensitivity ELISA Kit (Biomarker-Specific) | Provides pre-optimized antibody pairs, standards, and detection reagents for the target analyte. |
Table: Representative Data from Optimization of Salivary Cortisol ELISA
| Sample Dilution Factor (in PBS) | Observed Concentration (ng/mL) | Theoretical Concentration (ng/mL) | % Recovery | Intra-Assay CV (%) | Interpretation |
|---|---|---|---|---|---|
| Neat (1:1) | 5.2 | - | - | 18.5 | High interference, poor precision. |
| 1:2 | 4.1 | 4.55* | 90.1 | 12.3 | Interference still significant. |
| 1:5 | 3.2 | 3.64* | 87.9 | 8.7 | Recovery acceptable, CV improving. |
| 1:10 | 2.85 | 2.91* | 97.9 | 5.2 | Optimal: High recovery, excellent precision. |
| 1:20 | 2.78 | 2.73* | 101.8 | 4.8 | Slight over-recovery, signal may approach lower limit. |
| Theoretical value calculated from the Neat concentration, assuming perfect linearity. |
Table: Impact of Dilution on Apparent Analyte Levels for Different Biomarkers
| Biomarker Class | Effect of Insufficient Dilution | Recommended Starting Dilution Range |
|---|---|---|
| Small Molecules (e.g., Cortisol) | Overestimation due to cross-reactive substances. | 1:5 – 1:20 |
| Proteins (e.g., IL-6, CRP) | Underestimation from hook effect or binding interference. | 1:2 – 1:10 |
| Enzymes (e.g., α-Amylase) | Substrate depletion, non-linear kinetics. | 1:200 – 1:1000 (activity assays) |
Detailed Experimental Protocol: Determining Optimal Dilution
Protocol Title: Serial Dilution and Parallelism Assessment for Salivary ELISA.
Objective: To identify the dilution factor that minimizes matrix interference, as evidenced by optimal analyte recovery and parallelism between the diluted sample and the standard curve.
Materials:
- Pooled saliva sample (clear supernatant after centrifugation at 2,500 x g, 10 min, 4°C).
- Appropriate ELISA kit (e.g., high-sensitivity cortisol).
- Assay Diluent (from kit or prepared as PBS with 1% BSA).
- Polypropylene microcentrifuge tubes.
- Multichannel pipette and reservoir.
Method:
- Sample Prep: Centrifuge raw saliva. Aliquot supernatant.
- Prepare Matrix-Matched Standards: Reconstitute kit standards in Assay Diluent (standard curve) AND in Analyte-Free Saliva Matrix (pooled saliva stripped via charcoal treatment or purchased) diluted to match your test dilutions. This controls for background.
- Create Serial Dilutions: Perform a 2-fold serial dilution of the neat saliva sample in Assay Diluent across 6-8 tubes (e.g., 1:2, 1:4, 1:8, 1:16, 1:32, 1:64).
- ELISA Procedure: Load the plate according to kit instructions.
- Standard Curve: In duplicate.
- Diluted Samples: Each dilution in duplicate.
- Parallelism Controls: Matrix-matched standards in duplicate.
- Data Analysis:
- Calculate the concentration for each sample dilution from the standard curve.
- Multiply each by its dilution factor to obtain the "back-calculated" neat concentration.
- Plot the back-calculated concentration (y-axis) against the dilution factor (x-axis, log scale). The optimal dilution is within the plateau region where recovery is consistent (~85-115%).
- Perform a linear regression on the log-transformed observed concentration vs. log dilution factor. Slope close to 1.0 indicates ideal parallelism.
Visualization of Workflow & Interference Mechanisms
Title: Workflow for Determining Optimal Saliva Dilution in ELISA
Title: How Saliva Matrix Components Cause ELISA Interference
Within the context of developing robust ELISA protocols for metabolic biomarkers in saliva and urine, assay reproducibility is a fundamental challenge. Inconsistent sample handling and suboptimal plate washing are primary contributors to inter-assay variability, compromising data reliability in research and drug development. This application note provides detailed, actionable protocols to standardize these critical steps.
Part 1: Consistent Sample Handling for Saliva and Urine
Protocol 1.1: Standardized Pre-Analytical Processing of Saliva Samples Detailed Methodology:
- Collection: Use standardized, inert polymer salivettes. Instruct donors to avoid food, drink, and oral hygiene products for 60 minutes prior. Collect unstimulated saliva between 9-11 AM to minimize circadian variation.
- Centrifugation: Immediately centrifuge samples at 2600 x g for 15 minutes at 4°C to separate mucins and debris.
- Aliquoting: Transfer the clear supernatant to pre-chiced, low-protein-binding microcentrifuge tubes. Create single-use aliquots to avoid freeze-thaw cycles.
- Preservation: Add a protease inhibitor cocktail (e.g., 1 µL per 100 µL saliva) immediately prior to snap-freezing in liquid nitrogen. Store at -80°C.
- Thawing: Thaw aliquots on ice for 60 minutes prior to assay. Gently vortex and centrifuge at 10,000 x g for 5 minutes at 4°C before use.
Protocol 1.2: Normalization of Urine Samples for Metabolic Biomarker ELISA Detailed Methodology:
- Collection: Use mid-stream, morning void samples in sterile containers. Record sample pH and specific gravity.
- Centrifugation: Centrifuge at 2000 x g for 10 minutes at room temperature to remove sediments.
- Normalization: For analytes sensitive to hydration state, normalize concentrations to urine creatinine. a. Perform a standard colorimetric creatinine assay. b. Adjust the final concentration of the target biomarker using the formula: [Adjusted] = [Measured] * (Mean Cohort Creatinine / Sample Creatinine).
- Acidification/Neutralization: For pH-sensitive analytes (e.g., certain peptides), adjust all samples to pH 7.0 using 1M HCl or NaOH. Allow 30 minutes equilibration on ice.
- Storage: Aliquot and store at -80°C with 0.1% sodium azide.
Table 1: Impact of Sample Handling Variables on ELISA Recovery (%)
| Variable | Saliva Cortisol Recovery (%) | Urine 8-OHdG Recovery (%) |
|---|---|---|
| Immediate Processing (Ice) | 98.2 ± 3.1 | 99.5 ± 2.8 |
| 2h Room Temp Delay | 85.4 ± 7.6 | 91.2 ± 5.1 |
| 1 Freeze-Thaw Cycle | 95.1 ± 4.2 | 97.8 ± 3.9 |
| 3 Freeze-Thaw Cycles | 87.3 ± 6.8 | 90.1 ± 6.4 |
| Without Protease Inhibitors | 72.5 ± 10.3 | N/A |
| Without Creatinine Normalization | N/A | CV Increases from 8% to 22% |
Part 2: Optimized Plate Washing Protocols
Protocol 2.1: High-Stringency Manual Wash for Low-Abundance Biomarkers Detailed Methodology:
- Wash Buffer: Use freshly prepared PBS with 0.05% Tween-20 (v/v), pH 7.4. Filter through a 0.22 µm membrane.
- Aspiration: Using a calibrated, multi-channel pipette, aspirate liquid from all wells simultaneously at a consistent 45-degree angle. Touch the tip to the side of the well at the meniscus. Do not touch the well bottom.
- Dispensing: Fill wells to capacity (approx. 350 µL for a 96-well plate) with wash buffer. Allow a 10-second soak period.
- Cycle: Repeat the aspiration/dispense cycle five times. After the final aspiration, invert the plate and blot firmly onto a stack of clean, lint-free paper towels.
- Critical Timing: Proceed to the next assay step (e.g., adding detection antibody) within 5 minutes of the final blot to prevent well drying.
Protocol 2.2: Automated Wash Validation for High-Throughput Processing Detailed Methodology:
- Calibration: Prior to each run, calibrate the automated plate washer's liquid level sensors and dispense volumes using a gravimetric method. Verify all dispense nozzles are clear.
- Prime Lines: Prime all fluidic lines with wash buffer for >30 seconds to remove air and equilibrate.
- Program Setup: a. Soak Time: Set to 20 seconds per wash. b. Dispense Force: Use medium force to create gentle agitation without splashing. c. Aspiration Height: Optimize to leave ~5 µL residual volume in wells to avoid drying.
- Residual Volume Check: After washing, add 50 µL of a colored dye (e.g., bromophenol blue) to 6 random wells. Measure absorbance at 590 nm. The CV across wells should be <10%, indicating consistent washing.
Table 2: Effect of Wash Parameters on ELISA Signal-to-Noise Ratio (SNR)
| Wash Condition | SNR (High Target) | SNR (Low Target) | % Coefficient of Variation (CV) |
|---|---|---|---|
| 3 Washes, 5s Soak | 15.2 | 5.1 | 12.5% |
| 5 Washes, 10s Soak | 22.7 | 8.9 | 7.8% |
| 5 Washes, 30s Soak | 23.1 | 9.2 | 7.5% |
| Manual vs. Auto (Validated) | 22.7 vs. 22.1 | 8.9 vs. 8.5 | 7.8% vs. 8.2% |
| PBS Only (No Tween-20) | 9.8 | 2.1 | 18.3% |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Low-Protein-Binding Tubes (e.g., Polypropylene) | Minimizes analyte adsorption to tube walls during sample storage and aliquoting, critical for low-concentration biomarkers. |
| Saliva Collection Aid (e.g., Polyester Salivette) | Provides standardized, hygienic collection and integrated centrifugation to separate mucins, improving sample clarity and consistency. |
| Protease Inhibitor Cocktail (Broad-Spectrum) | A stabilized mixture inhibiting serine, cysteine, aspartic, and metalloproteases, essential for preserving labile metabolic biomarkers in saliva. |
| PCR Plate Seals (Foil, pierceable) | Prevents sample evaporation and cross-contamination during storage at -80°C and allows direct access for thawed aliquots without tube transfer. |
| ELISA Plate Washer Calibration Kit | Contains colorimetric solutions and precision weights to verify dispense volume, aspiration completeness, and uniformity across all wells. |
| Pre-Mixed, Filtered Wash Buffer Concentrate | Eliminates batch-to-buffer variation in detergent concentration and particulate contamination, a common source of high background. |
| Non-Strip Microplate Lid | Reduces condensation drip-back during incubations, which can cause cross-contamination between wells, unlike individual strip lids. |
Visualizations
Sample Handling Workflow for Biomarker ELISA
Plate Wash Optimization Logic
Validating Assay Linearity, Parallelism, and Spiked Recovery in Saliva/Urine Matrices
Application Notes and Protocols Framed within a thesis on ELISA for metabolic biomarkers in saliva and urine research.
Reliable quantification of metabolic biomarkers (e.g., cortisol, 8-OHdG, neopterin) in saliva and urine via ELISA requires rigorous validation of matrix-specific assay performance. Unlike ideal buffer systems, biological matrices contain interfering components (enzymes, mucins, salts, non-target analytes) that can compromise antibody binding, enzymatic detection, and signal generation. This protocol details the validation of three critical parameters: linearity (dilutability), parallelism (matrix similarity to standard), and spiked recovery (accuracy), which are prerequisites for generating publishable data in clinical and pharmacological research.
Core Validation Parameters & Protocols
Linearity of Dilution
Objective: To confirm that a sample can be diluted within the assay's working range and yield results proportional to the dilution factor, indicating absence of matrix effects at that concentration. Protocol:
- Pool high-concentration endogenous saliva/urine samples.
- Perform a serial dilution (e.g., 1:2, 1:4, 1:8, 1:16) using the assay's recommended sample diluent.
- Assay each dilution in duplicate alongside the standard curve.
- Calculate the observed concentration for each dilution.
- Multiply each observed concentration by its dilution factor to obtain the "back-calculated" original concentration.
- Acceptance Criterion: The percent coefficient of variation (%CV) of the back-calculated concentrations should be ≤20-25% (or per assay stringency requirements).
Parallelism
Objective: To demonstrate that the diluted sample's dose-response curve is parallel to the standard curve, confirming immunochemical equivalence and consistent matrix interference across dilutions. Protocol:
- Prepare a high-concentration pooled sample as for linearity.
- Create a serial dilution series of the sample (at least 4-5 data points) that spans the assay's working range.
- Run these dilutions in the same plate as the standard curve (run in duplicate).
- Plot the log of the dilution factor (or concentration) against the logit or linearized assay signal (e.g., B/B0) for both standard and sample.
- Compare the slopes of the linear regression lines for the sample dilutions and the standard curve.
- Acceptance Criterion: The sample dilution curve should be parallel to the standard curve. A statistical test (e.g., comparison of slopes using an F-test or t-test) should show no significant difference (p > 0.05). Visual inspection of overlaid curves is also essential.
Spiked Recovery
Objective: To assess the assay's accuracy and matrix interference by measuring the recovery of a known quantity of purified analyte added (spiked) into the matrix. Protocol:
- Obtain a low-endogenous analyte pool (e.g., stripped matrix or sample with low baseline levels).
- Prepare "Spiked" samples by adding a known, moderate concentration of the purified analyte standard (from the ELISA kit) to the matrix. Prepare at least three spike levels (low, mid, high within the dynamic range).
- Prepare corresponding "Unspiked" samples (matrix + diluent only) and "Spike Standard" (analyte standard in diluent only) at the same nominal concentrations.
- Assay all samples in duplicate.
- Calculate Recovery: Observed Spike = [Spiked Sample] - [Unspiked Sample] % Recovery = (Observed Spike / Expected Spike) x 100 where Expected Spike is the nominal concentration of the added standard.
- Acceptance Criterion: Mean recovery is typically acceptable within 80-120%, with %CV <15% across spike levels.
Data Presentation
Table 1: Representative Linearity of Dilution Data for Salivary Cortisol ELISA
| Dilution Factor | Observed Conc. (ng/mL) | Back-Calculated Conc. (ng/mL) | % of Expected |
|---|---|---|---|
| Neat | 8.50 | 8.50 | 100.0 |
| 1:2 | 4.12 | 8.24 | 96.9 |
| 1:4 | 1.98 | 7.92 | 93.2 |
| 1:8 | 0.95 | 7.60 | 89.4 |
| Mean ± SD | 8.07 ± 0.38 | ||
| %CV | 4.7% |
Table 2: Spiked Recovery Assessment in Urine for 8-OHdG ELISA
| Spike Level (ng/mL) | Unspiked Conc. (ng/mL) | Spiked Observed (ng/mL) | Observed Spike | % Recovery |
|---|---|---|---|---|
| 2.0 | 0.5 | 2.45 | 1.95 | 97.5 |
| 10.0 | 0.5 | 10.2 | 9.7 | 97.0 |
| 25.0 | 0.5 | 24.1 | 23.6 | 94.4 |
| Mean Recovery % ± SD | 96.3 ± 1.6 | |||
| %CV | 1.7% |
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in Saliva/Urine ELISA Validation |
|---|---|
| Assay Diluent (Matrix-Specific) | Optimized buffer to reduce nonspecific binding and mimic the standard curve matrix for parallelism studies. |
| Analyte-Depleted/Stripped Matrix | Saliva or urine processed to remove endogenous analyte; critical baseline control for spike-recovery experiments. |
| Recombinant/Purified Biomarker Standard | High-purity analyte for generating standard curves and preparing precise spike solutions. |
| Protease & Phosphatase Inhibitor Cocktails | Added to sample collection tubes to prevent biomarker degradation in saliva/urine pre-assay. |
| Heterophilic Antibody Blocking Reagent | Suppresses interference from human anti-animal antibodies present in some samples. |
| Standard Curve Fitting Software | Enables 4PL or 5PL logistic regression for optimal curve fitting and parallelism slope analysis. |
Visualizations
Assay Validation Decision Workflow
Matrix Effects on Assay Parallelism
Within the context of developing and validating ELISA protocols for metabolic biomarkers in saliva and urine, the selection of appropriate controls is paramount. These biofluids present unique challenges, including high variability in sample composition, potential interfering substances, and analyte instability. Robust controls are non-negotiable for distinguishing true biological signal from analytical noise, ensuring inter-assay comparability, and validating the precision and accuracy of the method. This application note details the implementation of three cornerstone control strategies: pooled patient samples, internal standards, and commercial quality control (QC) materials.
Control Strategies: Definitions and Applications
Pooled Samples: Created by combining aliquots of actual patient saliva or urine samples. They represent the natural matrix and the average analyte concentration of the study population, serving as a process control for assay reproducibility. Internal Standards: Known quantities of a stable, often recombinant or synthetic, form of the analyte (or an analogous molecule) spiked directly into each sample prior to analysis. They correct for sample-specific losses during preparation. Commercial QC Materials: Lyophilized or liquid preparations of the target analyte in a defined matrix, available at multiple concentrations (e.g., low, medium, high). They provide an independent, standardized benchmark for assay accuracy and longitudinal performance.
Quantitative Comparison of Control Types
Table 1: Comparative Analysis of ELISA Control Strategies
| Feature | Pooled Patient Samples | Internal Standards | Commercial QC Materials |
|---|---|---|---|
| Primary Purpose | Monitor assay precision & drift; bridge data across plates/runs. | Correct for individual sample recovery & matrix effects. | Verify assay accuracy & standardization against a reference. |
| Matrix Relevance | High (identical to test samples). | High (processed within test sample). | Variable (may be artificial or surrogate matrix). |
| Concentration | Defined by the cohort; fixed once pooled. | Known spike concentration; can be titrated. | Pre-assigned target values & ranges. |
| Cost | Low (generated in-house). | Moderate (reagent purchase). | High (recurrent purchase). |
| Preparation | Labor-intensive; requires ethical approval & large sample volume. | Simple spike into each sample. | Reconstitution or direct use. |
| Best for | Inter-assay precision, longitudinal studies. | Normalization of recovery in complex matrices (e.g., saliva). | Initial validation, troubleshooting, regulatory compliance. |
Detailed Experimental Protocols
Protocol 4.1: Creation and Use of a Salivary Biomarker Pool
Objective: To generate a stable, representative pooled saliva sample for inter-plate QC.
- Collection: Collect saliva from ≥20 donors under standardized conditions (fasting, time of day). Centrifuge (10,000 x g, 10 min, 4°C) to remove debris. Store supernatants at -80°C.
- Screening & Pooling: Assay individual samples via ELISA. Exclude outliers (>3 SD from mean). Thaw qualified samples on ice, mix gently, and combine equal volumes into a sterile container.
- Aliquoting & Validation: Mix the pool thoroughly. Dispense into single-use aliquots (e.g., 100 µL) to avoid freeze-thaw cycles. Assay 20 aliquots across 5 separate days to establish a mean concentration and acceptable range (e.g., mean ± 2SD).
- Application: Include one aliquot of the pool in duplicate on every ELISA plate. Plot values on a Levey-Jennings control chart to monitor trends.
Protocol 4.2: Implementing a Protein-Based Internal Standard for Urine ELISA
Objective: To normalize for analyte loss during the sample pre-treatment phase of a urine biomarker assay.
- Selection: Choose a stable, non-human protein (e.g., plant protein) not found in urine that can be detected by a separate, orthogonal assay (e.g., fluorescent tag, different ELISA).
- Spiking: Add a fixed volume of the internal standard solution to each urine sample (test, calibrators, controls) immediately after thawing and prior to any centrifugation or dilution step.
- Parallel Analysis: Process the sample through the ELISA protocol. In a separate plate well or assay, quantify the recovered internal standard.
- Correction: Calculate the recovery percentage of the internal standard for each sample. Adjust the measured target analyte concentration: Corrected [Analyte] = (Measured [Analyte] / Recovery Fraction).
Protocol 4.3: Integrating Commercial QC Materials into a Validation Run
Objective: To verify the accuracy of a newly established salivary cortisol ELISA.
- Selection: Purchase QC materials at three levels (low, mid, high physiologic range). Record the lot-specific target value and range.
- Integration: Reconstitute or thaw QC materials according to the manufacturer's instructions. Include them as unknown samples in the ELISA run, in duplicate.
- Evaluation: Calculate the mean observed concentration for each QC level. Determine if the observed value falls within the manufacturer's stated acceptable range. Calculate percent bias: [(Observed - Target) / Target] x 100%. Bias should typically be <15-20%.
Visualizing Control Integration in the ELISA Workflow
Diagram Title: ELISA Workflow with Integrated Control Strategies
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Controlled Biomarker ELISA
| Item | Function & Rationale |
|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Gold standard for MS-based assays; chemically identical to analyte, corrects for extraction efficiency and ion suppression. |
| Recombinant Protein/Analyte Analog | Used as a non-isotopic internal standard or for spike-and-recovery experiments to assess matrix interference. |
| Matrix-Matched Commercial QC | Lyophilized QC material prepared in a proxy matrix (e.g., synthetic saliva, dialyzed urine) providing consistent performance. |
| Stable Coating Antibody/Buffer System | For generating in-house plate-based calibrators. Ensures the standard curve is exposed to the same capture surface as samples. |
| Protease & Phosphatase Inhibitor Cocktails | Added during saliva/urine collection and pooling to preserve native biomarker structure and concentration. |
| Blocking Buffer with Inert Proteins | Critical for reducing non-specific binding in complex matrices like saliva, improving signal-to-noise ratio. |
| Precision Pipettes & Calibrated Liquid Handler | Essential for accurate and reproducible spiking of internal standards and dispensing of QC materials. |
| Laboratory Information Management System (LIMS) | Tracks QC data, generates control charts, and flags deviations automatically for compliance. |
Ensuring Reliability: Validation, Cross-Platform Comparison, and Clinical Translation
1. Introduction Within the thesis "Development and Validation of a Multiplex ELISA for Metabolic Biomarkers in Saliva and Urine," establishing rigorous validation parameters is critical. This document outlines detailed application notes and protocols for determining Sensitivity (Limit of Detection - LOD, Limit of Quantification - LOQ), Precision, Accuracy, and Specificity. These parameters are essential for ensuring the reliability of biomarker data for research and drug development applications.
2. Key Validation Parameters: Definitions & Protocols
2.1. Sensitivity: LOD and LOQ
- Definition: LOD is the lowest analyte concentration detectable but not necessarily quantifiable. LOQ is the lowest concentration that can be quantified with acceptable precision and accuracy (typically ±20% CV and 80-120% recovery).
- Protocol:
- Prepare a dilution series of the analyte in the appropriate matrix (pooled, analyte-free saliva or urine).
- Analyze a minimum of 20 replicates of the blank (matrix alone) and low-concentration samples over multiple runs.
- LOD Calculation: Mean(blank) + 3SD(blank). Alternatively, use a calibration curve method: LOD = 3.3σ/S, where σ is the residual standard deviation of the regression line, and S is its slope.
- LOQ Calculation: Mean(blank) + 10SD(blank) or LOQ = 10σ/S. Verify that at the LOQ, the CV is ≤20% and recovery is 80-120%.
2.2. Precision
- Definition: The closeness of agreement between independent test results. It includes repeatability (intra-assay) and intermediate precision (inter-assay).
- Protocol:
- Use three quality control (QC) samples (low, medium, high concentration) in the relevant matrix.
- Repeatability: Analyze each QC sample in a minimum of 6 replicates within the same assay run.
- Intermediate Precision: Analyze each QC sample in duplicate across at least three independent assay runs, performed by different analysts on different days.
- Calculate the coefficient of variation (%CV) for each level.
2.3. Accuracy
- Definition: The closeness of agreement between the measured value and an accepted reference value (spike recovery).
- Protocol (Spike/Recovery):
- Prepare pooled saliva/urine samples. Spike known concentrations of the analyte into the matrix at three levels (low, mid, high).
- Analyze both spiked and unspiked samples. Calculate the recovered concentration: [Measured] - [Endogenous].
- Calculate %Recovery: (Recovered Concentration / Spiked Concentration) * 100.
- Parallelism (Dilutional Linearity): Assess by serially diluting a high-concentration sample with matrix and comparing measured vs. expected values.
2.4. Specificity/Selectivity
- Definition: The ability to measure the analyte unequivocally in the presence of interfering components (e.g., cross-reactivity, matrix effects).
- Protocol:
- Cross-Reactivity: Test structurally similar compounds (e.g., metabolic analogs) at high concentrations. Calculate %Cross-reactivity = (Measured Conc. of Analog / Actual Conc. of Analog) * 100.
- Matrix Interference: Compare the calibration curve in assay buffer to a curve prepared in the biological matrix (e.g., 10 different donor pools). Significant shifts in signal or parallelism indicate interference.
3. Summarized Quantitative Data from Validation Studies
Table 1: Example Validation Summary for a Salivary Cortisol ELISA
| Parameter | Result | Acceptance Criteria |
|---|---|---|
| LOD | 0.08 ng/mL | N/A |
| LOQ | 0.25 ng/mL | CV ≤20%, Recovery 80-120% |
| Precision (Intra-assay %CV) | Low QC: 5.2%, Med QC: 4.1%, High QC: 3.8% | <15% |
| Precision (Inter-assay %CV) | Low QC: 8.5%, Med QC: 7.2%, High QC: 6.9% | <20% |
| Accuracy (%Mean Recovery) | Low: 94%, Med: 102%, High: 97% | 80-120% |
| Specificity (vs. Corticosterone) | <0.1% Cross-reactivity | <1% |
Table 2: Key Research Reagent Solutions
| Item | Function in ELISA Validation |
|---|---|
| Analyte-Free Matrix | Pooled, charcoal-stripped saliva/urine for preparing calibration standards and assessing background. |
| High-Quality Calibrators | Pure analyte in defined solvent for generating the standard curve. |
| QC Samples (Low, Med, High) | Pooled matrix spiked with known analyte levels for monitoring precision and accuracy across runs. |
| Cross-Reactivity Panel | Structurally related compounds to test assay specificity. |
| Assay Buffer / Diluent | Optimized buffer to minimize matrix effects and maintain analyte stability. |
| Blocking Buffer | Protein solution (e.g., BSA) to prevent nonspecific binding to the plate. |
4. Experimental Workflow Diagram
Diagram 1: ELISA Validation Parameter Workflow
5. Detailed Experimental Protocol: Precision & Accuracy Run
Title: Protocol for a Combined Intra- and Inter-Assay Precision & Accuracy Experiment Objective: To determine repeatability, intermediate precision, and accuracy of the ELISA for a target metabolic biomarker in saliva. Materials: As per Table 2: Research Reagent Solutions. Procedure:
- Preparation: Thaw all QC samples (Low, Medium, High) and required matrix. Prepare calibration curve standards in analyte-free saliva.
- Plate Layout: Designate wells for blanks, standards (in duplicate), QCs (in sestuplicate), and any test samples.
- Assay Execution: Perform the ELISA according to the established protocol (incubation, washing, detection).
- Repetition: Repeat the entire experiment (Steps 1-3) on two additional days, using fresh reagents and a different analyst if possible.
- Data Analysis:
- Generate a standard curve and interpolate QC concentrations.
- Precision: Calculate the mean, SD, and %CV for each QC level within each run (intra-assay) and across all three runs (inter-assay).
- Accuracy: For each QC level, calculate %Bias: [(Mean Measured Concentration - Nominal Concentration) / Nominal Concentration] * 100.
This application note details protocols for correlating salivary biomarker measurements with serum/plasma gold standards using ELISA. Saliva offers a non-invasive sampling advantage for metabolic biomarker research in longitudinal and pediatric studies. However, establishing robust correlation requires stringent validation. This document provides a standardized framework for comparative analysis, central to thesis work on ELISA protocols for non-invasive biofluids.
The quantification of metabolic biomarkers in saliva via Enzyme-Linked Immunosorbent Assay (ELISA) presents a promising, non-invasive alternative to serum/plasma analysis. The core thesis of the broader research posits that with optimized protocols, salivary ELISA can achieve clinically acceptable correlation with established serum/plasma measurements, enabling its use in drug development pharmacokinetics (PK), pharmacodynamics (PD), and disease monitoring. Key challenges include lower analyte concentrations in saliva, variable sample viscosity, and the potential for matrix interference.
Key Comparative Data from Current Literature
Recent studies provide quantitative data on correlation strength (Pearson's r or Spearman's ρ) between salivary and serum/plasma ELISA results for various biomarker classes.
Table 1: Correlation Coefficients for Selected Metabolic Biomarkers
| Biomarker Class | Specific Analyte | Saliva vs. Serum r | Saliva vs. Plasma r | Sample Processing Note | Reference (Year) |
|---|---|---|---|---|---|
| Stress Hormones | Cortisol | 0.72 - 0.89 | 0.75 - 0.92 | Passive drool, centrifuged | Recent Meta-Analysis (2023) |
| Alpha-amylase | 0.45 - 0.65 | 0.50 - 0.68 | Saliva supernatant used | Recent Study (2024) | |
| Immune Markers | C-reactive Protein (CRP) | 0.60 - 0.78 | 0.58 - 0.80 | High-sensitivity ELISA required | Review (2023) |
| Interleukin-6 (IL-6) | 0.55 - 0.70 | 0.52 - 0.72 | Pre-treated with protease inhibitor | Study (2024) | |
| Drugs/Metabolites | Caffeine | 0.85 - 0.95 | 0.88 - 0.96 | Parotid saliva, timed collection | PK Study (2023) |
| Lithium | 0.80 - 0.90 | 0.82 - 0.91 | Stimulated whole saliva | Therapeutic Monitoring (2022) |
Table 2: Typical Concentration Ranges and ELISA Sensitivity Requirements
| Analyte | Typical Serum/Plasma Range | Typical Saliva Range | Recommended ELISA Sensitivity for Saliva |
|---|---|---|---|
| Cortisol | 2-20 µg/dL (AM) | 0.05-0.3 µg/dL | < 0.01 µg/dL |
| CRP | 0.1-10 mg/L | 0.001-0.1 mg/L | < 0.001 mg/L |
| IL-6 | 0-10 pg/mL | 0-5 pg/mL | < 0.5 pg/mL |
| Caffeine (post-dose) | 5-15 mg/L | 0.5-5 mg/L | < 0.1 mg/L |
Detailed Experimental Protocols
Protocol 1: Paired Sample Collection & Pre-processing
Objective: To collect matched saliva and blood samples from participants to minimize inter-individual and temporal variability in correlation studies.
Materials: Saliva collection aid (e.g., Salivette), serum separator tubes (SST), EDTA/K2 EDTA plasma tubes, centrifuge, -80°C freezer, cold chain equipment.
Procedure:
- Participant Preparation: Instruct participant to fast (water allowed) for 1 hour, avoid brushing teeth, eating, or drinking (except water) 30 minutes prior. Document time of collection.
- Simultaneous Collection:
- Saliva: Have participant passively drool into a polypropylene vial or use a synthetic swab (Salivette). Collection time: 2-5 minutes. For stimulated saliva, place 10 µL of 2% citric acid on tongue at 30s intervals.
- Blood: Draw venous blood via standard phlebotomy into SST (for serum) and EDTA tubes (for plasma).
- Immediate Processing:
- Saliva: Centrifuge swab/vial at 4°C, 1500-3000 x g for 15 minutes. Carefully aspirate the clear supernatant into a fresh cryovial. Avoid the mucin pellet.
- Blood for Serum: Allow SST to clot at RT for 30 min. Centrifuge at 4°C, 2000 x g for 10 min. Aliquot supernatant (serum).
- Blood for Plasma: Centrifuge EDTA tube at 4°C, 2000 x g for 10 min. Aliquot supernatant (plasma).
- Storage: Flash-freeze all aliquots in liquid nitrogen or dry ice and store at ≤ -80°C. Avoid repeated freeze-thaw cycles (maximum 2 cycles).
Protocol 2: Parallel Salivary & Serum/Plasma ELISA with Matrix Normalization
Objective: To run ELISA on paired samples using the same assay kit (or validated cross-reactive kits) with steps to mitigate saliva matrix effects.
Materials: Commercial ELISA kit validated for serum/plasma; PBS; protease inhibitor cocktail; bovine albumin (BSA); salivary alpha-amylase; plate reader.
Procedure:
- Kit Validation for Saliva: Perform a spike-and-recovery experiment (see Protocol 3) to confirm the kit's suitability for saliva.
- Sample Pre-treatment:
- Thaw samples on ice.
- Saliva: Dilute samples 1:2 to 1:5 in the provided assay diluent or PBS containing 0.5% BSA and 1X protease inhibitors. For amylase-rich samples, consider pre-incubation with an amylase inhibitor.
- Serum/Plasma: Use as per kit instructions, typically diluted in provided diluent.
- Parallel Assay Execution:
- Run all paired samples on the same microtiter plate to minimize inter-plate variance.
- Prepare standard curves using the kit's calibrator diluted in the same matrix as the sample (i.e., create a separate standard curve in artificial saliva/pooled saliva for salivary analysis if matrix effects are significant).
- Load samples and standards in duplicate or triplicate.
- Follow the kit's exact incubation, wash, and development steps.
- Data Calculation: Generate two standard curves (serum/plasma matrix and saliva matrix). Apply the respective curve to calculate concentrations for each sample type.
Protocol 3: Validation via Spike-and-Recovery & Linearity of Dilution
Objective: To assess accuracy and matrix interference in the salivary ELISA.
Materials: Purified biomarker standard, analyte-free saliva (pooled and charcoal-stripped), assay diluent.
Procedure:
- Spike-and-Recovery:
- Prepare a high-concentration spike solution of the purified analyte.
- Spike the solution into the analyte-free saliva pool at low, mid, and high concentrations within the assay's dynamic range.
- Run the spiked samples and an unspiked control through the ELISA.
- Calculate Recovery: % Recovery = [(Measured Conc. in Spiked Sample - Measured Conc. in Unspiked) / Theoretical Spike Conc.] x 100. Target: 80-120%.
- Linearity of Dilution:
- Take a native saliva sample with a high endogenous level of the analyte.
- Serially dilute it (e.g., 1:2, 1:4, 1:8) with the assay diluent or PBS.
- Run all dilutions in the ELISA.
- Assessment: The observed concentration should be proportional to the dilution factor. Plot observed vs. expected concentration; linear regression should have an R² > 0.95.
Visualization of Workflows & Relationships
Title: Workflow for Saliva-Serum ELISA Correlation Study
Title: Factors Affecting Saliva-Serum Biomarker Correlation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Saliva-Based ELISA Correlation Studies
| Item / Reagent Solution | Function & Importance | Example Product/Catalog Note |
|---|---|---|
| Passive Drool Collection Aid | Enables hygienic, standardized collection of whole saliva without stimulants that may dilute analyte. Critical for consistency. | Salimetrics Oral Swab (SOS), Salivette (polyester or synthetic). |
| Protease & Amylase Inhibitor Cocktail | Preserves protein/peptide biomarkers in saliva by inhibiting endogenous degradative enzymes, stabilizing samples pre-assay. | Ready-to-use cocktails from Sigma-Aldrich (e.g., P8340) or Salimetrics. |
| Artificial Saliva / Zero-Analyte Matrix | Serves as a diluent for creating saliva-specific standard curves and for use in spike-and-recovery validation experiments. | BioreclamationIVT Artificial Saliva, or prepared in-lab per ISO standards. |
| High-Binding, Low-Protein-Binding Microplates | Optimized plates ensure consistent antibody/antigen binding for the ELISA, minimizing non-specific binding from salivary mucins. | Nunc MaxiSorp (high binding), Corning Costar UltraLow Attachment plates. |
| High-Sensitivity ELISA Kit (HS) | Essential for detecting low-abundance analytes in saliva where concentrations can be 10-1000x lower than in serum. | Kits with detection limits in pg/mL or fg/mL range (e.g., R&D Systems HS Quantikine). |
| Matrix-Matched Calibrators | Calibrators prepared in artificial or pooled saliva. Corrects for matrix effects, improving accuracy of salivary quantification. | Must be prepared in-house from commercial calibrators or sourced from specialty vendors. |
| Polypropylene Collection & Storage Tubes | Prevents adsorption of hydrophobic biomarkers (e.g., steroids) to tube walls. Critical for accurate recovery. | DNA LoBind or Protein LoBind tubes from Eppendorf. |
Benchmarking ELISA Against Mass Spectrometry (LC-MS/MS) for Metabolite Quantification
This application note provides a comparative analysis of Enzyme-Linked Immunosorbent Assay (ELISA) and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) for quantifying low-molecular-weight metabolic biomarkers in saliva and urine matrices. Situated within a thesis on ELISA protocol development for non-invasive biomarker research, this document details experimental protocols, presents quantitative performance data, and discusses the complementary roles of these platforms in drug development and clinical research.
The quantification of metabolites in biofluids like saliva and urine is critical for research in metabolic disorders, oncology, and pharmacodynamics. ELISA offers high-throughput, antibody-based specificity, while LC-MS/MS provides broad, label-free multiplexing capability with high structural specificity. This benchmarking study evaluates their relative analytical performance for key metabolic biomarkers, including cortisol, 8-hydroxy-2'-deoxyguanosine (8-OHdG), and serotonin, in the context of non-invasive sampling.
Comparative Performance Data
Table 1: Analytical Performance Metrics for Salivary Cortisol Quantification
| Parameter | Sandwich ELISA (Commercial Kit) | LC-MS/MS (Reverse-Phase C18) |
|---|---|---|
| Lower Limit of Quantification (LLOQ) | 0.5 µg/dL | 0.1 µg/dL |
| Dynamic Range | 0.5 - 5.0 µg/dL | 0.1 - 50.0 µg/dL |
| Intra-Assay Precision (%CV) | 5.2% | 4.1% |
| Inter-Assay Precision (%CV) | 8.7% | 6.5% |
| Sample Volume Required | 50 µL | 10 µL |
| Total Assay Time | 3.5 hours | 25 minutes (runtime) + sample prep |
| Cross-Reactivity with Corticosterone | ~20% | None |
Table 2: Recovery and Matrix Effects in Urine (8-OHdG Spiked)
| Matrix | ELISA Mean Recovery (%) | LC-MS/MS Mean Recovery (%) | LC-MS/MS Matrix Suppression (%) |
|---|---|---|---|
| Neat Buffer | 98 | 99 | N/A |
| Diluted Urine (1:10) | 105 | 97 | 15% |
| Diluted Urine (1:5) | 118 | 95 | 32% |
Table 3: Comparative Workflow and Resource Analysis
| Aspect | ELISA | LC-MS/MS |
|---|---|---|
| Throughput (Samples/Operator Day) | 192 (single-plex) | 96 (multi-plex) |
| Capital Equipment Cost | Low (Plate Reader) | Very High (Triple Quadrupole MS) |
| Per-Sample Consumable Cost | Moderate | High |
| Technical Expertise Required | Moderate | Very High |
| Assay Development Timeline | Weeks (if kit exists) | Months |
| Multiplexing Capacity | Low (typically 1-2 analytes) | High (10-100s of analytes) |
Detailed Experimental Protocols
Protocol 1: Competitive ELISA for Salivary Cortisol
This protocol is optimized for 96-well plate format.
Materials: Salivary cortisol ELISA kit (e.g., Salimetrics), phosphate-buffered saline (PBS), microplate washer, absorbance reader (450 nm).
Procedure:
- Sample Preparation: Centrifuge saliva samples at 1500 x g for 15 minutes. Use supernatant directly or dilute 1:10 with assay buffer.
- Plate Setup: Add 25 µL of standard, control, or sample to appropriate wells pre-coated with cortisol conjugate.
- Add Antibody: Add 100 µL of cortisol antibody solution to each well. Incubate for 60 minutes at room temperature on a shaker.
- Wash: Aspirate and wash wells 4 times with 400 µL wash buffer.
- Add Substrate: Add 100 µL of Tetramethylbenzidine (TMB) substrate. Incubate for 30 minutes in the dark.
- Stop Reaction: Add 100 µL of stop solution (1M H2SO4).
- Read Plate: Measure absorbance at 450 nm within 10 minutes. Calculate concentrations using a 4-parameter logistic (4PL) curve fit.
Protocol 2: LC-MS/MS Quantification of Urinary 8-OHdG and Creatinine
This protocol uses reversed-phase chromatography and negative electrospray ionization.
Materials: Acquity UPLC HSS T3 column (1.8 µm, 2.1 x 100 mm), Triple quadrupole mass spectrometer (e.g., SCIEX 6500+), 8-OHdG and 8-OHdG-¹⁵N₅ (internal standard), creatinine-d₃, 0.1% Formic acid in water and methanol.
Procedure:
- Sample Preparation: Thaw urine on ice. Centrifuge at 14,000 x g for 10 min. Dilute 50 µL supernatant with 200 µL of internal standard solution (8-OHdG-¹⁵N₅ and creatinine-d₃ in 0.1% FA).
- LC Conditions: Column temperature: 40°C. Flow rate: 0.4 mL/min. Mobile Phase A: 0.1% FA in H₂O; B: 0.1% FA in MeOH. Gradient: 2% B to 95% B over 7 minutes.
- MS/MS Conditions: Ionization: ESI-, MRM mode. Source temp: 500°C. For 8-OHdG: Q1 283.1 > Q3 167.0 (quantifier). For creatinine: Q1 112.1 > Q3 44.1.
- Data Analysis: Quantify using the ratio of analyte peak area to internal standard peak area, plotted against a calibration curve (1-500 ng/mL for 8-OHdG). Normalize 8-OHdG concentration to urinary creatinine.
Visualizations
Title: ELISA Protocol Key Steps
Title: LC-MS/MS Core Workflow
Title: Platform Selection Decision Guide
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions for Biomarker Quantification
| Item | Function & Rationale |
|---|---|
| Stable Isotope-Labeled Internal Standards (e.g., Cortisol-d4) | Added to samples prior to LC-MS/MS processing to correct for variable matrix effects, ion suppression, and recovery losses during sample preparation. |
| MRM Transition Libraries | Pre-optimized lists of precursor → product ion pairs for known metabolites, accelerating LC-MS/MS method development and enabling targeted multiplexing. |
| Matched Antibody Pair (Capture & Detection) | Essential for developing a sensitive and specific sandwich ELISA; requires validation for the target metabolite in the specific biofluid matrix. |
| Competitive ELISA Coating Antigen | A known quantity of the target metabolite (or analog) immobilized on the plate to compete with the analyte in the sample for antibody binding. |
| SPE Cartridges (Mixed-Mode) | For solid-phase extraction (SPE) cleanup of saliva/urine prior to LC-MS/MS; removes salts and interfering compounds, improving sensitivity. |
| Chromatographic Guard Column | A short column placed before the analytical column to protect it from particulates and irreversibly binding matrix components in biological samples. |
| Blocking Buffer (e.g., BSA in PBS-T) | Used in ELISA to coat any remaining protein-binding sites on the plate after coating, minimizing non-specific binding of antibodies. |
| MS-Compatible Mobile Phase Additives (e.g., Formic Acid) | Enhances analyte ionization efficiency in ESI and improves chromatographic peak shape; must be volatile to not contaminate the MS ion source. |
ELISA provides a robust, accessible, and high-throughput platform for quantifying specific metabolites when validated kits are available, making it suitable for focused clinical studies. LC-MS/MS offers superior specificity, wider dynamic range, and powerful multiplexing capabilities, albeit with higher cost and complexity, making it ideal for discovery-phase research and assays requiring absolute structural confirmation. A tiered approach, using LC-MS/MS for initial assay development and validation and ELISA for subsequent large-scale clinical application, represents an effective strategy within a thesis focused on advancing non-invasive metabolic biomarker research.
1. Introduction Within the broader thesis on ELISA protocol development for metabolic biomarkers in saliva and urine research, cortisol stands out as a critical steroid hormone and biomarker of the hypothalamic-pituitary-adrenal (HPA) axis. Tracking its diurnal rhythm and acute stress responses in saliva provides a non-invasive window into metabolic and psychological stress, relevant for psychiatric disorders, endocrine diseases, and drug development. This application note details protocols and considerations for reliable salivary cortisol assessment.
2. The Scientist's Toolkit: Research Reagent Solutions Table 1: Essential Materials for Salivary Cortisol ELISA
| Item | Function/Benefit |
|---|---|
| High-Sensitivity Salivary Cortisol ELISA Kit | Specifically designed to measure the low concentrations (nmol/L range) found in saliva, with antibodies cross-reactive for free cortisol. |
| Saliva Collection Device (e.g., Sarstedt Salivette) | Contains a neutral cotton swab; standardizes collection, minimizes interference, and simplifies sample processing. |
| Microplate Reader (450 nm filter) | For measuring the absorbance of the stopped ELISA reaction, quantifying cortisol concentration. |
| Vortex Mixer & Centrifuge | Essential for homogenizing saliva samples and precipitating mucins/debris after thawing and before assay. |
| Piperting System (10-1000 µL) | For accurate transfer of standards, samples, and reagents in microliter volumes. |
| ELISA Data Analysis Software | Converts absorbance values into concentrations using a 4- or 5-parameter logistic (4PL/5PL) curve fit. |
3. Experimental Protocol: Saliva Collection, Processing, and ELISA
3.1. Participant Preparation & Sample Collection
- Instructions to Participants: Avoid eating, drinking (except water), brushing teeth, or using tobacco for at least 60 minutes prior to collection. Rinse mouth with water 10 minutes before.
- Timed Collection: For diurnal profiles, collect immediately upon waking (0 min), then at +30 min, +60 min, and in the evening (e.g., 10 PM).
- Procedure: Place the cotton swab of the collection device in the mouth until saturated (1-3 minutes). Do not chew. Place swab back into the tube without touching it.
3.2. Sample Processing & Storage
- Centrifuge collection tubes at 4°C, 1500 x g for 10-15 minutes.
- Transfer the clear supernatant (saliva) into a cryovial.
- Store samples at ≤ -20°C immediately; for long-term storage, use -80°C. Avoid repeated freeze-thaw cycles (>2 cycles).
3.3. Salivary Cortisol ELISA Procedure (Adapted from typical commercial kit protocols) Table 2: Typical ELISA Protocol Steps and Parameters
| Step | Parameter | Details |
|---|---|---|
| Sample Prep | Thawing & Centrifugation | Thaw samples on ice or at 4°C. Re-centrifuge at 10,000 x g for 10 min at 4°C to remove precipitates. |
| Assay Setup | Standard Curve Range | 0.012 - 3.0 µg/dL (or 0.33 - 82.8 nmol/L). Includes a zero (0) standard. |
| Incubation | Volume & Time | Add 25-100 µL of standard/sample per well. Add conjugate (cortisol-HRP), then antibody. Incubate 60-120 min at room temp (RT) on a plate shaker. |
| Washing | Cycles & Buffer | Wash 3-6 times with 300 µL/well of diluted wash buffer. Blot thoroughly. |
| Detection | Substrate Incubation | Add TMB substrate (100 µL/well). Incubate in the dark for 15-30 min at RT. |
| Stop & Read | Solution & Wavelength | Add 50-100 µL stop solution (e.g., 1M H₂SO₄). Read absorbance at 450 nm within 15 min. |
| Analysis | Curve Fit | Use 4PL or 5PL regression on software. Multiply result by sample dilution factor. |
4. Data Presentation and Interpretation Table 3: Representative Salivary Cortisol Data from a Diurnal Rhythm Study
| Subject Group | Cortisol Awakening Response (CAR) AUC (nmol/L•min) | Morning Peak (nmol/L) | Evening Level (nmol/L) | Diurnal Slope |
|---|---|---|---|---|
| Healthy Controls (n=25) | 250.4 ± 45.2 | 15.3 ± 3.1 | 2.1 ± 0.9 | -0.55 ± 0.12 |
| Major Depressive Disorder (n=25) | 145.8 ± 67.5* | 12.1 ± 4.8 | 4.5 ± 2.1* | -0.28 ± 0.15* |
| Burnout Patients (n=25) | 85.3 ± 52.1* | 9.8 ± 3.5* | 3.8 ± 1.8* | -0.23 ± 0.10* |
(p < 0.05 vs. Controls; AUC: Area Under the Curve; Data is illustrative)*
5. Key Signaling Pathway and Workflow
Diagram 1: HPA Axis to Salivary Cortisol ELISA Workflow (85 chars)
Diagram 2: End-to-End Salivary Cortisol Research Protocol (85 chars)
This application note is a component of a broader thesis investigating the optimization of Enzyme-Linked Immunosorbent Assay (ELISA) protocols for the quantification of metabolic biomarkers in non-invasive biofluids, specifically saliva and urine. Within drug development, the monitoring of renal safety biomarkers in urine is a critical application. The reliable detection of biomarkers such as Cystatin C, Neutrophil Gelatinase-Associated Lipocalin (NGAL), and Kidney Injury Molecule-1 (KIM-1) via ELISA allows for the early identification of drug-induced kidney injury (DIKI), enabling timely intervention and compound selection. This case study details the protocol and considerations for quantifying these key renal biomarkers in urine matrices.
Key Renal Biomarkers and Their Significance
The table below summarizes primary urinary renal biomarkers monitored in preclinical and clinical drug development.
Table 1: Key Urinary Renal Biomarkers for Drug Safety Assessment
| Biomarker | Full Name | Primary Renal Source | Clinical Significance in DIKI | Typical Assay Range (Urine) |
|---|---|---|---|---|
| NGAL | Neutrophil Gelatinase-Associated Lipocalin | Proximal Tubule, Loop of Henle | Very early marker of proximal tubular damage; rises within 2-6 hours. | 0.1 - 1000 ng/mL |
| KIM-1 | Kidney Injury Molecule-1 | Proximal Tubule | Specific to renal injury; indicates dedifferentiation and repair processes. | 0.01 - 10 ng/mL |
| Cystatin C | Cystatin C | Glomerular Filtration (filtered) | Sensitive marker of glomerular filtration rate (GFR) changes. | 10 - 5000 ng/mL |
| Clusterin | Clusterin (Apolipoprotein J) | Distal Tubule, Collecting Duct | Marker of chronic/repetitive injury and tubular regeneration. | 1 - 500 ng/mL |
| Osteopontin | Osteopontin | Thick Ascending Limb, Distal Tubule | Indicates inflammation and macrophage infiltration. | 10 - 2000 ng/mL |
Detailed ELISA Protocol for Urinary NGAL
This protocol exemplifies a sandwich ELISA suitable for quantifying NGAL in rat or human urine, adaptable to other biomarkers with appropriate antibody pairs.
Materials & Pre-Assay Preparation:
- Coated Plate: 96-well microplate pre-coated with capture anti-NGAL antibody.
- Standards: Recombinant NGAL protein in standard diluent (e.g., assay buffer + 1% BSA). Prepare a 7-point serial dilution.
- Samples: Fresh or frozen (-80°C) urine samples. Centrifuge at 10,000×g for 10 minutes to remove debris. Dilute samples 1:10 to 1:100 in assay buffer to fall within the standard curve.
- Detection Antibody: Biotinylated anti-NGAL detection antibody.
- Streptavidin-HRP: Streptavidin conjugated to Horseradish Peroxidase.
- Wash Buffer: PBS with 0.05% Tween-20.
- Substrate: TMB (3,3',5,5'-Tetramethylbenzidine).
- Stop Solution: 1M Sulfuric Acid or 1M Phosphoric Acid.
- Microplate Reader capable of measuring absorbance at 450 nm (and 570/630 nm for wavelength correction).
Procedure:
- Reagent Preparation: Bring all reagents, samples, and standards to room temperature (RT). Prepare all working solutions as per kit instructions.
- Standard & Sample Addition: Add 100 µL of each standard, diluted sample, and blank (assay buffer) to appropriate wells. Incubate for 2 hours at RT on a plate shaker.
- Washing: Aspirate liquid and wash each well 4 times with 300 µL wash buffer. Blot plate on clean absorbent paper.
- Detection Antibody Incubation: Add 100 µL of biotinylated detection antibody to each well. Incubate for 1 hour at RT on a shaker. Repeat wash step (Step 3).
- Enzyme Conjugate Incubation: Add 100 µL of Streptavidin-HRP solution to each well. Incubate for 30 minutes at RT on a shaker, protected from light. Repeat wash step (Step 3).
- Substrate Reaction: Add 100 µL of TMB substrate to each well. Incubate for 15-20 minutes at RT in the dark until a clear blue color develops.
- Stop Reaction: Add 100 µL of stop solution to each well. The color will change from blue to yellow.
- Measurement: Measure the absorbance at 450 nm within 30 minutes. Subtract any background measurement at 570 nm or 630 nm.
- Data Analysis: Generate a standard curve (4- or 5-parameter logistic fit) using the average absorbance of the standards. Interpolate sample concentrations from the curve and apply the dilution factor.
Critical Notes:
- Matrix Effects: Always prepare standards in a matrix matching the sample (e.g., pooled normal urine at the same dilution) if the kit does not provide validated matrix-specific standards.
- Normalization: Report biomarker concentration normalized to urinary creatinine to account for urine dilution variability.
Pathway and Workflow Visualizations
Diagram Title: Pathway of Drug-Induced Kidney Injury & Biomarker Detection
Diagram Title: Urinary Biomarker ELISA Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Urinary Renal Biomarker ELISA
| Item | Function & Importance |
|---|---|
| High-Bind ELISA Plates | Polystyrene plates with superior protein binding capacity for effective capture antibody coating. |
| Matched Antibody Pair | A pair of monoclonal/polyclonal antibodies targeting different epitopes on the biomarker for sandwich ELISA specificity. |
| Recombinant Protein Standard | Highly purified, quantified protein for generating the standard curve, essential for accurate quantification. |
| Biotin-Streptavidin System | Amplification system (biotinylated detection Ab + Streptavidin-HRP) that enhances assay sensitivity. |
| Stable Chemiluminescent/Colorimetric Substrate | TMB or other substrates provide a stable, sensitive signal for HRP, proportional to biomarker concentration. |
| Urine Creatinine Assay Kit | Essential companion assay to normalize biomarker concentration for urine flow rate, critical for data interpretation. |
| Matrix-Matched Calibrator Diluent | Buffer spiked with inert protein or pooled normal urine to mimic sample matrix and correct for interference in standards. |
| Plate Sealer & Automated Washer | Ensures consistent incubation conditions and reproducible, thorough washing to reduce background noise. |
Application Notes
The integration of multiplex ELISA arrays and point-of-care (POC) devices represents a paradigm shift in metabolic biomarker research, enabling high-throughput, minimally invasive monitoring. Saliva and urine, as readily available biofluids, contain a diverse array of metabolic indicators for stress, inflammation, cardiovascular risk, and endocrine function. Traditional single-analyte ELISA protocols, while foundational, are labor-intensive and sample-volume consuming for comprehensive metabolic panels. The evolution toward multiplexed, automated, and decentralized testing addresses these limitations, accelerating biomarker validation and clinical translation.
Table 1: Comparison of ELISA Formats for Metabolic Biomarker Analysis
| Feature | Traditional Sandwich ELISA | Multiplex ELISA Array (Luminex/MSD) | Emerging POC ELISA Device |
|---|---|---|---|
| Analytes per Run | 1 | Up to 100+ | Typically 1-10 |
| Required Sample Volume | 50-100 µL per analyte | 25-50 µL for a full panel | 10-50 µL total |
| Throughput Time | 4-8 hours (hands-on) | 3-5 hours (mostly automated) | 10-30 minutes |
| Sensitivity (Typical) | Low pg/mL | Comparable or slightly lower | 1-2 log lower |
| Primary Advantage | Gold standard, high sensitivity | Multiplexing, sample efficiency | Speed, ease-of-use, portability |
| Key Challenge | Low multiplexing, high volume | Complex data analysis, cost | Limited multiplexing, sensitivity |
| Best For | Single biomarker validation | Discovery/validation panels | Rapid screening, field use |
Table 2: Promising Saliva/Urine Metabolic Biomarkers for Multiplex/POC Development
| Biomarker Category | Example Analytes (Saliva) | Example Analytes (Urine) | Associated Metabolic Process |
|---|---|---|---|
| Stress & HPA Axis | Cortisol, Alpha-amylase, DHEA | Cortisol, Cortisone, Norepinephrine | Glucocorticoid metabolism |
| Oxidative Stress | 8-OHdG, Malondialdehyde (MDA) | 8-isoprostane, MDA, GSH/GSSG Ratio | Lipid peroxidation, redox balance |
| Inflammation | IL-1β, IL-6, TNF-α, CRP | MCP-1, NGAL, IL-8 | Innate immune response |
| Cardiometabolic Risk | MMP-9, Myeloperoxidase | KIM-1, Cystatin C, Microalbumin | Tissue remodeling, renal function |
Experimental Protocols
Protocol 1: Multiplex ELISA Array for a Salivary Cytokine & Stress Hormone Panel
- Objective: Simultaneously quantify IL-1β, IL-6, TNF-α, and Cortisol from a single saliva sample.
- Principle: Magnetic bead-based immunoassay (Luminex xMAP technology). Beads are dyed with distinct fluorescent intensities, each conjugated to a unique capture antibody. Analytes are detected via biotinylated detection antibodies and streptavidin-phycoerythrin.
- Materials: Human Salivary Cytokine Magnetic Bead Panel (e.g., MilliporeSigma), Biotinylated Cortisol Conjugate, Phosphate-Buffered Saline (PBS), Bovine Serum Albumin (BSA), Tween-20, Streptavidin-PE, Luminex analyzer.
- Procedure:
- Sample Preparation: Centrifuge saliva samples at 10,000 x g for 10 min at 4°C. Use clear supernatant. Dilute 1:2 with assay buffer.
- Bead Preparation: Vortex magnetic bead suspension for 60 sec. Add 25 µL of mixed beads to each well of a 96-well filter plate.
- Wash: Wash plate 2x with 100 µL wash buffer using a vacuum manifold.
- Incubation: Add 25 µL of standards, controls, or samples to appropriate wells. Add 25 µL of detection antibody cocktail (includes biotinylated cortisol competitor). Seal and incubate for 2 hours on a plate shaker at room temperature, protected from light.
- Detection: Wash plate 2x. Add 50 µL of Streptavidin-PE to each well. Incubate for 30 minutes on a shaker.
- Wash & Resuspend: Wash plate 3x. Add 100 µL of sheath fluid to resuspend beads. Analyze immediately on the Luminex analyzer.
- Data Analysis: Use a 5-parameter logistic curve to calculate analyte concentrations from median fluorescent intensity (MFI).
Protocol 2: Lateral Flow POC Device Prototype for Urinary NGAL
- Objective: Rapid, semi-quantitative detection of Neutrophil Gelatinase-Associated Lipocalin (NGAL) for acute kidney injury screening.
- Principle: Competitive or sandwich lateral flow immunoassay. For NGAL (higher concentration), a sandwich format is typical.
- Materials: Nitrocellulose membrane, conjugate pad (Gold nanoparticle-anti-NGAL), sample pad, absorbent pad, backing card, monoclonal anti-NGAL (test line), goat anti-mouse IgG (control line), urine collection cup.
- Procedure:
- Conjugate Application: Apply gold nanoparticle-antibody conjugate to the conjugate pad and dry.
- Membrane Stripping: Strip the nitrocellulose membrane with capture antibody (Test line, T) and control antibody (Control line, C) using a dispenser. Dry.
- Assembly: Laminate sample pad, conjugate pad, membrane, and absorbent pad onto a backing card. Cut into individual strips.
- Assay Run: Dip the strip sample pad into 100 µL of untreated urine sample. Allow capillary flow for 10-15 minutes.
- Reading: Visual or smartphone-based readout. The appearance of both T and C lines indicates a positive result. The intensity of the T line inversely correlates with NGAL concentration when using a reader.
Visualizations
Multiplex ELISA Array Workflow for Biomarker Panels
Lateral Flow POC Device Assembly and Flow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Role in Research |
|---|---|
| Magnetic Bead Panels (Luminex/MSD) | Pre-configured multiplex assay kits with spectrally distinct beads, enabling simultaneous quantification of curated biomarker panels from minimal sample volume. |
| High-Sensitivity ELISA Kits (Single-Plex) | Essential for validating the performance (sensitivity, dynamic range) of new biomarkers before their inclusion in multiplex arrays. Often the gold standard. |
| Stabilized Biotinylated Detection Antibodies | Critical for multiplex assay development; biotinylation allows universal detection via Streptavidin-PE, and stabilization ensures batch-to-batch consistency. |
| Matrix-Matched Standards & Controls | Calibrators and controls prepared in artificial saliva or synthetic urine are vital for accurate quantification, correcting for sample matrix effects. |
| Gold Nanoparticles (AuNPs) / Latex Microspheres | The primary signaling labels (conjugates) in lateral flow POC devices. Their size and conjugation efficiency directly impact test sensitivity. |
| Nitrocellulose Membranes (Various Pore Sizes) | The substrate for capillary flow and antibody immobilization in lateral flow strips. Pore size controls flow rate and assay time. |
| Recombinant Antigen Proteins | Used as positive controls, for standard curve generation, and for spiking experiments to determine recovery and interference in complex saliva/urine matrices. |
Conclusion
ELISA remains a robust, accessible, and highly adaptable platform for the quantification of metabolic biomarkers in saliva and urine, offering significant value for non-invasive monitoring in research and drug development. Success hinges on a deep understanding of sample-specific pre-analytical variables, meticulous protocol optimization to overcome matrix effects, and rigorous analytical validation. While challenges related to sensitivity and multiplexing exist, ELISA provides a reliable bridge between discovery-phase mass spectrometry and potential clinical deployment. Future directions will likely involve the increased adoption of validated salivary and urinary ELISA panels for dynamic metabolic phenotyping, their integration into digital health platforms for remote sampling, and their crucial role in de-risking drug candidates by providing early, non-invasive pharmacodynamic readouts. By adhering to the principles outlined across foundational knowledge, methodological rigor, troubleshooting, and validation, researchers can confidently generate high-quality, reproducible data from these valuable biofluids.